Short abstract
Intussusception is common in children. Double simultaneous intussusception is a peculiar variety of intussusception with only 14 previously reported cases. We report a unique case of a child who suffered from double simultaneous intussusception with two lead points (Meckel’s diverticulum and intestinal duplication). The patient was successfully treated with manual reduction along with resection of Meckel’s diverticulum and intestinal duplication. The child recovered well.
Keywords: Double simultaneous intussusception, child, Meckel’s diverticulum, intestinal duplication, laparotomy, abdominal pain
Introduction
Intussusception is a common aetiology of acute abdominal pain in children. Intussusception occurs in children of all ages, with predominance in children aged younger than 2 years old.1–3 The most common intussusception is ileocolic intussusception, which accounts for approximately 98%. Double intussusception is rare. To date, only 14 cases of double intussusception (Table 1) have been reported.4–17 Occurrence of double simultaneous intussusception with two explicit leading points has not been previously reported.
Table 1.
Clinical data in children with double simultaneous intussusception.
| Author | Age | Sex | Symptoms | Type | Treatment | Prognosis | Cause |
|---|---|---|---|---|---|---|---|
| Mustafa R, 19767 | 32 days | Male | Bowel protruding through the umbilicus for 2 hours |
Double ileo-vitelline duct | Manual reduction and resection of the vitellointestinal duct | Uneventful | Patent vitellointestinal duct |
| Him FP, 19808 | 7 months | Male | Diarrhoea for 3 days and vomiting for 2 days | Double compound: ileocaecal and colocolic; ileocolic and colocolic | Manual reduction | Uneventful | Idiopathic |
| Bensen JM, 19929 | 5 weeks | Male | Sudden prolapse of the bowel through the umbilicus | Double ileo-vitelline duct | Manual reduction and resection of the vitellointestinal duct | Uneventful | Patent vitellointestinal duct |
| Scholz S, 200010 | 11 years | Female | Regular abdominal pain | Double ileoileal | Manual reduction and resection of the mass | Asymptomatic | Heterotopic pregnancy |
| Kıyan G, 200211 | 8 month | Female | A 48-hour history of irritability, abdominal pain and current jelly-type rectal bleeding and bilious vomiting | Ileocolic and colocolic | Manual reduction | Uneventful | Idiopathic |
| Ahmet, K, 200412 | 8 years | Female | Abdominal pain, vomiting, and bloody stool for 7 days | Double colocolic | Manual reduction | Uneventful | Idiopathic |
| Chen YH, 20064 | 4 years | Female | Abdominal pain and bilious drainage after the first laparotomy | Jejunojejunal and ileocecal | First laparotomy: manual reduction of ileocecal intussusception; second laparotomy: resection of the jejunojejunal intussusception | Uneventful | Angiolipoma; idiopathic |
| Singh JK, 200913 | 10 days | Male | Poor feeding, lethargy, and abdominal distension for 2 days | Ileoileal and ileocolic | Surgical resection | Died of coagulopathy and septicaemia on the 5th postoperative day | Idiopathic |
| Pandey A, 201014 | 10 years | Male | Pain in the abdomen and no passage of flatus and faeces for 8 days, vomiting for 3 days | Jejunojejunal and ileoileal | Resection of jejunojejunal intussusception, manual reduction of ileoileal intussusception | Uneventful | Ileal polyp |
| Shiu JR, 201015 | 17 months | Male | Painless haematochezia and anaemia for 1 day | Ileocolic and ileoileal | Manual reduction of the ileoileal intussusception; resection of the ileocolic intussusception | Uneventful | Idiopathic |
| Destro F, 20146 | 5 years | Male | Seven-day history of cramping abdominal pain |
Double ileoileal | Laparoscopy: manual reduction, resection of the tract containing the mass, and appendectomy | Uneventful | Lipoma |
| Wahid FN, 201416 | 11.5 months | Male | Cramping abdominal pain and bilious vomiting 5 days after bilateral partial nephrectomies | Jejunojejunal and ileoileal | Manual reduction | Uneventful | Postoperative |
| Davidson J, 201517 | 15 years | Female | Five-day history of intermittent and cramping abdominal pain with bilious vomiting and constipation | Not mentioned | Intussusceptions were resolved before laparotomy | Follow-up | Peutz–Jeghers syndrome |
| Jolley H, 20175 | 8 months | Female | Increasing abdominal distension, bilious emesis, and a bloody bowel on postoperative day 1 | Double ileoileal | Manual reduction | Uneventful | Postoperative |
| Our case | 21 months | Female | Paroxysmal abdominal pain for 1 day | Double ileoileal | Manual reduction, resection of Meckel’s diverticulum, and intestinal duplication | Uneventful | Meckel’s diverticulum and intestinal duplication |
In this report, we present a novel case of double simultaneous intussusception with two lead points (Meckel’s diverticulum and intestinal duplication). We also review the epidemiology, pathogenesis, diagnosis, and therapies of this rare condition by analysing all previously reported cases.
