Abstract
Background
The aim of this study was to compare the effect of 2 methods for treating toe-in gait in children (reverse-shoe wearing and orthopedic insoles) and to determine whether reverse-shoe wearing results in hallux valgus.
Material/Methods
Between July 2012 and July 2014, 337 children diagnosed with toe-in gait over 2 years were recruited. For 139 children, parents selected use of reverse-shoe wearing treatment (RS group) and for 198 children, parents selected orthopedic insoles treatment (OI group). There were 98 children in the RS group and 167 in the OI group who completed the 12-month therapy and follow-up. We excluded 28 children who failed to complete the study, and 44 children who ceased treatment within the first month were selected as controls. Patients were assessed for up to 24 months after the cessation of treatment. Foot progression angle (FPA) and presence and degree of hallux valgus angle (HVA) were recorded.
Results
FPA was significantly reduced after 6 months in both RS and OI groups (P<0.05). FPA returned to almost normal after 12 months of treatment, with no significant difference between the 2 groups. There were 29 cases (51 feet) of hallux valgus in the RS group after 12-month treatment; the HVA had significantly declined by 2 years after treatment with normal shoe wearing but did not return to normal.
Conclusions
Corrective treatment should be used with children diagnosed with toe-in gait over 2 years showing no remission. Both reverse-shoe wearing and orthopedic insoles show similar levels of treatment success, but reverse-shoe wearing has a significant adverse effect of hallux valgus.
MeSH Keywords: Child, Foot Orthoses, Hallux Valgus, Hallux Varus
Background
Toe-in gait is a condition commonly seen in pediatric orthopedic clinics [1–3], although it is rarely observed in children younger than 3 years of age [4–6]. Other than an abnormal toe-in gait pattern and occasional stumbling, there are generally no further clinical manifestations of the condition. Toe-in gait can be considered a normal developmental variation, which usually resolves with age and disappears by 3 years of age. Where present in children 3 years and older, a formal pediatric examination is recommended to observe skeletal growth and ensure the gait pattern is resolving. In refractory cases, intervention is advised. The traditional method for treating toe-in gait is the use of reverse-shoe wearing, which remains popular with both clinicians and parents. There is now a greater variety of orthotic devices available for treating this condition, including braces, gait plates, and wedges; however, the effectiveness of these different methods for improving gait pattern remains unclear [7–9]. The aim of this study was to compare the effect of reverse-shoe wearing and orthopedic insoles for treating toe-in gait and to measure the incidence of adverse effects.
Material and Methods
We examined 3755 children who presented to our clinic between July 2012 and July 2014 who were diagnosed as having toe-in gait according to foot progression angle. Cases due to the following conditions were excluded: nervous system disease (e.g., cerebral palsy), skeletal dysplasia (e.g., developmental dislocation of the hip), metabolic disease, and those having undergone lower-limb surgery [7,10,11]. We selected 337 children (153 males and 184 females) diagnosed as having bilateral toe-in gait, who were over 2 years of age and were not showing signs of significant improvement. This study was approved by the Ethics Committee at our institution. All parents or guardians were informed of the purpose of the study and full consent was obtained before inclusion. Parents were informed that 2 treatments were available – reverse-shoe wearing or orthopedic insoles – and allowed to select their preferred method. Reverse-shoe wearing (RS group) was chosen in 139 cases (73 males, 66 females; mean age 5.87 years) and 198 chose orthopedic insoles (OI group) (94 males, 104 females; mean age 5.91 years).
