Short abstract
Objective
We assessed our results of short-segment decompression and fixation for osteoporotic thoracolumbar fractures with neurological deficits.
Methods
We evaluated 20 elderly patients (age, 60–89 years; mean, 73.2 years) with osteoporotic thoracolumbar fractures and neurological deficits. They underwent short-segment decompression and fixation and followed up for 40.6 (range, 24–68) months. A visual analog scale (VAS) and the Oswestry Disability Index (ODI) were used to measure back pain and disability. We also analyzed patients’ radiologic findings and neurological status. Perioperative and postoperative complications were recorded.
Results
At the latest follow-up, the average VAS score for back pain and ODI scores had significantly improved. The radiologic assessment showed significant improvements in local kyphosis, anterior vertebral height, and the vertebral wedge angle compared with the original measures. Neurological function also improved in 18 of 20 patients. No major complications occurred perioperatively. Our techniques included preservation of the posterior ligament complex, decortication of facet joints for fusion, no tapping to increase the screw insertional torque, pre-contouring of the rods according to the “adaptive” curve obtained from postural reduction, and postoperative spinal bracing.
Conclusions
Posterior short-segment decompression and fixation could be an effective surgical option for osteoporotic thoracolumbar burst fractures with neurological deficits.
Keywords: Vertebral osteoporotic fracture, neurological deficits, posterior surgery, short-segment, postural reduction, aging population
Introduction
Thoracolumbar fractures frequently develop after low-energy trauma in the aged population because of osteoporosis.1 However, the optimal treatment for such injuries often depends on the individual’s condition and remains inconclusive.2–8 In the aged spine, the retropulsed bone fragments may cause canal compromise because of coexisting stenosis. Thus, surgical intervention is sometimes required to obtain neural canal decompression for the neurological deficits following osteoporotic vertebral collapse.
For unstable fractures, posterior long-segment fixation provides a more stable construct, but the procedure may increase perioperative morbidities in older patients with comorbidities. Thus, short-segment fixation might be an alternative surgical option in this population. The results of short-segment instrumentation are reportedly satisfactory, but the study populations were young.9–12 Treating fragile fractures is more challenging. Only a few reports have described short-segment fixation for osteoporotic vertebral fractures.13–16
Because the aging population is increasing, it seems important to critically discuss the potential application of short-segment reconstruction for osteoporotic thoracolumbar fractures. The purpose of this study was to describe our technical modifications and outcomes of short-segment decompression and reconstruction for osteoporotic thoracolumbar fractures with neurological compromise.
Patients and methods
This was a retrospective clinical review of prospectively collected data in a single institute. The study protocol was approved by the ethic review board of National Cheng Kung University Hospital. Written informed consent was obtained from all patients. Consecutive patients with an osteoporotic fracture at a single level of the thoracolumbar region participated in this study. All patients had neurological deficits following the fracture. The bone mineral density (BMD) of the vertebrae was measured using dual-energy X-ray absorptiometry, and a T-score of less than −2.5 from the lumbar spine was set as the criterion for osteoporosis.
Patients were treated with posterior short-segment decompression and reconstruction at the fracture level. The surgical indication was an unstable thoracolumbar fracture and neurological compromise, such as lower limb numbness, weakness, paraplegia, or cauda equina syndrome. The unstable fractures included two- or three-column injury according to the Denis three-column concept17 and fractures with an intervertebral cleft. All patients had sustained only mild injuries, including injury following a slip, standing, or bending. We excluded patients with translational displacement at the fracture site (fracture–dislocation), loss of structural integrity within the posterior osteoligamentous complex (such as flexion–distraction ligament disruption) in preoperative images, spondylolisthesis of the adjacent vertebrae, malignancy, chronic steroid administration, previous spinal surgery, prior vertebroplasty, and infection.
