Short abstract
Midregional pro-atrial natriuretic peptide (MR-proANP), first isolated in 1981, is a novel peptide with multiple biological functions, especially within the cardiovascular system. This peptide plays an important role in many processes, including natriuresis, diuresis, and other physiological and pathophysiological pathways in the human body. Several electronic databases (PubMed, EBSCO, Scopus, and ScienceDirect) were analyzed in the present literature review. The aim of this study was to elucidate the wide roles of MR-proANP, which can be analyzed because of the development of a new sandwich immunoassay, and to determine the possible diagnostic and prognostic implications of MR-proANP on cardiovascular disease and other disorders. The studies discussed in this literature review provide valuable data on the role of ANP in the pathogenesis, diagnostic process, prognosis, and potential therapeutic strategies for disease. Although ANP is mainly associated with cardiovascular disease, it may be used as a biomarker in diabetology, neurology, and metabolic disorders.
Keywords: MR-proANP, cardiovascular disease, heart failure, myocardial infarction, natriuretic peptides, biomarker
Clinical significance: The MR-proANP level may be useful in patients with many disorders. For instance, it may be used:
To diagnose and assess the severity of both chronic and acute heart failure
To indicate the risk of major cardiovascular events (such as nonfatal myocardial infarction or death from cardiovascular disease) and the development of diabetes
To indicate the time from onset of atrial fibrillation to presentation
To predict mortality in patients with stroke
As a prognostic biomarker of renal progression
Introduction
Midregional pro-atrial natriuretic peptide (MR-proANP) is a novel peptide with multiple biological functions, especially in the cardiovascular system. Its use as a biomarker has gained growing interest in the last few years.
ANP plays an important role in the regulation of many physiological and pathophysiological pathways. Thus far, the role of ANP has been determined in natriuresis, diuresis, vasodilatation and inhibition of the renin-angiotensin-aldosterone system, and the sympathetic nervous system.1 Studies have shown that pathologies within the above-mentioned mechanisms are also partially dependent on the function of ANP. Investigators have described the role of ANP in the pathogenesis of acute ischemic stroke,2–4 diabetes,5–8 chronic kidney disease,9,10 and lung disease (especially pneumonia).
However, few studies have addressed the role of MR-proANP, and much remains unknown. This review was performed to elucidate the wide role of MR-proANP, which can be analyzed because of the development of a new sandwich immunoassay,11 and determine the possible diagnostic and prognostic implications of MR-proANP in cardiovascular disease and other disorders.
Methods
The literature review involved the analysis of several electronic databases: PubMed, EBSCO, Scopus, and ScienceDirect. The search results were based on keywords consistent with the language of the Medical Subject Headings of the National Library of Medicine (MR-proANP, acute and chronic heart failure, myocardial infarction, arrhythmia, dyspnea, acute ischemic stroke, diabetes, and chronic kidney disease). Several publications dated from 1986 to 2016, available in both English and Polish, were analyzed. This study protocol was approved by the Bioethical Commission of Medical University in Lodz.
Results
ANP as a peptide
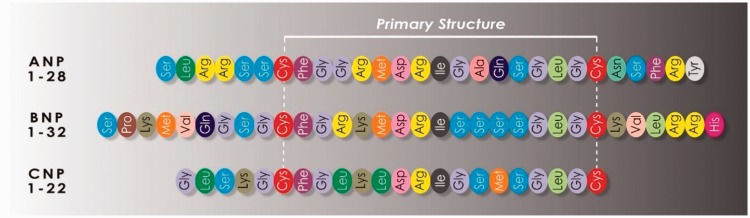
In 1981, after many years of study, de Bold et al.12 proved for the first time that intravenous administration of atrial myocardial extract evokes diuretic and natriuretic effects in rats. This and subsequent experiments led to the discovery of a whole family of peptides with natriuretic, diuretic, and smooth muscle-relaxing properties: the so-called natriuretic peptides.1 Among them, we have recognized the following to date: ANP; brain natriuretic peptide, also called B-type natriuretic peptide (BNP); and C-type natriuretic peptide (CNP) (Figure 1).
Figure 1.
Structure of the natriuretic peptides.
