Abstract
A 76-year-old man taking theophylline was admitted to our hospital with congestive heart failure and supraventricular tachycardia (SVT). After admission, he developed cardiogenic shock as a result of SVT storm, which was refractory to medical treatment including adenosine and electrical cardioversion. The serum theophylline concentration at admission was identified as toxic. Therefore, theophylline toxicity was considered as a major cause of the SVT storm. Hemodynamic stability was achieved by using mechanical circulatory support. Additionally, continuous hemodiafiltration was performed to remove theophylline, and it was effective for suppression of SVT. The patient was successfully weaned off mechanical circulatory support. After the patient’s general status had improved, an electrophysiological study was performed, and it showed orthodromic atrioventricular reentrant tachycardia with a right free wall accessory pathway. Radiofrequency catheter ablation was successfully performed.
<Learning objective: SVT is often hemodynamically stable and medically well-controllable with adenosine. However, SVT is occasionally refractory or life-threatening under specific conditions such as theophylline toxicity, since theophylline has an inhibitor effect on adenosine. Mechanical circulatory support should be used in case of life-threatening SVT storm associated with theophylline toxicity.>
Keywords: Supraventricular tachycardia storm, Theophylline toxicity, Mechanical circulatory support
Introduction
Theophylline is widely used for management of patients with chronic obstructive pulmonary disease and bronchial asthma. However, in some cases, theophylline toxicity causes major complications because of its narrow therapeutic window [1]. Cardiac arrhythmia, including supraventricular tachycardia (SVT) and multifocal atrial tachycardia, is one of the complications of theophylline toxicity [2]. In most cases, supraventricular arrhythmias are hemodynamically stable and well-controllable with medical treatment. However, in few cases, mechanical circulatory support was needed to control such arrhythmias, which are refractory to medical therapy [3], [4]. We describe here a case of life-threatening SVT storm associated with theophylline toxicity, in which mechanical support, as well as continuous hemodiafiltration (CHDF), was effective.
Case report
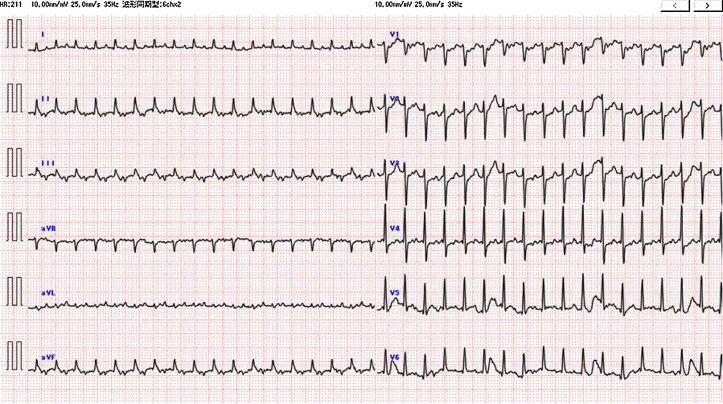
A 76-year-old man with a history of smoking was referred to our hospital with worsening dyspnea. He had been taking medication for chronic obstructive pulmonary disease for 3 months, including theophylline (200 mg twice a day), long-acting muscarinic antagonists, and a long-acting beta-agonist inhaler. On arrival at hospital, his blood pressure was 121/63 mmHg, pulse was 192 bpm, breathing rate was 30/min, and body temperature was 36.3 °C. An electrocardiogram showed SVT with a ventricular rate of 211 bpm (Fig. 1). In the past, he had never experienced heart palpitation. A laboratory examination showed an elevation of N-terminal pro-brain natriuretic peptide concentration (17,310 pg/mL). A chest X-ray demonstrated acute pulmonary edema with cardiac enlargement (Fig. 2A). A transthoracic echocardiogram revealed global severe hypokinesis of the left ventricle (LV) with a reduced left ventricular ejection fraction (LVEF) of 20%. The LV end-diastolic diameter was 54 mm and neither major valvular disease nor pericardial effusion was found. At the emergency room, intravenous adenosine (20 mg) was repetitively administered to terminate his regular, short RP’ tachycardia (Fig. 1). However, there was no response to adenosine, and SVT was not terminated.
