Abstract
Despite a good outcome for many patients, approximately 20% of patients experience chronic pain after total knee arthroplasty (TKA).
Chronic pain after TKA can affect all dimensions of health-related quality of life, and is associated with functional limitations, pain-related distress, depression, poorer general health and social isolation.
In both clinical and research settings, the approach to assessing chronic pain after TKA needs to be in-depth and multidimensional to understand the characteristics and impact of this pain. Assessment of this pain has been inadequate in the past, but there are encouraging trends for increased use of validated patient-reported outcome measures.
Risk factors for chronic pain after TKA can be considered as those present before surgery, intraoperatively or in the acute postoperative period. Knowledge of risk factors is important to guide the development of interventions and to help to target care. Evaluations of preoperative interventions which optimize pain management and general health around the time of surgery are needed.
The causes of chronic pain after TKA are not yet fully understood, although research interest is growing and it is evident that this pain has a multifactorial aetiology, with a wide range of possible biological, surgical and psychosocial factors that can influence pain outcomes.
Treatment of chronic pain after TKA is challenging, and evaluation of combined treatments and individually targeted treatments matched to patient characteristics is advocated. To ensure that optimal care is provided to patients, the clinical- and cost-effectiveness of multidisciplinary and individualized interventions should be evaluated.
Cite this article: EFORT Open Rev 2018;3:461-470. DOI: 10.1302/2058-5241.3.180004
Keywords: total knee arthroplasty, chronic pain, epidemiology, impact, assessment, risk factors, aetiology, treatment
Introduction
The International Association for the Study of Pain (IASP) defines chronic pain as pain persisting for three months or longer.1 Chronic post-surgical pain is widely accepted to be pain of at least three to six months duration that develops or increases in intensity after a surgical procedure and significantly affects health-related quality of life.2,3 In 1998, a UK study found that surgery was the cause of chronic pain in 22.5% of patients attending pain clinics.4 Despite marked improvements in pain from many surgical procedures, chronic pain has become a recognized adverse consequence of any surgery,5 with an estimated prevalence of moderate–severe pain of 12% after diverse surgery types.6 However, advancements in prevention and treatment of this pain have been limited,7,8 and the need for further research to improve outcomes and care for patients has been acknowledged.9 To raise awareness about the burden of chronic post-surgical pain, 2017 was the International Association for the Study of Pain’s (IASP) ‘Global year against pain after surgery’. Chronic post-surgical pain will also be included as a recognized pain syndrome in the forthcoming 11th Revision of the International Classification of Diseases.10
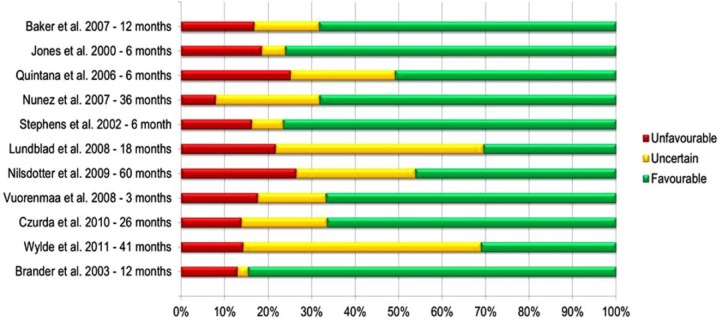
After total knee arthroplasty (TKA), pain severity plateaus at between three and six months after surgery,11,12 and therefore chronic pain after TKA is best defined as pain that is present and bothersome at least three to six months after surgery. While it is possible that pain outcomes can improve up to one year after surgery,13 people with persistent pain at three to six months can be disappointed with their outcome,14 and it may be possible to provide appropriate, targeted management in this early subacute phase, potentially halting progression into longer-term pain and disability.15 Despite a good outcome for many, a considerable proportion of patients have chronic pain after TKA. In a systematic review of prospective studies of patients undergoing TKA, 10% to 34% of patients reported unfavourable pain outcomes at between three months and five years after surgery16 (Fig. 1). In a high-quality study in multiple centres with low losses to follow-up, 20% of patients reported unfavourable pain outcomes at six months.17 More recent cohort studies have found similar results, with 16% to 33% of patients reporting chronic pain after TKA.18-21 This equates to a high number of patients experiencing this adverse outcome after surgery. For example, in the UK, nearly 100 000 primary TKA operations are performed annually22,23 and therefore there are potentially 20 000 patients who experience chronic pain after TKA every year. It is also possible that the true prevalence of chronic pain after TKA is even higher than estimated in research studies, as some patients may be reluctant to report that they have pain.24 Given that the need for TKA has been predicted to increase in the future, it is likely that the number of patients affected will continue to increase.25,26
Fig. 1.
Studies of total knee arthroplasty (TKA) reporting proportion of patients with pain at follow-up. Reproduced from Beswick et al,16 with permission from BMJ Publishing Group Ltd.
Prevention and treatment of chronic pain after TKA should be a research and clinical priority for several reasons. Orthopaedic surgery, which often focuses on the treatment of pain, has been found to be associated with an almost three-fold risk of moderate to severe chronic pain after surgery compared with other surgical procedures.6 Within orthopaedics, the prevalence of chronic pain after TKA is much higher than after total hip arthroplasty.16 Unlike many other types of surgery, TKA is an elective operation with the primary aim being pain relief. Surgeons often consider implant failure as the reason for revision surgery; however, the patient is likely to consider the operation as unsuccessful if they have a poor long-term pain outcome.27
This review summarizes the major advancements in understanding chronic pain after TKA to provide a comprehensive overview of the current state of understanding on this topic, including the epidemiology, impact, assessment, risk factors, aetiology and treatment.