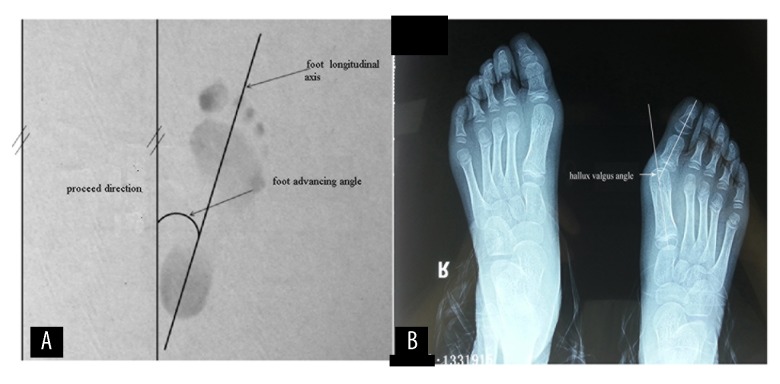
All of the patients were provided with a 1-year treatment, including some children who improved after 6 months of treatment. Patients were assessed at the orthopedic clinic by a local doctor in general practice every 6 months; foot progression angle and presence of and degree of hallux valgus angle were measured when walking barefoot (Figure 1A, 1B). Patients’ feelings were also recorded. Cases of hallux valgus were assessed over a further 24-month period following cessation of treatment. Foot progression angle was defined as the angle between the longitudinal axis of the foot and the direction of travel [12]. We measured the hallux valgus angle by radiographic work-up while weight-bearing, and the hallux valgus angle was defined as the angle between the longitudinal axis of the first metatarsal and first proximal phalanx. The diagnostic criterion used to assess the degree of hallux valgus was the presence of hallux valgus angle greater than 20° [13]. The foot progression angle and hallux valgus angle were recorded as mean ± the standard deviation (SD). A two-way t test was used to compare changes in foot progression and hallux valgus angles, and the recovery rate of the 2 groups was tested by the chi-square test; statistical significance was set as P≤0.05.
Figure 1.
Schematic diagram of foot progression angle (A) and hallux valgus angle (B), showing how these values are measured.
Families that did not attend follow-up were contacted by telephone to request attendance, and the reasons for not continuing with treatment were noted. Children who were treated for less than 1 month were selected as the control group, under the assumption that treatment would have had no significant effect on gait over such a short time period.
Results
Patient profile and compliance with treatment
The age distribution analysis of children diagnosed with toe-in gait is summarized in Figure 2. The incidence rate was 24% at 2 years and declined with age.
Figure 2.

Age distribution ratio of toe-in gait children presenting at clinic between July 2012 and July 2014, n=3755.
Compliance rates for full treatment over the study period were 70.5% (n=98) and 84.3% (n=167) for RS and OI, respectively. Failure to complete treatment was observed with 41 cases of RS and 31 cases of OI. Non-compliant patients were followed up by telephone to request further attendance at clinic, record treatment time, and analyze the reasons for not continuing with treatment. Of these, 51 patients were treated for less than 1 month, and only 44 cases completed the follow-up. Compared to the OI group, the RS group was more prone to prematurely terminating treatment (29.5% versus 15.6%, P<0.05). The main reason for failure to comply was foot discomfort (RS, 44%; OI, 35%). The second most common reason was stumbling and falling (RS, 34%; OI, 23%), resulting in upper-limb fracture in 3 children. The third most common reason was that some children disliked wearing reserve shoes (10%) or orthopedic insoles (19%), but without obvious discomfort. The fourth most common reason was that some parents thought that children felt unwell during the therapy process (RS, 12%; OI, 23%), even when this was accounted for by concurrent and unrelated conditions, such as upper-respiratory tract infections, and this resulted in failure to complete therapy. Figure 3 summarizes the overall treatment time and the reasons for poor compliance. Treatment duration was less than 1 month for 32 cases (23.0%) in the RS group and 19 cases (9.6%) in the OI group. The higher incidence rate in the RS group may be due to the fact that this treatment method was more likely to result in foot discomfort or pain.
Figure 3.
Reasons for treatment noncompliance in the reverse-shoes (RS) group (A) and orthopedic insoles (OI) group (B); duration of treatment received in these groups (C).
Efficacy of treatment
We used the cases that failed to continue with treatment after 1 month but returned to the clinic for assessment as the control group (n=44). To determine treatment efficacy, we measured the foot progression angle at 6 and 12 months (Table 1) and calculated the recovery rate, where recovery was defined as the foot progression angle becoming positive (Table 2). These results show that after 6 months, the foot progression angle of the control group had a small range of return, but only 7 cases recovered to normal, whereas a significant reduction in the progression angle after 6 months was seen in both the RS and OI groups (P<0.05). After 6 months of treatment, the recovery rates were 65.31% and 40.12% in the left foot, and 60.20% and 41.32% in the right foot, for RS and OI groups, respectively. Recovery rates were higher after 12 months of treatment, with progression angle approaching 10o and a recovery rate of 89.8% and 88.62% in the left foot and 87.76% and 91.62% in the right foot for RS and OI groups, respectively. At 6 months, the RS group showed a greater response to treatment than the OI group, with higher recovery rates and improved progression angle (P<0.05). However, by 12 months, there was no significant difference in cure or progression angle between the 2 groups (P>0.05) (Figure 4). Progression angle did improve in the control group over time, but by 12 months, only 15 feet returned to within normal parameters.