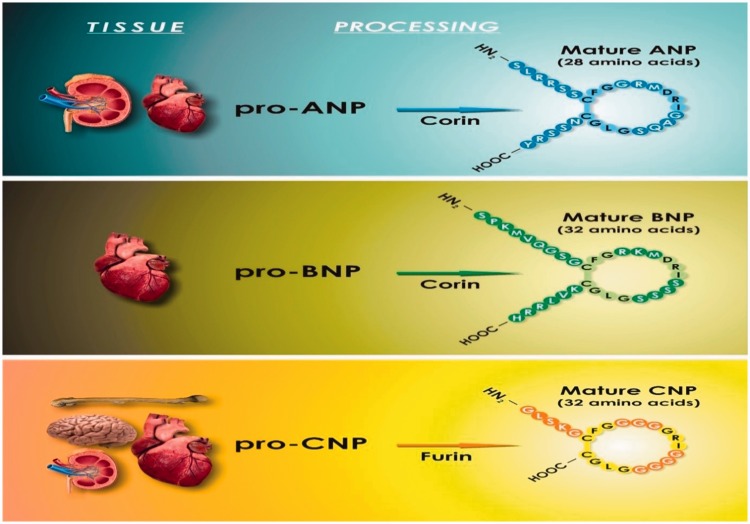
The ANP propeptide is composed of 151 amino acid residues. Hydrolysis of the N-terminus part leads to the formation of pro-ANP consisting of 126 amino acid residues. In the next phase, the pro-ANP is released into the blood circulation, where it is digested by corin (ANP-converting enzyme) to the N-terminus fragment consisting of 98 amino acids and the C-terminus fragment consisting of 28 amino acids (i.e., the active form of ANP) (Figure 2).1
Figure 2.
Tissue expression of natriuretic peptides and conversion from prohormones to mature peptides.
Mature ANP is encoded by the NPPA gene located in the short arm of chromosome 1, which contains three exons and two introns. Its expression changes during an organism’s development; in an adult human, ANP is present mainly in the cardiac atria.1
ANP release depends on many factors, such as the secretion of catecholamines, endothelins, arginine vasopressin, or thyroid hormones. An increased intravascular volume with a resultant increase in vascular wall tension, chronic hypoxia, and increased osmolarity are also stimulators of ANP release.1
Natriuretic peptide receptors
Guanylyl cyclase receptors
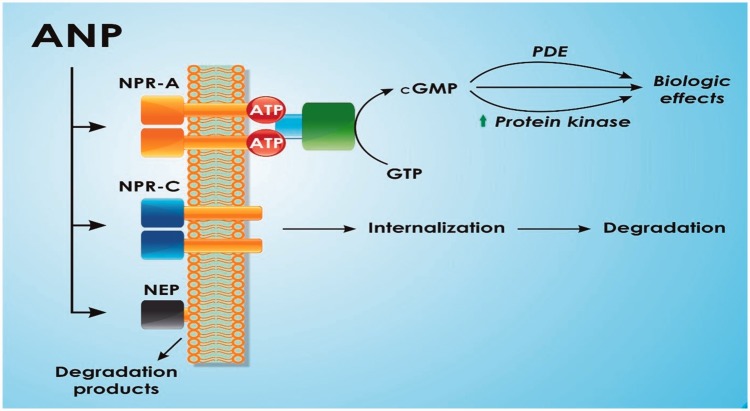
Natriuretic peptides act by affecting membrane receptors on the surface of target cells. There are three types of these receptors: natriuretic peptide receptor (NPR)-A, NPR-B, and NPR-C. NPR-A shows the highest binding affinity to ANP with lower affinity to BNP and CNP, whereas NPR-B binds mainly CNP and to a lesser extent to ANP and BNP. The highest expression of the NPR-A gene can be found in the heart, blood vessels, kidneys, adrenal glands, and lungs, whereas the NPR-B gene is mainly expressed in the brain.1
NPR-A and NPR-B are transmembrane proteins that belong to the family of guanylate cyclase-associated receptors. After ligand binding by the receptor, guanosine triphosphate is converted to cyclic guanosine monophosphate, starting the signal cascade in the cell that translates into the physiological effects of natriuretic peptides.1
Natriuretic peptide clearance receptor
NPR-C is regarded as the elimination receptor because its main action is removal of natriuretic peptides from the blood circulation (the ligand–NPR-C complex is subjected to internalization and degradation). Natriuretic peptides can also be removed by neutral endopeptidase, which is present in the blood vessels and kidneys.1
The action of ANP at cells is presented in Figure 3.
Figure 3.
Action of atrial natriuretic peptide (ANP) at target cells. After ANP binding by natriuretic peptide receptor (NPR)-A, guanosine triphosphate is converted to cyclic guanosine monophosphate, starting the signal cascade in the cell that translates into the physiological effects of natriuretic peptides. ANP also binds to NPR-C, after which it is removed from the blood circulation. Finally, ANP may be removed by extracellular neutral endopeptidases.
Physiologic effects of natriuretic peptides
The effects of the actions of natriuretic peptides are multidirectional. They maintain the appropriate blood pressure and volume of circulating blood by decreasing cardiac preload and afterload as well as widening blood vessels.1,13
At the renal level, natriuretic peptides lead to contraction of efferent arterioles and relaxation of afferent arterioles in nephrons, which increases the activity and amount of glomerular filtration. Natriuretic peptides decrease sodium reabsorption in renal tubules, thus leading to natriuresis. They also inhibit renin, angiotensin, and aldosterone secretion.1,13
Additionally, natriuretic peptides increase vascular wall permeability and increase fluid shift from the intravascular to extravascular compartment, thus enhancing the hypotensive effect evoked by natriuresis and vasodilation.1,13
The physiological actions of natriuretic peptides are listed in Table 1.