Surgical techniques
Following general endotracheal tube intubation, postural reduction of the segmental kyphosis was achieved by placing the patient in a prone, hyperextended position on a four-poster spinal frame. The spontaneous reduction by ligamentotaxis was then confirmed with an image intensifier. Using the standard posterior midline approach, decompression with bilateral laminotomy was performed at the collapsed vertebrae. The midline structures (spinous process and supraspinous and interspinous ligaments) were preserved intact. We removed the ligamentum flavum, trimmed the lamina to release the nerve root, and impacted the retropulsed fragment into the vertebral body. The superior and inferior articular facet joints of the fractured vertebrae were decorticated for fusion. Polyaxial pedicle screws were then inserted without tapping to increase the insertional torque into the vertebrae just above and below the fractured vertebrae (Figure 1). The rods were contoured according to the segmental kyphosis or lordosis obtained from the image intensifier, the shape of which was equal to the spinal alignment after postural reduction with achievement of a smooth curve. No further distraction or other reduction methods were used. During tightening, no rods gave way, which would have jeopardized vertebral anchoring, especially for osteoporotic bones.
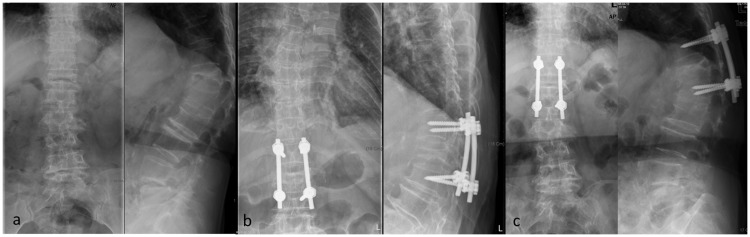
Figure 1.
Posterior short-segment reconstruction: instrumentation at one level above and one level below the fractured vertebra with posterolateral fusion. (a) Preoperatively. (b) Postoperatively. (c) Two years postoperatively.
Tricortical iliac autografts, allografts, or hybrids were used for posterolateral and facet joint fusion. No vertebroplasty was performed in this series. All patients were allowed to ambulate with a thoracolumbar orthosis on the third postoperative day, with muscle strengthening exercises beginning 2 weeks later. We recommended removal of the thoracolumbar orthosis after 3 months.
Outcomes
We carefully reviewed the charts, operative notes, preoperative and postoperative radiographs, and follow-up records of all patients from the time of surgery until the final follow-up assessment. Data were collected according to the following measures: back pain intensity was recorded using a 10-point visual analog scale, the functional outcome after surgery was evaluated using the Oswestry Disability Index, and, Frankel’s grading system was used to assess neurologic improvement. In addition, perioperative and postoperative complications were recorded during follow-up.
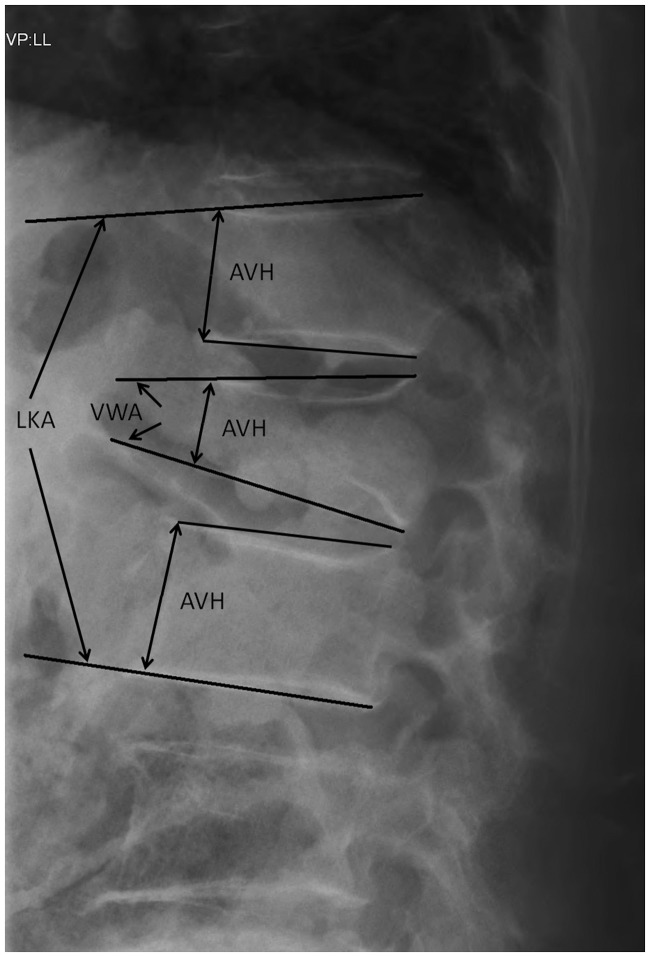
All radiographs were taken in the sitting position. Digital radiographs of the vertebral bodies were reviewed using a picture archiving and communication system. The local kyphotic angle (LKA) was measured from the superior endplate of the intact vertebrae cephalad to the fracture and the inferior endplate of the intact vertebrae caudad to the fracture. The anterior vertebral height (AVH) ratio (% of normal) was also recorded, for which the normal AVH was obtained by averaging the AVHs of the nonfractured vertebrae above and below the fractured vertebral body. The vertebral wedge angle (VWA) before and after surgery was measured from the superior and inferior endplate of the fractured vertebrae (Figure 2).
