Abstract
Background:
Chronic low back pain (CLBP) adversely affects quality of life (QOL) in nursing professionals. Integrated yoga has a positive impact on CLBP. Studies assessing the effects of yoga on CLBP in nursing population are lacking. Aim: This study was conducted to evaluate the effects of integrated yoga and physical exercises on QOL in nurses with CLBP.
Methods:
A total of 88 women nurses from a tertiary care hospital of South India were randomized into yoga group (n = 44; age – 31.45 ± 3.47 years) and physical exercise group (n = 44; age – 32.75 ± 3.71 years). Yoga group was intervened with integrated yoga therapy module practices, 1 h/day and 5 days a week for 6 weeks. Physical exercise group practiced a set of physical exercises for the same duration. All participants were assessed at baseline and after 6 weeks with the World Health Organization Quality of Life-brief (WHOQOL-BREF) questionnaire.
Results:
Data were analyzed by Paired-samples t-test and Independent-samples t-test for within- and between-group comparisons, respectively, using the Statistical Package for the Social Sciences (SPSS). Within-group analysis for QOL revealed a significant improvement in physical, psychological, and social domains (except environmental domain) in both groups. Between-group analysis showed a higher percentage of improvement in yoga as compared to exercise group except environmental domain.
Conclusions:
Integrated yoga was showed improvements in physical, psychological, and social health domains of QOL better than physical exercises among nursing professionals with CLBP. There is a need to incorporate yoga as lifestyle intervention for nursing professionals.
Keywords: Exercises, low back pain, nurses, quality of life, yoga
Introduction
Nursing profession is the largest chunk of health-care professionals.[1] Physical, psychological, and psychosocial challenges contribute to musculoskeletal disorders among nurses. Chronic low back pain (CLBP) is the most common musculoskeletal disorder among the nurses. It is reported that 63%–86% of nursing professionals suffer from LBP in their lifetime.[1,2] CLBP in nurses is multifactorial, and the risk factors pertain to lifestyle, physical, psychological, psychosocial, and occupational domains, namely, age, gender, physical status, smoking, workplace stress, awkward postures, poor ergonomics, carrying and repositioning of patients, prolonged standing, night shifts, working without sufficient breaks, and psychological stress are important causative/risk factors for CLBP in nurses. Nurses are required to lift and transport patients or equipment, often in difficult environment particularly in developing nations where lifting aids are not always available or practicable. These multiple factors contribute toward higher prevalence of CLBP in this population.[3] CLBP is one of the main concerns, which negatively impacts the quality of life (QOL) leading to reduced work productivity, absenteeism, and disabilities among nurses.[4] Harrington and Gill stated that LBP is the most common cause of early retirement on grounds of ill health, sickness absenteeism, job changes, and a fall in the work speed among the working population. Especially for young nurses, the mental demands of work have a critical influence on their QOL and workability.[5]
QOL measurements are being used increasingly relevant in the evaluation of disease progression, treatment, and the management of musculoskeletal disorders. QOL is recognized as a concept representing individual responses to the physical, mental, and social effects of illness on daily living, which influences the extent of personal satisfaction with life circumstances that can be achieved. Measuring QOL is recognized as an important add-on to objectify clinical effectiveness in recent clinical trials.[6,7] CLBP is a major deterrent for QOL, and the QOL scores correlate with pain and disability of CLBP. Furthermore, QOL correlated inversely with poor quality of sleep in nursing population. Such multifactorial problems of CLBP demand a multifaceted approach for management.[8,9,10]
Yoga has emerged as a popular mind-body therapy for CLBP as suggested by emerging scientific literature across the globe.[11] Yoga adopts a multifaceted approach utilizing practices at body (postures), breath (breathing techniques), and mind levels (meditation and relaxation techniques), respectively. According to national surveys, yoga practice and research have increased exponentially and in the last decade with over 10 million Americans practicing yoga for health reasons in 2002 and over 13 million in 2007.[11,12,13] Literature review reveals that viniyoga, hatha yoga, Iyengar yoga, and integrated yoga are the most commonly used forms to treat LBP.[14,15,16]
In a systematic review, Chou and Huffman concluded that there was a fair evidence reflecting efficacy of yoga therapy in subacute or CLBP.[17] In another similar review which included four randomized controlled trials (RCTs), it was observed that the intervention by Iyengar yoga and viniyoga for a period of 12–24 weeks was beneficial in CLBP.[15] Yet, another meta-analysis consisting of eight RCTs by Cramer et al. found strong evidence for short-term effectiveness (pain, back-specific disability, and global improvement parameters) and moderate evidences (back-specific disability) for long-term effectiveness of yoga on CLBP. Yoga was not found to be associated with serious adverse events.[18]
A study by Tekur et al. had observed usefulness of yoga intervention in improving QOL in patients with CLBP. However, this study was used in general population with intense residential yoga intervention. We did not come across any study that has assessed the same in nursing population with an OPD or outdoor setup intervention (1 h/day). As discussed earlier, nursing population is more prone for CLBP due to specific demands of the occupation.