Table 1.
The effect of treatment on foot progression for in-toed gait (mean ±SD).
| Children (case) | Age (years) | Pre-treatment FPA (degree) | 6 momths treatment FPA (degre) | 12 momths treatment FPA (degre) | P value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Left | Right | Left | Right | Left | Right | ||||
| Control group | 44 | 5.82 ±0.73 | −28.35 ±5.77 | −30.56 ±5.08 | −24.77 ±5.32 | −26.34 ±5.48 | −19.59 ±4.51 | −18.97 ±4.06 | P4>0.05 |
| P5<0.05 | |||||||||
| P6<0.05 | |||||||||
| RS group | 98 | 5.91 ±0.71 | −27.40 ±5.02 | −28.84 ±4.83 | 4.49 ±3.01 | 4.64 ±3.39 | 10.84 ±3.83 | 8.97 ±2.97 | P4<0.05 |
| P5<0.05 | |||||||||
| P6<0.05 | |||||||||
| OI group | 167 | 5.83 ±0.81 | −29.06 ±5.55 | −30.23 ±4.98 | −4.83 ±3.83 | −5.23 ±3.92 | 8.36 ±2.57 | 9.30 ±3.38 | P4<0.05 |
| P5<0.05 | |||||||||
| P6<0.05 | |||||||||
| P value | P1>0.05 | P1>0.05 | P1>0.05 | P1<0.05 | P1<0.05 | P1<0.05 | P1<0.05 | ||
| P2>0.05 | P2>0.05 | P2>0.05 | P2<0.05 | P2<0.05 | P2<0.05 | P2<0.05 | |||
| P3>0.05 | P3>0.05 | P3>0.05 | P3<0.05 | P3<0.05 | P3>0.05 | P3>0.05 | |||
RS – indicates reverse shoes; OI – orthopedic insoles; FPA – foot progression angle. P1 – RS group vs. control group; P2 – OI group vs. control group; P3 – RS group vs. OI group; P4 – pre-treatment vs. 6 months’ treatment; P5 – pre-treatment vs. 12 months’ treatment; P6–12 months’ treatment vs. 6 months’ treatment.
Table 2.
Recovery rate with the two treatment methods.
| Children (cases) | Recovery cases after 6 months (cases) | Recovery cases after 12 months (cases) | |||
|---|---|---|---|---|---|
| Left | Right | Left | Right | ||
| Control group | 44 | 4 | 3 | 7 | 8 |
| 9.09% | 6.82% | 15.91% | 18.18% | ||
| RS group | 98 | 64 | 59 | 88 | 86 |
| 65.31% | 60.20% | 89.80% | 87.76% | ||
| OI group | 167 | 67 | 69 | 148 | 153 |
| 40.12% | 41.32% | 88.62% | 91.62% | ||
| P value | P1<0.05 | P1<0.05 | P1<0.05 | P1<0.05 | |
| P2<0.05 | P2<0.05 | P2<0.05 | P2<0.05 | ||
| P3<0.05 | P3<0.05 | P3>0.05 | P3>0.05 | ||
RS– indicates reverse shoes; OI – orthopedic insoles. P1 – RS group vs. control group; P2 – OI group vs. control group; P3 – RS group vs. OI group.
Figure 4.

Recovery rate at 6 and 12 months in the 3 groups: control, reverse-shoe wearing (RS), and orthopedic insoles (OI).
Effect of treatment on hallux valgus incidence
We found that erythrodysesthesia in the first metatarsophalangeal joint always occurred in children in the RS group, resulting in mild hallux valgus. The hallux valgus incidence rate was significantly higher (P<0.05) in the RS group (51 feet, 29 patients) than in the OI group (3 feet, 2 patients) (Table 3), and the hallux valgus angle of the RS group was significantly greater than control and OI groups (Table 4; Figure 5). The 29 cases of hallux valgus in the RS group resolved with normal shoe wear over the following 2 years (Table 5; Figure 6), although the hallux valgus angle still remained greater than that observed in the control group.