Table 1.
Physiological actions of natriuretic peptides (based on Volpe et al.)
| Target | Biological effects |
|---|---|
| Kidney |
|
| Heart |
|
| Hemodynamic system |
|
| Endocrine system |
|
ANP in the cardiovascular system: pathophysiology
Because of the development of a new sandwich immunoassay that recognizes a midregional sequence of pro-ANP, we can analyze MR-proANP and use it as a promising biomarker in many disorders.11 It has been hypothesized that MR-proANP might be more useful than ANP or its precursor fragments because of its greater analytical stability, lack of receptor binding and protein interactions, and longer half-life.11
Chronic heart failure
As indicated in the 2016 European Society of Cardiology guidelines,14 the prevalence of heart failure (HF) is approximately 1% to 2% of the adult population in developed countries and exceeds 10% among people >70 years of age. It is a very common cause of hospitalization in patients >65 years of age (among this group of patients presenting to primary care facilities with breathlessness on exertion, one in six will have unrecognized HF). The lifetime risk of HF at age 55 years is 33% for men and 28% for women.14
Patients with HF often exhibit nonspecific signs and symptoms, making discrimination between HF and other conditions difficult. This heterogeneity of presentation results in delays in definitive diagnosis and treatment.
The natriuretic peptides (ANP and BNP) represent the gold standard biomarkers in HF. The cardiac hypertrophy that accompanies myocardial failure causes increased ventricular production of ANP and BNP.1 These peptides have been established not only as excellent diagnostics markers but also as very useful parameters with which to assess the disease severity15 and prognosis.16 The most commonly measured natriuretic peptide, which is used in the diagnosis of HF, is BNP and its precursor N-terminal proBNP (NT-proBNP). ANP is currently considered inferior to BNP, mostly because the assessment of ANP is considered less reproducible.17
In a few studies, MR-proANP was suggested to be a more distinct marker of cardiac abnormalities and risk than BNP in subgroups of patients with confounding conditions that were difficult to assess.18 von Haehling et al.19 proved that in patients with chronic HF, elevated levels of MR-proANP were associated with an increased risk of death, and this effect was independent of other established prognosticators including the left ventricular ejection fraction (LVEF), NT-proBNP, New York Heart Association class, sex, age, and creatinine level. Their analyses also revealed that MR-proANP predicts mortality in specific subgroups of patients such as those with mildly impaired kidney function and obesity.19 Moertl et al.20 showed that MR-proANP outperformed NT-proBNP and BNP in prediction of death. Compared with an earlier study, they suggested that natriuretic peptides were more highly dependent on the LVEF, glomerular filtration rate, and presence of ankle edema and confirmed that age, body mass index, and sex do not have a major impact on natriuretic peptide levels. They also proved that MR-proANP, NT-proBNP, and BNP are good, comparable markers of the severity of left ventricular systolic dysfunction.20 Yasue et al.21 also provided evidence that secretion of ANP and BNP from the left ventricle depends on the severity of left ventricular dysfunction, making ANP and BNP useful markers of the degree of left ventricular dysfunction in patients with HF.
Acute HF
Acute HF (AHF) is a life-threatening medical condition requiring urgent evaluation and treatment and typically leading to urgent hospital admission. This term includes de novo AHF, which occurs in patients who are presenting with symptoms for the first time, and acute decompensation of chronic HF, which indicates worsening of the symptoms of HF.11
The initial diagnosis of AHF should be based on an interview (symptoms, prior cardiovascular history, and potential cardiac and noncardiac precipitants) and physical examination (signs of congestion or hypoperfusion) and confirmed by appropriate additional investigations such as chest radiographs, electrocardiography, laboratory tests (with specific biomarkers), and echocardiography.14
In patients presenting with AHF, early initiation of appropriate therapy is of utmost importance.
