Short abstract
Objective
This study was performed to determine the most common causes, locations, and treatments of metastasizing primary tumors through evaluation of patients with metastatic bone tumors who were admitted to our clinic.
Methods
In total, 96 patients with metastatic bone tumors who were admitted to our clinic from 2000 to 2016 were included in the study.
Results
The breast (30 patients, 31.3%) and lung (18 patients, 18.8%) were the most commonly metastasized primary organs. The femur was the most commonly metastasized bone.
Conclusions
Bone tumors in patients of advanced age are, unless otherwise proven, considered to be metastatic, and the development of specific diagnostic and treatment algorithms is needed. Clinicians should attempt to improve the general condition of patients with tumors exhibiting bone metastasis to increase the patients’ quality of life by providing early mobilization. Thus, appropriate patient selection and proper internal fixation are essential.
Keywords: Bone tumor, metastasis, pathological fracture, primary organs, bone localization, femur
Introduction
Skeletal metastases account for 70% to 80% of all malignant bone lesions.1 Skeletal metastases are more commonly found than primary bone tumors. Approximately one-third of each diagnosed extraskeletal carcinoma results in skeletal metastasis.2 Bone is one of the most commonly metastasized areas after the lungs and liver.3 Although the tumor generally spreads via hematogenous route, lymphatic and direct spread may also be observed.4 Although healthy bone shows equilibrium between osteoblastic bone formation and osteoclastic bone degradation, this equilibrium is disturbed when a tumor cell penetrates through the bony area.5
Diagnosis and treatment planning by a systemic approach reduces the failure rate in patients with skeletal metastasis.6 Whereas biopsy is generally diagnostic, the primary tumor may not be diagnosed despite performing a biopsy; the primary tumor is found in only 3% to 4% of patients diagnosed with bone metastasis.7 Although all types of cancer can metastasize to bone, most metastases arise from prostate, breast, lung, kidney, and thyroid cancers. In the present study, the primary causes and locations of metastatic bone tumors were investigated and compared with the literature. We believe that our study will contribute to the literature on the bone regions where pathologic fractures most frequently occur.
Materials and methods
All patients participating in the study provided written informed consent. After ethics committee approval was obtained from the Inonu University Committee on Scientific Research and Publication Ethics (approval no. 2017/1-5), the data of patients who were hospitalized due to a diagnosis of a metastatic bone tumor or whose treatment was planned in our clinic from 2000 to 2016 were evaluated. The most common causes of admission to our clinic due to metastatic bone lesions were pain and pathological fracture. Seventy-five patients underwent a surgical intervention with fixation, and the remaining patients were followed up with radiotherapy.
Statistical analysis
Statistical comparisons were performed using the paired-samples t-test and IBM SPSS Statistics, version 21 (IBM Corp., Armonk, NY, USA). Statistical significance was accepted at p < 0.05.
Results
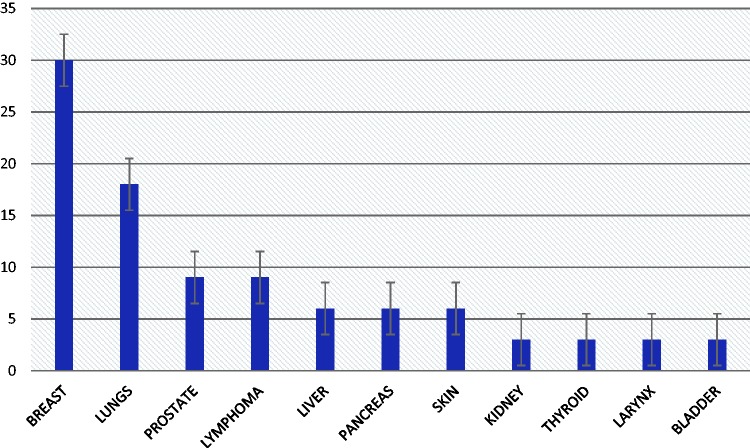
In total, 96 patients were included in this study (51 men, 45 women; mean age, 64.5 years; age range, 45–87 years). The primary tumors causing bone metastasis among the patients were located in the breast in 30 (31.3%) patients, lung in 18 (18.8%) patients, and prostate in 9 (9.4%) patients. The remaining patients had lymphoma, kidney, and liver tumor metastases (Figure 1). Breast cancer was the most frequently observed (p < 0.05).
