Short abstract
Objective
To determine the effectiveness of a narrative medicine educational intervention on the empathic abilities and academic achievement of Chinese nursing students.
Methods
A cluster randomised controlled trial was conducted between January 2015 and July 2017. Six class clusters (two controls, four interventions) comprising 180 nursing students were included in this trial. After pre-tests to obtain baseline measurements, two control classes (Group 1) attended regular medical education courses, two intervention classes (Group 2) received theoretical narrative medicine education for 1 term, and two intervention classes (Group 3) received narrative medicine education that integrated theory with practice for 2 terms. The empathic ability and academic achievement of the groups were compared, and longitudinal changes in empathic ability were measured.
Results
Students in Group 3 showed higher empathic ability and academic achievement than students in Group 1. Empathic ability was measured at six time points and showed between-group differences. The empathy scores of students in Group 3 increased abruptly after the two-term intervention.
Conclusions
Narrative medicine education that combines theory with practice is an effective strategy for improving nursing students’ empathic ability and academic achievement.
Keywords: Narrative medicine, clinical educational intervention, empathy, academic achievement, nursing students, China
Introduction
Medical science has the dual attributes of natural science and social science. Medical staff not only provide high-quality medical services to patients, but also provide emotional companionship and spiritual support. An examination of the medical services available in China today reveals that patients have a surprisingly low degree of satisfaction in advanced treatment options, and there are fierce conflicts between medical staff and patients. Medical education students consider grades and technology more important than providing humanistic care to patients, and they maintain this perspective when they join the medical workforce. This viewpoint also underlies ineffective doctor–patient communication and the lack of high-quality humanistic care in Chinese hospitals.1,2 Therefore, it is important to enhance the empathic ability of medical students.
Empathy is the process of understanding another person’s inner experiences and feelings and viewing the world from the other person’s perspective.3 People who have high empathy levels can imagine themselves in the position of others and understand their perspectives after listening to their narratives.4 In the clinical context of communicating with patients, empathy includes emotional (an internal capability to imagine the patient’s emotions, feelings and perspectives), moral (a desire to empathise), cognitive (an ability to correctly identify and understand feelings) and behavioural (an ability to express an understanding of those feelings to the patient) dimensions.5 Published reports show that empathy between medical staff and patients in clinical activities can help to improve physician occupational well-being and patient satisfaction, compliance and therapeutic outcomes.6–8 Empathy is also important for establishing good doctor–patient communication.9 Therefore, medical students should receive empathy education. In medical schools in developed countries, empathy education is currently conducted using different methods,10 such as situated teaching,11 simulation of the patient experience12 and reflective discussion.13 The American Association of Medical Colleges (AAMC) requires all American medical schools to offer empathy training courses.14
The concepts of narrative medicine and empathy are inseparable. Narrative medicine was first proposed by Rita Charon in 2001 and refers to medicine practiced with narrative competence. Narrative medicine is based on a model of empathy, reflection, professionalism and trust that can be applied in clinical practice, particularly in oncology. If the staff respect and understand the patients’ narratives, they can respond empathically to the patients’ suffering.15,16 In this way, patients are recognised as individuals rather than solely as patients; this viewpoint can help doctors, nurses, caregivers and patients to form alliances to address disease together.17 Moreover, narrative medicine can provide meaningful support to patients in clinical practice and breaks new ground in compassionate healthcare.18
Many medical schools, particularly those in developed countries, include narrative medicine education as part of students’ empathy education.19 For example, at the University of North Carolina at Chapel Hill School of Nursing, USA, patients with chronic disease were asked to show their narratives to nursing students, and a question-and-answer session was held to hear their stories.20 Such courses may help to improve the empathy of medical students.
However, only a few studies have examined whether a narrative medicine education program can help to improve nursing students’ empathic ability or academic achievement, and there has been no such research on nursing students in mainland China. The present study reviewed the current literature and designed a narrative medicine education program based on that literature. The following questions were investigated in this study: 1) Can narrative medicine education improve nursing students’ empathic ability and academic achievement? 2) What type of narrative medicine education program is more effective? 3) What is the average change in the students’ empathy scores?