Personal and economic impact
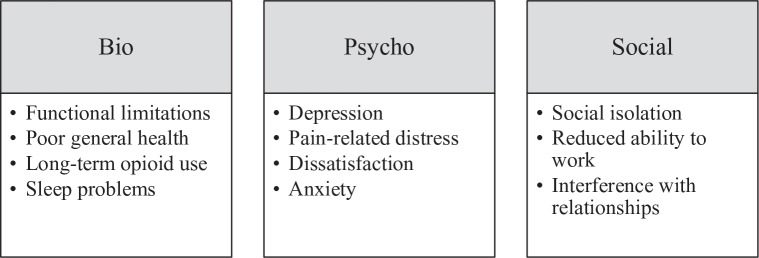
Chronic pain after TKA can affect all dimensions of health-related quality of life, and has been found to be associated with functional limitations, depression, anxiety, poorer general health, sleep problems and long-term opioid use.28 -32 Older people with chronic pain after joint arthroplasty can experience interference with relationships and become socially isolated, which is a risk factor for other problems and can limit their capacity to bring about change or to seek help for their pain.31,33,34 Some people experience considerable pain-related distress, and this is often highest in those who experience no change or deterioration in pain symptoms following surgery.35 Pain relief is the main expectation of patients undergoing TKA,36 and those who have continuing pain are often the most dissatisfied and disappointed with the outcome of their surgery.14,28,37 An overview of the biopsychosocial impact of chronic pain after TKA is provided in Figure 2.
Fig. 2.
Overview of the biopsychosocial impact of chronic pain after total knee arthroplasty (TKA).
Chronic pain management has been estimated to account for 4.6 million general practitioner appointments per year in the UK, at a cost of around £69 million.38 In England in 2005, there were over 66 million prescriptions for analgesic drugs, in addition to over-the-counter purchases, at a net ingredient cost of £510 million.39 European data show that national healthcare and socioeconomic costs of conditions associated with chronic pain represent 3% to 10% of gross domestic product, largely due to hospitalization.40 More specifically, the economic impact of chronic pain after TKA for individuals, healthcare services and society is largely unknown. The cost of investigations for patients presenting with a painful TKA was estimated to be approximately £5000 per patient in one orthopaedic centre in the United Kingdom.41 Approximately 7% of patients persistently use opioids in the first year after joint arthroplasty.42 Chronic knee pain is associated with reduced work productivity,43 suggesting that chronic pain after TKA could also impact on people’s ability to participate in paid employment. Further research is needed to evaluate the economic impact of chronic pain after TKA, as it is likely to be substantial given the costs associated with chronic pain.
Assessment
Pain as a subjective, lived and sensory experience presents particular challenges to assessment.44 In both clinical and research settings, the approach to assessing chronic pain after TKA needs to be in-depth and multidimensional to understand the characteristics and impact of this pain. There is useful guidance available about how to structure a comprehensive pain history for clinical use,44 and there are many questionnaires that enable assessment of pain in research.44 However, pain assessment may need to be tailored to the condition, and assessment of pain outcome after TKA is often inadequate.45 Historically, there has been a reliance on using surgeon-administered tools, such as the American Knee Society Score, which includes a single question on pain severity. Over time, there are encouraging recent trends for increased use of validated patient-reported outcome measures, which provide more robust and patient-centred assessments of pain.45 These include the Oxford Knee Score,46 Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)47 and Knee Injury and Osteoarthritis Outcome Score (KOOS).48 Some examples of patient-reported outcome measures that can be used to assess chronic pain after TKA are provided in Table 1. Although patient-reported outcome measures are the most appropriate way to produce a standardized assessment of pain, it is important to acknowledge that patients can experience difficulties with completing patient-reported outcome measures about chronic pain.49,50 For example, questions often ask for an average rating of pain over a specified time period, which can be challenging for patients as pain after TKA often fluctuates over time and varies with activity levels and medication use. Also, patients can find it difficult to conceptualize the pain in their replaced knee as distinct from pain elsewhere.
Table 1.
Examples of patient-reported outcome measures to assess chronic pain after total knee arthroplasty
| Questionnaire name | Number of questions | Description |
|---|---|---|
| Western Ontario and McMaster Universities Osteoarthritis Index pain scale47 | 5 | Disease-specific questionnaire assessing pain severity |
| Oxford Knee Score pain scale53 | 7 | Joint-specific questionnaire assessing pain severity and interference |
| Knee Injury and Osteoarthritis Outcome Score48 | 9 | Joint and disease-specific questionnaire assessing pain severity and frequency |
| Brief Pain Inventory Short-form54 | 11 | Generic questionnaire with a pain severity subscale (four items) and a pain interference subscale (seven items) |
| Short-Form McGill Pain questionnaire110 | 15 | Generic questionnaire assessing sensory and affective qualities of pain |
| Chronic Pain Grade111 | 7 | Generic questionnaire assessing pain intensity and pain-related disability |
| Pain visual analogue scale | 1 | Unidimensional assessment of pain severity |
| PainDETECT55 | 9 | Neuropathic pain questionnaire |
| Douleur Neuropathique 458 | 10 | Neuropathic pain questionnaire |
There have been a number of recent advances in pain assessment. One example is the move towards assessing pain as a separate domain from function, acknowledging that pain and function are distinct outcomes with different trajectories and predictors.51,52 A separate pain score can be calculated on many of the most commonly used orthopaedic patient-reported outcome measures, such as the WOMAC,47 Oxford Knee Score53 and the KOOS,48 and these can be used in conjunction with pain-specific assessment tools such as the Brief Pain Inventory54 and PainDETECT.55 Another example is the recognition that determination of pain character is important for informing treatment and management. Rest pain and pain-on-movement are distinct dimensions of pain, with different predictors and potential differences in underlying mechanisms, and it is important to assess these domains of pain separately.20,56 Pain can also be categorized as nociceptive or neuropathic, where the former arises from activity in neural pathways secondary to tissue damage and the latter arises from a lesion or disease of the somatosensory nervous system. Guidelines are available for the assessment of patients with neuropathic pain,57 and different neuropathic screening questionnaires and pain assessments tools have been developed, such as the PainDETECT55 and Douleur Neuropathique 4.58
There is considerable variation in the assessment of chronic pain after TKA,45 and recently a core outcome set has been developed to facilitate standardization.59 A core outcome set is an agreed standardized collection of outcomes which should be measured and reported, as a minimum, in all trials for a specific clinical area.60 Their purpose is to ensure that assessment is focused on outcomes important to key stakeholders and that assessment is standardized to facilitate synthesis of data. The core outcome set for chronic pain after TKA reflects the complex and multidimensional nature of pain, recommending that as a minimum the following aspects of pain should be assessed: pain intensity, pain interference with daily living, pain and physical functioning, temporal aspects of pain, pain description, emotional aspects of pain, use of pain medication and improvement and satisfaction with pain relief.59 Implementation of this core outcome set within research has the potential to facilitate a move towards improving the quality and consistency of pain assessment within orthopaedics.