Fig. 1.
Electrocardiogram on admission. An electrocardiogram shows regular tachycardia of a narrow QRS complex at 211 bpm.
Fig. 2.
(A) Chest X-ray (anteroposterior view) shows acute pulmonary edema with cardiac enlargement (cardiothoracic ratio of 55%). (B) Electrocardiographic monitoring after admission shows supraventricular tachycardia, which was triggered by a sporadic atrial extra-systole.
After admission, SVT continued, and his systolic blood pressure gradually decreased to 60 mmHg. Electrocardiographic monitoring showed that there were frequent, sporadic atrial extra-systoles and SVT was initiated just after these atrial extra-systoles (Fig. 2B). Tachyarrhythmia was temporarily converted to sinus rhythm by electrical cardioversion. However, SVT recurred soon after electrical cardioversion. Even with intravenous infusion of amiodarone, sinus rhythm was difficult to maintain after electrical cardioversion, and SVT restarted immediately after sporadic atrial extra-systoles. The serum theophylline concentration at admission was 38.5 μg/mL, which was toxic (normal therapeutic range: 10–20 μg/mL). Therefore, theophylline toxicity was considered as a major cause of SVT storm.
A blood test at 15 h after admission showed multi-organ dysfunction with acute renal failure (serum creatinine level, 1.55 mg/dL) and acute hepatic dysfunction (aspartate aminotransferase, 8106 U/L; alanine aminotransferase, 1626 U/L). Arterial blood gas analysis under 10 L/min oxygen by mask showed metabolic acidosis with a pH of 6.977, PCO2 of 40.6 mmHg, PO2 of 85.5 mmHg, and lactic acid level of 18 mmol/L. We decided to use mechanical circulatory support to control the life-threatening SVT storm. Right heart catheterization prior to mechanical circulatory support showed right atrial pressure of 12 mmHg, mean pulmonary artery pressure of 40 mmHg, pulmonary capillary wedge pressure of 30 mmHg, cardiac output 2.4 L/min, and cardiac index 1.4 L/min per m2. Percutaneous cardiopulmonary support (PCPS) was initiated with percutaneous cannulation of the left femoral artery and vein, and an intra-aortic balloon pump was also placed via the right femoral artery. CHDF was subsequently initiated to remove the theophylline. Metabolic abnormalities and theophylline toxicity improved once PCPS flow and CHDF were established. A total of 20 h after CHDF initiation, the theophylline concentration decreased to the normal therapeutic range (8.2 μg/mL). After achieving hemodynamic stability, an intravenous verapamil infusion could be initiated, which was also effective for suppression of SVT. Under mechanical circulatory support, we could maintain sinus rhythm, and sporadic atrial extra-systoles disappeared (Fig. 3). It was a possible option to perform catheter ablation at the time of PCPS introduction. However, the SVT could be controlled by combined modality therapy fortunately, we decided to perform elective catheter ablation. PCPS and CHDF were successfully removed after 3 days. On the 16th day, echocardiography showed that LVEF had improved to 41%. This finding suggested that his reduced LVEF was tachycardia-induced cardiomyopathy, and he had asymptomatic tachyarrhythmia associated with theophylline toxicity in a chronic course.
Fig. 3.
Summary of the acute clinical course of the patient. The serum theophylline concentration was reduced and tachycardia disappeared after initiation of percutaneous cardiopulmonary support (PCPS) and continuous hemodiafiltration (CHDF). IABP; intra-aortic balloon pump.
On the 36th day, cardiac catheterization, including coronary angiography and an electrophysiological study, was performed after the patient’s general status had improved. Coronary angiography showed no significant stenosis in major coronary arteries. An electrophysiological study (EPS) showed retrograde ventriculoatrial conduction via the accessory pathway in the lateral tricuspid annulus and provoked atrioventricular reentrant tachycardia with this accessory pathway (Fig. 3). During the procedure, the SVT was terminated with a bolus of intravenous adenosine 10 mg. Radiofrequency catheter ablation for this accessory pathway was successfully performed, and any tachycardia could not be induced. His general status fully recovered, and he was then discharged on day 46. After discharge, sinus rhythm was maintained for 5 months. Finally, LVEF improved to 63% and the NT-pro BNP level decreased to 99 pg/mL.