Case presentation
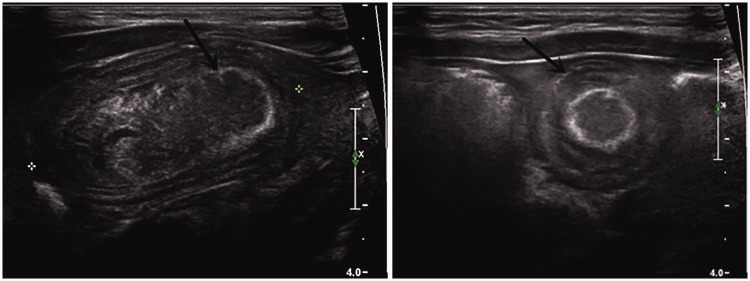
A 21-month- old girl was referred to our hospital (Wuxi Children’s Hospital, Wuxi, China) with a history of paroxysmal abdominal pain for 1 day. The parents of the patient denied any fever, vomiting, abdominal distension, diarrhoea, bloody urine, and faeces. Abdominal ultrasound showed that there were two concentric circles in the left and right lower abdomen (Figure 1). This finding indicated that there might be a double simultaneous intussusception. The result of abdominal computed tomography (Figure 2) was consistent with transabdominal ultrasound.
Figure 1.
Abdominal ultrasound shows two concentric circles in the left and right lower abdomen (black arrow).
Figure 2.
Abdominal computed tomography shows two intussusceptions in the left and right lower abdomen.
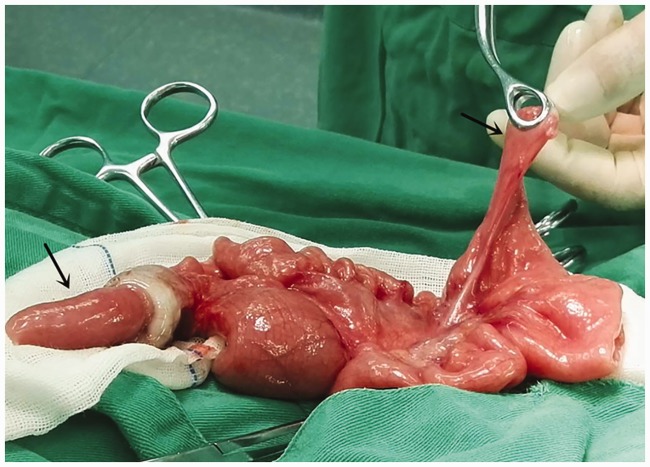
The patient initially received an air enema reduction, but this failed. The patient then received an exploratory laparotomy with emergency general anaesthesia. In the laparotomy, double ileoileal intussusception was found. One intussusception was approximately 65 cm from the ileocecal valve. The lead point of one of the intussusceptions was Meckel’s diverticulum, which was approximately 5 cm in length and 1 cm in width, and it was connected with the normal mesentery. Meckel’s diverticulum settled into the intestine approximately 15 cm along the basal part of the ileal wall. Another intussusception had intestinal duplication as the lead point and was approximately 110 cm from the cecum. The intestinal duplication was approximately 10 cm in length with a 2-cm-wide basal area and was interconnected with the ileum without apparent mesenteric vessels (Figure 3). There was partial necrosis in the intestinal intussusception. There were no other obvious abnormalities from the small intestine to the ligament of Treitz by further exploration. The two intussusceptions were successfully cured by manual reduction.