Risk factors
Knowledge of risk factors for chronic pain after TKA is important to guide the development of interventions and help to target care. Interventions that address modifiable risk factors may improve post-surgical outcomes. Understanding of non-modifiable risk factors (e.g. sex, age) may help in the design of tailored care for specific patient groups. Risk factors can be considered as those present before surgery, intraoperatively or in the acute postoperative period and can be biological, psychosocial or surgical.61
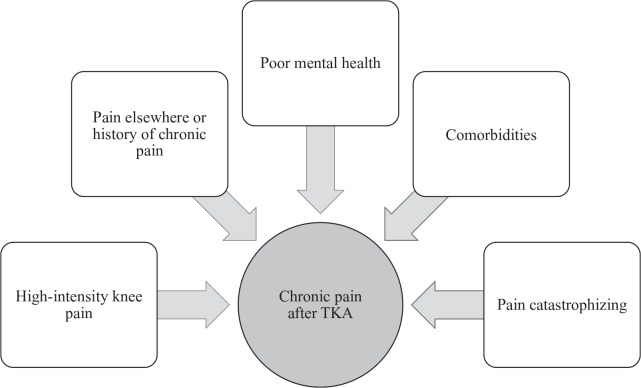
Associations between variables measured before TKA and long-term pain outcomes have been studied extensively.62,63 A systematic review and meta-analysis found that the strongest preoperative risk factors for chronic pain after TKA are preoperative pain severity, poor mental health, pain catastrophizing and presence of patient comorbidities62 (Fig. 3). Preoperative pain severity is one of the most studied risk factors, and there is strong evidence that more severe preoperative pain is associated with more severe postoperative pain.11,51,56,64,65 Chronic pain elsewhere in the body is also associated with long-term pain after surgery,66 suggesting that this pain may be due to an altered central modulation of pain, as part of a more generalized pain condition.67-69 Poor mental health, such as symptoms of depression and anxiety, is common in patients waiting for TKA70 and has been found to be predictive of a poorer long-term pain outcome after surgery.52,71-73 Pain catastrophizing, defined as an exaggerated negative orientation toward actual or anticipated pain experiences, has been identified as a strong risk factor for chronic pain after TKA in numerous studies,74,75 through influencing people’s response to and experience of pain. Multi-morbidity in patients undergoing TKA is common, with around 70% of patients having at least one comorbidity.63 A higher number of comorbidities has been found to be associated with more pain after TKA,62 although there is no strong evidence that any one specific comorbidity is a risk factor.63
Fig. 3.
Preoperative risk factors for chronic pain after total knee arthroplasty (TKA).
Despite the identification of preoperative risk factors, attempts to develop prediction models have had limited success. Multivariable models have had low predictive power, explaining < 20% of the variability in chronic pain severity,52,76,77 and studies have not yet evaluated the effectiveness of predictive models to guide treatment aimed at prevention.78 Because of this, no algorithm with high sensitivity and specificity has yet been developed to guide preoperative identification of patients at risk of chronic pain after TKA. The difficulty in prediction is probably due to the complex nature of this pain and potential interactions between multiple risk factors. We do not yet understand why there is discordance between radiographic knee osteoarthritis and pain severity,79 and future research to understand the variable relationship between pain and structural joint damage in osteoarthritis may help to elucidate chronic pain after TKA. It is clear, however, that any approach to targeting risk factors before surgery requires a personalized assessment using a biopsychosocial framework to understand an individual’s motivations, expectations and risk factors. Such a model would help inform patient and clinician decision-making about the most appropriate treatment plan. Evaluations of complex interventions that aim to optimize health and reduce risk factors in the perioperative period are needed.
An operation itself is an important risk factor for chronic pain,5 and therefore factors relating to the operation and early recovery may be of importance. Perioperative factors, such as type of surgery, implant type and surgery duration have been shown to have little influence on long-term pain outcomes.62 Post-surgical factors may be risk factors for chronic pain through limiting rehabilitation and recovery; however, a systematic review has found that there is insufficient evidence to draw firm conclusions about the association between postoperative factors and chronic pain after TKA.80 Although acute postoperative pain is often assumed to be associated with chronic pain, and is a strong risk factor for other surgical populations,6 there is little evidence to support this association in patients with TKA after controlling for preoperative pain severity.56,81 However, ongoing work to understand the transition of acute postoperative pain to chronic pain in a surgical setting may help to inform strategies to minimize suboptimal pain outcomes after TKA.61,82
In summary, while the potential value for identifying at-risk patients and targeting appropriate interventions is clear, further research on risk factors is needed. In the absence of robust predictive models, it is crucial that patients are aware of the potential risk of chronic pain after TKA so that their consent for surgery is fully informed.
