Abstract
Takotsubo cardiomyopathy is an acquired transient cardiomyopathy that causes severe systolic dysfunction in the absence of coronary disease. Here we present a case of reverse takotsubo cardiomyopathy. A 67-year-old female was admitted for weakness and falls due to severe malnutrition. During her stay she was diagnosed with an eating disorder. She also developed chest pain during her hospitalization and was taken urgently for catheterization which showed normal coronary arteries with akinetic basal and inferior walls and hyperkinesis of the apex. Her ejection fraction decreased to 25% from 60% five days previously. She was diagnosed with reverse takotsubo. She was placed on an appropriate heart failure regimen and eventually transferred to inpatient rehabilitation. In its typical form, takotsubo causes apical ballooning due to hyperkinetic basal and inferior wall motion and apical hypokinesis. Reverse takotsubo causes a depressed basal segment with apical hyperkinesis usually brought on by severe emotional or physical stress. Our case is the first documented report of an eating disorder causing the reverse type of takotsubo cardiomyopathy.
<Learning objective: The reader will be able to recognize stress-induced cardiomyopathy in the right clinical setting and understand that there are different variants of this condition that can present with multiple different wall motion abnormalities.>
Keywords: Reverse takotsubo, Stress-induced cardiomyopathy, Takotsubo cardiomyopathy
Introduction
Stress-induced cardiomyopathy or takotsubo cardiomyopathy is a syndrome defined by a reversible systolic dysfunction of the left ventricle in the absence of a causal coronary artery syndrome. It is usually associated with extreme emotional stress and is referred to as the “broken-heart syndrome”. The most common manifestation is apical depression, which creates the characteristic finding of apical ballooning on echocardiography. There are less common forms of this condition that can present with varying patterns of systolic dysfunction. These variants of takotsubo have been shown to have different clinical presentations and are associated with different triggers of stress. We present a case of reverse takotsubo cardiomyopathy caused by an eating disorder.
Case report
A 67-year-old woman with a history of Crohn's disease, severe malnutrition, and peptic ulcer disease was admitted for weakness and recurrent falls. In the weeks prior to admission she had decreased oral intake due to severe nausea and vomiting. On the day of admission she had several pre-syncopal falls at home prompting her visit to the emergency center. She had a surgical history of a partial gastrectomy, right hemi-colectomy, and gastroduodenostomy as a result of her severe Crohn's disease. She was a non-smoker, previously worked as a nurse, and denied any family history of cardiac disease.
Physical examination revealed normal vital signs with no orthostatic hypotension. She appeared poorly nourished, profoundly weak, and exhibited a flat affect with anhedonia. Her physical examination was unremarkable. Workup for syncope including electrocardiography (ECG) and cardiac biomarkers was negative. She had a trans-thoracic 2D echo which showed a normal ejection fraction with no wall motion abnormalities. She also underwent esophagogastroduodenoscopy, which showed patent anastomoses through her stomach and duodenum. She was prescribed a calorie counting diet and appetite stimulating anti-depressants; however, this failed due to nausea and food avoidance. She was eventually placed on total parenteral nutrition (TPN). She was evaluated by a psychiatrist and was diagnosed with avoidant/restrictive food intake disorder, a condition based on a lack of interest in food and persistent failure to meet nutritional needs. She developed low-grade fevers during admission and TPN was discontinued due to concern of infection.