Figure 2.
LKA: local kyphotic angle, AVH: anterior vertebral height, VWA: vertebral wedge angle.
Statistical analysis
Observers independent of the principal surgeon performed the radiographic and clinical assessments. Wilcoxon’s signed-rank test was used to statistically evaluate changes in the parameters, with a p-value of <0.05 indicating significance. Statistical analyses were performed with SPSS 15.0 software for Windows (SPSS, Inc., Chicago, IL, USA).
Results
Twenty-two patients were included in this study. Table 1 summarizes the patients’ demographic data. Twenty patients were available for follow-up for an average of 40.6 months (range, 24–68 months) after surgical treatment, while two patients died of comorbidities within the initial 6 months after the operation. The mean age of the patients was 73.2 years. The fractures were located from T10 to L5. The mean T-score was −3.38 ± 0.47 as measured by dual-energy X-ray absorptiometry.
Table 1.
Demographic data
| Sex, female/male | 15/5 |
|---|---|
| Mean age, years | 73.2 ± 10.7 (range, 60–89) |
| Fracture level | T10: 1, T12: 6, L1: 4, L2: 2, L3: 1, L4: 5, L5: 1 |
| Presenting Frankel grade | D: 7, C: 11, B: 2 |
| Bone mineral density | −3.38 ± 0.47 |
Data are presented as n or mean ± standard deviation.
The mean operative time was 143.2 minutes (range, 100–198 minutes), and the mean blood loss volume was roughly 252.9 ml (range, 180–650 ml); blood transfusion was required in only two patients (10%). The hospital stay ranged from 6 to 14 days (mean, 9.7 days).
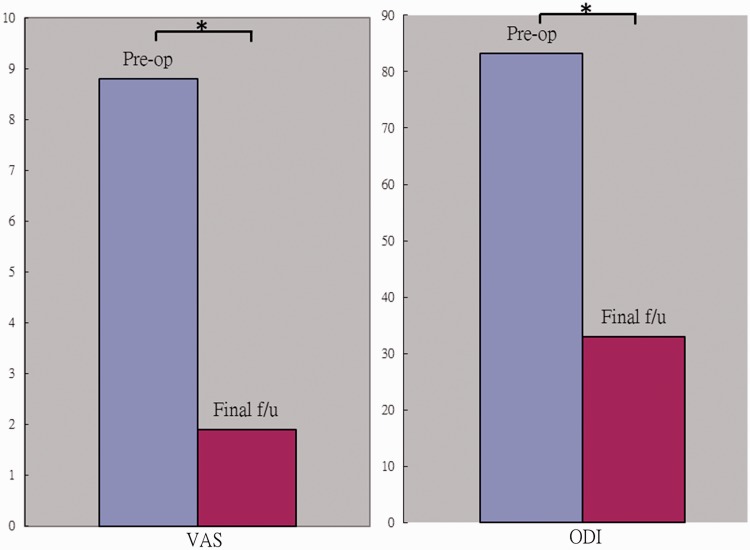
At the time of the last follow-up, the average visual analog scale score for back pain had improved from 8.8 ± 1.9 (range, 4–10) to 1.9 ± 1.7 (range, 0–5) (p < 0.05), and the Oswestry Disability Index scores had also improved in all 20 patients from 83.2% ± 12.0% preoperatively to 33.0% ± 20.1% at the last follow-up (p < 0.05) (Figure 3). Improvements were most pronounced in back pain, sitting endurance, standing endurance, and living independence. At the time of the last follow-up, neurological improvement of one or more Frankel grades was seen in 18 of the 20 patients; the other 2 patients had an unchanged Frankel grade (Table 2). Moreover, most patients (90%) were subjectively satisfied with the surgery.