Aetiology
The causes of chronic pain after TKA are not yet fully understood, although research interest is growing and it is evident that this pain has a multifactorial aetiology. The potential causes of chronic pain after TKA have been covered extensively in other reviews,83-89 and therefore only a brief overview of biological and surgical factors is provided in Table 2. Psychosocial factors may also negatively influence pain outcomes,90 and depression is commonly present in patients with chronic pain after TKA.28,29,91 Depression and poor social support has been associated with greater dissatisfaction in patients with chronic pain after TKA.28
Table 2.
Overview of biological and surgical factors contributing to chronic pain after total knee arthroplasty
| Factor | Examples |
|---|---|
| Biological 67,68,83-89,112 | Sensitizing impact of long-term pain from osteoarthritis Complex Regional Pain Syndrome Pain originating from the hip Patellofemoral pain Allergy-related problem Inflammatory response |
| Surgical 83-89 | Infection Localized nerve injury Prosthetic loosening Malalignment Malrotation Incorrect sizing Instability Stiffness |
There is consensus in the literature that revision surgery for chronic pain after TKA should not be performed unless the cause of pain is clearly identified as implant-related, as revision surgery for unexplained pain has consistently been shown to result in poor outcomes.91-93
Chronic pain after TKA is one of the biggest challenges that face people undergoing TKA and orthopaedic surgeons and health professionals who provide treatment. Given the wide range of possible biological, surgical and psychosocial factors that can influence pain outcomes, there is a clear need for a multidisciplinary approach.
Treatment and management
Chronic pain of all causes is undertreated,94 and many people lack adequate access to effective pain management.95 In England, the 2012 National Pain Audit96 reported considerable variation in access to specialist services for chronic pain and variation in levels of care. For example, 67% of services in England fell below minimum recommended levels of staffing with notable lack of provision of specialities including psychology and physiotherapy. In orthopaedics, there is national and international variation in the identification, assessment and management of patients with chronic pain after TKA, and service provision is often patchy and inconsistent.97 This is reflected in patients’ experiences, with some experiencing a sense of abandonment after surgery, and expressing a wish for easily accessible individualized advice and support that considered their pain in the context of their lives.35 Barriers to healthcare professionals providing healthcare to patients with chronic pain after TKA include complexities in assessment and management and a lack of explicit access points to services.98
There is a clear need to improve care for patients with chronic pain after TKA, and the benefits of this would be broad ranging, impacting upon patients, health services and society. For patients, better pain management reduces distress and increases quality of life, function, social participation and mental wellbeing.99 Early identification and targeted treatment of pain may ameliorate pain and prevent long-term disability.100 For health services, appropriate, targeted pain management may improve service efficiency and increase patient satisfaction. For society, improved outcome after TKA may increase participation in the workforce, often a reason for conducting TKA in the first instance.101
Despite the importance of effective pain management, there is a lack of evidence-based recommendations to guide clinical decisions around the optimal management of chronic pain after TKA. Pain management interventions for patients undergoing TKA have largely focused on perioperative pain control, rather than management of chronic pain.102 There is a scarcity of research which has sought to improve pain management in the long-term, particularly the months beyond surgery, a potentially valuable window when intervention may prevent longer-term pain and associated disability. A systematic review identified only one published randomized controlled trial evaluating a pharmacological intervention for the management of chronic pain after TKA,78 a single injection with antinociceptive and anticholinergic activity. No trials of multidisciplinary interventions or individualized treatments were identified. This is also a challenge faced by other surgical specialities, with a systematic review finding a lack of evidence on the effectiveness of interventions to manage chronic pain after diverse surgery types.7 Treatment of chronic pain is challenging, and evaluation of combined treatments and individually targeted treatments matched to patient characteristics is advocated.100 These are often referred to as complex interventions.
There is acknowledgement among orthopaedic healthcare professionals that a multidisciplinary approach with a focus on stratification is needed.84,98,103 Stratified care is a way of ensuring that resources are targeted towards those who are in most need and likely to benefit. It has been argued that we do not need new interventions for pain, and that what is needed is improved access to existing treatments with combination treatments matched to patient characteristics.100 For example, surgical or prosthesis-related problems may require physiotherapy, bracing or revision surgery. Nerve injury may respond to neuropathic pain medication, while nociceptive and regional pain may be treated with analgesic and opioid medication. Patients with chronic pain after TKA may also benefit from a broader pain management approach including psychological therapies. To facilitate this model of care, robust screening, evaluation and assessment processes are needed so that patients can receive targeted, possibly multi-modal, interventions.83,84 This model of care is being introduced in some surgical settings104 and a randomized controlled trial to evaluate a new multidisciplinary and individualized care pathway for patients with chronic pain after TKA105 is ongoing (ISRCTN92545361). In this trial, patients attend a one-hour assessment clinic with a trained Extended Scope Practitioner to identify potential causes of pain and are then referred to appropriate, existing services. In summary, management of chronic pain after TKA needs to take a comprehensive and multidisciplinary approach and may include pain management clinicians, physiotherapists, occupational therapists, psychologists, orthopaedic surgeons, microbiologists, radiologists and general practitioners. Involvement of patients’ family or significant others in postoperative management may help to improve outcomes after TKA.
An important potential barrier to providing effective pain management for patients is that not all people with chronic pain will present at services and seek help for their pain. A European survey of almost 6000 adults with musculoskeletal pain suggested that over a quarter had never sought medical help for their pain, despite many being in constant or daily pain.106 Research in the United Kingdom found that 75% of adults aged over 35 years experiencing hip or knee pain had not sought help from a general practitioner or allied health professional in the previous 12 months.107 Half of adults with severely disabling knee pain may not consult a general practitioner.108 Non-use of services is likely to be influenced by individual and social, structural and organizational factors. The average age of patients at TKA surgery is 70 years.22 Older people may perceive pain as a normal part of ageing and not present to healthcare centres.109 Given the high numbers of patients who are likely to have poor pain outcomes after surgery, there is potentially a large hidden population with unexpressed need for care, but who are experiencing ongoing pain and disability. Further research is needed to understand the reasons for non-use of services and to develop guidance to improve access and uptake of healthcare by patients who are living with chronic pain after TKA.