Figure 1.
Localization of metastasizing primary tumors.
The locations of skeletal metastases were the femur in 51 (53.1%) patients, vertebrae in 21 (21.9%) patients, and humerus in 18 (18.8%) patients. Other patients had involvement of other skeletal areas such as the pelvis and tibia.
The most common causes of admission among our patients were pain and pathological fractures (Figure 2).
Figure 2.
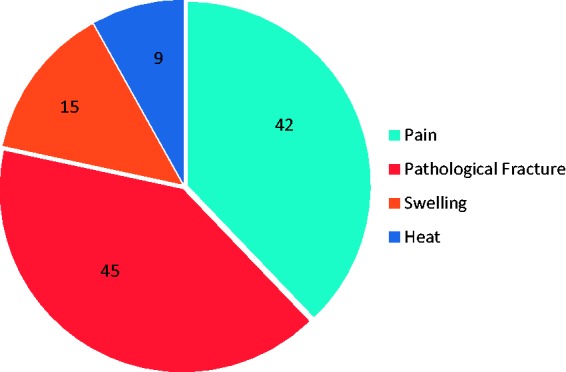
Symptoms on admission.
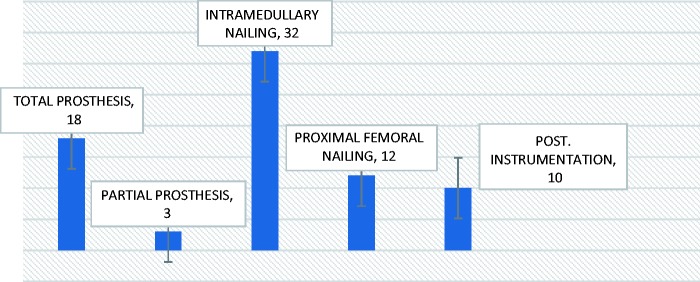
Prophylactic internal fixation and cementing were performed in 54 patients, and partial or total arthroplasty was performed for 21 patients. Only radiotherapy was administered for the remaining 21 patients who did not undergo surgery (Figure 3).
Figure 3.
Treatments administered.
Discussion
Bone is one of the most common sites of cancer metastasis in humans and is a significant source of morbidity and mortality. Bone metastases are considered incurable and result in pain, pathologic fracture, and decreased quality of life.8
Evaluation of a patient in whom a bone malignancy is suspected begins with an appropriate anamnesis and physical examination. This is followed by laboratory and imaging studies. The anamnesis should focus on the patient’s complaints and the course of the disease.9 Although patients with bone metastasis typically describe insidious pain, patients with pathological fractures report acute pain without trauma or following a minor trauma. The presence of previous symptoms at the site of the pathological fracture may be determined when the anamnesis of the patient is investigated thoroughly.10
Death in patients with cancer is often due to metastasis, and one of the most common sites is bone. The general pathogenesis of bone metastasis involves proliferation of the primary neoplasm, local tissue invasion, intravasation into blood vessels, extravasation into the bone marrow, a variable time of tumor cell dormancy, proliferation within bone, and modification of the bone microenvironment.8,11
The literature describes numerous established in vivo animal models of skeletal metastasis that vary by host animal, cancer type, and method of tumor injection.8,12
Advanced-stage cancers frequently metastasize to the bone, leading to skeletal morbidities such as bone destruction, bone pain, limitation of movement, pathological fractures, and spinal cord compression.13 Bone metastasis occurs most commonly as a result of breast cancer in women and of prostate and lung cancers in men. During the diagnostic phase, four radiological techniques are used in the clinical setting: radiography, computed tomography, nuclear imaging (technetium-99m-tagged bone scintigraphy and 18F-fluorodeoxyglucose positron emission tomography/computed tomography), and magnetic resonance imaging. In elderly patients, each bone tumor should be evaluated as a metastatic bone tumor unless proven otherwise.14,15
Skeletal metastases occur most commonly in the vertebrae, ribs, pelvis, and proximal femur and less commonly in the upper extremities and cranial bones.16 Various studies have revealed sites of metastatic involvement in the vertebrae (69%, most commonly in the anterior and middle columns), pelvis (41%), femur (25%), upper extremities (15%), and cranium (14%).16,17 In the present study, unlike in the literature, femoral involvement was more common (Table 1).
