Short abstract
Objectives
This study was performed to explore the mechanism of proximal fibular osteotomy (PFO) for treatment of medial compartment knee osteoarthritis (OA) and evaluate the relevant factors influencing the treatment outcome.
Methods
Fifty-two patients with medial compartment knee OA with varus deformities were prospectively selected. Radiographs were obtained preoperatively and postoperatively. Knee function and OA severity were evaluated using the Hospital for Special Surgery (HSS) knee score and the Kellgren–Lawrence (KL) score. Multivariable linear regression models were used to examine associations between increases in the HSS score and selected factors influencing knee OA.
Results
Sixty-seven knee joints of 45 patients undergoing PFO were included. The HSS scores were significantly better at the final follow-up than preoperatively. Regression analysis identified five factors influencing changes in the HSS score: the change in the vertical distance between the fibular head and tibial plateau, the KL score for tibiofibular joint arthritis, the body mass index, the inclination of the tibiofibular joint, and the preoperative HSS score.
Conclusions
PFO is a simple and effective procedure for medial compartment knee OA. Greater distal displacement of the fibular head suggests greater range of motion of the tibiofibular joint and more evident improvement of postoperative OA symptoms.
Keywords: Knee osteoarthritis, proximal fibular osteotomy, tibiofibular joint, mechanism, Hospital for Special Surgery knee score, Kellgren–Lawrence score
Introduction
Knee osteoarthritis (OA) is a common chronic, progressive, degenerative disease in older individuals. Knee varus deformities characterized by a mechanical femorotibial axis of <180° on full-leg standing anteroposterior radiographs and a narrowed medial joint space are common in patients with knee OA and affect 74% of patients with idiopathic OA.1
High tibial osteotomy is a commonly accepted method for the treatment of knee varus deformities resulting from medial femorotibial OA in young and active patients. After high tibial osteotomy in several studies, all patients returned to work with the same intensity, and most resumed their sporting activities.2,3 However, because this is a technically demanding procedure, complications are common and include nonunion, neurovascular injury, implant irritation, and infection.4
Additionally, we found that after removal of the proximal section of the fibula, patients with medial compartment knee OA showed greater improvement in lower extremity alignment, knee range of motion (ROM), and local pain at an early stage.5,6 Early rebalancing of the periarticular soft tissue and ligaments may play a significant role in symptom improvement. Therefore, we performed a prospective study to explore the mechanism and influencing factors of proximal fibular osteotomy (PFO) for the treatment of medial knee OA.
Materials and methods
This study obtained Institutional Review Board approval (No. Ke2014-004-1) and was conducted in accordance with the Helsinki Declaration. All patients agreed to participate in this study and provided written informed consent.
Study population
From March 2014 to May 2014, patients with OA in the medial compartment complicated with varus deformities of the knee were selected at the authors’ hospital. A clinician diagnosed OA according to the American College of Rheumatology criteria.7 The inclusion criteria were OA mainly involving the medial compartment of the knee joint (however, because some patients with combined mild patellofemoral arthritis and lateral compartment OA displayed medial compartment pain as a primary symptom, they were also included in the experimental study), medial compartment OA with a Kellgren–Lawrence (KL) score of >2 points, a knee joint with varus deformity and medial space narrowing, and provision of written informed consent to a surgical plan involving fibular osteotomy. The exclusion criteria were post-traumatic knee OA, inflammatory joint disease, or a history of previous operations or fractures. Patients who fit the inclusion criteria, for whom conservative management had failed, and who had radiographic evidence of significant varus of lower extremity alignment during weight loading were good candidates for fibulectomy.
Surgical procedure
Under epidural anesthesia, the patients were placed in the supine position with a lower limb tourniquet inflated. A 3- to 5-cm lateral incision was made at the proximal third of the fibula to avoid injury to the common fibular nerve and the tibial attachments of the soft tissue structures crossing the knee joint. The fascia was then incised parallel to the septum between the peroneus and soleus; the muscles were separated, and the fibula was exposed. A 2-cm section of the fibula was removed at the fibular neck 6 to 10 cm below the fibular head with an oscillating saw or a fretsaw. Following resection, the fibula ends were sealed with bone wax. After irrigation of the incision with a large volume of normal saline, the muscles, fascia, and skin were sutured separately. Postoperatively, the patients were ambulated as soon as pain could be tolerated. The patients were routinely ambulatory by the third postoperative day.