Thus, the present randomized controlled study was planned to compare the effect of integrated yoga and physical exercise of similar intensity on QOL of nurses suffering from LBP.
Methods
Subjects
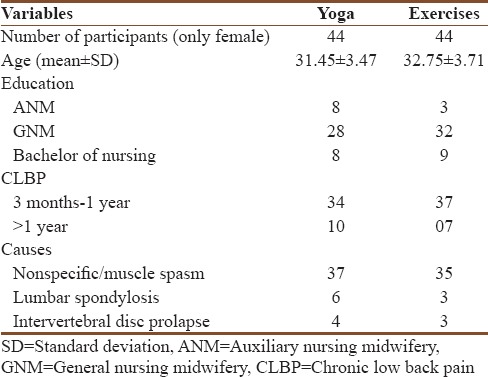
This study was conducted among nursing population, who were diagnosed by an orthopedician to be suffering from CLBP. Participants were working in the tertiary care teaching hospital in Kolar district of Karnataka state in India. They were randomly divided into two groups: yoga (n = 44; age – 31.45 ± 3.47 years) and physical exercise (n = 44; age – 32.75 ± 3.71 years) using random number generator (www.randomizer.org). Participants in the two groups did not differ much in relation to their age, education, or duration of illness between the groups as shown in Table 1.
Table 1.
Sociodemographic and clinical variables comparison between yoga and exercises
Two groups' randomized controlled single-blind design was followed with participants from both the groups (yoga and exercise) receiving intervention for 6 weeks. Assessments for QOL were performed at two points of time at baseline and after 6 weeks of interventions. The statistician and the interviewer were unaware of the allocation status of the participants.
The inclusion requirements were as follows: (a) female nurses with diagnosis of either nonspecific LBP, lumbar spondylosis, or intervertebral disc prolapse, suffering from LBP for 3 months or more as diagnosed by an orthopedician and (b) knowledge of English, Hindi, and Kannada language. The exclusion criteria were as follows: (a) pain due to organic causes such as infective and inflammatory conditions, metabolic disorders, and posttraumatic condition, (b) patients with degenerative disorders of muscles, (c) patients with comorbid cardiac or neuropsychiatric illness, (d) history of major surgery or injury in the past, (e) pregnant women, and (f) patients with neurological complications of CLBP.
Written informed consent was taken from all the participants before the study and Institutional Ethical Clearance was obtained.
Study profile
From January 2015 to December 2016, nurses were screened and referred by the orthopedician. Out of 176 nurses referred for the study, 88 satisfied the study criteria. Informed consent was obtained. Baseline assessments were done, and they were randomly allocated to yoga (n = 44) and control (n = 44) groups. They underwent intervention (either integrated yoga or physical exercise) for 6 weeks; repeat assessments were performed on both groups. There were no dropouts in the study. Figure 1 provides a flow diagram of the study profile.
Figure 1.
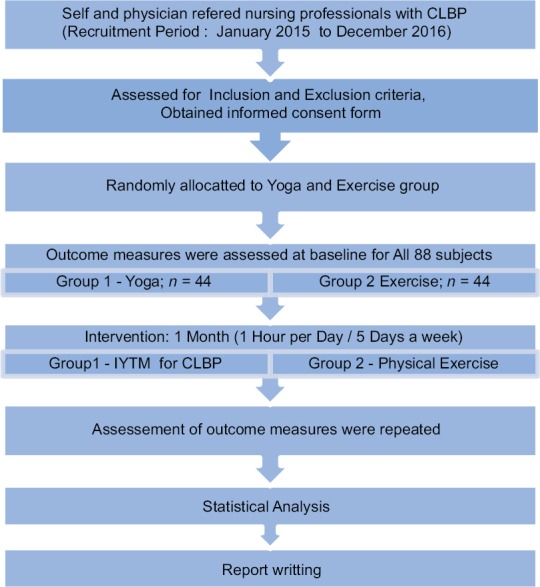
Trail profile
Materials
Assessment
The World Health Organization Quality of Life-brief (WHOQOL-BREF) questionnaire English and Kannada version was used to assess the QOL of the participants.