Table 1.
Localization within skeletal system.
| Bone/tissue involved | Patients (n) |
|---|---|
| Femur | 51 |
| Vertebrae | 21 |
| Humerus | 18 |
| Pelvis | 15 |
| Tibia | 3 |
| Soft tissue | 3 |
| Ribs | 6 |
A major complaint of patients with skeletal metastasis is pain, which is acute, does not resolve with rest, and rapidly intensifies. The fact that pain wakes patients from their sleep may be significant for metastatic bone disease.17,18 Approximately 25% of the lesions are painless and may be identified via bone and radiological screening.1,19 Consistent with the literature, the most common causes of admission among our patients were pain and pathological fractures.
The treatment options for bone metastases include radiotherapy, surgery, bisphosphonates, radionuclide therapy, and analgesics in addition the standard anticancer treatment. The major objective is to reduce pain, prevent the development of pathological fractures, improve mobility and function, improve quality of life, and extend the lifespan.19,20
According to the 12-score rating system for the risk of pathological fractures in long bones recommended by Mirels21 in 1989, fractures with a score of >8 are at high risk and require internal fixation, while radiotherapy is sufficient for lesions with a score of <7.
Surgery may be performed for patients who have developed a pathological fracture or have a risk of fracture development. A lytic lesion of >2.5 cm and/or cortical bone destruction of >50% indicates a risk of fracture.22,23 Surgery is performed if the life expectancy is >6 weeks, the patient is able to tolerate the surgery, the planned procedure is expected to make mobilization easier, and/or pain in lytic lesions of other weight-bearing bones persists despite a sufficient dose of radiotherapy.24 Seventy-five patients underwent operations in our study because their scores were ≥8 according to the criteria established by Mirels21; follow-up was recommended for the remaining 21 patients.
Prophylactic internal fixation performed after thorough evaluation of risk factors prevents pathological fractures and consequent loss of function.25 Internal fixation may be performed if the expected survival is >6 weeks, the patient’s general condition is suitable for surgery, mobilization is expected after internal fixation, the structure and quality of the bone both proximal and distal to the focal bone lesion can support the internal fixation, and/or pain persists despite ≥4 weeks of a sufficient dose of radiotherapy.26
Fixation methods include prophylactic intramedullary nailing and application of a prosthesis. Whereas prosthesis replacement surgeries are preferred in lesions that cause destruction of the articular surface, internal fixation is performed in combination with bone cement in diaphyseal and metaphyseal lesions of long tubular bones. Locked intramedullary nails are preferred in internal fixation. After wound healing is completed, radiotherapy may be required for local control of the tumor.27 Arthroplasty procedures may be needed in addition to internal fixation methods and were performed for the patients hospitalized in our clinic.
In conclusion, bone tumors in patients of advanced age are, unless proven otherwise, considered to be metastatic, and treatment should be planned according to this fact. In treatment of metastatic tumors, orthopedic surgical treatment is palliative and should be performed with the aim of relieving pain and enabling early mobilization and general medical care for the patient.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Azad GK, Taylor B, Rubello D, et al. Molecular and functional imaging of bone metastases in breast and prostate cancers: an overview. Clin Nucl Med 2016; 41: 44–50. [DOI] [PubMed] [Google Scholar]
- 2.Lan LS, Ping YJ, Na WL, et al. Down-regulation of toll-like receptor 4 gene expression by short interfering RNA attenuates bone cancer pain in a rat model. Mol Pain 2010; 6: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellido T, Plotkin LI. Novel actions of bisphosphonates in bone: preservation of osteoblast and osteocyte viability. Bone 2011; 49: 50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Body JJ. Bisphosphonates for malignancy-related bone disease: current status, future developments. Support Care Cancer 2006; 14: 408–418. [DOI] [PubMed] [Google Scholar]