Follow-up and clinical evaluations
Anteroposterior and lateral radiographs of the knee joint and a full-length standing radiograph of both lower extremities were obtained preoperatively and at 3, 6, 12, 18, 24, and 36 months postoperatively. The severity of knee OA was evaluated using the KL score.8 Knee pain was assessed using a visual analog scale. The Hospital for Special Surgery (HSS) knee score and ROM of the knee joint were used to evaluate knee function in all patients at baseline and at each follow-up visit.
On the basis of age, sex, height, weight, HSS score, and all imaging data mentioned above, the following nine factors potentially related to the outcome of fibulectomy were measured: body mass index (BMI), preoperative and postoperative HSS scores and the difference between them, tibiofemoral arthritis KL score, tibiofibular arthritis KL score, preoperative and postoperative femorotibial angle (FTA) of the lower extremity and the difference between them, inclination of proximal tibiofibular articulation, distance from the level of the fibular osteotomy to the top of the fibular head, length of the resected fibular section, and preoperative and postoperative distance from the top of the fibular head to the tibial plateau and the difference between them.
Statistical analyses
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA). Continuous variables are expressed as mean ± standard deviation, and dichotomous variables are expressed as percentage. Repeated-measures analysis of variance was used to evaluate the presence of significant differences with regard to the values observed at different time points before and after surgery. An increased HSS score (score at 18 months postoperatively − preoperative score) served as the dependent variable, and the above evaluation indicators of experimental measurement served as independent variables. Univariate linear regression analysis was performed. Factors showing significant differences (P < 0.05) in the univariate analysis were further analyzed using a multiple linear regression model. A P value of <0.05 was considered statistically significant.
Results
Fifty-two patients (45 women and 7 men, mean age of 62.5 ± 6.7 years) with mainly medial compartment OA complicated with knee varus deformity were randomly selected from among all outpatients from March 2014 to May 2014. The mean BMI was 27.38 ± 4.24 kg/m2. Forty-five of these patients, representing a total of 67 lateral knee joints (35 right knees and 32 left knees), underwent PFO and were followed up for 36 months (during this time, 7 patients were lost to follow-up). The mean disease duration was 7.32 ± 4.51 years. None of the patients had received intra-articular injection or surgery within 6 months prior to enrollment in the study. The patients’ characteristics are shown in Table 1.
Table 1.
Patients’ characteristics
| Parameter | Values |
|---|---|
| Age, years | 62.5 ± 6.7 |
| Sex | |
| Female | 45 |
| Male | 7 |
| Body mass index, kg/m2 | 27.38 ± 4.24 |
| Disease duration, years | 7.32 ± 4.51 |
| Side | |
| Left | 32 |
| Right | 35 |
Data are presented as mean ± standard deviation or n.
After the surgery, 8 of the 67 affected limbs presented with symptoms of superficial peroneal nerve injury. In these limbs, the skin of the distal lateral calf and the dorsal foot exhibited varying degrees of numbness. Among the 8 limbs with apparent superficial peroneal nerve injury, the symptoms of nerve injury had disappeared in 6 limbs at the 12-month follow-up and in the remaining 2 limbs at the 18-month follow-up. One affected limb showed constrained dorsiflexion of the ipsilateral big toe after the surgery, with a muscle strength grade of 1; this was combined with lateral skin numbness of the ipsilateral leg. The big toe dorsiflexion function of this patient returned to normal 6 months later, and the muscle strength grade was 5.
Evaluation of surgical treatment
The HSS knee score, ROM, and visual analog scale score of the 67 affected limbs were collected preoperatively and at 6 weeks, 3 months, 6 months, 12 months, 18 months, 24 months, and 36 months postoperatively. Knee symptoms and function were significantly improved during the 36-month follow-up period (P < 0.001) (Table 2).
Table 2.