WHOQOL-BREF developed by the WHO is a standardized comprehensive instrument for assessment of QOL comprising 26 items. The scale provides a measure of an individual's perception of QOL on four domains: (1) physical health (seven items), (2) psychological health (six items), (3) social relationships (three items), and (4) environmental health (eight items). In addition, it also includes two questions for “overall QOL” and “general health” facets. The domain scores are scaled in a positive direction (i.e., higher scores denote higher QOL). The range of scores is 4–20 for each domain. The internal consistency of WHOQOL-BREF ranged from 0.66 to 0.87 (Cronbach's alpha coefficient). The scale has been found to have good discriminant validity. It has good test–retest reliability and is recommended for use in health surveys and to assess the efficacy of any intervention at suitable intervals according to the need of the study.[19,20]
Intervention
Integrated approach of yoga therapy (IAYT) is based on the basic principle that there are five layers of the existence to human beings, namely, Annamaya Kosa (physical level), Pranamaya Kosa (subtle energy level), Manomaya Kosa (emotional level), Vijnanamaya Kosa (level of intellect), and Anandamaya Kosa (level of bliss). Yogic pathophysiology propounds that the disturbances at the emotional level (adhi) percolate to the physical level (vyadhi) through the layer of prana. Furthermore, all layers are interrelated and they affect each other indirectly. The IAYT is an approach which consists in not only dealing with physical layer but also includes using techniques to operate on different layers of our existence. The practices at body level (Annamaya Kosa) include yogasanas, loosening practices, at subtle energy level (Pranamaya Kosa) include breathing practices and pranayama, and at the mind level (Manomaya Kosa) are meditations and relaxation techniques.
A 1-h integrated yoga therapy module (IYTM) was designed after reviewing the literature in the field of yoga and LBP by utilizing the components of yoga at the body, subtle energy, and mind level, respectively. The designed IYTM was validated by subject experts.[21] Tekur et al. used as a similar intervention in an earlier study.[22] This yoga module was practiced 5 days a week for 6 weeks. The details of yoga practice are provided in Table 2.
Table 2.
Intervention: Integrated yoga therapy module versus physical exercises
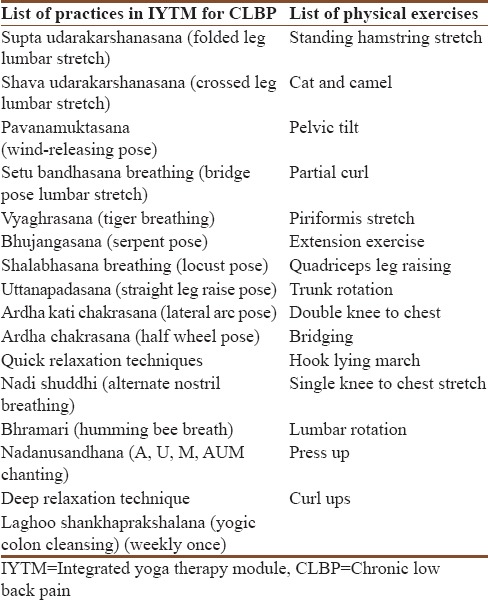
Control group intervention
Control group practiced physical exercise of similar intensity as IYTM for the same duration and frequency as shown in Table 2 provides the details of control intervention.
Data collection
Data were taken at the same time of the day on the 1st and 43rd day. Orientation to yoga program was given to the participants for 3 days, and then on the next day, predata collection was done after satisfactory performance. WHOQOL-BREF assessments were done on day 1 and day 43 (after 6 weeks). A trained psychologist assisted in data collection.
Data analysis
Statistical Package for the Social Sciences (SPSS) - (Version 21.0., Armonk, NY: IBM Corp.) was used for all analyses. Data of all four domains were normally distributed on Shapiro–Wilk test. Hence, the parametric tests were used. “Paired-samples t-test” and “Independent-samples t-test” were used to analyze within- and between-group data, respectively.