Materials & methods
Participants
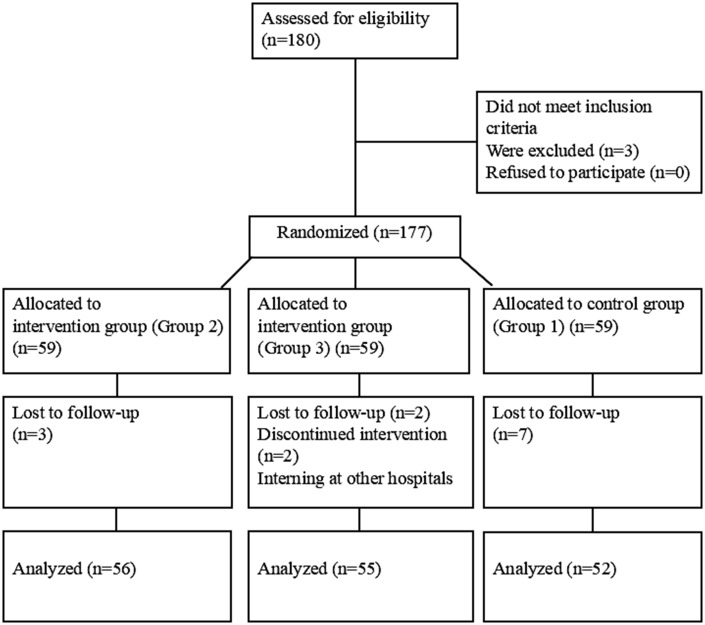
A cluster sampling strategy was used. The process of selection and allocation of eligible participants is shown in Figure 1. The participants were Grade 3 students at a nursing school in northeast China. Of the sixteen classes, six (30 students per class) were randomly selected to participate in this study. The target study population was all 180 of the nursing students in these classes. Taking each class as a unit, the six classes were randomly divided into three groups: one observation group (Group 1) and two experimental groups (Groups 2 and 3). The exclusion criteria were as follows: students who were taking doctor–patient communication-related courses and students who were planning to take those courses during the study. All participants provided written or verbal informed consent. Ethical approval was not required for this work. There was no risk from participation in the program and the responses were treated confidentially. Narrative medicine courses are offered in many medical schools and the program was conducted in accordance with ethical standards.
Figure 1.
Flow chart of sample selection of 180 nursing students, 2015–2017
Procedure
The study was conducted between January 2015 and July 2017. A cluster randomised controlled trial was conducted and data were collected pre- and post-intervention. First, empathic ability was compared among the three groups before and after the intervention, and students’ academic achievement level at the time of their graduation was obtained and compared. The purpose of this comparison was to assess the effectiveness of educational interventions. Second, to explore the change in students’ empathic ability and to provide a basis for the timing of the educational intervention, empathic ability was measured six times: T1: January 2015 (pre-intervention; the conclusion of the first term of Grade 3), T2: July 2015 (post-step 1 intervention; the conclusion of the second term of Grade 3), T3: January 2016 (post-step 2 intervention; the conclusion of the first term of Grade 4), T4: July 2016 (0.5 years after the intervention; the conclusion of the second term of Grade 4), T5: January 2017 (1 year after the intervention; 6 months after graduation), and T6: July 2017 (1.5 years after the intervention; 1 year after graduation). T5 and T6 were during the first year of students’ post-graduation employment. Then, the longitudinal change in the empathic ability of each group was analysed.