HSS knee score, ROM outcomes, and VAS scores at different time points
| HSS score | ROM of knee joint (°) | VAS score | |
|---|---|---|---|
| Preoperatively | 52.27 ± 11.27 | 80.52 ± 10.38 | 6.03 ± 1.45 |
| 6 weeks postoperatively | 71.43 ± 11.71* | 92.31 ± 13.91* | 3.17 ± 1.59* |
| 3 months postoperatively | 74.61 ± 12.95* | 97.99 ± 16.77* | 2.70 ± 1.55* |
| 6 months postoperatively | 76.25 ± 13.66* | 102.39 ± 19.68* | 2.55 ± 1.53* |
| 12 months postoperatively | 76.96 ± 13.76* | 106.57 ± 21.11* | 2.53 ± 1.48* |
| 18 months postoperatively | 77.25 ± 14.07* | 108.73 ± 22.82* | 2.48 ± 1.43* |
| 24 months postoperatively | 78.54 ± 15.01* | 112.91 ± 21.13* | 2.29 ± 1.69* |
| 36 months postoperatively | 78.63 ± 15.19* | 113.66 ± 21.33* | 2.22 ± 1.61* |
| P value | <0.001 | <0.001 | <0.001 |
Data are presented as mean ± standard deviation.
HSS, Hospital for Special Surgery; ROM, range of motion; VAS, visual analog scale.
*vs. preoperatively; P < 0.001.
Linear regression analyses
An increased HSS score at 18 months postoperatively served as the dependent variable, and 10 influencing factors served as independent variables. These 10 independent variables were BMI, preoperative HSS score, tibiofemoral arthritis KL score, tibiofibular arthritis KL score, inclination of the proximal tibiofibular articulation (intersection angle with the horizontal plane), preoperative FTA of the lower extremity, changes in the FTA of the lower extremity at 18 months postoperatively, changes in the vertical distance between the top of the fibular head and the tibial plateau, distance from the resected plane to the fibular head, and length of the resected fibula. Univariate linear regression analysis was performed; the results are shown in Table 3.
Table 3.
Results of univariate linear regression analysis and multivariate stepwise regression analysis of different factors
| Influencing factor | Univariate linear regression analysis |
Multivariate stepwise regression analysis |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | T | P | β (95% CI) | B | SE | t | P | β (95% CI) | |
| Body mass index* | −0.987 | 0.431 | −2.292 | 0.025 | −0.273 (−1.848, −0.127) | −0.651 | 0.299 | −2.176 | 0.033 | −0.180 (−1.249, −0.053) |
| Preoperative HSS score* | −0.644 | 0.145 | −4.431 | <0.001 | −0.482 (−0.935, −0.354) | −0.474 | 0.113 | −4.197 | <0.001 | −0.354 (−0.699, −0.248) |
| Tibiofemoral arthritis KL score | 2.649 | 2.448 | 1.082 | 0.283 | 0.133 (−2.240, 7.538) | – | – | – | – | – |
| Proximal tibiofibular arthritis KL score* | −7.086 | 1.867 | −3.795 | <0.001 | −0.426 (−10.815, −3.357) | −7.199 | 1.417 | −5.082 | <0.001 | −0.433 (−10.032, −4.366) |
| Inclination of proximal tibiofibular articulation* | 0.526 | 0.204 | 2.576 | 0.012 | 0.304 (0.118, 0.934) | 0.562 | 0.147 | 3.816 | <0.001 | 0.325 (0.267, 0.856) |
| Preoperative FTA of the lower extremity | −0.194 | 0.400 | −0.485 | 0.629 | −0.060 (−0.994, 0.605) | – | – | – | – | – |
| Changes in the FTA of the lower extremity at 18 months postoperatively | −0.442 | 0.767 | −0.576 | 0.567 | −0.071 (−1.973, 1.090) | – | – | – | – | – |
| Changes in the vertical distance between the top of the fibular head and the tibial plateau* | 23.493 | 7.355 | 3.194 | 0.002 | 0.368 (8.805, 38.181) | 15.198 | 5.364 | 2.833 | 0.006 | 0.238 (4.472, 25.923) |
| Distance between the resected plane and the fibular head | −0.473 | 0.979 | −0.484 | 0.630 | −0.060 (−2.428, 1.481) | – | – | – | – | – |
| Length of the resected fibula | −0.395 | 0.422 | −0.936 | 0.353 | −0.115 (−1.239, 0.448) | – | – | – | – | – |
*From the univariate linear regression analysis, the difference was statistically significant (P < 0.05); thus, the factor was included in the multivariate linear regression analysis. SE, standard error; CI, confidence interval; HSS, Hospital for Special Surgery; KL, Kellgren–Lawrence; FTA, femorotibial angle
Univariate linear regression analysis showed that 5 of the 10 assessed factors had a statistically significant relationship with the outcome of fibulectomy (P < 0.05) (Table 3): BMI, preoperative HSS score, proximal tibiofibular arthritis KL score, inclination of the proximal tibiofibular articulation (intersection angle with the horizontal plane), and change in the vertical distance between the top of the fibular head and the tibial plateau. These five factors were subsequently included in the multivariate linear regression analysis. This analysis resulted in values of R2 = 0.769, F = 17.613, and P = 0.0002, indicating that the sample data in the present study fit the linear regression model well. The regression equation was Y = 66.282 − (0.651 × BMI) − (0.474 × preoperative HSS score) − (7.199 × proximal tibiofibular arthritis KL score) + (0.562 × inclination of proximal tibiofibular articulation) + (15.198 × change in distance from the fibular head to the tibial plateau) (Table 3).