Table 3.
Incidence rate of hallux valgus by treatment group after 12 months.
| Children (cases) | Hallux valgus (cases) | ||
|---|---|---|---|
| Left | Right | ||
| RS Group | 98 | 24 | 27 |
| 24.49% | 27.55% | ||
| OI group | 167 | 1 | 2 |
| 0.59% | 1.18% | ||
| P value | <0.05 | <0.05 | |
RS – indicates reverse shoes; OI – orthopedic insoles.
Table 4.
Comparison of hallux valgus angle by treatment group at 12 months (mean ±SD).
| Children (cases) | Hallux valgus (cases) | ||
|---|---|---|---|
| Left | Right | ||
| Control group | 44 | 7.63±3.01 | 7.91±3.29 |
| RS group | 98 | 16.45±4.34 | 17.79±5.12 |
| OI group | 167 | 8.11±3.18 | 7.85±3.17 |
| P value | P1<0.05 | P1<0.05 | |
| P2>0.05 | P2>0.05 | ||
| P3<0.05 | P3<0.05 | ||
RS – indicates reverse shoes; OI – orthopedic insoles.P1 – RS group vs. control group; P2 – OI group vs. control group; P3 – RS group vs. OI group.
Figure 5.

Hallux valgus angle at 12 months in the 3 groups – control, reverse-shoe wearing (RS) and orthopedic insoles (OI) treatment – shown by left and right foot.
Table 5.
Changes in hallux valgus angle in the RS group post-treatment with normal shoe wear (mean ±SD).
| 0 month | 6 months | 12 months | 18 months | 24 months | |
|---|---|---|---|---|---|
| Hallux valgus angle (left foot) | 27.82±3.34 | 24.38±4.19 | 21.94±3.03 | 20.73±3.71 | 18.58±3.89 |
| Hallux valgus angle (right foot) | 28.35±4.21 | 23.35±3.67 | 20.79±3.96 | 18.95±3.42 | 17.95±3.44 |
| P value (left) | >0.05 | <0.05 | <0.05 | <0.05 | |
| P value (right) | >0.05 | <0.05 | <0.05 | <0.05 |
Figure 6.

Hallux valgus angle after wearing normal shoes in the reverse-shoe wearing (RS) treatment group, where * indicates 12 months later, and there were significant decreases in the hallux valgus angle.
Discussion
Toe-in gait is very common among children under 3 years of age [5,14]. It is generally caused by metatarsal adduction, internal rotation of the tibia, or internal rotation of the femur. Rotation of the tibia is the most common cause [9,15–17]. The tibia can twist naturally by 13°–18° during growth, with rotation usually ceasing by 6 years [16,17]. Therefore, toe-in gait is a physiological condition that does not normally require special treatment. The age distribution analysis of children diagnosed at our hospital showed a higher incidence rate in children ages 1–3 years, which declined to 10% at 4 years, but then remained stable until age 10. This suggests that children with toe-in gait younger than 3 years can mostly self-heal, but older children require treatment, especially where there has been no improvement within 2 years of diagnosis.
In the 2 treatment groups, we found that the cure rate with reverse-shoe wearing was greater than with orthopedic insoles at 6 months, but by 12 months the 2 types of treatment showed no significant difference [11,18]. Overall, 5–6-year-old children with toe-in gait showed a 90% cure rate after 12 months with either of the 2 treatment methods, but the natural recovery rate remained low. The higher cure rate observed in the RS group at 6 months is probably due to the wider correction range exerted. In order to maintain stable walking with reverse-shoe wearing, external rotation of the tibia is required, which plays a positive role in correcting the gait. In contrast, orthopedic insoles restrict the toe-off pattern: as the toes leave the ground, the orthopedic insole forces the foot to complete this action from the first metatarsal bone, then transfers this pressure onto the tibia, allowing a gradual gait correction. The more severe action of the reverse-shoes method is one of the reasons why children felt uncomfortable during treatment and were more likely to discontinue, with some cases of fractures occurring during treatment if the child was unable to adjust to using the shoes.