Figure 3.
The last visual analog scale score for back pain and the Oswestry Disability Index scores improved significantly compared with the preoperative scores. *p < 0.05. Pre-op: preoperatively, f/u: follow-up, VAS: visual analog scale, ODI: Oswestry Disability Index.
Table 2.
Neurological function
| Frankel grade | Preoperative | Final follow-up |
|---|---|---|
| D | 7 | 6E, 1D |
| C | 11 | 5E, 6D |
| B | 2 | 1C, 1B |
The average LKA, representing sagittal alignment, improved from 14.2° ± 19.9° before surgery to 4.0° ± 19.3° after surgery (p < 0.05). At the last follow-up, the average loss of kyphosis correction was 2.9°, representing a statistically significant 7.3° improvement in the LKA (p < 0.05) (Table 3).
Table 3.
Summary of radiographic data preoperatively, postoperatively, and at the latest follow-up
| Radiograph | Mean | SD | Min. | Max. |
|---|---|---|---|---|
| Local kyphosis (o) | ||||
| Preoperative | 14.2 | 19.9 | −20.8 | 39.2 |
| Postoperative | 4.0 | 19.3 | −28.4 | 33.2 |
| Follow-up | 6.9 | 18.9 | −26.5 | 34.8 |
| Anterior body height (%) | ||||
| Preoperative | 46.1 | 14.6 | 17.5 | 77.0 |
| Postoperative | 63.3 | 18.4 | 20.2 | 91.7 |
| Follow-up | 57.4 | 17.6 | 17.2 | 88.2 |
| Vertebral wedge angle (o) | ||||
| Preoperative | 18.4 | 7.6 | 13.6 | 43.6 |
| Postoperative | 10.8 | 6.5 | 11.1 | 37.0 |
| Follow-up | 12.7 | 6.7 | 12.0 | 38.6 |
SD: standard deviation, Min.: minimum, Max.: maximum
Negative numbers represent lordosis and positive numbers represent kyphosis.
Measurements of the AVH ratio (% of normal) and VWA reflected the anatomical shape of the fractured vertebrae. The mean preoperative AVH ratio and VWA were 46.1% ± 14.6% and 18.4° ± 7.6°, respectively, and improved to 63.3% ± 18.4% and 10.8° ± 6.5° after surgery (p < 0.05). At the final follow-up, statistically significant corrections were observed in the AVH ratio (11.3%) and VWA (5.7°) (p < 0.05), as shown in Table 3.
Complications
As shown in Table 4, major complications were noted during the perioperative period; however, wound dehiscence with superficial infection developed in one patient and responded to antibiotic treatment. No late or deep infection developed in this series.
Table 4.
Complications
| Complications | n |
|---|---|
| Early | |
| Wound dehiscence with superficial infection | 1 |
| Late | |
| Hardware failure | |
| Broken screws | 1 |
| Implant irritation | 1 |
| Adjacent segment degeneration | 3 |
Although one case of implant failure due to a broken screw was noted at the 4-year follow-up, no further treatment was needed because no back pain or further deformity had occurred in this patient. In contrast, the instrumentation had to be removed in one patient after solid fusion because of hardware prominence and discomfort.
Furthermore, three patients developed adjacent segment degeneration (ASD); two were distal and one was proximal to the fusion level. Two of the patients underwent further surgery because of intractable pain, and one chose conservative management in the pain clinic.
Discussion
This study was performed to report the effects of short-segment decompression and reconstruction for treatment of osteoporotic burst fractures in the aging population. The results demonstrated satisfactory clinical application of this method in selected patients who can tolerate postoperative bracing. Moreover, effective pain control and improved outcomes were obtained in our series.