Discussion
The proximal tibiofibular joint (PTFJ), a sliding articular joint located between the lateral tibial condyle and the fibular head in the posterolateral corner of the knee, serves as the attachment for numerous tendons and ligaments that are integral to knee structure and function. As a micro-joint, the PTFJ can produce relative movement between the tibia and the fibula in any direction.9,10 When the fibula is taken as a whole, the ROM of the PTFJ is limited by the distal syndesmosis and the interosseous membrane. Even when the knee is flexed, the proximal tibiofibular articulation can be moved approximately 1 cm in both the anterior and posterior directions.11
Some authors have noted that the posterolateral structure of the knee plays an important role in the balance of the periarticular soft tissue.12 Most ligament insertions involve the fibular head; these insertions include those of the lateral collateral ligament, arcuate ligament, fabellofibular ligament, popliteofibular ligament, and popliteus tendon.13 LaPrade et al.14 reported that the above-mentioned structure helps to transmit the lateral tensile force generated by knee joints that are load-bearing to the fibular head, thus affecting forces on the proximal tibiofibular articulation and its activities.
In reviewing the musculature of the lower extremity, it is important to note that the flexor hallucis longus, extensor digitorum longus, peroneus longus, peroneus brevis, tibialis posterior, and soleus all contain some fibers originating from the proximal fibula.15 We believe that the soleus and peroneus longus are two of the strongest muscles in the above-mentioned list and that they may provide most of the tensile force on the proximal fibula.
After patients underwent partial PFO, the proximal fibula that remained was no longer subject to constraints from the distal fibula and the tibiofibular syndesmosis, increasing the relative ROM of the PTFJ. Muscles attached to the proximal fibula, such as the soleus and peroneus longus, pulled the fibular head in the distal direction, and the tensile force was simultaneously transmitted from the posterolateral structure that ended at the fibular head to the lateral femoral condyle. Therefore, the lateral knee joint space was narrowed to counteract knee varus deformities resulting from load bearing, thereby reducing the pressure on the medial compartment of the knee and relieving the patients’ medial knee pain.
According to the above principle and coupled with a measurement index of variables showing multiple linear correlations with a surgical outcome, the clinical significance was elucidated as follows.
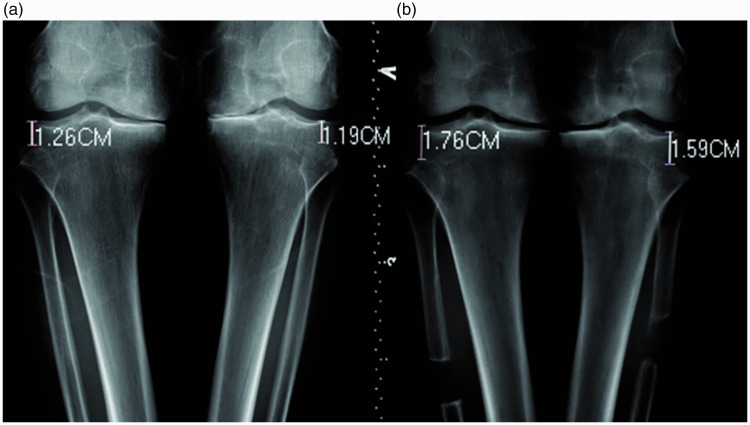
In patients with progressive knee OA and varus deformities, the posterolateral structure is pulled under a tensile force in response to a widened lateral space of the knee. The structure, including the lateral collateral ligament, will transmit the tensile force to the fibular head at the tendon insertion points. Therefore, during load-bearing activities of the knee joint such as standing and walking, knee varus imposes stress on the PTFJ.16 After the proximal section of the fibula was resected in the present study, the muscles attached to the proximal fibula produced tensile force transmitted by the fibular head to the lateral femoral condyle to counteract the knee varus. The greater the displacement of the fibular head as it was pulled distally, the more the varus deformities were corrected, the more evidently the medial compartment was decompressed, and the more significant the improvement that was observed in the postoperative results (Figure 1), showing a positive linear correlation (P < 0.05, regression coefficient = 15.198).