Narrative medicine program
The narrative medicine program was divided into two parts: theoretical education and clinical practice education. The students in Group 2 received theoretical education only. For the junior students, the course occurred during the spring term and lasted for 4 months. The courses were conducted by a teacher well trained in narrative medicine. Students had 12 weekly sessions that comprised an hour-long class. The class consisted of narrative medicine theory, observation and discussion of movies, and reading and analysis of medical narrative books.21 The main reference book for the theoretical education was Narrative Medicine: Honoring the Stories of Illness, written by Rita Charon.15 The movies were Wit, Tuesdays with Morrie, and Patch Adams. The books were The Illness Narratives: Suffering, Healing & the Human Condition, by Arthur Kleinman; The Wheel of Life, by Elisabeth Kubler Ross; The Grace in Dying: How We Are Transformed Spiritually as We Die, by Kathleen Dowling Singh and How We Die: Reflections on Life’s Final Chapter, by Sherwin Bernard Nuland. The students were required to closely read the books and watch the movies after class. During the class, the teacher and the students discussed the stories and analysed their meaning. The aim of the discussion was to help students try to understand the patients’ experiences and develop a deeper understanding of the meaning of medicine. Key words and phrases used in the course were ‘company’, ‘empathy’, ‘holistic care’ and ‘life and death’. The course focused on helping students to gain a preliminary understanding of narrative medicine and to develop their narrative abilities. The course grade was composed of group reports (six people per group) and research papers. The students’ grades could replace an optional course grade, which was earned during the same class hour.
The students in Group 3 received both theoretical education and clinical practice education. These students received the same theoretical education as those in Group 2. The clinical practice education occurred during the autumn term, from September to December, when the students were in graduate class and beginning clinical practice. Their mentors were teaching nurses who had been trained in narrative medicine. The students were divided into groups (10 students per group) with one mentor per group. First, the students were asked to listen to the patients’ stories and respond to their narratives. The key focus in this part of the class was parallel chart writing. Students were required to write the patients’ parallel charts according to the patients’ narratives; the parallel charts supplemented the standard medical records and included the patients’ life situations, physical feelings and psychological and social needs. The parallel charts emphasised social, cultural and ethical aspects.22 Then, the team members shared the patients’ stories and explored the patients’ multiple needs. Second, both the nursing students and the patients wrote and exchanged diaries. In the diaries, students wrote about the patients’ physical and mental trauma and built an understanding of them and a dialogue with them. This approach was aimed at helping them to develop deeper, high-quality nurse–patient communication and construct a community based on emotion, morality and personal values. The range of dimensions on which the students helped the patients could be expanded according to the patients’ needs.23 Third, students were asked to perform reflective writing to review and interpret their experiences.24 The cases included several first experiences in clinical practice, such as the first time in charge of a patient and participation in surgery. Moreover, the students could include information about the patients who impressed them, the process of their communication with the patients and their own experiences with illness, as well as their thoughts about the patients, medical care or their medical career journey. The mentors encouraged the students to adopt diverse forms of expression, such as prose and poetry. Through reflective writing, the students re-examined the nurse–patient relationship and the role of the nurse; consequently, their nursing-related thought processes and their relational and ethical competence were optimised. The aim was to develop students’ critical thinking, and importance was attached to the emotional dimensions of both the patients and the students. In this way, students could achieve a deeper understanding of care and a guide for their future behaviour. In this program, students were asked to complete two parallel charts, exchange diaries with one patient and write two reflective papers. In addition, each team held a 2-hour seminar once every 2 weeks, during which they discussed their clinical work, writing and experience, and shared their introspections.25 For the final report, each group gave a presentation about what they had learned from the program; they shared their thoughts about the patients’ feelings and discussed ways to provide humanistic care. The teachers who conducted the theoretical and clinical education reviewed these presentations and scored the groups according to their performance in the learning process, the assignment and the presentation. The group that performed the best was rewarded.