Vertebral body collapse, kyphosis, persistent back pain, or disability might occur after vertebral fractures if not treated adequately.18,19 Though the management of thoracolumbar fracture remains a matter of discussion,20 many surgeons advocate surgical treatment, especially for unstable fractures or neurologically compromised patients.18,19,21 Surgical procedures have included decompression, anterior or posterior fixation, or both, with or without fusion.2,3,6,11,22,23 Nevertheless, how to improve surgery for vertebral fractures combined with osteoporosis in aged patients remains obscure. Some challenges should be taken into consideration, including fragile vertebrae, age, medical comorbidities, and possible perioperative morbidities.
The anterior route provides direct access for neural decompression24; however, associated visceral and vascular injuries have been reported in the literature.25,26 The posterior approach is a well-established procedure with which most spine surgeons are familiar; thus, we believe that posterior surgery with short-segment fixation is safer for patients with high surgical risk. Although spinal canal decompression can be achieved by ligamentotaxis in posterior surgery, some retropulsed fragments may remain. Further, it also increases the risk of spinal canal compromise because of the possible coexisting spinal stenosis commonly seen in older patients. We therefore impacted the retropulsed fragments into the posterior wall of the vertebral body to achieve circumferential decompression. Our outcomes were primarily positive, with most (18/20) of our patients showing improvement in their neurological symptoms.
Although long-segment posterior fixation provides superior rigid fixation, this method may be associated with great physiological challenges and perioperative morbidities in elderly patients. Because of the improved rigidity and stiffness of pedicle screw-based posterior spinal instrumentation systems, short-segment reconstruction has become more reliable. Some authors have reported success with short-segment instrumentation in treating thoracolumbar burst fractures10,11,27,28; however, the study populations in these studies were young patients with relatively good bone quality. Our series showed significant pain control, functional improvements, and acceptable deformity correction in the osteoporotic spine. We attributed these improvements to our technique modifications: preservation of the posterior ligament complex, facet joint decortication for fusion, no tapping to increase the screw insertional torque, short-segment instrumentation with an “adaptive” curve, and postoperative spinal bracing for 3 months.
In an in vitro biomechanical study, Tai et al.29 reported no difference in intervertebral displacement between the intact and bilateral laminotomy groups under flexion motion. Gillespie and Dickey30 observed similar findings and suggested that the supraspinous/interspinous ligament complex is the largest contributor to resistance of applied flexion moments in the porcine lumbar spine. These results indicate that the posterior spinal ligaments play an important role in segmental stability if they remain intact. In our series, we excluded patients without an intact posterior osteoligamentous complex; furthermore, the midline structures (spinous process and supraspinous and interspinous ligaments) were preserved during decompression. Therefore, the undamaged structures could provide additional stability after short-segment instrumentation.
Although the correction of sagittal alignment was only from the posture without a specific reduction maneuver, we defined the main surgical goals of this method as pain control and functional improvement instead of notable deformity correction in such an aged population. Moreover, we considered that the angle corrected by postural reduction was the “flexible angle,” which would not cause excessive stress on the instrumentation and potentially lead to hardware failure prior to osseous union. In actuality, the improvements observed in the radiological parameters (LKA, AVH ratio, and VWA) measured in the postoperative period and at the last follow-up were comparable with those in previous reports of short-segment fixation.10,14,27,31 Optimal sagittal alignment in elderly patients with osteoporosis is a matter of debate, and more long-term follow-up focusing on residual kyphosis is necessary.
In the long-term follow-up, three patients developed symptomatic ASD and two needed reoperations. Because of the increased stress and mobility of the adjacent segments, posterior surgery has been blamed for causing ASD as a late complication. Although our understanding of the fate of the transitional segments after spinal fusion remains inconclusive, some reports have suggested that the occurrence of ASD is related to the length of the fusion and the age of the patients.32–34 Long-segment fusion might exert excessive load and motion to the adjacent segments. Therefore, we speculated that more ASD might have occurred if long-segment fixation had been used in a population of such advanced age.