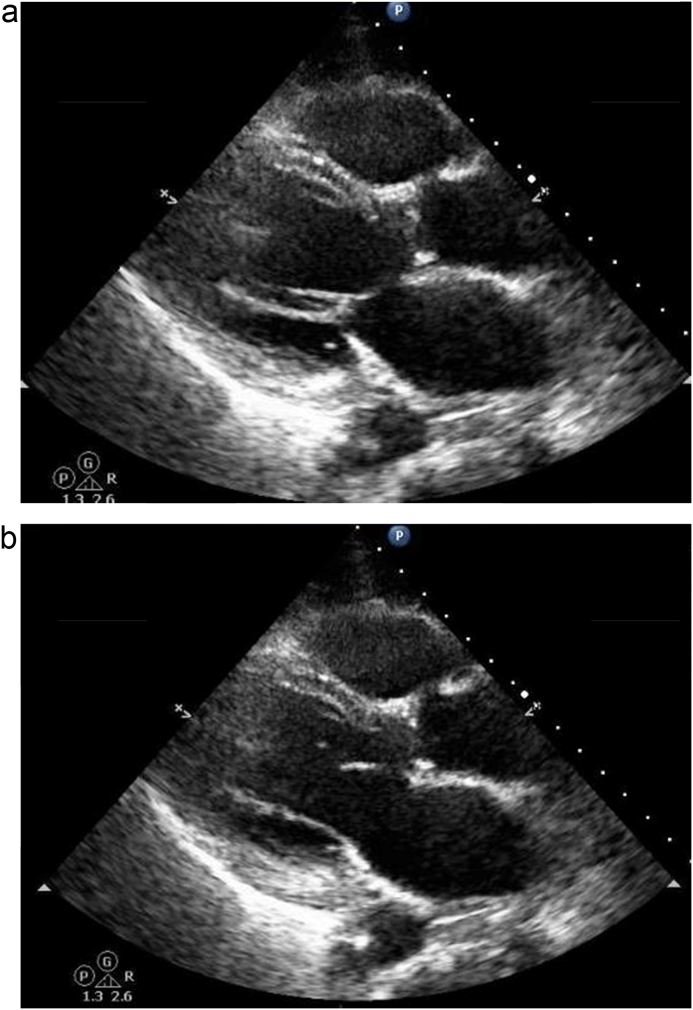
On the 13th day of her hospital stay she developed severe sub-sternal chest pain with shortness of breath. An ECG showed sinus tachycardia with no ST elevation (Fig. 3). A chest X-ray showed bilateral vascular congestion as seen in Fig. 1. Troponin was mildly elevated at ng/mL and B-natriuretic peptide was elevated at 4870 pg/mL. Levels of potassium, magnesium, and phosphorous, which had been measured twice daily since starting TPN remained within normal limits. She was started on a heparin and nitroglycerin continuous infusion. A bedside transthoracic echocardiogram showed multiple regional wall abnormalities and an ejection fraction of 30% as seen in Fig. 2a and b. She was taken emergently for catheterization.
Fig. 3.
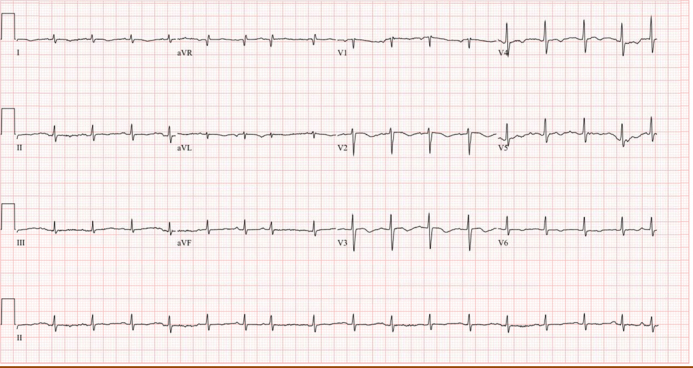
Electrocardiograph at onset of symptoms showing sinus tachycardia, T-wave flattening in the inferior leads, and T-wave inversions in the anterior and lateral leads.
Fig. 1.
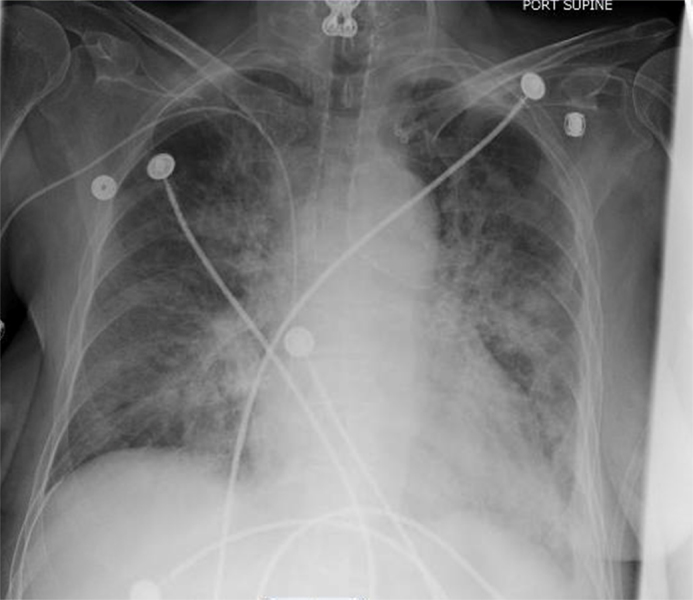
Chest X-ray performed after onset of acute shortness of breath demonstrating bilateral airspace opacities and pulmonary edema.