Although our results showed that by 12 months both methods showed equal recovery rates, the success of a treatment should not be measured purely by outcome, but also by adverse effects and compliance. The degree of comfort experienced by patients is a subjective feeling difficult to quantify and easily distorted by parental influence. We therefore did not carry out any statistical analysis of comfort in this study. However, we did observe that erythrodysesthesia in the first metatarsophalangeal joint always occurred in children in the RS group and we found that some of these children showed mild hallux valgus. A moderate-to-severe hallux valgus deformity leads to dysfunction of the great toe during walking and can induce pain or even require surgery [19–21], especially in adult women, and is exacerbated by wearing fashion footwear, such as winkle-picker and high-heel shoes. Hallux valgus is uncommon in children, so we measured the hallux valgus angle of each child after 12 months of treatment. The incidence and angle of hallux valgus was greater in the RS than the OI group. By examining the insoles of these shoes, we found that the outline of the insoles was similar to the foot outline of hallux valgus children. As the toes of the foot are differing lengths, the first and sometimes second toes experienced valgus to obtain adequate space in the reverse-shoe wearing feet (Figure 7). This can have a serious effect on bone development. Although the 29 cases of hallux valgus in the RS group returned to normal within 2 years of wearing normal shoes, the hallux valgus angle was still larger than that in the control group. Therefore, the longer the therapy duration, the more serious the adverse effects may become.
Figure 7.
Schematic diagram of reverse-shoes and hallux valgus cases in this group. Reversing the shoe insoles shows foot outline is similar to actual foot (A); a child (female, 5 years old) with hallux valgus after 12 months of therapy (B); erythrodysesthesia in first metatarsophalangeal joint showing a hallux valgus angle greater than 20° (C).
Previous studies examining treatment efficacies on foot progression angle with toe-in gait have not used control groups [6–9] and therefore cannot exclude the possibility that the condition naturally self-resolves in some children. One advantage of our study is that we used children who failed to continue with treatment after 1 month as a control group; this allowed us to demonstrate that natural resolution rates for toe-in gait were significantly lower than those seen with treatment. However, a limitation of our study was that we chose foot progression angle to evaluate the efficacy of treatment for toe-in gait. Despite measuring the incidence and angle of hallux valgus, a more objective method for determining treatment success, such as a gait analyzer or foot stress analyzer, is required [21,22]. Stress distribution in the ankle, knee, and hip joints should be observed [16,18] and long-term follow-up is required to fully assess therapy success [23].
Conclusions
In conclusion, children with toe-in gait at 5–6 years of age benefit from active treatment and we found that the use of orthopedic insoles over a period of 12 months produced good results.
Footnotes
Source of support: Departmental sources
References
- 1.Rerucha CM, Dickison C, Baird DC. Lower extremity abnormalities in children. Am Fam Physician. 2017;96:226–33. [PubMed] [Google Scholar]
- 2.Evans AM. Mitigating clinician and community concerns about children’s flatfeet, intoeing gait, knock knees or bow legs. J Paediatr Child Health. 2017;53:1050–53. doi: 10.1111/jpc.13761. [DOI] [PubMed] [Google Scholar]
- 3.Faulks S, Brown K, Birch JG. Spectrum of diagnosis and disposition of patients referred to a pediatric orthopaedic center for a diagnosis of intoeing. J Pediatr Orthop. 2017;37:e432–35. doi: 10.1097/BPO.0000000000001007. [DOI] [PubMed] [Google Scholar]