Figure 3.
Photograph of surgery. The left black arrow shows Meckel’s diverticulum, which is approximately 5 cm in length and 1 cm in width, and it is interconnected with the ileum without apparent mesenteric vessels. The right arrow shows intestinal duplication, which is approximately 10 cm in length with a 2-cm-wide basal area, and is connected with the normal mesentery.
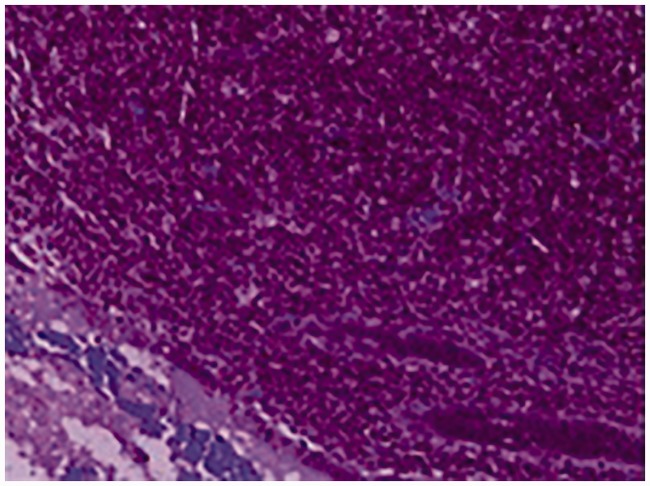
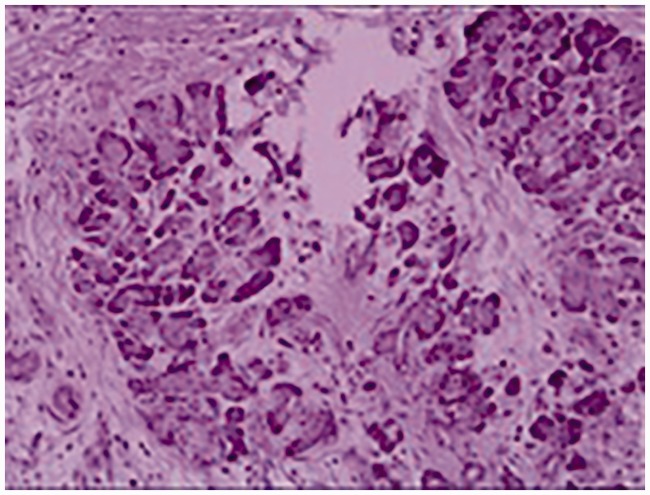
The patient then underwent resection of Meckel’s diverticulum and intestinal duplication, as well as appendectomy. Postoperative pathology showed that Meckel’s diverticulum had congestion and oedema with infiltration of lymphocytes and eosinophilic cells (Figure 4). The intestinal duplication was infiltrated by lymphocytes with a blind end, which contained heterotopic pancreatic tissue (Figure 5). Postoperative recovery of the patient was good, and there were no adverse events after a 6-month follow-up.
Figure 4.
Postoperative pathology shows that Meckel’s diverticulum has congestion and oedema with infiltration of lymphocytes and eosinophilic cells.
Figure 5.
Postoperative pathology shows that the intestinal duplication is infiltrated with lymphocytes with a blind end, which contains heterotopic pancreatic tissue.
This article is a case report and literature review, and thus no ethical approval was required. We obtained written informed consent from the patient.