Results
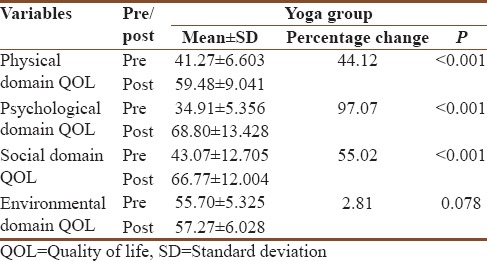
Within-group comparisons in yoga group
Within-group pre- and postcomparison showed that, after the yoga intervention, there was a significant improvement in three domains of WHOQOL-BREF, namely, physical (P < 0.01), psychological (P < 0.01), and social (P < 0.01) with a trend of insignificant positive impact in environmental domain (P = 0.07) [Table 3].
Table 3.
Within yoga group (pre and post) comparison of World Health Organization Quality of Life-BREF scores
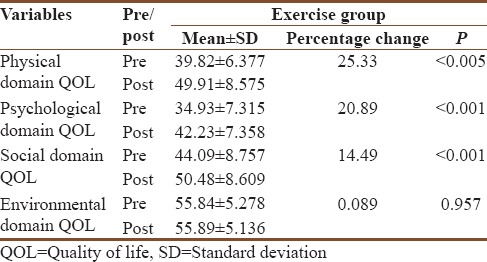
Within-group comparisons in exercise group
Similar to yoga group, exercise group also showed a significant improvement in three domains, namely, physical (P < 0.01), psychological (P < 0.01), and social (P < 0.01) with no significant difference in the environmental domain (P = 0.95) [Table 4].
Table 4.
Within exercise group (pre and post) comparison of World Health Organization Quality of Life-BREF scores
Between-group comparisons in yoga versus control group
Preintervention data
There was a no significant difference between the yoga and control groups at the baseline for all the four domains of WHOQOL-BREF: (a) physical (P = 0.296), (b) psychological (P = 0.987), (c) social (P = 0.661), and (d) environmental (P = 0.904) as shown in Table 5.
Table 5.
Between group (yoga vs. exercise) comparison of World Health Organization Quality of Life-BREF
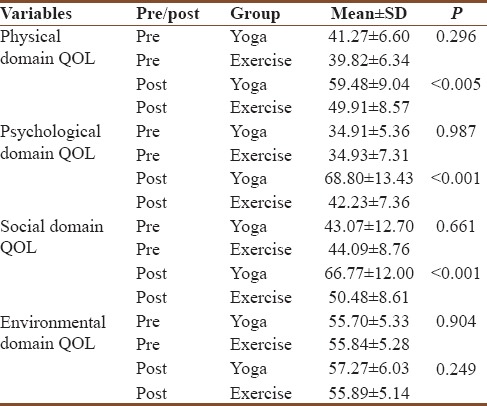
Postintervention data
There was a significant difference between the yoga and control groups after the intervention in the following domains of WHOQOL-BREF: (a) physical (P < 0.01), (b) psychological (P < 0.01), and (c) social (P < 0.01) with the scores of yoga group being higher than those of the control group for all the three domains, respectively. There was no significant difference between the groups for environmental domains(P = 0.249).
Discussion
At the end of 6 weeks of intervention as mentioned before, we observed that both the groups showed significant improvements in physical, psychological, and social domains of WHOQOL-BREF, whereas the environmental domain did not show significant improvements in either of the groups. As compared to the control group, patients who performed yoga reported significantly higher scores on the psychological domain (yoga – 97.7% and control – 20.89%). It was further observed that percentage improvement in physical and social domains was higher in the yoga group as compared to the exercise group (physical domain: yoga – 44.12% vs. control – 25.33%; and social domain: yoga – 55.02% vs. control – 14.49%).
Previously, Tekur et al.[22] demonstrated the usefulness of a 7 day intensive residential integrated yoga in improving QOL in 80 patients with CLBP in a highly controlled setting where patients were away from their occupational and other duties. They observed a significant improvement in all the four domains of WHOQOL-BREF in the yoga-based lifestyle module as compared to physical exercise-based lifestyle change module. One of the limitations with such trials is that they are not practical for working young nursing population and difficult to replicate such studies. In our study, we used 1-h yoga program which included all major components of yoga therapy, namely, asanas, pranayama, and relaxation. The exercise group also followed similar duration and frequency of intervention. We also observed improvement in physical, psychological, and social domains in both the groups but not in the environmental domain. The percentage improvements were higher in yoga group than the exercise group for physical, psychological, and social domains, respectively. This may be because the intervention offered by Tekur et al. was much more intensive than ours and the residential setup involved exposure to such an environment which was significantly different from the workplace. We performed this research in much more pragmatic setup and observed similar outcomes.