Like BNP and NT-proBNP, MR-proANP is prognostic for adverse outcomes in patients with acutely decompensated HF. The investigators of the GISSI-HF study proved the prognostic value of MR-proANP for mortality (area under the receiver operating characteristic curve, 0.74; optimal cutoff point, 278 pmol/L).22 In the PRIDE study, an elevated MR-proANP level was prognostic and reclassified the mortality risk at 1 and 4 years.23
Because of the high sensitivity of natriuretic peptides, their levels should be measured in all patients with acute dyspnea and suspected AHF to help differentiate AHF from noncardiac causes of acute dyspnea. In the Biomarkers in Acute Heart Failure (BACH) trial, MR-proANP was measured in 1641 patients with acute dyspnea. The researchers found that MR-proANP (cutoff point of 120 pmol/L) was noninferior to BNP (cutoff point of 100 pg/mL) in the diagnosis of AHF and appeared to improve diagnostic accuracy in the BNP gray zone (BNP level of 100–500 pg/mL) and in obese patients.24 Potocki et al.25 suggested that the MR-proANP levels were significantly higher in patients with dyspnea and that the addition of this biomarker to clinical decision-making in the emergency department significantly improved the diagnostic accuracy of HF. Consistent with the BACH trial, they also found that MR-proANP provides incremental diagnostic information in patients presenting with BNP levels in the gray zone.25 Heining et al.26 also concluded that the MR-proANP level was significantly higher in patients with HF than in patients with other causes of dyspnea.
In contrast, Gegenhuber et al.27 compared MR-proANP levels with NT-proBNP and BNP levels in 251 patients with dyspnea. They suggested that the diagnostic information obtained by MR-proANP measurements was similar to that obtained by NT-proBNP measurements and that these peptides may be equally useful in the diagnosis of acute destabilized HF in patients with shortness of breath.
Stable coronary artery disease and acute coronary syndrome
Stable coronary artery disease occurs due to episodes of mismatch between myocardial oxygen demand and supply related to hypoxia or ischemia. These episodes are usually inducible by exercise or stress and lead to transient chest discomfort. Stable coronary artery disease also includes the stabilized and often asymptomatic phases that follow acute coronary syndrome.28
Natriuretic peptides may play an important role as diagnostic and prognostic tools in patients with coronary artery disease. MR-proANP provides more refined risk assessment than ANP and BNP. Ahluwalia et al.29 proved that MR-proANP was strongly associated with the risk of major cardiovascular events (such as nonfatal myocardial infarction, ischemic stroke, or death from cardiovascular disease) and together with BNP offered significant risk prediction compared with the traditional risk model.
The term acute myocardial infarction should be used when there is evidence of myocardial necrosis in a clinical setting consistent with acute myocardial ischemia. According to the third universal definition of myocardial infarction,30 myocardial injury is detected when blood levels of sensitive and specific biomarkers such as cardiac troponin or creatine kinase–myocardial band are increased. Cardiac troponin I and T are components of the contractile apparatus of myocardial cells and are expressed almost only in the heart.30 The preferred biomarker is cardiac troponin (I or T), which has high myocardial tissue specificity as well as high clinical sensitivity.30
Acute coronary syndrome carries a high risk of death and development of major cardiovascular events. Increasing numbers of emerging biomarkers have been suggested to help in the risk stratification of patients with acute coronary syndrome. Although little is known about their clinical value, such information may help to identify patients at high risk of major adverse cardiovascular events.
A few studies have suggested that measurement of MR-proANP is helpful in the risk stratification of patients with acute coronary syndrome. The LAMP study showed that MR-proANP is an important prognostic biomarker after the development of myocardial infarction independent of established conventional risk factors.31 The researchers proved that the clinical value of MR-proANP is equal to that of NT-proBNP for the prediction of death, but they did not perform a comparison with a novel, more sensitive troponin assay.31 In another study, von Haehling et al.32 theorized that MR-proANP can be used to identify high-risk patients because it may help in the prediction of all-cause mortality and major adverse cardiovascular events in patients presenting with symptomatic coronary artery disease.
Meune et al.33 recently evaluated the prognostic and diagnostic value of MR-proANP. They found that although it could not add diagnostic value to a sensitive troponin assay, it could improve the predictive power of the assay; an increased MR-proANP concentration was associated with an increased risk of death or acute myocardial infarction at 360 days independent of and in addition to cardiac troponin T, high-sensitivity cardiac troponin T, and the Thrombolysis In Myocardial Infarction risk score.33
Tzikas et al.34 reported that MR-proANP is a significant predictor of future cardiovascular events in patients with acute chest pain. Its predictive value was greater than that of troponin I, BNP (they proved that MR-proANP is more quickly released in the circulation than BNP with determination directly on admission), and clinical risk scoring systems such as the GRACE score.34
In another study, Moertl et al.20 determined that MR-proANP was inversely associated with the LVEF and outperformed BNP and NT-proBNP in the prediction of all-cause mortality and cardiovascular mortality. These results were confirmed in a study performed by Lindberg et al.35
Another group of researchers looked for correlations between the MR-proANP level and left ventricular function. They reported a strong association between impaired left ventricular function in patients with coronary artery disease and MR-proANP, indicating that MR-proANP is a good predictor of impaired left ventricular function.36
In contrast, Wang et al.37 found no association between plasma natriuretic peptides levels and the risk of coronary heart disease. This finding may have resulted from the characterization of the group involved in that study (ambulatory cohort).