- 4.Mooney JF., 3rd Lower extremity rotational and angular issues in children. Pediatr Clin North Am. 2014;61:1175–83. doi: 10.1016/j.pcl.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Sielatycki JA, Hennrikus WL, Swenson RD, et al. In-toeing is often a primary care orthopedic condition. J Pediatr. 2016;177:297–301. doi: 10.1016/j.jpeds.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 6.Nourai MH, Fadaei B, Rizi AM. In-toeing and out-toeing gait conservative treatment; hip anteversion and retroversion: 10-year follow-up. J Res Med Sci. 2015;20:1084–87. doi: 10.4103/1735-1995.172833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mabuchi A, Kitoh H, Inoue M, et al. The biomechanical effect of the sensomotor insole on a pediatric intoeing gait. ISRN Orthop. 2012;2012 doi: 10.5402/2012/396718. 396718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganjehie S, Saeedi H, Farahmand B, et al. The efficiency of gait plate insole for children with in-toeing gait due to femoral antetorsion. Prosthet Orthot Int. 2017;41:51–57. doi: 10.1177/0309364616631349. [DOI] [PubMed] [Google Scholar]
- 9.Ahn JK, Kwon DR, Park GY, et al. Therapeutic effect of microcurrent therapy in children with in-toeing gait caused by increased femoral anteversion: A pilot study. Ann Rehabil Med. 2017;41:104–12. doi: 10.5535/arm.2017.41.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byun HY, Shin H, Lee ES, et al. The Availability of Radiological Measurement of Femoral Anteversion Angle: Three-Dimensional Computed Tomography Reconstruction. Ann |Rehabil Med. 2016;40:237–43. doi: 10.5535/arm.2016.40.2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Sullivan R, Kiernan D, Walsh M, et al. The difficulty identifying intoeing gait in cerebral palsy. Irish Med J. 2013;106:144–45. [PubMed] [Google Scholar]
- 12.Bohne WH, Root L. Hypoplasia of the fibula. Clin Orthop Relat Res. 1977:107–12. [PubMed] [Google Scholar]
- 13.Gicquel T, Fraisse B, Marleix S, et al. Percutaneous hallux valgus surgery in children: Short-term outcomes of 33 cases. Orthop Traumatol Surg Res. 2013;99:433–39. doi: 10.1016/j.otsr.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Thackeray C, Beeson P. In-toeing gait in children: A review of the literature. Foot. 1996;6:1–4. [Google Scholar]
- 15.Khan SS, Khan SJ, Usman J. Effects of toe-out and toe-in gait with varying walking speeds on knee joint mechanics and lower limb energetics. Gait Posture. 2017;53:185–92. doi: 10.1016/j.gaitpost.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 16.Presedo A, Simon AL, Mallet C, et al. Correlation between transverse plan kinematics and foot progression angle in children with spastic diplegia. J Pediatr Orthop B. 2017;26:211–16. doi: 10.1097/BPB.0000000000000416. [DOI] [PubMed] [Google Scholar]
- 17.Davids JR, Davis RB, Jameson LC, et al. Surgical management of persistent intoeing gait due to increased internal tibial torsion in children. J Pediatr Orthop. 2014;34:467–73. doi: 10.1097/BPO.0000000000000173. [DOI] [PubMed] [Google Scholar]
- 18.Uhlrich SD, Silder A, Beaupre GS, et al. Subject-specific toe-in or toe-out gait modifications reduce the larger knee adduction moment peak more than a non-personalized approach. J Biomech. 2018;66:103–10. doi: 10.1016/j.jbiomech.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chowdhary A, Drittenbass L, Stern R, et al. Technique tip: Simultaneous first metatarsal lengthening and metatarsophalangeal joint fusion for failed hallux valgus surgery with transfer metatarsalgia. Foot Ankle Surg. 2017;23:e8–e11. doi: 10.1016/j.fas.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Nakasa T, Ishikawa M, Ikuta Y, et al. In-vivo imaging of the sentinel vein using the near-infrared vascular imaging system in hallux valgus patients. J Orthop Sci. 2017;22:1066–70. doi: 10.1016/j.jos.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Hida T, Okuda R, Yasuda T, et al. Comparison of plantar pressure distribution in patients with hallux valgus and healthy matched controls. J Orthop Sci. 2017;22:1054–59. doi: 10.1016/j.jos.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 22.Bennett HJ, Shen G, Cates HE, et al. Effects of toe-in and toe-in with wider step width on level walking knee biomechanics in varus, valgus, and neutral knee alignments. Knee. 2017;24:1326–34. doi: 10.1016/j.knee.2017.08.058. [DOI] [PubMed] [Google Scholar]
- 23.Naqvi G, Stohr K, Rehm A. Proximal femoral derotation osteotomy for idiopathic excessive femoral anteversion and intoeing gait. SICOT J. 2017;3:49. doi: 10.1051/sicotj/2017033. [DOI] [PMC free article] [PubMed] [Google Scholar]