Underplaying mechanism of integrated yoga therapy module
The probable mechanism of action of yoga may be through improvement of autonomic functions through triggering neurohormonal mechanisms that suppress sympathetic activity through downregulation of the hypothalamic–pituitary–adrenal axis.[23] Mindfulness-based practices may also enhance cognitive flexibility, which may further reduce stress, anxiety, and pain, thereby improving QOL.[24] Furthermore, the cellular effects of mechanical and fluid pressure on structures such as cartilage suggest that yoga postures might alter joint function. Low levels of intermittent fluid pressure, as occur during joint distraction, have been shown in vitro to decrease production of catabolic cytokines, such as interleukin-1 and tumor necrosis factor.[25] Yoga may be one way to provide the motion and forces on joints needed to preserve integrity. In addition, pranayama, meditations, and relaxation techniques following yogasanas help to relax joints and muscles, reduce oxidative stress, and calm the mind.[26] This study implicates a probable role of integrated yoga therapy in the management of patients suffering from CLBP.
In a cross-sectional study on 501 nurses from different hospitals of Turkey, it was observed that there was a positive correlation between QOL as assessed by WHOQOL-BREF and job satisfaction (assessed using Short-Form Minnesota Questionnaire).[27] Similarly, another cross-sectional study on 435 female nurses from five regional centers in Taiwan revealed that associations between scores on the sleep-quality and QOL scales were statistically significantly inversely correlated.[28] Another survey on 1534 nursing professionals from eight different hospitals in Taiwan found that improved QOL of nurses translated into better workability (which may indirectly contribute to better health-care service delivery to the patients).[29] In the above study, it was also observed that mental demands of work were a critical influence on QOL and workability, especially in young nursing professionals. The authors further recommended countermeasures such as enhancing the ability to cope with the job's mental demands for improving and maintaining the workability of nurses.
Yoga may be considered one such intervention which has been found useful in enhancing the ability to cope with mental demands and thereby improve QOL and workability of nurses. An anonymous E-mail survey was conducted between April and June 2010 of North American nurses interested in mind-body training to reduce stress.[30] Of the 342 respondents, 96% were women and 92% were Caucasian. Most (73%) reported one or more health conditions, notably anxiety (49%), back pain (41%), gastrointestinal problems such as irritable bowel syndrome (34%), or depression (33%). Their median occupational stress level was 4 (0 = none and 5 = extreme stress). Nearly all (99%) reported already using one or more mind-body practices to reduce stress. The most common mind-body practices used by the nurses were as follows: intercessory prayer (86%), breath-focused meditation (49%), healing or therapeutic touch (39%), yoga/tai chi/qi gong (34%), or mindfulness-based meditation (18%). The greatest expected benefits were for greater spiritual well-being (56%); serenity, calm, or inner peace (54%); better mood (51%); more compassion (50%); or better sleep (42%).[30]
Physical domain of WHOQOL-BREF features such as mobility, fatigue, pain, sleep, and work capacity. The higher percentage of improvement in the yoga group compared to exercises therapy group can be credited to better reduction in pain and disability with improvement in spinal flexibility.[31]
Psychological domain features such as feelings, self-esteem, spirituality, thinking, learning, and memory. The higher percentage of improvement in the yoga group compared to exercises therapy group may be credited to better reduction in stress, anxiety, and depression.[31,32]
Social domain of WHOQOL-BREF features questions relating to problems in interpersonal relationships and social support. Yoga also acts like cognitive behavioral therapy; this may be the reason for the superior impact of yoga intervention compared to physical exercises in nurses with CLBP.
Environmental domain deals with problems relating to financial resources, physical safety, and physical environment such as pollution, noise, and climate. As working environment remained same throughout, this might have been the reason, we did not able to notice any significant changes in the environmental domain in both the groups.
Thus, yoga appears to be an integrated therapeutic tool and feasible intervention for improving QOL in nursing professionals compared to physical exercise as it offers holistic approach.