Atrial fibrillation
Atrial fibrillation (AF) is a very common arrhythmia in the general population, especially in those of advanced age. Elevated concentrations of natriuretic peptides have been reported in patients with AF.38,39
Rossi et al.38 compared patients with AF to patients with sinus rhythm with similar clinical characteristics, left atrial overload, LVEF, and pulmonary pressure. They presented a theory that AF is independently associated with a higher N-terminal ANP N-ANP level and blurs the relationship between N-ANP and reduced left ventricular function. In contrast, they found that the BNP level is not independently affected by AF and is strongly associated with left ventricular dysfunction, for which it can be used as a marker in both patients with sinus rhythm and those with AF.38
Roy et al.40 proved that the plasma concentration of ANP in patients with chronic AF decreases after conversion to sinus rhythm. Mookherjee et al.39 confirmed that the ANP level is elevated in patients with AF regardless of the presence or absence of HF; they also proved that after successful cardioversion, the ANP level decreases independent of the mode of cardioversion or presence of HF.
Meune et al.41 measured the MR-proANP plasma concentration at presentation in consecutive patients with onset of AF but no evidence of AHF. They suggested that patients with an AF onset of <48 hours had lower MR-proANP concentrations than those with an AF onset of >48 hours and that the MR-proANP concentration may therefore reliably identify the time from onset of AF to presentation.41
In another study, the researchers measured the MR-proANP concentration in patients after radiofrequency ablation.42 They observed an increase in the MR-proANP level immediately after radiofrequency ablation, followed by a decrease the day after ablation (regardless of the actual rhythm). This finding indicates that radiofrequency ablation is a strong stimulus for the deliverance of MR-proANP.42
Hypertension
Hypertension is a disease of civilization. It affects 16% to 37% of the population globally. Although it usually does not cause symptoms, it is a major risk factor for coronary artery disease, stroke, HF, and AF.
The MR-proANP level rises in patients with hypertension. Sagnella et al.43 proved that the plasma MR-proANP level is significantly higher in patients with than without hypertension. This result was confirmed in studies performed by Kohno et al.44 and Hu et al.45 Hu et al.45 also proved that the MR-proANP level is associated with the severity of hypertension.
In contrast, Cappellin et al.46 proved that the MR-proANP level did not reliably predict the hypertensive condition. Nilsson et al.47 also found no correlation between the MR-proANP plasma concentration and blood pressure.
Irzmański et al.48 and Yasumoto et al.49 found a relationship among the plasma level of N-ANP, hypertension, and left ventricular hypertrophy. They proved that patients with hypertension and left ventricular hypertrophy have a significantly higher N-ANP level than do healthy patients.
Finally, Khaleghi et al.50 theorized that MR-proANP may be a marker of target organ damage in the setting of hypertension, especially in African-Americans.
Table 2 summarizes the role of MR-proANP in the cardiovascular system.
Table 2.
Roles of MR-proANP in cardiovascular system
| Diagnostic and prognostic marker in HF |
| Marker of the degree of left ventricular dysfunction in patients with HF |
| Prognostic factor for adverse outcomes in patients with acutely decompensated HF |
| Indicator of the risk of major cardiovascular events (such as nonfatal MI or death from CVD) |
| Indicator of the time from onset of atrial fibrillation to presentation |
| Marker of hypertension severity |
| Marker of target organ damage in the setting of hypertension |
MR-proANP, midregional pro-atrial natriuretic peptide; HF, heart failure; MI, myocardial infarction; CVD, cardiovascular disease.
MR-proANP in noncardiac disorders
Acute ischemic stroke
Stroke is the third leading cause of death and the primary cause of long-term disability worldwide. Estrada et al.2 found that the ANP level was higher in the acute phase of ischemic stroke than in healthy controls. Makikallio et al.3 compared the ANP level between patients with ischemic stroke and healthy controls and reported higher levels in patients with stroke. The researchers also showed that higher ANP levels were present in patients who died than survived, indicating that ANP may be a good predictor of mortality in patients with stroke.3
Katan et al.4 showed that the MR-proANP level on admission was increased in patients with stroke and confirmed that MR-proANP is a valuable prognostic marker in patients with ischemic stroke (independent of other comorbidities such as chronic HF, AF, and age).
MR-proANP in other disorders
Chronic kidney disease is a major health problem with an increasing incidence and prevalence. Natriuretic peptides are involved in renal homeostasis; therefore, MR-proANP may be a promising candidate peptide for the prognosis of chronic kidney disease. Dieplinger et al.9 investigated the prognostic value of MR-proANP for renal progression in patients with primary nondiabetic chronic kidney disease. They showed that an increased MR-proANP plasma concentration at baseline was a strong predictor of their renal end point, namely doubling of the baseline serum creatinine level. They also observed a continuous increase in the MR-proANP plasma concentration across glomerular filtration rate stages, indicating an association with disease severity.9 Ogawa et al.10 confirmed that the ANP level was higher in patients with chronic renal failure in proportion to volume status.