Measures
Empathic ability
The Chinese version of the Jefferson Scale of Empathy (JSE) was used to measure individual differences in empathy among the nursing students. The scale was constructed in 2001 at the Jefferson Medical College, USA, to assess empathy in the context of patient care and medical education.26 Although many scales have been used to measure empathic ability, the JSE focuses on the empathy between medical staff and patients. Measurements of the empathy of doctors, nurses or medical students include awareness of the experiences, concerns and perspectives of patients, the ability to verbalise an understanding of these concepts and the will to help patients.27–29 The JSE comprises 20 items; responses are scored on a 7-point Likert scale by conversion to a numerical score ranging from 1 to 7. A score of 1 corresponds to a response of ‘Strongly Disagree’ and a score of 7 corresponds to ‘Strongly Agree’.29 Therefore, scores on the JSE range from 20 to 140, with higher scores indicating higher levels of empathy. The JSE has been successfully used in many countries and has good reliability and validity.30 The Chinese version of the JSE has shown satisfactory reliability and validity in clinical studies and has been widely used in China.31
Academic achievement
Measurement of the nursing students’ academic achievement included their internship score and graduation thesis achievement. The test used a percentage grading system. The students’ transcripts were provided by the teacher.
Statistical analyses
Epi Info version 3.1 (Centers for Disease Control and Prevention, Atlanta, GA, USA) was used for the entry and summary of the data. IBM SPSS Statistics, version 20 (IBM Corp., Armonk, NY, USA) was used to analyse the data. All data are expressed as mean values ± the standard deviation. One-way analysis of variance (ANOVA) with a least significant difference (LSD) test was used to compare the three groups on empathic ability and academic achievement. A repeated measures ANOVA was used to measure longitudinal changes in empathic ability. The level of statistical significance was set at P<0.05.
Results
Demographic and baseline characteristics of the participants
In total, 163 students (90.56%) participated in all stages of the study. The mean age of participants was 17.96 ± 0.37 years (range: 16–19 years). Of participants, 10 were male, and 153 were female. Before the intervention, there was no significant difference in age, sex or empathy score among the three groups. The baseline sociodemographic characteristics and empathy scores of the students before the intervention are shown in Table 1.
Table 1.
Demographics and baseline data of 163 nursing students by group, 2015–2017
| Group 1 | Group 2 | Group 3 | F or χ2 | P | |
|---|---|---|---|---|---|
| Age | 17.94 (0.465) | 17.96 (0.328) | 17.96 (0.328) | 0.066 | 0.936a |
| Sex: male/female | 3/48 | 3/53 | 4/52 | 0.163 | 0.922b |
| Empathy score (T1) | 103.69 (12.23) | 104.66 (13.58) | 104.70 (14.13) | 0.097 | 0.908a |
Notes: aANOVA. bChi-square test. Data show mean (standard deviation).
Comparison of empathic ability and achievement among the different student groups
One-way ANOVA was used to compare the students’ internship scores, graduation thesis achievement and empathic ability after the educational intervention. The results in Table 2 show significant differences in internship scores (P<0.05) but not in graduation thesis achievement and empathic ability among the three groups. However, the LSD test revealed significant differences between Group 1 and Group 3 in internship scores, graduation thesis achievement and empathic ability (P<0.05).
Table 2.
Comparison of empathic ability, internship score and graduation thesis achievement for nursing students in three groups, 2015–2017
| Group 1 | Group 2 | Group 3 | F | P | |
|---|---|---|---|---|---|
| Internship score | 84.92 (6.63) | 86.89 (5.36) | 88.05 (5.09)a | 4.175 | 0.018 |
| Graduation thesis achievement | 84.83 (5.03) | 85.68 (5.02) | 86.85 (3.66)a | 2.720 | 0.076 |
| Empathy score (T3) | 104.79 (11.82) | 107.91 (13.01) | 110 (13.51)a | 2.742 | 0.067 |
Notes: aThe difference compared with Group 1 (P<0.05) (using least significant difference test). Data show mean (standard deviation).