The strengths of the study are as follows: (a) this multidisciplinary study encompasses the fields of yogic science, orthopedics, and psychology; (b) a large sample of 88 CLBP patients were enrolled for the study with no dropouts, (c) no earlier study has reported effect of integrated yoga intervention on QOL of nurses suffering from CLBP; (d) because the study involved a pragmatic approach, the acceptability and adherence to therapy were good; and (e) as yoga and control program was delivered through a standard protocol, it could be reproduced in the exact way for future interventions.
This study has a few limitations, namely: this study was a preliminary attempt to assess the response of nursing population suffering from CLBP, and future studies should incorporate more objective variables such as electromyography, radio-imaging, biochemical measures, and other advanced objective variables of autonomic functions.
Conclusions
IYTM improves physical, psychological, and social health domains of QOL among nursing professionals with CLBP more than the physical exercises. There is a need to incorporate yoga as lifestyle intervention for nursing professionals with CLBP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are thankful for the management of Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, India, for their support throughout. We acknowledge the participants who gave their consent and participated in this study. We acknowledge Dr. Ananta Bhattacharyya, Dr. Balaram Pradhan, and Mr. Ravishankar S. for their support.
References
- 1.Bls.gov. Registered Nurses Have Highest Employment in Healthcare Occupations; Anesthesiologists Earn the Most: The Economics Daily: U.S. Bureau of Labor Statistics. 2018. [Last accessed on 2018 Feb 22]. Available from: https://www.bls.gov/opub/ted/2015/registered-nurses-have-highest-employment-in-healthcare-occupations-anesthesiologists-earn-the-mosthtm .
- 2.Genç A, Kahraman T, Göz E. The prevalence differences of musculoskeletal problems and related physical workload among hospital staff. J Back Musculoskelet Rehabil. 2016;29:541–7. doi: 10.3233/BMR-160655. [DOI] [PubMed] [Google Scholar]
- 3.Sikiru L, Hanifa S. Prevalence and risk factors of low back pain among nurses in a typical Nigerian hospital. Afr Health Sci. 2010;10:26–30. [PMC free article] [PubMed] [Google Scholar]
- 4.Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: Prevalence and associated risk factors among hospital staff. J Adv Nurs. 2009;65:516–24. doi: 10.1111/j.1365-2648.2008.04905.x. [DOI] [PubMed] [Google Scholar]
- 5.Moradi T, Maghaminejad F, Azizi-Fini I. Quality of working life of nurses and its related factors. Nurs Midwifery Stud. 2014;3:e19450. [PMC free article] [PubMed] [Google Scholar]
- 6.Kaplan RM. The significance of quality of life in health care. Qual Life Res. 2003;12(Suppl 1):3–16. doi: 10.1023/a:1023547632545. [DOI] [PubMed] [Google Scholar]
- 7.Baumstarck K, Boyer L, Boucekine M, Michel P, Pelletier J, Auquier P, et al. Measuring the quality of life in patients with multiple sclerosis in clinical practice: A necessary challenge. Mult Scler Int. 2013;2013:524894. doi: 10.1155/2013/524894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kovacs FM, Abraira V, Zamora J, Teresa Gil del Real M, Llobera J, Fernández C, et al. Correlation between pain, disability, and quality of life in patients with common low back pain. Spine (Phila Pa 1976) 2004;29:206–10. doi: 10.1097/01.BRS.0000107235.47465.08. [DOI] [PubMed] [Google Scholar]
- 9.Kovacs FM, Abraira V, Zamora J, Fernández C. Spanish Back Pain Research Network. The transition from acute to subacute and chronic low back pain: A study based on determinants of quality of life and prediction of chronic disability. Spine (Phila Pa 1976) 2005;30:1786–92. doi: 10.1097/01.brs.0000172159.47152.dc. [DOI] [PubMed] [Google Scholar]
- 10.Habibi E, Pourabdian S, Atabaki AK, Hoseini M. Evaluation of work-related psychosocial and ergonomics factors in relation to low back discomfort in emergency unit nurses. Int J Prev Med. 2012;3:564–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Cramer H, Lauche R, Dobos G. Characteristics of randomized controlled trials of yoga: A bibliometric analysis. BMC Complement Altern Med. 2014;14:328. doi: 10.1186/1472-6882-14-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shannahoff-Khalsa DS. Patient perspectives: Kundalini yoga meditation techniques for psycho-oncology and as potential therapies for cancer. Integr Cancer Ther. 2005;4:87–100. doi: 10.1177/1534735404273841. [DOI] [PubMed] [Google Scholar]