The main limitation of this study is the small number of patients. However, few surgical cases with osteoporotic thoracolumbar fractures and neurological deficits are available for review. Additionally, no comparison group was available in this study. Nevertheless, the clinical efficacy in the present study was comparable with that of previous clinical studies of other surgical techniques.10,11,27,31,35 Controlled randomized studies with larger samples are necessary to clarify the role of short-segment reconstruction in the treatment of osteoporotic burst fractures. We excluded patients with fracture–dislocation, spondylolisthesis of the adjacent vertebrae, and posterior ligament disruption and selected only patients with minor trauma mechanisms. Consequently, this method may not be appropriate to all osteoporotic burst fractures.
Conclusion
In conclusion, short-segment decompression and fixation was effective for vertebral osteoporotic fractures with neurological deficits. It could be an alternative surgical option for compromised and osteoporotic thoracolumbar fractures in selected patients with low-energy injuries.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
The study protocol was approved by the ethic review board of National Cheng Kung University Hospital.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by grants from the Ministry of Science and Technology of Taiwan (MOST 103-2314-B-006-085-MY2, MOST 103-2218-E-006-029).
References
- 1.Arciero RA, Leung KY, Pierce JH. Spontaneous unstable burst fracture of the thoracolumbar spine in osteoporosis. A report of two cases. Spine (Phila Pa 1976) 1989; 14: 114–117. [DOI] [PubMed] [Google Scholar]
- 2.Kaneda K, Taneichi H, Abumi K, et al. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am 1997; 79: 69–83. [DOI] [PubMed] [Google Scholar]
- 3.Katonis PG, Kontakis GM, Loupasis GA, et al. Treatment of unstable thoracolumbar and lumbar spine injuries using Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976) 1999; 24: 2352–2357. [DOI] [PubMed] [Google Scholar]
- 4.Sasso RC, Renkens K, Hanson D, et al. Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech 2006; 19: 242–248. [DOI] [PubMed] [Google Scholar]
- 5.Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech 2005; 18: 485–488. [DOI] [PubMed] [Google Scholar]
- 6.Uchida K, Kobayashi S, Matsuzaki M, et al. Anterior versus posterior surgery for osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine. Eur Spine J 2006; 15: 1759–1767. [DOI] [PubMed] [Google Scholar]
- 7.Wood K, Buttermann G, Mehbod A, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am 2003; 85-A: 773–781. [DOI] [PubMed] [Google Scholar]
- 8.Bakhsheshian J, Dahdaleh NS, Fakurnejad S, et al. Evidence-based management of traumatic thoracolumbar burst fractures: a systematic review of nonoperative management. Neurosurg Focus 2014; 37: E1. [DOI] [PubMed] [Google Scholar]
- 9.Altay M, Ozkurt B, Aktekin CN, et al. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J 2007; 16: 1145–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butt MF, Farooq M, Mir B, et al. Management of unstable thoracolumbar spinal injuries by posterior short segment spinal fixation. Int Orthop 2007; 31: 259–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. a five to seven-year prospective randomized study. J Bone Joint Surg Am 2009; 91: 1033–1041. [DOI] [PubMed] [Google Scholar]
- 12.Wang L, Li J, Wang H, et al. Posterior short segment pedicle screw fixation and TLIF for the treatment of unstable thoracolumbar/lumbar fracture. BMC Musculoskelet Disord 2014; 15: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakano A, Ryu C, Baba I, et al. Posterior short fusion without neural decompression using pedicle screws and spinous process plates: A simple and effective treatment for neurological deficits following osteoporotic vertebral collapse. J Orthop Sci 2017; 22: 622–629. [DOI] [PubMed] [Google Scholar]
- 14.Kashii M, Yamazaki R, Yamashita T, et al. Surgical treatment for osteoporotic vertebral collapse with neurological deficits: retrospective comparative study of three procedures–anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur Spine J 2013; 22: 1633–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sudo H, Ito M, Kaneda K, et al. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J 2013; 13: 1726–1732. [DOI] [PubMed] [Google Scholar]