Discussion
Although intussusception is common in children, double simultaneous intussusception is a rare condition, which may be categorized into four types 4 These types include the following: two separate intestines prolapsing into the same distal intestine, resulting in a characteristic “triple-circle” sign by sonography; two separate intussusceptions in two separate sites; double compound intussusception; and double prolapse of the proximal and distal intestine through a patent vitellointestinal duct. Only 14 cases of double intussusception have been reported.4–17
Double simultaneous intussusception may be mainly attributed to an explicit lead point, the idiopathic status, or even the postoperative status. The lead point is the main factor, including a patent vitellointestinal duct, heterotopic pregnancy, ileal polyp, angiolipoma, lipoma, and Peutz–Jeghers syndrome. Most of the previously reported cases showed only one lead point. However, this is the first case of double intussusception with two lead points. Additionally, five patients with double intussusception were idiopathic. The postoperative status is another factor that should be taken into consideration. Two previous cases of double intussusception occurred after initial operations within 5 days, including exploratory5 laparotomy and bilateral partial nephrectomy.
The clinical features of double simultaneous intussusception mainly consist of abdominal pain, abdominal distension, vomiting, and bloody stool, similar to common intussusception to some extent.18,19 However, some other concomitant symptoms should not be ignored, such as diarrhoea, poor feeding, irritability, and lethargy, especially in infants. The proximal and distal intestines passing through a patent vitellointestinal duct is a special type of prolapse of double intussusception, which is rare with unambiguous features.
The diagnosis of double intussusception mainly depends on the medical history, a physical check-up, and an auxiliary examination. The medical history refers to clinical manifestations discussed above. The most useful sign of a physical check-up is an abdominal mass. An abdominal mass was apparent in less than half of the reported cases of double intussusception6,8,10,11,13,16 and none of them presented as two palpable masses. Some of these patients can have abdominal tension and increased bowel sounds. Abdominal ultrasound is the most common in auxiliary examination for double intussusception and the main feature is double concentric circular or triple-circle sign, which is also apparent in less than half of the cases. Additionally, X-ray and computed tomography are important auxiliary methods.20 Among all of the cases of double intussusception, only eight patients (including our patient)5,7,9,12,14,15,17 were diagnosed before surgery, while the remaining seven patients were diagnosed during intraoperative inspection.
Treatment of double simultaneous intussusception is different from common intussusception to some extent. Most intussusceptions can be treated with non-surgical methods, such as enema with barium, air, or water. In all of the 15 cases of double simultaneous intussusception, most children accepted enema with air or water, but all of these treatments failed. This failure could have been due to the structure of double simultaneous intussusception, which is more complex and tighter than just intussusception. Therefore, we suggest that children who are diagnosed with double simultaneous intussusception should accept surgery directly. This could avoid unnecessary treatment, as well as wasting time and decreasing the risk of bowel necrosis. Surgical methods include laparotomy (majority) and laparoscopic surgery.21,6
Postoperative recovery of most children with double simultaneous intussusception is usually good. Only one newborn with double simultaneous intussusception died because of coagulopathy and septicaemia.13 Therefore, clinical doctors need to pay more attention to patients after surgery, especially to younger patients with a poor physical condition. Follow-up after discharge from hospital after treating double simultaneous intussusception is also important.
Conclusion
In conclusion, double simultaneous intussusception is rare. To the best of our knowledge, this is the first case of double simultaneous intussusception caused by Meckel’s diverticulum and intestinal duplication in a child. The diagnosis of this condition mainly depends on the medical history, a physical check-up, and an auxiliary examination, while only approximately half of these cases can be diagnosed before surgery. Generally, non-surgical methods are invalid for double simultaneous intussusception and emergent exploration is suggested. Most patients can recover well after surgery and postoperative follow-up is recommended. With further development of technology, more similar cases of double simultaneous intussusception are likely to be reported.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by Wuxi Young Medical Talents (Grant No. QNRC023) and the Medical Innovation Team of Jiangsu Province (Grant No. CXTDB2017016).