Conclusions
Chronic pain is a recognized adverse outcome after TKA. While research in this field has advanced over recent years, there are a number of key priorities for further research. To ensure that optimal care is provided to patients, the clinical and cost-effectiveness of multidisciplinary and individualized interventions should be evaluated. More work is needed to determine whether it is possible to develop a perioperative risk prediction tool so that patients at high risk of developing chronic pain after TKA can be identified and provided with targeted interventions. Parallel to this, there is a need to develop a better understanding of the complex aetiology of chronic pain after TKA. Research into the personal, societal and economic impact of chronic pain after TKA and its treatment is also required, as well as guidance on how to engage and help patients to access care.
Acknowledgments
This review article was informed by work undertaken as part of the Support and Treatment After Joint Replacement (STAR) Programme, a five-year programme of work to improve the postoperative prediction and management of chronic pain after total knee arthroplasty. As such, this article benefits from the input of the whole STAR team (https://www.bristol.ac.uk/translational-health-sciences/research/musculoskeletal/orthopaedic/research/star/).
Footnotes
ICMJE Conflict of interest statement: A. Blom declares grant funding from Stryker, activity outside the submitted work.
Funding statement
This article presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research programme (RP-PG-0613-20001). This article was also supported by the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- 1. International Association for the Study of Pain. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 1986;3:S1-226. [PubMed] [Google Scholar]
- 2. Macrae WA. Chronic pain after surgery. Br J Anaesth 2001;87:88-98. [DOI] [PubMed] [Google Scholar]
- 3. Werner MU, Kongsgaard UE. I. Defining persistent post-surgical pain: is an update required? Br J Anaesth 2014;113:1-4. [DOI] [PubMed] [Google Scholar]
- 4. Crombie IK, Davies HT, Macrae WA. Cut and thrust: antecedent surgery and trauma among patients attending a chronic pain clinic. Pain 1998;76:167-171. [PubMed] [Google Scholar]
- 5. Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth 2008;101:77-86. [DOI] [PubMed] [Google Scholar]
- 6. Fletcher D, Stamer UM, Pogatzki-Zahn E, et al. Chronic postsurgical pain in Europe: An observational study. Eur J Anaesthesiol 2015;32:725-734. [DOI] [PubMed] [Google Scholar]
- 7. Wylde V, Dennis J, Beswick AD, et al. Systematic review of management of chronic pain after surgery. Br J Surg 2017;104:1293-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bruce J, Quinlan J. Chronic Post Surgical Pain. Rev Pain 2011;5:23-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kalso E. IV. Persistent post-surgery pain: research agenda for mechanisms, prevention, and treatment. Br J Anaesth 2013;111:9-12. [DOI] [PubMed] [Google Scholar]
- 10. Treede RD, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain 2015;156:1003-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lenguerrand E, Wylde V, Gooberman-Hill R, et al. Trajectories of Pain and Function after Primary Hip and Knee Arthroplasty: The ADAPT Cohort Study. PLoS One 2016;11:e0149306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Halket A, Stratford PW, Kennedy DM, et al. Using hierarchical linear modeling to explore predictors of pain after total hip and knee arthroplasty as a consequence of osteoarthritis. J Arthroplasty 2010;25:254-262. [DOI] [PubMed] [Google Scholar]
- 13. Phillips JR, Hopwood B, Arthur C, et al. The natural history of pain and neuropathic pain after knee replacement: a prospective cohort study of the point prevalence of pain and neuropathic pain to a minimum three-year follow-up. Bone Joint J 2014;96-B:1227-1233. [DOI] [PubMed] [Google Scholar]
- 14. Scott CE, Howie CR, MacDonald D, et al. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg [Br] 2010;92-B:1253-1258. [DOI] [PubMed] [Google Scholar]
- 15. Shipton EA, Tait B. Flagging the pain: preventing the burden of chronic pain by identifying and treating risk factors in acute pain. Eur J Anaesthesiol 2005;22:405-412. [DOI] [PubMed] [Google Scholar]
- 16. Beswick AD, Wylde V, Gooberman-Hill R, et al. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2012;2:e000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jones CA, Voaklander DC, Johnston DWC, et al. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol 2000;27:1745-1752. [PubMed] [Google Scholar]
- 18. Petersen KK, Simonsen O, Laursen MB, et al. Chronic postoperative pain after primary and revision total knee arthroplasty. Clin J Pain 2015;31:1-6. [DOI] [PubMed] [Google Scholar]
- 19. Sugiyama Y, Iida H, Amaya F, et al. Prevalence of chronic postsurgical pain after thoracotomy and total knee arthroplasty: a retrospective multicenter study in Japan (Japanese Study Group of Subacute Postoperative Pain). J Anesth 2018;32:434-438. [DOI] [PubMed] [Google Scholar]
- 20. Noiseux NO, Callaghan JJ, Clark CR, et al. Preoperative predictors of pain following total knee arthroplasty. J Arthroplasty 2014;29:1383-1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. van der Wees PJ, Wammes JJ, Akkermans RP, et al. Patient-reported health outcomes after total hip and knee surgery in a Dutch University Hospital Setting: results of twenty years clinical registry. BMC Musculoskelet Disord 2017;18:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Joint Registry for England W, Northern Ireland and the Isle of Man. 14th Annual Report Hemel Hempstead, 2017. http://www.njrreports.org.uk/Portals/0/PDFdownloads/NJR%2014th%20Annual%20Report%202017.pdf (date last accessed 27 July 2018).