Type 2 diabetes mellitus is one of the most prevalent metabolic diseases worldwide. Although natriuretic peptides mediate various cardiovascular and metabolic effects, their role in diabetes is not fully understood.5 Previous data support the hypothesis that a low ANP level increases the risk of developing insulin resistance and type 2 diabetes.6 Magnusson et al.7 also suggested that there may be an association between serum natriuretic peptide levels and the risk of developing diabetes. Jujić et al.8 described the role of the ANP system in the etiology of type 2 diabetes. Still, more studies are needed to prove the role of ANP in the development of diabetes.
Obesity is a leading preventable cause of death worldwide, with increasing rates in adults and children. In 2014, 600 million adults (13%) and 42 million children under the age of 5 years were obese.51 Obesity is more common in women than men.51 Authorities view it as one of the most serious public health problems of the 21st century. In 2013, the American Medical Association classified obesity as a disease.51 Obesity is associated with decreased circulating levels of ANP and a negative linear relationship between body mass index and natriuretic peptide plasma concentrations.52
Conclusion
The herein-described studies of the multiple functions of MR-proANP prove its important role in different physiological and pathological pathways. These studies provide valuable data about the role of ANP in the pathogenesis, diagnostic process, prognosis, and potential therapeutic strategies of various diseases. Although ANP is mainly associated with cardiovascular diseases, it may be used as a biomarker in diabetology, neurology, and metabolic disorders. We anticipate that new studies will be carried out in the future and that MR-proANP will become a reliable prognostic and diagnostic factor, especially in cardiovascular disease.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med 1988; 339: 321–328. [DOI] [PubMed] [Google Scholar]
- 2.Estrada V, Tellez M, Moya J, et al. High plasma levels of endothelin-1 and atrial natriuretic peptide in patients with acute ischemic stroke. Am J Hypertens 1994; 7: 1085–1089. [DOI] [PubMed] [Google Scholar]
- 3.Makikallio AM, Mäkikallio TH, Korpelainen JTet al. Natriuretic peptides and mortality after stroke. Stroke 2005; 36: 1016–1020. [DOI] [PubMed] [Google Scholar]
- 4.Katan M, Fluri F, Schuetz P, et al. Midregional pro-atrial natriuretic peptide and outcome in patients with acute ischemic stroke. J Am Coll Cardiol 2010; 56: 1045–1053. [DOI] [PubMed] [Google Scholar]
- 5.Berezin AE. Cardiac biomarkers in diabetes mellitus: new dawn for risk stratification? Diabetes Metab Syndr 2017; 11(Suppl 1): S201–S208: 10.2016/j.dsx.2016.12.032 [DOI] [PubMed] [Google Scholar]
- 6.Feng Y, Wang D, Bi Het al. The role of natriuretic peptides in diabetes and its complications. Biomed Pharmacother 2016; 84: 1826–1832. [DOI] [PubMed] [Google Scholar]
- 7.Magnusson M, Jujic A, Hedblad Bet al. Low plasma level of atrial natriuretic peptide predicts development of diabetes: the prospective Malmo diet and cancer study. J Clin Endocrinol Metab 2012; 97: 638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jujic A, Nilsson PM, Engström Get al. Atrial natriuretic peptide and type 2 diabetes development – biomarker and genotype association study. Plos One 2014; 9: e89201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dieplinger B, Mueller T, Kollerits B, et al. Pro-A-type natriuretic peptide and pro-adrenomedullin predict progression of chronic kidney disease: the MMKD Study. Kidney Int 2009; 75: 408–414. [DOI] [PubMed] [Google Scholar]
- 10.Ogawa K, Smith AI, Hodsman GPet al. Plasma atrial natriuretic peptide: concentrations and circulating forms in normal man and patients with chronic renal failure. Clin Exp Pharmacol Physiol 1987; 14: 95–102. [DOI] [PubMed] [Google Scholar]
- 11.Morgenthaler NG, Struck J, Thomas Bet al. Immunoluminometric assay for the midregion of pro-atrial natriuretic peptide in human plasma. Clin Chem 2004; 50: 234–236. [DOI] [PubMed] [Google Scholar]
- 12.de Bold AJ, Borenstein HB, Veress AT, et al. A rapid and potent natriuretic response to intravenous injection of atrial myocardial extract in rats. Life Sci 1981; 28: 89–94. [DOI] [PubMed] [Google Scholar]