- 5.Zhu YF, Ungart R, Seidtlitz E, et al. Differences in electrophysiological properties of functionally identified nociceptive sensory neurons in an animal model of cancer-induced bone pain. Mol Pain 2016; 1: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costa L. Bisphosphonates: reducing the risk of skeletal complications from bone metastasis. Breast 2007; 16: 16–20. [DOI] [PubMed] [Google Scholar]
- 7.Duo J, Han X, Zhang L, et al. Comparison of FDG PET/CT and gadolinium-enhanced MRI for the detection of bone metastases in patients with cancer: a meta-analysis. Clin Nucl Med 2013; 38: 343–348. [DOI] [PubMed] [Google Scholar]
- 8.Simmons JK, Hildreth BE, Supsavhad W, et al. Animal models of bone metastasis. Vet Pathol 2015; 52: 827–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sevimli R. Distribution and evaluation of primary bone and soft tissue tumors admitted from Malatya province and surrounding provinces. Med Sci 2017; 6:546–550. [Google Scholar]
- 10.Jeremic B, Shibamoto Y, Acimovic L, et al. A randomized trial of three single-dose radiation therapy regimens in the treatment of metastatic bone pain. Int J Radiat Oncol Biol Phys 1998; 42: 161–167. [DOI] [PubMed] [Google Scholar]
- 11.Gdowski AS, Ranjan A, Vishwanatha JK. Current concepts in bone metastasis, contemporary therapeutic strategies and ongoing clinical trials. J Exp Clin Cancer Res 2017; 36: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie HY, Shao ZM, Li DQ. Tumor microenvironment: driving forces and potential therapeutic targets for breast cancer metastasis. Chin J Cancer 2017; 36: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Estrada RS, Goodwin CR, Walls AR, et al. A model of metastatic bone cancer pain in the lumbar spine. Global Spine J 2017; 5: s-0035–1554446. [Google Scholar]
- 14.Ofluoglu O, Boriani S, Gasbarrini A, et al. Diagnosis and planning in the management of musculoskeletal tumors: surgical perspective. Semin Intervent Radiol 2010; 27: 185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qu X, Huang X, Yan W, et al. A meta-analysis of (18)FDG-PET-CT, (18)FDG-PET, MRI and bone scintigraphy for diagnosis of bone metastases in patients with lung cancer. Eur J Radiol 2011; 2: 25. [DOI] [PubMed] [Google Scholar]
- 16.Rougraff BT, Kneisl JS, Simon MA. Skeletal metastases of unknown origin. A prospective study of a diagnostic strategy. J Bone Joint Surg [Am] 1993; 75: 1276–1281. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal DI. Radiologic diagnosis of bone metastases. Cancer 1997; 80: 1595–1607. [DOI] [PubMed] [Google Scholar]
- 18.Shen CT, Qiu ZL, Han TT, et al. Performance of 18F-fluorie PET or PET/CT for the detection of bone metastases: a meta-analysis. Clin Nucl Med 2015; 40: 103–110. [DOI] [PubMed] [Google Scholar]
- 19.Tokuda O, Harada Y, Ohishi Y, et al. Investigation of computer-aided diagnosis system for bone scans: a retrospective analysis in 406 patients. Ann Nucl Med 2014; 28: 329–339. [DOI] [PubMed] [Google Scholar]
- 20.Wagner G. Frequency of pain in patients with cancer. Recent Results Cancer Res 1984; 89: 64–71. [DOI] [PubMed] [Google Scholar]
- 21.Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 1989; 249: 256–264. [PubMed] [Google Scholar]
- 22.Weinstein JN. Differential diagnosis and surgical treatment of pathologic spine fractures. Instr Course Lec 1992; 41: 301–315. [PubMed] [Google Scholar]
- 23.Yanagawa T, Shinozaki T, Iizuka Y, et al. Role of 2-deoxy-2-[F-18] fluoro-D-glucose positron emission tomography in the management of bone and soft-tissue metastases. J Bone Joint Surg [Br] 2010; 92: 419–423. [DOI] [PubMed] [Google Scholar]
- 24.Popper HH. Progression and metastasis of lung cancer. Cancer Metastasis Rev 2016; 35: 75–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Macedo F, Ladeira K, Pinho F, et al. Bone metastases: an overview. Oncol Rev 2017; 11: 321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koizumi M, Motegi K, Koyama M, et al. Diagnostic performance of a computer-assisted diagnosis system for bone scintigraphy of newly developed skeletal metastasis in prostate cancer patients: search for low-sensitivity subgroups. Ann Nucl Med 2017; 31: 521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Okabe H, Aoki K, Yogosawa S, et al. Downregulation of CD24 suppresses bone metastasis of lung cancer. Cancer Sci 2018; 109: 112–120. [DOI] [PMC free article] [PubMed] [Google Scholar]