- 23. Scottish Arthroplasty Project. Biennial report, 2017. http://www.arthro.scot.nhs.uk/Reports/Main.html (date last accessed 24 July 2018).
- 24. Woolhead GM, Donovan JL, Dieppe PA. Outcomes of total knee replacement: a qualitative study. Rheumatology (Oxford) 2005;44:1032-1037. [DOI] [PubMed] [Google Scholar]
- 25. Culliford D, Maskell J, Judge A, et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage 2015;23:594-600. [DOI] [PubMed] [Google Scholar]
- 26. Inacio MCS, Paxton EW, Graves SE, et al. Projected increase in total knee arthroplasty in the United States - an alternative projection model. Osteoarthritis Cartilage 2017;25:1797-1803. [DOI] [PubMed] [Google Scholar]
- 27. Wylde V, Blom AW. The failure of survivorship. J Bone Joint Surg [Br] 2011;93-B:569-570. [DOI] [PubMed] [Google Scholar]
- 28. Howells N, Murray J, Wylde V, et al. Persistent pain after knee replacement: do factors associated with pain vary with degree of patient dissatisfaction? Osteoarthritis Cartilage 2016;24:2061-2068. [DOI] [PubMed] [Google Scholar]
- 29. Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: Prevalence, sensory qualities, and postoperative determinants. Pain 2011;152:566-572. [DOI] [PubMed] [Google Scholar]
- 30. Fuzier R, Serres I, Bourrel R, et al. Analgesic drug consumption increases after knee arthroplasty: a pharmacoepidemiological study investigating postoperative pain. Pain 2014;155:1339-1345. [DOI] [PubMed] [Google Scholar]
- 31. Pinto PR, McIntyre T, Ferrero R, et al. Persistent pain after total knee or hip arthroplasty: differential study of prevalence, nature, and impact. J Pain Res 2013;6:691-703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hassett AL, Marshall E, Bailey AM, et al. Changes in anxiety and depression are mediated by changes in pain severity in patients undergoing lower-extremity total joint arthroplasty. Reg Anesth Pain Med 2018;43:14-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Smith TO, Dainty JR, MacGregor AJ. Changes in social isolation and loneliness following total hip and knee arthroplasty: longitudinal analysis of the English Longitudinal Study of Ageing (ELSA) cohort. Osteoarthritis Cartilage 2017;25:1414-1419. [DOI] [PubMed] [Google Scholar]
- 34. Hawton A, Green C, Dickens AP, et al. The impact of social isolation on the health status and health-related quality of life of older people. Qual Life Res 2011;20:57-67. [DOI] [PubMed] [Google Scholar]
- 35. Jeffery AE, Wylde V, Blom AW, et al. ‘It's there and I'm stuck with it’: patients' experiences of chronic pain following total knee replacement surgery. Arthritis Care Res (Hoboken) 2011;63:286-292. [DOI] [PubMed] [Google Scholar]
- 36. Scott CE, Bugler KE, Clement ND, et al. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg [Br] 2012;94-B:974-981. [DOI] [PubMed] [Google Scholar]
- 37. Baker PN, van der Meulen JH, Lewsey J, et al. The role of pain and function in determining patient satisfaction after total knee replacement: Data from the National Joint Registry for England and Wales. J Bone Joint Surg [Br] 2007;89-B:893-900. [DOI] [PubMed] [Google Scholar]
- 38. Belsey J. Primary care workload in the management of chronic pain. A retrospective cohort study using a GP database to identify resource implications for UK primary care. J Med Economics 2002;5:39-50. [Google Scholar]
- 39. Phillips C. The economics of chronic pain. In: Wilson P, Watson P, Haythornthwaite J, et al. eds. Clinical pain management. 2nd ed. Boca Raton, Florida: CRC Press, Taylor & Francis Group, 2008:75-85. [Google Scholar]
- 40. Breivik H, Eisenberg E, O'Brien T, et al. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health 2013;13:1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kassam A, Dieppe P, Toms AD. An analysis of time and money spent on investigating painful Total Knee Replacements. B J Med Pract 2012;5:a526. [Google Scholar]
- 42. Kim SC, Choudhry N, Franklin JM, et al. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthritis Cartilage 2017;25:1399-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Agaliotis M, Fransen M, Bridgett L, et al. Risk factors associated with reduced work productivity among people with chronic knee pain. Osteoarthritis Cartilage 2013;21:1160-1169. [DOI] [PubMed] [Google Scholar]
- 44. Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth 2008;101:17-24. [DOI] [PubMed] [Google Scholar]
- 45. Wylde V, Bruce J, Beswick A, et al. The assessment of chronic post-surgical pain after knee replacement: A systematic review. Arthritis Care Res (Hoboken) 2014;65:1795-1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dawson J, Fitzpatrick R, Murray D, et al. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg [Br] 1998;80-B:63-69. [DOI] [PubMed] [Google Scholar]
- 47. Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833-1840. [PubMed] [Google Scholar]
- 48. Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS)-development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998;28:88-96. [DOI] [PubMed] [Google Scholar]
- 49. Wylde V, Jeffery A, Dieppe P, et al. The assessment of persistent pain after joint replacement. Osteoarthritis Cartilage 2012;20:102-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gooberman-Hill R, Woolhead G, MacKichan F, et al. Assessing chronic joint pain: Lessons from a focus group study. Arthritis Care Res (Hoboken) 2007;57:666-671. [DOI] [PubMed] [Google Scholar]
- 51. Judge A, Arden NK, Cooper C, et al. Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford) 2012;51:1804-1813. [DOI] [PubMed] [Google Scholar]
- 52. Lopez-Olivo MA, Landon GC, Siff SJ, et al. Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis 2011;70:1775-1781. [DOI] [PubMed] [Google Scholar]
- 53. Harris K, Dawson J, Doll H, et al. Can pain and function be distinguished in the Oxford Knee Score in a meaningful way? An exploratory and confirmatory factor analysis. Qual Life Res 2013;22:2561-2568. [DOI] [PubMed] [Google Scholar]
- 54. Cleeland C. The brief pain inventory: user guide, 2009. https://www.mdanderson.org/documents/Departments-and-Divisions/Symptom-Research/BPI_UserGuide.pdf (date last accessed 10 July 2018).