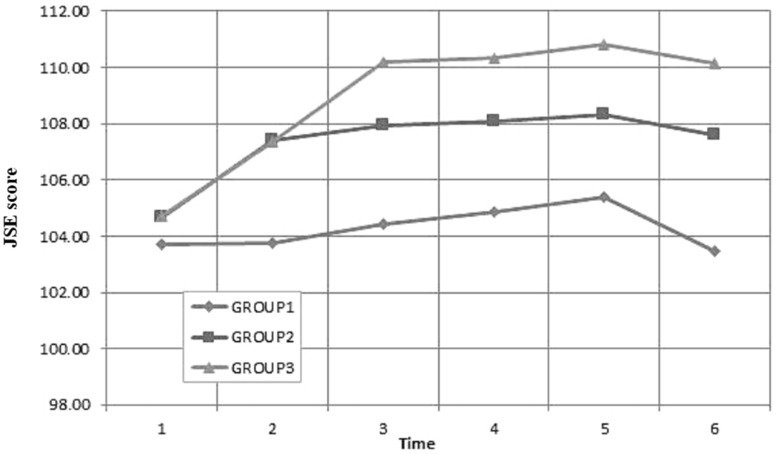
Longitudinal changes in empathic ability
The repeated measures data were used to measure the longitudinal change in the empathic ability of the students in each group at different time points. The results showed that the empathic ability of each group varied over time. For Group 3, empathic ability increased rapidly after T3 (after the two-term intervention), and the differences in empathic ability between T1 and T3, T4, T5 and T6 were statistically significant (P<0.05). Table 3 shows the numerical results and Figure 2 shows a graphical representation of these changes.
Table 3.
Longitudinal change in empathic ability for students in the three groups, 2015–2017
| T1 | T2 | T3 | T4 | T5 | T6 | |
|---|---|---|---|---|---|---|
| G1 | 104.08 (12.43) | 104.06 (11.75) | 104.79 (11.82) | 105.25 (11.84) | 105.73 (11.94) | 103.85 (12.00) |
| G2 | 104.59 (13.48) | 107.45 (13.34) | 107.91 (13.01) | 108.04 (13.21) | 108.27 (13.09) | 107.57 (12.83) |
| G3 | 104.42 (14.11) | 107.07 (14.08) | 110 (13.51)a | 110.11 (13.30)a | 110.62 (13.22)a | 109.98 (13.37)a |
Notes: aThe difference compared with T1 (P<0.05). Data show mean (standard deviation).
Figure 2.
Longitudinal change in empathic ability of three groups of nursing students, 2015–2017 JSE: Jefferson Scale of Empathy.
Discussion
This study generated three main findings. First, students who received both theoretical education and clinical practice education (Group 3) showed a higher empathic ability than students who did not participate in the narrative medicine program (Group 1) and those who received theoretical education only (Group 2). This suggests that a combination of theory and practice in narrative medical education is effective in improving the empathic ability and comprehensive performance of nursing students. Other studies have confirmed the positive role of narrative medical education in improving empathy and achievement. For example, Chen et al.32 confirmed that a 2-month narrative medicine program improved healthcare providers’ empathy. The students in the present study developed a concept of narrative medicine through theoretical education, and the practical education allowed them to master the narrative method more systematically and put the concepts into clinical practice. Therefore, narrative medical education combined with theory and practice may be more effective than narrative medicine alone. There are several possible reasons why this model of narrative medical education helped to improve students’ empathy. First, by exchanging diaries with the patients, the students were able to talk deeply with patients about topics such as the effects of trauma on the body and mind and the experience of the soul, and could better understand the patients’ life circumstances. Students developed a deeper, high-quality level of nurse–patient communication, which helps to establish an emotion-, morality- and value-based community. Through this process, the nursing students deepened their sympathy, empathy and empathetic understanding of the fate of the patients. Second, parallel chart writing is an important way to improve empathy. Students listen to and respect the patients’ stories; this helps them to move from a perspective characterised by data-based rationality and objectivity to a perspective that recognises patient experience-based subjectivity when communicating with and caring for patients. By recording patient narratives, nursing students learn to develop empathy and an understanding of the patients’ circumstances, including their physical, psychological, social and spiritual needs. Students use these experiences in the care of other patients and continue to deepen their empathy in practice.33 Third, reflective writing may be a key way to improve empathic ability.34 Psychological/behavioural theories of reflection focus on the cognitive aspects of reflection, the practice of retrospective self-review and critical self-assessment, which culminate in decision making about how to change one’s behaviours when next faced with a similar situation.35 Thus, if students do not understand the feelings of patients on some occasions, they may write and think about this experience, which may help them to improve their empathic ability the next time they encounter the same type of situation. Students also engaged in reflective writing in which they shared their own experiences with illness, an action that may counteract the traditional distancing of nurses’ minds from their bodies.36 When a ‘white coat’ is replaced with ‘viral bronchiolitis’ and the student perceives him/herself in the role of a patient rather than a medical practitioner, a more empathic and self-aware practice occurs. Thus, reflective writing reinforces nursing students’ perception of themselves and others, which may improve their empathic ability.