- 13.Volpe M, Carnovali M, Mastromarino V. The natriuretic peptides system in the pathophysiology of heart failure: from molecular basis to treatment. Clin Sci 2015; 130: 57–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 15.Sakurai S, Adachi H, Hasegawa Aet al. Brain natriuretic peptide facilitates severity classification of stable chronic heart failure with left ventricular dysfunction. Heart 2003; 89: 661–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doust JA, Pietrzak E, Dobson Aet al. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. BMJ 2005; 330: 625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoshibayashi M, Saito Y, Nakao K. Brain natriuretic peptide versus atrial natriuretic peptide – physiological and pathophysiological significance in children and adults: a review. Eur J Endocrinol 1996; 135: 265–268. [DOI] [PubMed] [Google Scholar]
- 18.Eggers KM, Venge P, Lind L. Mid-regional pro-atrial natriuretic peptide levels in the elderly: Clinical and prognostic implications, and comparison to B-type natriuretic peptides. Clin Chim Acta 2013; 419: 62–66. [DOI] [PubMed] [Google Scholar]
- 19.von Haehling S, Jankowska EA, Morgenthaler NGet al. Comparison of midregional pro-atrial natriuretic peptide with n-terminal pro-B-type natriuretic peptide in predicting survival in patients with chronic heart failure. J Am Coll Cardiol 2007; 50: 1973–1980. [DOI] [PubMed] [Google Scholar]
- 20.Moertl D, Berger R, Struck Jet al. Comparison of midregional pro-atrial and B-type natriuretic peptides in chronic heart failure. J Am Coll Cardiol 2009; 53: 1783–1790. [DOI] [PubMed] [Google Scholar]
- 21.Yasue H, Yoshimura M, Sumida Het al. Localization and mechanism of secretion of B-type natriuretic peptide in comparison with those of A-type natriuretic peptide in normal subjects and patients with heart failure. Circulation 1994; 90: 195–203. [DOI] [PubMed] [Google Scholar]
- 22.Gaggin HK, Januzzi JL., Jr Biomarkers and diagnostics in heart failure. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 2013; 1832: 2442–2450. [DOI] [PubMed] [Google Scholar]
- 23.Shah RV, Truong QA, Gaggin HK, et al. Mid-regional pro-atrial natriuretic peptide and pro-adrenomedullin testing for the diagnostic and prognostic evaluation of patients with acute dyspnea. Eur Heart J 2012; 33: 2197–2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maisel A, Mueller C, Nowak R, et al. Mid-region pro-hormone markers for diagnosis and prognosis in acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial . J Am Coll Cardiol 2010; 55: 2062–2076. [DOI] [PubMed] [Google Scholar]
- 25.Potocki M, Breidthardt T, Reichlin T. Comparison of midregional pro-atrial natriuretic peptide with N-terminal pro-B-type natriuretic peptide in the diagnosis of heart failure. J Intern Med 2010; 267: 119–129. [DOI] [PubMed] [Google Scholar]
- 26.Heining L, Giesa C, Ewig S. MR-proANP, MR-proADM and PCT in patients presenting with acute dyspnea in a medical emergency unit. Lung 2016; 194: 185–191. [DOI] [PubMed] [Google Scholar]
- 27.Gegenhuber A, Struck J, Poelz W. Midregional pro-A-type natriuretic peptide measurements for diagnosis of acute destabilized heart failure in short-of-breath patients: comparison with B-type natriuretic peptide and amino-terminal proBNP. Clin Chem 2006; 52: 827–831. [DOI] [PubMed] [Google Scholar]
- 28.Task Force Members, Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013; 34: 2949–3003. [DOI] [PubMed] [Google Scholar]
- 29.Ahluwalia N, Blacher J, Szabo de Edelenyi Fet al. Prognostic value of multiple emerging biomarkers in cardiovascular risk prediction in patients with stable cardiovascular disease. Atherosclerosis 2013; 228: 478–484. [DOI] [PubMed] [Google Scholar]
- 30.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Glob Heart 2102; 7: 275–295. [DOI] [PubMed] [Google Scholar]
- 31.Khan SQ, Dhillon O, Kelly D, et al. Plasma N-terminal B-type natriuretic peptide as an indicator of long-term survival after acute myocardial infarction: comparison with plasma midregional pro-atrial natriuretic peptide; the LAMP (Leicester Acute Myocardial Infarction Peptide) Study. J Am Coll Cardiol 2008; 51: 1857–1864. [DOI] [PubMed] [Google Scholar]
- 32.von Haehling S, Papassotiriou J, Hartmann Oet al. Mid-regional pro-atrial natriuretic peptide as a prognostic marker for all-cause mortality in patients with symptomatic coronary artery disease. Clin Sci (Lond) 2012; 123: 601–610. [DOI] [PubMed] [Google Scholar]