- 55. Freynhagen R, Baron R, Gockel U, et al. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 2006;22:1911-1920. [DOI] [PubMed] [Google Scholar]
- 56. Sayers A, Wylde V, Lenguerrand E, et al. Rest pain and movement-evoked pain as unique constructs in hip and knee replacements. Arthritis Care Res (Hoboken) 2016;68:237-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Haanpaa M, Attal N, Backonja M, et al. NeuPSIG guidelines on neuropathic pain assessment. Pain 2011;152:14-27. [DOI] [PubMed] [Google Scholar]
- 58. Bouhassira D, Attal N, Alchaar H, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005;114:29-36. [DOI] [PubMed] [Google Scholar]
- 59. Wylde V, MacKichan F, Bruce J, et al. Assessment of chronic post-surgical pain after knee replacement: development of a core outcome set. Eur J Pain 2015;19:611-620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Williamson PR, Altman DG, Bagley H, et al. The COMET Handbook: version 1.0. Trials 2017;18(Suppl 3):280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother 2009;9:723-744. [DOI] [PubMed] [Google Scholar]
- 62. Lewis GN, Rice DA, McNair PJ, et al. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2015;114:551-561. [DOI] [PubMed] [Google Scholar]
- 63. Blom AW, Artz N, Beswick AD, et al. Improving patients' experience and outcome of total joint replacement: the RESTORE programme. Southampton (UK): NIHR Journals Library, 2016. [PubMed] [Google Scholar]
- 64. Alattas SA, Smith T, Bhatti M, et al. Greater pre-operative anxiety, pain and poorer function predict a worse outcome of a total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:3403-3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Lindberg MF, Miaskowski C, RustoEn T, et al. Factors that can predict pain with walking, 12 months after total knee arthroplasty. Acta Orthop 2016;87:600-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Dave AJ, Selzer F, Losina E, et al. The association of pre-operative body pain diagram scores with pain outcomes following total knee arthroplasty. Osteoarthritis Cartilage 2017;25:667-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wylde V, Sayers A, Odutola A, et al. Central sensitization as a determinant of patients' benefit from total hip and knee replacement. Eur J Pain 2017;21:357-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Petersen KK, Arendt-Nielsen L, Simonsen O, et al. Presurgical assessment of temporal summation of pain predicts the development of chronic postoperative pain 12 months after total knee replacement. Pain 2015;156:55-61. [DOI] [PubMed] [Google Scholar]
- 69. Baert IA, Lluch E, Mulder T, et al. Does pre-surgical central modulation of pain influence outcome after total knee replacement? A systematic review. Osteoarthritis Cartilage 2016;24:213-223. [DOI] [PubMed] [Google Scholar]
- 70. Khatib Y, Jenkin D, Naylor JM, et al. Psychological traits in patients waiting for total knee arthroplasty. a cross-sectional study. J Arthroplasty 2016;31:1661-1666. [DOI] [PubMed] [Google Scholar]
- 71. Masselin-Dubois A, Attal N, Fletcher D, et al. Are psychological predictors of chronic postsurgical pain dependent on the surgical model? A comparison of total knee arthroplasty and breast surgery for cancer. J Pain 2013;14:854-864. [DOI] [PubMed] [Google Scholar]
- 72. Wylde V, Trela-Larsen L, Whitehouse MR, et al. Preoperative psychosocial risk factors for poor outcomes at 1 and 5 years after total knee replacement. Acta Orthop 2017;88:530-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Pinto PR, McIntyre T, Ferrero R, et al. Risk factors for moderate and severe persistent pain in patients undergoing total knee and hip arthroplasty: a prospective predictive study. PLoS One 2013;8:e73917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Burns LC, Ritvo SE, Ferguson MK, et al. Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: a systematic review. J Pain Res 2015;8:21-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Vissers MM, Bussmann JB, Verhaar JA, et al. Psychological factors affecting the outcome of total hip and knee arthroplasty: a systematic review. Semin Arthritis Rheum 2012;41:576-588. [DOI] [PubMed] [Google Scholar]
- 76. Judge A, Arden NK, Cooper C, et al. Predictors of outcomes of total knee replacement surgery. Rheumatology 2012;51(10):1804-13. [DOI] [PubMed] [Google Scholar]
- 77. Sanchez-Santos MT, Garriga C, Judge A, et al. Development and validation of a clinical prediction model for patient-reported pain and function after primary total knee replacement surgery. Sci Rep 2018;8:3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Beswick AD, Wylde V, Gooberman-Hill R. Interventions for the prediction and management of chronic postsurgical pain after total knee replacement: systematic review of randomised controlled trials. BMJ Open 2015;5:e007387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord 2008;9:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Wylde V, Beswick AD, Dennis J, et al. Post-operative patient-related risk factors for chronic pain after total knee replacement: a systematic review. BMJ Open 2017;7:e018105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Gilron I, Vandenkerkhof E, Katz J, et al. Evaluating the association between acute and chronic pain after surgery: impact of pain measurement methods. Clin J Pain 2017;33:588-594. [DOI] [PubMed] [Google Scholar]
- 82. Chapman CR, Vierck CJ. The transition of acute postoperative pain to chronic pain: an integrative overview of research on mechanisms. J Pain 2017;18:359,e1-59, e38. [DOI] [PubMed] [Google Scholar]
- 83. Mandalia V, Eyres K, Schranz P, et al. Evaluation of patients with a painful total knee replacement. J Bone Joint Surg [Br] 2008;90-B:265-271. [DOI] [PubMed] [Google Scholar]