Figure 1.
(a) Preoperative weight-bearing anteroposterior radiographs of both affected knees revealed varus deformity and a narrow joint space in the medial compartment. (b) After partial fibular osteotomy, the vertical distance between the fibular head and the tibial plateau was larger, with a wider medial joint space and less varus deformity in weight-bearing anteroposterior radiographs.
Tibiofibular arthritis is the main factor limiting the relative activity of the tibiofibular joint. Eichenblat and Nathan16 found that medial compartment knee OA was statistically correlated with tibiofibular joint OA in a cadaver study. Oztuna et al.17 found that proximal oblique-type tibiofibular articulation was more vulnerable to joint degeneration and that its severity was closely related to the severity of tibiofemoral arthritis. Therefore, PTFJ arthritis should be carefully evaluated prior to the treatment of knee OA; the higher the OA score, the smaller the postoperative displacement that the fibular head produces in a distal direction and the smaller the improvement in the HSS score. In the present study, when tibiofibular arthritis progressed into stage IV (serious articular surface damage or even fusion), almost no distal displacement was observed in the proximal fibula after surgery. Additionally, a significant improvement in the HSS score was not observed; in fact, the HSS score may have even decreased. Thus, the tibiofibular arthritis score was negatively correlated with HSS improvement (P < 0.05, regression coefficient = −7.199).
Stickles et al.18 demonstrated that obesity is an adverse factor in OA treatment. Weight gain in patients with knee varus will increase the pressure applied to the knee medial compartment. After an osteotomy, the muscles of the proximal fibula need to produce a larger traction force to counteract knee varus deformities resulting from load bearing. Therefore, the BMI was negatively correlated with improvement in the postoperative results (P < 0.05, regression coefficient = −0.675).
Ogden11 classified tibiofibular joints into two types: horizontal (<20° joint inclination) and oblique (>20° joint inclination). Oblique-type joints are thought to be more prone to joint instability.19 Our data showed that an increase in the inclination angle of the tibiofibular joint resulted in an increased postoperative HSS score (P < 0.05, regression coefficient = 0.562). A larger inclination angle of the tibiofibular joint may lead to a relatively larger ROM; thus, postoperatively, the fibular head has more potential to move in a distal direction, which may assist the muscles attached to the proximal fibula in pulling the lateral femoral condyle to counteract knee varus deformity.
The severity of preoperative symptoms showed certain negative correlations with improvements in the curative effect (P < 0.05, regression coefficient = −0.474), although no obvious effect was observed in terms of improvement in postoperative symptoms. A better preoperative score was more likely to lead to a better curative effect, but the score did not improve significantly. The severe symptoms and lower HSS scores presumably led to greater functionality and improved scores, although these scores were not as high as the preoperative scores in patients with mild symptoms. These results are in agreement with previous reports.20
Close attention is needed to avoid potential peroneal nerve injury during surgery. In the present study, 8 of the 67 (11.94%) affected limbs showed superficial peroneal nerve injury, and 1 (1.49%) had common peroneal nerve injury. To reduce iatrogenic injury to the peroneal nerve, we recommend the posterolateral approach, which passes the space between the fibula longus muscle and the soleus muscle to expose the proximal fibula.
The limitations of this study include its lack of a control group and the possibility of bias due to the relatively small sample size. Further clinical trials and biomechanical studies are needed to validate the results.