- 13.Moadel AB, Shah C, Wylie-Rosett J, Harris MS, Patel SR, Hall CB, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. J Clin Oncol. 2007;25:4387–95. doi: 10.1200/JCO.2006.06.6027. [DOI] [PubMed] [Google Scholar]
- 14.Verrastro G. Yoga as therapy: When is it helpful? J Fam Pract. 2014;63:E1–6. [PubMed] [Google Scholar]
- 15.Posadzki P, Ernst E. Yoga for low back pain: A systematic review of randomized clinical trials. Clin Rheumatol. 2011;30:1257–62. doi: 10.1007/s10067-011-1764-8. [DOI] [PubMed] [Google Scholar]
- 16.Tekur P, Singphow C, Nagendra HR, Raghuram N. Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med. 2008;14:637–44. doi: 10.1089/acm.2007.0815. [DOI] [PubMed] [Google Scholar]
- 17.Chou R, Huffman LH. American Pain Society, American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2007;147:492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. [DOI] [PubMed] [Google Scholar]
- 18.Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29:450–60. doi: 10.1097/AJP.0b013e31825e1492. [DOI] [PubMed] [Google Scholar]
- 19.Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 20.Skevington SM, Lotfy M, O'Connell KA. WHOQOL Group. The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 21.Patil NJ, Nagarathna R, Tekur P, Patil DN, Nagendra HR, Subramanya P, et al. Designing, validation, and feasibility of integrated yoga therapy module for chronic low back pain. Int J Yoga. 2015;8:103–8. doi: 10.4103/0973-6131.158470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tekur P, Chametcha S, Hongasandra RN, Raghuram N. Effect of yoga on quality of life of CLBP patients: A randomized control study. Int J Yoga. 2010;3:10–7. doi: 10.4103/0973-6131.66773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sengupta P. Health impacts of yoga and pranayama: A state-of-the-art review. Int J Prev Med. 2012;3:444–58. [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D, et al. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010;68:29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 25.van Valburg AA, van Roy HL, Lafeber FP, Bijlsma JW. Beneficial effects of intermittent fluid pressure of low physiological magnitude on cartilage and inflammation in osteoarthritis. An in vitro study. J Rheumatol. 1998;25:515–20. [PubMed] [Google Scholar]
- 26.Nagarathna R, Nagendra HR. Yoga for Back Pain. 1st ed. Bangalore: Swami Vivekananda Yoga Prakashan; 2008. pp. 31–85. [Google Scholar]
- 27.Cimete G, Gencalp NS, Keskin G. Quality of life and job satisfaction of nurses. J Nurs Care Qual. 2003;18:151–8. doi: 10.1097/00001786-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Shao MF, Chou YC, Yeh MY, Tzeng WC. Sleep quality and quality of life in female shift-working nurses. J Adv Nurs. 2010;66:1565–72. doi: 10.1111/j.1365-2648.2010.05300.x. [DOI] [PubMed] [Google Scholar]
- 29.Chiu MC, Wang MJ, Lu CW, Pan SM, Kumashiro M, Ilmarinen J, et al. Evaluating work ability and quality of life for clinical nurses in Taiwan. Nurs Outlook. 2007;55:318–26. doi: 10.1016/j.outlook.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 30.Kemper K, Bulla S, Krueger D, Ott MJ, McCool JA, Gardiner P, et al. Nurses' experiences, expectations, and preferences for mind-body practices to reduce stress. BMC Complement Altern Med. 2011;11:26. doi: 10.1186/1472-6882-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alexander GK, Rollins K, Walker D, Wong L, Pennings J. Yoga for self-care and burnout prevention among nurses. Workplace Health Saf. 2015;63:462–70. doi: 10.1177/2165079915596102. [DOI] [PubMed] [Google Scholar]
- 32.Botha E, Gwin T, Purpora C. The effectiveness of mindfulness based programs in reducing stress experienced by nurses in adult hospital settings: A systematic review of quantitative evidence protocol. JBI Database System Rev Implement Rep. 2015;13:21–9. doi: 10.11124/jbisrir-2015-2380. [DOI] [PubMed] [Google Scholar]