- 16.Uchida K, Nakajima H, Yayama T, et al. Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: comparisons with posterior surgery without vertebroplasty and anterior surgery. J Neurosurg Spine 2010; 13: 612–621. [DOI] [PubMed] [Google Scholar]
- 17.Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res 1984; ▪: 65–76. [PubMed] [Google Scholar]
- 18.Dickson JH, Harrington PR, Erwin WD. Results of reduction and stabilization of the severely fractured thoracic and lumbar spine. J Bone Joint Surg Am 1978; 60: 799–805. [PubMed] [Google Scholar]
- 19.Jacobs RR, Asher MA, Snider RK. Thoracolumbar spinal injuries. A comparative study of recumbent and operative treatment in 100 patients. Spine (Phila Pa 1976) 1980; 5: 463–477. [PubMed] [Google Scholar]
- 20.Sheng X, Ren S. Surgical techniques for osteoporotic vertebral collapse with delayed neurological deficits: A systematic review. Int J Surg 2016; 33 Pt A: 42–48. [DOI] [PubMed] [Google Scholar]
- 21.Willen J, Lindahl S, Nordwall A. Unstable thoracolumbar fractures. A comparative clinical study of conservative treatment and Harrington instrumentation. Spine (Phila Pa 1976) 1985; 10: 111–122. [DOI] [PubMed] [Google Scholar]
- 22.Wang ST, Ma HL, Liu CL, et al. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?: a prospective, randomized study. Spine (Phila Pa 1976) 2006; 31: 2646–2652; discussion 53. [DOI] [PubMed] [Google Scholar]
- 23.Jindal N, Sankhala SS, Bachhal V. The role of fusion in the management of burst fractures of the thoracolumbar spine treated by short segment pedicle screw fixation: a prospective randomised trial . J Bone Joint Surg Br 2012; 94: 1101–1106. [DOI] [PubMed] [Google Scholar]
- 24.D'Aliberti G, Talamonti G, Villa F, et al. Anterior approach to thoracic and lumbar spine lesions: results in 145 consecutive cases. J Neurosurg Spine 2008; 9: 466–482. [DOI] [PubMed] [Google Scholar]
- 25.Baker JK, Reardon PR, Reardon MJ, et al. Vascular injury in anterior lumbar surgery. Spine (Phila Pa 1976) 1993; 18: 2227–2230. [DOI] [PubMed] [Google Scholar]
- 26.Rajaraman V, Vingan R, Roth P, et al. Visceral and vascular complications resulting from anterior lumbar interbody fusion. J Neurosurg 1999; 91: 60–64. [DOI] [PubMed] [Google Scholar]
- 27.Parker JW, Lane JR, Karaikovic EE, et al. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976) 2000; 25: 1157–1170. [DOI] [PubMed] [Google Scholar]
- 28.Kanna RM, Shetty AP, Rajasekaran S. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J 2015; 15: 256–264. [DOI] [PubMed] [Google Scholar]
- 29.Tai CL, Hsieh PH, Chen WP, et al. Biomechanical comparison of lumbar spine instability between laminectomy and bilateral laminotomy for spinal stenosis syndrome - an experimental study in porcine model. BMC Musculoskelet Disord 2008; 9: 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gillespie KA, Dickey JP. Biomechanical role of lumbar spine ligaments in flexion and extension: determination using a parallel linkage robot and a porcine model. Spine (Phila Pa 1976) 2004; 29: 1208–1216. [DOI] [PubMed] [Google Scholar]
- 31.Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976) 1992; 17: S317–S324. [DOI] [PubMed] [Google Scholar]
- 32.Cheh G, Bridwell KH, Lenke LG, et al. Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976) 2007; 32: 2253–2257. [DOI] [PubMed] [Google Scholar]
- 33.Gillet P. The fate of the adjacent motion segments after lumbar fusion. J Spinal Disord Tech 2003; 16: 338–345. [DOI] [PubMed] [Google Scholar]
- 34.Nagata H, Schendel MJ, Transfeldt EE, Lewis JL. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976) 1993; 18: 2471–2479. [DOI] [PubMed] [Google Scholar]
- 35.Chen C, Lv G, Xu B, Zhang X, Ma X. Posterior short-segment instrumentation and limited segmental decompression supplemented with vertebroplasty with calcium sulphate and intermediate screws for thoracolumbar burst fractures. Eur Spine J 2014; 23: 1548–1557. [DOI] [PubMed] [Google Scholar]