Conclusions
The findings of this study suggest that PFO is a simple and effective procedure for the treatment of medial compartment knee OA. The surgical outcome of medial compartment OA depends on the severity of the tibiofibular joint OA and shows a linear correlation with the patient’s BMI, the inclination of proximal tibiofibular articulation, and preoperative knee function. In general, a greater distal displacement generated by the fibular head suggests better ROM of the tibiofibular joint and more obvious improvement in postoperative symptoms.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Shiozaki H, Koga Y, Omori G, et al. Epidemiology of osteoarthritis of the knee in a rural Japanese population. Knee 1999; 6: 183–188. DOI: 10.1016/S0968-0160(99)00011-3. [DOI] [Google Scholar]
- 2.Faschingbauer M, Nelitz M, Urlaub S, et al. Return to work and sporting activities after high tibial osteotomy. Int Orthop 2015; 39: 1527–1534. DOI: 10.1007/s00264-015-2701-2. [DOI] [PubMed] [Google Scholar]
- 3.Saragaglia D, Rouchy RC, Krayan A, et al. Return to sports after valgus osteotomy of the knee joint in patients with medial unicompartmental osteoarthritis. Int Orthop 2014; 38: 2109–2114. DOI: 10.1007/s00264-014-2435-6. [DOI] [PubMed] [Google Scholar]
- 4.Woodacre T, Ricketts M, Evans JT, et al. Complications associated with opening wedge high tibial osteotomy–A review of the literature and of 15 years of experience. Knee 2016; 23: 276–282. DOI: 10.1016/j.knee.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 5.Yang ZY, Chen W, Li CX, et al. Medial Compartment Decompression by Fibular Osteotomy to Treat Medial Compartment Knee Osteoarthritis: A Pilot Study. Orthopedics 2015; 38: e1110–1114. DOI: 10.3928/01477447-20151120-08. [DOI] [PubMed] [Google Scholar]
- 6.Wang X, Wei L, Lv Z, et al. Proximal fibular osteotomy: a new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J Int Med Res 2017; 45: 282–289. DOI: 10.1177/0300060516676630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association . Arthritis Rheum 1986; 29: 1039–1049. [DOI] [PubMed] [Google Scholar]
- 8.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957; 16: 494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scott J, Lee H, Barsoum W, et al. The effect of tibiofemoral loading on proximal tibiofibular joint motion. J Anat 2007; 211: 647–653. DOI: 10.1111/j.1469-7580.2007.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soavi R, Girolami M, Loreti I, et al. The mobility of the proximal tibio-fibular joint. A Roentgen Stereophotogrammetric Analysis on six cadaver specimens. Foot Ankle Int 2000; 21: 336–342. DOI: 10.1177/107110070002100411. [DOI] [PubMed] [Google Scholar]
- 11.Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 1974: 186–191. [PubMed] [Google Scholar]
- 12.Ferrari DA, Ferrari JD, Coumas J. Posterolateral instability of the knee. J Bone Joint Surg Br 1994; 76: 187–192. [PubMed] [Google Scholar]
- 13.Terry GC, LaPrade RF. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med 1996; 24: 732–739. DOI: 10.1177/036354659602400606. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade RF, Tso A, Wentorf FA. Force measurements on the fibular collateral ligament, popliteofibular ligament, and popliteus tendon to applied loads. Am J Sports Med 2004; 32: 1695–1701. DOI: 10.1177/0363546503262694. [DOI] [PubMed] [Google Scholar]
- 15.Kendall FP, Mccreary EK, Provance PG, et al. Muscles testing and function: with posture and pain. Philadelphia: Lippincott Williams and Wilkins, 2013. [Google Scholar]
- 16.Eichenblat M, Nathan H. The proximal tibio fibular joint. An anatomical study with clinical and pathological considerations. Int Orthop 1983; 7: 31–39. [DOI] [PubMed] [Google Scholar]
- 17.Oztuna V, Yildiz A, Ozer C, et al. Involvement of the proximal tibiofibular joint in osteoarthritis of the knee. Knee 2003; 10: 347–349. [DOI] [PubMed] [Google Scholar]
- 18.Stickles B, Phillips L, Brox WT, et al. Defining the relationship between obesity and total joint arthroplasty. Obes Res 2001; 9: 219–223. DOI: 10.1038/oby.2001.24. [DOI] [PubMed] [Google Scholar]
- 19.Boya H, Ozcan O, Oztekin HH. Radiological evaluation of the proximal tibiofibular joint in knees with severe primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2008; 16: 157–159. DOI: 10.1007/s00167-007-0442-5. [DOI] [PubMed] [Google Scholar]
- 20.Lim JT, Luscombe KL, Jones PW, et al. The effect of preoperative symptom severity on functional outcome of total knee replacement–patients with the lowest preoperative scores achieve the lowest marks. Knee 2006; 13: 216–219. DOI: 10.1016/j.knee.2006.01.006. [DOI] [PubMed] [Google Scholar]