References
- 1.Kawasaki Y, Shinozaki S, Yano T, et al. Intussusception due to an inverted Meckel's diverticulum diagnosed by double-balloon enteroscopy. Case Rep Gastroenterol 2017; 11: 632–636. 2017/12/29. DOI: 10.1159/000481161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiang J, Jiang B, Parashar U, et al. Childhood intussusception: a literature review. PloS One 2013; 8: e68482. 2013/07/31. DOI: 10.1371/journal.pone.0068482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards EA, Pigg N, Courtier J, et al. Intussusception: past, present and future. Pediatr Radiol 2017; 47: 1101–1108. 2017/08/06. DOI: 10.1007/s00247-017-3878-x. [DOI] [PubMed] [Google Scholar]
- 4.Chen YH, Diau GY, Chang CH, et al. Double site intussusception in a four-year-old girl. J Med Sci 2006; 26: 191–193. [Google Scholar]
- 5.Jolley H, Gefen AM, Ginsburg H, et al. Double ileoileal intussusception following surgical reduction of ileocolic intussusception in an 8-month-old female. J Pediatr 2017; 186: 208. [DOI] [PubMed] [Google Scholar]
- 6.Francesca D, Noemi C, Michela M, et al. An interesting case of double compound intussusception without intestinal occlusion in a 5-year-old boy. European J Pediatr Surg Rep 2014; 2: 20–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mustafa R. Double intussusception of the small bowel through a patent vitello-intestinal duct. Br J Surg 1976; 63: 452. [DOI] [PubMed] [Google Scholar]
- 8.Him FP, Weng YK, Hoi CW. A case of double compound intussusception in an infant. Singapore Med J 1980; 21: 540–541. [PubMed] [Google Scholar]
- 9.Benson JM, Sparnon AL. Double intussusception of ileum through a patent vitello-intestinal duct: report of a case and literature review. Aust N Z J Surg 1992; 62: 411–413. [DOI] [PubMed] [Google Scholar]
- 10.Scholz S, Loff S, Wirth H. Double ileoileal intussusception caused by a giant polypoid mass of heterotopic pancreas in a child. Eur J Pediatr 2000; 159: 861–862. [DOI] [PubMed] [Google Scholar]
- 11.Kiyan G, Tugtepe H, Iskit SH, et al. Double intussusception in an infant. J Pediatr Surg 2002; 37: 1643. [DOI] [PubMed] [Google Scholar]
- 12.Kazez A, Ozel SK, Kocakoc E, et al. Double intussusception in a child. J Ultrasound Med 2004; 23: 1659–1661. [DOI] [PubMed] [Google Scholar]
- 13.Singh JK, Bawa M, Kanojia RP, et al. Idiopathic simultaneous intussusceptions in a neonate. Pediatr Surg Int 2009; 25: 445–447. [DOI] [PubMed] [Google Scholar]
- 14.Pandey A, Rawat JD, Wakhlu A, et al. Simultaneous occurrence of jejuno-jejunal and ileo-ileal intussusception in a child: a rare occurrence. BMJ Case Rep 2011; 2011: bcr0820103294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shiu JR, Chao HC, Chen CC, et al. Rare concurrent ileoileal and ileocolic intussusceptions in a child presenting with painless hematochezia. Pediatr Neonatol 2010; 51: 359–362. [DOI] [PubMed] [Google Scholar]
- 16.Wahid FN, Malkan AD, Mccarville MB, et al. Double small bowel intussusception complicating bilateral partial nephrectomies. J Pediatr Surg Case Rep 2014; 2: 30–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davidson J, Wright NJ, Kufeji D. Differential diagnosis of double site intussusception in childhood: a 15-year-old girl presenting with bowel obstruction. BMJ Case Rep 2015; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu ML, Lee KH, Li YL. The crescent-in-doughnut sign in intussusception. Abdom Radiol (NY) 2018; 43: 1266–1267. [DOI] [PubMed] [Google Scholar]
- 19.Gluckman S, Karpelowsky J, Webster AC, et al. Management for intussusception in children. Cochrane Database Syst Rev 2017; 6: CD006476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Grezia G, Gatta G, Rella R, et al. Abdominal hernias, giant colon diverticulum, GIST, intestinal pneumatosis, colon ischemia, cold intussusception, gallstone ileus, and foreign bodies: our experience and literature review of incidental gastrointestinal MDCT findings. Biomed Res Int 2017; 2017: 5716835. DOI: 10.1155/2017/5716835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kleizen KJ, Hunck A, Wijnen MH, et al. Neurological symptoms in children with intussusception. Acta Paediatrica 2014; 80: 293–298. [DOI] [PubMed] [Google Scholar]