Second, students who received both theoretical education and clinical practice education showed higher academic achievement than students who did not receive narrative medicine education. This result is similar to that reported by Tsai et al.,37 who found that narrative medicine training improved objective structured clinical exam (OSCE) performance. In the present study, the internship scores of students who received narrative medicine education were higher than those of students who did not receive narrative medicine education, possibly because narrative medical education deepens students’ understanding of the essence of medicine and their concept of holistic care. Therefore, during the internship, students paid more attention to the humanistic care of patients when communicating with patients and performing nursing duties. Students were able to better understand patients’ feelings and give them appropriate and targeted help. The patients and teachers also rated the students who received narrative medical education more highly, and these students received a higher internship score. In contrast, the nursing students in Group 3 received higher scores on their graduation theses, but no difference was found between the graduation thesis scores of Group 1 and Group 2. This indicates that a narrative medicine program that combines theory with practice is effective, probably because parallel chart writing provides opportunities to practice critical thinking and to improve and optimise medical service.38 Group 3 students developed theses that were more in-depth in their conclusions and more diverse in scope. In addition, through the clinical narrative medical training, the students became more adept at listening to the complaints and analysing the medical history of the patients. Therefore, the training also improved students’ ability to diagnose illness and provide personalised care, which helped them to write better graduation theses.
Third, this study showed that the empathy scores of the three groups of students changed over time. The students were enrolled in clinical practice in the first term of Grade 4 (T3), and their empathy improved after the internship. This improvement may be related to the change in their identity from nursing students to ‘nurses’. At that time, they deepened their participation in patient care for patients and were more concerned about the patient’s care needs. However, after 1 year of work, their empathic ability declined; this change may be related to empathy burnout.39 Empathy burnout occurs because young nurses tend to take on a significant amount of basic care, and they are required to spend more time performing technical duties, which reduces the time and energy spent communicating with patients. Compared with empathic ability before the narrative medicine education (T1), the empathic ability of Group 3 was significantly higher at each time point after T3. This shows that the effect of clinical practice education on the empathic ability of nursing students is continuous and obvious. This trend also suggests that nursing educators and administrators should pay more attention to continuing the education of nurses. Narrative medical practice education could be provided to relieve burnout and enhance the empathic ability of young nurses who have been working for 1 year or longer.
Limitations
First, the sample size was small and most of the students were female; therefore, the impact of this intervention on male nursing students was difficult to assess. Therefore, our hypotheses must be tested in a larger sample with a more equal sex ratio. Second, the effects of time and experience on empathic ability require further study using different approaches, such as qualitative research. Additionally, the empathy of nurses should be tracked for a longer period. Third, as empathy is related to interpersonal communication, an exploration of patients’ perspectives of nurses’ empathy is necessary; as the JSE is a self-report measure, it would be preferable to use both the JSE and the patient-rated CARE (Consultation and Relational Empathy) Measure.40
Conclusion
This study indicates that a narrative medicine program that combines theory and practice is a useful evidence-based educational intervention for improving the empathic ability and academic achievement of nursing students. As their seniority increases, new nurses may experience burnout and their empathic ability may decline as soon as 1 year after graduation. Thus, narrative medical education should not only be provided for medical students, but should also be continued throughout the professional life of medical staff, and methods that combine theory with practice may be appropriate. However, narrative medicine interventions alone have limited effects, and more projects in medical humanities education should be implemented to improve medical students’ achievements, empathic ability and other competencies in clinical medical humanities. Medical staff would also benefit from similar projects.