- 33.Meune C, Twerenbold R, Drexler B. Midregional pro-A-type natriuretic peptide for diagnosis and prognosis in patients with suspected acute myocardial infarction. Am J Cardiol 2012; 109: 1117–1123. [DOI] [PubMed] [Google Scholar]
- 34.Tzikas S, Keller T, Ojeda FMet al. MR-proANP and MR-proADM for risk stratification of patients with acute chest pain. Heart 2013; 99: 388–395. [DOI] [PubMed] [Google Scholar]
- 35.Lindberg S, Jensen J, Pedersen S. MR-proANP improves prediction of mortality and cardiovascular events in patients with STEMI. Eur J Prev Cardiol 2015; 22: 693–700. [DOI] [PubMed] [Google Scholar]
- 36.Elmas E, Brueckmann M, Lang Set al. Midregional pro-atrial natriuretic peptide is a useful indicator for the detection of impaired left ventricular function in patients with coronary artery disease. Int J Cardiol 2008; 128: 244–249. [DOI] [PubMed] [Google Scholar]
- 37.Wang TJ, Larson MG, Levy Det al. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med 2004; 350: 655–663. [DOI] [PubMed] [Google Scholar]
- 38.Rossi A, Enriquez-Sarano M, Burnett JC, Jret al. Natriuretic peptide levels in atrial fibrillation: a prospective hormonal and Doppler-echocardiographic study. J Am Coll Cardiol 2000; 35: 1256–1262. [DOI] [PubMed] [Google Scholar]
- 39.Mookherjee S, Anderson G, Jr, Smulyan Het al. Atrial natriuretic peptide response to cardioversion of atrial flutter and fibrillation and role of associated heart failure. Am J Cardiol 1991; 67: 377–380. [DOI] [PubMed] [Google Scholar]
- 40.Roy D, Paillard F, Cassidy Det al. Atrial natriuretic factor during atrial fibrillation and supraventricular tachycardia. J Am Coll Cardiol 1987; 9: 509–514. [DOI] [PubMed] [Google Scholar]
- 41.Meune C, Vermillet A, Wahbi K, et al. Mid-regional pro atrial natriuretic peptide allows the accurate identification of patients with atrial fibrillation of short time of onset: a pilot study. Clin Biochem 2011; 44: 1315–1319. [DOI] [PubMed] [Google Scholar]
- 42.Charitakis E, Walfridsson H, Alehagen U. Short-term influence of radiofrequency ablation on NT-proBNP, MR-proANP, Copeptin and MR-proADM in patients with atrial fibrillation: data from the observational SMURF study. J Am Heart Assoc 2016; 5: e003557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sagnella GA, Markandu ND, Shore AC, et al. Raised circulating levels of atrial natriuretic peptides in essential hypertension. Lancet 1986; 1: 179–181. [DOI] [PubMed] [Google Scholar]
- 44.Kohno M, Yasunari K, Matsuura T, et al. Circulating atrial natriuretic polypeptide in essential hypertension. Am Heart J 1987; 113: 1160–1163. [DOI] [PubMed] [Google Scholar]
- 45.Hu W, Zhou PH, Zhang XB., et al. Plasma concentrations of adrenomedullin and natriuretic peptides in patients with essential hypertension. Exp Ther Med 2015; 9: 1901–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cappellin E, Gatti R, Antonelli G, et al. Natriuretic peptide fragment as possible biochemical markers of hypertension in the elderly. J Cardiovasc Med (Hagerstown) 2013; 14: 308–313. [DOI] [PubMed] [Google Scholar]
- 47.Nilsson P, Lindholm L, Scherstén B, et al. Atrial natriuretic peptide and blood pressure in a geographically defined population. Lancet 1987; 2: 883–885. [DOI] [PubMed] [Google Scholar]
- 48.Irzmański R, Pawlicki L, Charłusz M, et al. Concentration of natriuretic peptides in patients suffering from idiopathic arterial hypertension and left ventricular diastolic dysfunction confirmed by echocardiography. Clin Exp Hypertens 2012; 34: 530–540. [DOI] [PubMed] [Google Scholar]
- 49.Yasumoto K, Takata M, Ueno H, et al. Relation of plasma brain and atrial natriuretic peptides to left ventricular geometric patterns in essential hypertension. Am J Hypertens 1999; 12(9 Pt 1): 921–924. [DOI] [PubMed] [Google Scholar]
- 50.Khaleghi M, Al-Omari MA, Kondragunta V, et al. Relation of plasma midregional proatrial natriuretic peptide to target organ damage in adults with systemic hypertension. Am J Cardiol 2009; 103: 1255–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization. Obesity and Overweight. Fact Sheet N°311. Updated January 2015. Retrieved 2 February 2016.
- 52.Wang TJ, Larson MG, Levy Det al. Impact of obesity on plasma natriuretic peptide levels. Circulation 2004; 109: 594–600. [DOI] [PubMed] [Google Scholar]