Fig. 2.
Transthoracic echocardiogram demonstrating multiple regional wall motion abnormalities in the parasternal long-axis view in both end systole (a) and end diastole (b).
During her catheterization she was noted to have no coronary disease. A left ventriculogram showed a hyperdynamic apex with inferior and basal wall hypokinesis as seen in Video 1. Her estimated ejection fraction was 25%. Heparin and nitroglycerin were stopped and she was put on a heart failure medication regimen including a diuretic, beta-blocker, angiotensin-converting enzyme inhibitor, and aldosterone receptor antagonist. Her clinical status improved over the following few weeks. She had a percutaneous endoscopic gastrostomy tube placed and was discharged to inpatient rehabilitation.
Discussion
We present a case of a rare variant of stress-induced cardiomyopathy known as reverse or inverted takotsubo. The name is derived from the finding of basal hypokinesis as opposed to the common variant with apical hypokinesis. This type of takotsubo is thought to occur in about 2% of patients [1]. Other variations include hypokinesis of the mid ventricle in about 15%, global involvement of the ventricle, and focal involvement of an isolated section of the ventricle in about 1.5% [1].
Takotsubo or stress-induced cardiomyopathy is thought to be the result of catecholamine induced vascular spasm brought on by intense emotional or physical stress [1]. This has been demonstrated in a case report, which showed reversible ST segment elevation with the use of intra-coronary nitroglycerin in a patient with takotsubo [2]. It has been hypothesized that the area of hypokinesis is variable due to an asymmetric distribution of adrenergic receptors in the myocardium. According to the International Takotsubo Registry (ITR) physical stress is a more common precipitant than emotional stress, 36% versus 27.7%. Emotional triggers were more common among females as opposed to men who presented with more physical triggers. Psychiatric illness is also common in patients presenting with this disease occurring in about 42% of this population [1]. This disease also predominantly affects women who make up 89.8% of the ITR registry with the majority, 79.1%, over the age of 50 years [1].
There are important features that differentiate reverse takotsubo from its more classic form. The reverse type of takotsubo usually presents in a younger population with a mean age of 36 years versus 62 years for other types according to one study of 60 patients [3]. It has also been almost exclusively found in patients with emotional or physical stress as opposed to other subtypes with no known physiological trigger [4], [5], [6], [7], [8]. Case studies have reported refeeding syndrome, energy drinks, serotonin syndrome, amphetamine use, pheochromocytoma, and subarachnoid hemorrhage as examples of physiological stressors that induce reverse stress cardiomyopathy [4], [5], [6], [7], [8], [9]. Clinical manifestations also differ in this subtype with less shortness of breath, pulmonary edema, and cardiogenic shock at presentation. Additionally, troponin levels tend to be higher and ejection fraction lower in reverse takotsubo with a paradoxical faster recovery [1], [3].
This case represents a rare presentation of reverse takotsubo that was likely precipitated by her depression and underlying eating disorder. Avoidant/restrictive food intake disorder is more common in children with an estimated prevalence of 1% in the general population of children aged 8–18 years, however it can carry on into adulthood [10]. It is diagnosed by a combination of weight loss, nutritional deficiency, impaired psychosocial functioning, exclusion of a general medical condition, and unimpaired body image distortion seen in anorexia or bulimia. During our patient's hospital stay her caloric intake decreased due to persistent nausea to almost nothing per day, which was the likely trigger for her cardiomyopathy. Refeeding syndrome was a diagnostic consideration, however due to the close monitoring of her electrolytes which remained normal and the fact that her TPN had been discontinued 1 week prior to the development of symptoms we excluded this from our differential diagnosis.