Acknowledgments
The authors thank all the nursing students who participated in the study.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Zhao L, Zhang XY, Bai GY, et al. Violence against doctors in China. Lancet 2014; 384: 744. [DOI] [PubMed] [Google Scholar]
- 2.Li J, Qi F, Guo S, et al. Absence of humanities in China’s medical education system. Lancet 2012; 380: 648. [DOI] [PubMed] [Google Scholar]
- 3.Hojat M, Gonnella JS, Nasca TJ, et al. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry 2002; 159: 1563–1569. [DOI] [PubMed] [Google Scholar]
- 4.vvan Dijke J ,van Nistelrooij I ,Bos P, et al. Care ethics: an ethics of empathy? Nursing Ethics 2018: 969733018761172, DOI: 10.1177/0969733018761172. [DOI] [PubMed] [Google Scholar]
- 5.Ariso JM. Enhancing second-order empathy in medical practice by supplementing patients’ narratives with certainties. BMC Med Educ 2018; 18: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lipp MJ, Riolo C, Riolo M, et al. Showing you care: an empathetic approach to doctor–patient communication. Semin Othod 2016; 22: 88–94. [Google Scholar]
- 7.Hojat M, Louis DZ, Markham FW, et al. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med 2011; 86: 359–364. [DOI] [PubMed] [Google Scholar]
- 8.Lelorain S, Brédart A, Dolbeault S, et al. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology 2012; 21: 1225–1264. [DOI] [PubMed] [Google Scholar]
- 9.Larso EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA 2005; 293: 1100–1106. [DOI] [PubMed] [Google Scholar]
- 10.Brunero S, Lamont S, Coates M. A review of empathy education in nursing. Nurs Inq 2010; 17: 65–74. [DOI] [PubMed] [Google Scholar]
- 11.Lee KC, Yu CC, Hsieh PL, et al. Situated teaching improves empathy learning of the students in a BSN program: a quasi-experimental study. Nurse Educ Today 2018; 64: 138–143. [DOI] [PubMed] [Google Scholar]
- 12.Percy M, Richardson C. Introducing nursing practice to student nurses: how can we promote care compassion and empathy. Nurse Educ Pract 2018; 29: 200–205. [DOI] [PubMed] [Google Scholar]
- 13.Nelson SW, Germann CA, Macvane CZ, et al. Intern as patient: a patient experience simulation to cultivate empathy in emergency medicine residents. Western J Emerg Med 2018; 19: 41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hojat M, Gonnella JS, Mangione S, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ 2002; 36: 522–527. [DOI] [PubMed] [Google Scholar]
- 15.Charon R. Narrative medicine: honoring the stories of illness. New York: Oxford University Press, 2006, pp. 218–225. [Google Scholar]
- 16.Charon R. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA 2000; 286: 1897–1902. [DOI] [PubMed] [Google Scholar]
- 17.Rosti G. Role of narrative-based medicine in proper patient assessment. Support Care Cancer 2017; 25: 3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barber S, Morenoleguizamon CJ. Can narrative medicine education contribute to the delivery of compassionate care? A review of the literature. Med Humanities 2017; 43: 199–203. [DOI] [PubMed] [Google Scholar]
- 19.Wieżel I, Horodeńska M, Domańska-Glonek E, et al. Is there a need for narrative medicine in medical students’ education? A literature review. Med Sci Educator 2017; 15: 1–7. [Google Scholar]
- 20.Leonard CR, Zomorodi M, Foster BB. The impact of caring: teaching students empathy through the patient voice. Creat Nurs 2018; 24: 62–66. [DOI] [PubMed] [Google Scholar]