- 84. Toms AD, Mandalia V, Haigh R, et al. The management of patients with painful total knee replacement. J Bone Joint Surg [Br] 2009;91-B:143-150. [DOI] [PubMed] [Google Scholar]
- 85. Hofmann S, Seitlinger G, Djahani O, et al. The painful knee after TKA: a diagnostic algorithm for failure analysis. Knee Surg Sports Traumatol Arthrosc 2011;19:1442-1452. [DOI] [PubMed] [Google Scholar]
- 86. Park CN, White PB, Meftah M, et al. Diagnostic algorithm for residual pain after total knee arthroplasty. Orthopedics 2016;39:e246-e52. [DOI] [PubMed] [Google Scholar]
- 87. Cottino U, Rosso F, Pastrone A, et al. Painful knee arthroplasty: current practice. Curr Rev Musculoskelet Med 2015;8:398-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Piscitelli P, Iolascon G, Innocenti M, et al. Painful prosthesis: approaching the patient with persistent pain following total hip and knee arthroplasty. Clin Cases Miner Bone Metab 2013;10:97-110. [PMC free article] [PubMed] [Google Scholar]
- 89. Preston S, Petrera M, Kim C, et al. Towards an understanding of the painful total knee: what is the role of patient biology? Curr Rev Musculoskelet Med 2016;9:388-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Turk DC, Okifuji A. Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol 2002;70:678-690. [DOI] [PubMed] [Google Scholar]
- 91. Phillips JR, Hopwood B, Stroud R, et al. The characterisation of unexplained pain after knee replacement. Br J Pain 2017;11:203-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Mont MA, Serna FK, Krackow KA, et al. Exploration of radiographically normal total knee replacements for unexplained pain. Clin Orthop Relat Res 1996;331:216-220. [DOI] [PubMed] [Google Scholar]
- 93. Elson DW, Brenkel IJ. A conservative approach is feasible in unexplained pain after knee replacement: a selected cohort study. J Bone Joint Surg [Br] 2007;89-B:1042-1045. [DOI] [PubMed] [Google Scholar]
- 94. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287-333. [DOI] [PubMed] [Google Scholar]
- 95. McGhie J, Grady K. Where now for UK chronic pain management services? Br J Anaesth 2016;116:159-162. [DOI] [PubMed] [Google Scholar]
- 96. No authors listed. The National Pain Audit Report 2012. https://data.england.nhs.uk/dataset/the-national-pain-audit (date last accessed 06 December 2017).
- 97. Wylde V, Mackichan Dixon S, et al. Service provision for patients with chronic post-surgical pain after total knee replacement: An evaluation of current practice. J Pain Manag 2014;7:147-154. [Google Scholar]
- 98. MacKichan F, Wylde V, Gooberman-Hill R. Pathways through care for long-term pain after knee replacement: a qualitative study with healthcare professionals. Musculoskeletal Care 2015;13:127-138. [DOI] [PubMed] [Google Scholar]
- 99. Schofield P. Pain in older adults: epidemiology, impact and barriers to management Reviews in Pain. London: British Pain Society, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Turk DC, Wilson HD, Cahana A. Treatment of chronic non-cancer pain. Lancet 2011;377:2226-2235. [DOI] [PubMed] [Google Scholar]
- 101. Bardgett M, Lally J, Malviya A, et al. Return to work after knee replacement: a qualitative study of patient experiences. BMJ Open 2016;6:e007912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Marques EM, Jones HE, Elvers KT, et al. Local anaesthetic infiltration for peri-operative pain control in total hip and knee replacement: systematic review and meta-analyses of short- and long-term effectiveness. BMC Musculoskelet Disord 2014;15:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Lavand'homme P, Thienpont E. Pain after total knee arthroplasty: a narrative review focusing on the stratification of patients at risk for persistent pain. Bone Joint J 2015;97-B(Suppl A):45-8. [DOI] [PubMed] [Google Scholar]
- 104. Katz J, Weinrib A, Fashler SR, et al. The Toronto General Hospital Transitional Pain Service: development and implementation of a multidisciplinary program to prevent chronic postsurgical pain. J Pain Res 2015;8:695-702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Wylde V, Bertram W, Beswick A, et al. Clinical and cost-effectiveness of the STAR care pathway compared to usual care for patients with chronic pain after total knee replacement: study protocol for a UK randomised controlled trial. Trials 2018;19:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Woolf AD, Zeidler H, Haglund U, et al. Musculoskeletal pain in Europe: its impact and a comparison of population and medical perceptions of treatment in eight European countries. Ann Rheum Dis 2004;63:342-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Thorstensson CA, Gooberman-Hill R, Adamson J, et al. Help-seeking behaviour among people living with chronic hip or knee pain in the community. BMC Musculoskelet Disord 2009;10:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Bedson J, Mottram S, Thomas E, et al. Knee pain and osteoarthritis in the general population: what influences patients to consult? Fam Pract 2007;24:443-453. [DOI] [PubMed] [Google Scholar]
- 109. Abdulla A, Adams N, Bone M, et al. Guidance on the management of pain in older people. Age Ageing 2013;42(Suppl 1):i1-57. [DOI] [PubMed] [Google Scholar]
- 110. Melzack R. The short-form McGill Pain Questionnaire. Pain 1987;30:191-197. [DOI] [PubMed] [Google Scholar]
- 111. Von Korff M, Ormel J, Keefe FJ, et al. Grading the severity of chronic pain. Pain 1992;50:133-149. [DOI] [PubMed] [Google Scholar]
- 112. van Bussel CM, Stronks DL, Huygen FJ. Complex regional pain syndrome type I of the knee: a systematic literature review. Eur J Pain 2014;18:766-773. [DOI] [PubMed] [Google Scholar]