Our patient presented with severe pulmonary edema and shortness of breath, which is atypical of reverse takotsubo. We believe this to be a result of her severe malnutrition and hypoalbuminemia in the setting of an acute change in her ejection fraction. Several cases of reverse takotsubo have been reported in the literature, however our case represents a rare precipitant to this disease with an unusual clinical course. Careful clinical and psychosocial assessment in this patient led to the correct diagnosis and obviated the need for further cardiac testing.
Reverse takotsubo is a rare form of stress-induced cardiomyopathy and presents with apical hyperkinesis and basal/inferior hypokinesis. It is associated almost exclusively with physical or emotional stress, younger age, less severe symptoms, and faster recovery. This should be considered in any patient with known emotional stressors at low risk for atherosclerotic coronary disease and severe change in left ventricular function.
Conflict of interest
The authors have no conflict of interest.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jccase.2016.10.015.
Appendix A. Supplementary data
The following are the supplementary data to this article:
Left ventriculogram showing apical hyperkinesis and basal hypokinesis.
References
- 1.Templin C., Ghadri J.R., Diekmann J., Napp L.C., Bataiosu D.R., Jaguszewski M., Cammann V.L., Sarcon A., Geyer V., Neumann C.A., Seifert B., Hellermann J., Schwyzer M., Eisenhardt K., Jenewein J. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 2.Sansen V., Holvoet G. Takotsubo cardiomyopathy presenting as multivessel coronary spasm syndrome: case report and review of the literature. Acta Cardiol. 2007;62:507–511. doi: 10.2143/AC.62.5.2023415. [DOI] [PubMed] [Google Scholar]
- 3.Ramaraj R., Movahed M.R. Reverse or inverted takotsubo cardiomyopathy (reverse left ventricular apical ballooning syndrome) presents at a younger age compared with the mid or apical variant and is always associated with triggering stress. Congest Heart Fail. 2010;16:284–286. doi: 10.1111/j.1751-7133.2010.00188.x. [DOI] [PubMed] [Google Scholar]
- 4.Robles P. Reverse or inverted apical ballooning in a case of refeeding syndrome. World J Cardiol. 2015;7:361. doi: 10.4330/wjc.v7.i6.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Movahed M.R., Mostafizi K. Reverse or inverted left ventricular apical ballooning syndrome (reverse takotsubo cardiomyopathy) in a young woman in the setting of amphetamine use. Echocardiography. 2008;25:429–432. doi: 10.1111/j.1540-8175.2007.00604.x. [DOI] [PubMed] [Google Scholar]
- 6.Mehta N.K., Aurigemma G., Rafeq Z., Starobin O. Reverse takotsubo cardiomyopathy: after an episode of serotonin syndrome. Tex Heart Inst J. 2011;38:568–572. [PMC free article] [PubMed] [Google Scholar]
- 7.Gervais M.-K., Gagnon A., Henri M., Bendavid Y. Pheochromocytoma presenting as inverted takotsubo cardiomyopathy: a case report and review of the literature. J Cardiovasc Med (Hagerstown) 2015;16(Suppl. 2):S113–S117. doi: 10.2459/JCM.0b013e3283356651. [DOI] [PubMed] [Google Scholar]
- 8.Nanda S., Bhatt S.P., Dale T.H. Takotsubo cardiomyopathy – a new variant and widening disease spectrum. “Inverted takotsubo” pattern related to catecholamine toxicity. Int J Cardiol. 2009;132:438–439. doi: 10.1016/j.ijcard.2007.08.069. [DOI] [PubMed] [Google Scholar]
- 9.Piérard S., Vinetti M., Hantson P. Inverted (reverse) takotsubo cardiomyopathy following cerebellar hemorrhage. Case Reports Cardiol. 2014;2014:781926. doi: 10.1155/2014/781926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keel P.K., Brown T.A., Holm-Denoma J., Bodell L.P. Comparison of DSM-IV versus proposed DSM-5 diagnostic criteria for eating disorders: reduction of eating disorder not otherwise specified and validity. Int J Eat Disord. 2011;44:553–560. doi: 10.1002/eat.20892. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Left ventriculogram showing apical hyperkinesis and basal hypokinesis.