- 21.Skelton JR, Macleod JA, Thomas CP. Teaching literature and medicine to medical students, part II: why literature and medicine? Lancet 2001; 356: 2001–2003. [DOI] [PubMed] [Google Scholar]
- 22.Shapiro J. Narrative medicine and narrative writing. Fam Med 2012; 44: 309–311. [PubMed] [Google Scholar]
- 23.Charon R. Medicine, the novel, and the passage of time. Ann Intern Med 2000; 132: 63–68. [DOI] [PubMed] [Google Scholar]
- 24.Charon R, Hermann N. Commentary: a sense of story, or why teach reflective writing? Acad Med 2012; 87: 5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arntfield SL, Slesar K, Dickson J, et al. Narrative medicine as a means of training medical students toward residency competencies. Patient Educ Couns 2013; 91: 280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Meas 2001; 61: 349–365. [Google Scholar]
- 27.Hojat M. Ten approaches for enhancing empathy in health and human services cultures. J Health Human Services Admin 2009; 31: 412–450. [PubMed] [Google Scholar]
- 28.Hojat M, Gonnella JS. What matters more about the Interpersonal Reactivity Index and the Jefferson Scale of Empathy? Their underlying constructs or their relationships with pertinent measures of clinical competence and patient outcomes? Acad Med 2017; 92: 743–745. doi: 10.1097/ACM.0000000000001424 [preprint]. [DOI] [PubMed] [Google Scholar]
- 29.Hojat M. Empathy in patient care: antecedents, development, measurement, and outcomes. New York: Springer, 2007, pp. 12–20. [Google Scholar]
- 30.Costa P, de Carvalho-Filho MA, Schweller M, et al. Measuring medical students’ empathy: exploring the underlying constructs of and associations between two widely used self-report instruments in five countries. Acad Med 2017; 92: 860–867. [DOI] [PubMed] [Google Scholar]
- 31.Wen D, Ma X, Li H, et al. Empathy in Chinese physicians: preliminary psychometrics of the Jefferson Scale of Physician Empathy (JSPE). Med Teach 2013; 35: 609–610. [DOI] [PubMed] [Google Scholar]
- 32.Chen PJ, Huang CD, Yeh SJ. Impact of a narrative medicine programme on healthcare providers’ empathy scores over time. BMC Med Educ 2017; 17: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spencer AC. Stories as gift: patient narratives and the development of empathy. J Genet Couns 2016; 25: 687–690. [DOI] [PubMed] [Google Scholar]
- 34.Sklar DP. Health humanities and medical education: joined by a common purpose. Acad Med 2017; 92: 1647–1649. [DOI] [PubMed] [Google Scholar]
- 35.Charon R, Hermann N, Devlin MJ. Close reading and creative writing in clinical education: teaching attention, representation, and affiliation. Acad Med 2016; 91: 345–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DasGupta S, Charon R. Personal illness narratives: using reflective writing to teach empathy. Acad Med 2004; 79: 351–356. [DOI] [PubMed] [Google Scholar]
- 37.Tsai SL, Ho MJ. Can narrative medicine training improve OSCE performance? Med Educ 2012; 46: 1112–1113. [DOI] [PubMed] [Google Scholar]
- 38.Miller E, Balmer D, Hermann N, et al. Sounding narrative medicine: studying students’ professional identity development at Columbia University College of Physicians and Surgeons. Acad Med 2014; 89: 335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lu M, Ruan H, Xing W, et al. Nurse burnout in China: a questionnaire survey on staffing, job satisfaction, and quality of care. J Nurs Manag 2015; 23: 440–447. [DOI] [PubMed] [Google Scholar]
- 40.Mercer SW, Maxwell M, Heaney D, et al. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract 2004; 21: 699–705. [DOI] [PubMed] [Google Scholar]