Discussion
We describe here a rare case of life-threatening SVT storm caused by theophylline toxicity that resulted in tachycardia-induced cardiomyopathy with cardiovascular collapse. Mechanical circulatory support and CHDF were effective for controlling the patient’s arrhythmia.
Clinical manifestations of theophylline toxicity have a wide diversity. Mild theophylline toxicity includes nausea and vomiting, and severe toxicity includes cardiac arrhythmias, seizures, and death [1]. In patients with chronic theophylline intoxication, severe clinical manifestations, including cardiac arrhythmias, occur even if theophylline concentrations are relatively low [5]. Theophylline enhances atrial automaticity and intra-cardiac conduction, which increase the occurrence of atrial fibrillation, SVT, and multifocal atrial tachycardia [2]. Treatment of theophylline intoxication involves administration of activated charcoal and bowel irrigation in mild toxicity. The Massachusetts Poison Control System protocol recommends hemodialysis or hemoperfusion if patients present with recurrent seizures or cardiac arrhythmias, regardless of theophylline concentrations [5]. In our case, reducing theophylline concentrations by CHDF was effective for suppressing SVT. This finding suggested that theophylline toxicity was the main mechanism involved in SVT storm.
SVTs are frequently encountered in clinical practice. In most cases, these supraventricular arrhythmias are hemodynamically stable and medically well-controllable. However, our patient required PCPS to obtain hemodynamic stability. PCPS is a method of cardiac substitution in the situation of refractory cardiogenic shock or tachyarrhythmia, especially in ventricular fibrillation storm. Cardiogenic shock secondary to SVT requiring PCPS was reported in a few cases, primarily in the pediatric population [6]. In our case, hemodynamic stability could not be achieved while SVT continued because of severely reduced LV systolic function. PCPS was required until the concentration of theophylline decreased to the normal therapeutic range with CHDF.
Vagal maneuvers and pharmacological treatment are usually effective in termination of SVT. In particular, adenosine is the first choice because of its quick onset and short half-life. Paroxysmal SVT involving the atrioventricular node as a part of reentrant circuit is terminated with adenosine in over 90% of patients [7]. SVT is rarely difficult to control with traditional antiarrhythmic therapy. In our case, adenosine had no effect on SVT because of an extremely high concentration of theophylline, which interferes with adenosine’s actions or metabolism. Theophylline inhibits adenosine competitively at the A1 receptor [8]. This was supported by the finding that the provoked SVT during EPS was easily terminated with adenosine. Acidosis, excess endogenous catecholamines, and hypoxemia also promote development of SVT, in addition to theophylline toxicity. Furthermore, sporadic atrial extra-systoles caused by theophylline toxicity also promote immediate recurrence of SVT after electrical cardioversion.
In conclusion, we present a rare case of SVT storm associated with theophylline toxicity that resulted in tachycardia-induced cardiomyopathy with cardiovascular collapse. Our experience suggests that SVT is refractory or life-threatening under specific conditions, such as theophylline toxicity. Mechanical circulatory support should be used in case of life-threatening SVT storm associated with theophylline toxicity.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Shannon M. Predictors of major toxicity after theophylline overdose. Ann Intern Med. 1993;119:1161–1167. doi: 10.7326/0003-4819-119-12-199312150-00002. [DOI] [PubMed] [Google Scholar]
- 2.Sessler C.N., Cohen M.D. Cardiac arrhythmias during theophylline toxicity. A prospective continuous electrocardiographic study. Chest. 1990;98:672–678. doi: 10.1378/chest.98.3.672. [DOI] [PubMed] [Google Scholar]
- 3.Cheruvu C., Walker B., Kuchar D., Subbiah R.N. Successful ablation of incessant AV reentrant tachycardia in a patient on extracorporeal membrane oxygenation. Heart Lung Circ. 2014;23:e12–e15. doi: 10.1016/j.hlc.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 4.Kamada K., Kubo T., Sada M., Ishikita A., Tezuka M., Akiyama Y., Umezu R., Ogawa K., Horimoto K., Matsusaka H. Successful recovery of tachycardia-induced cardiomyopathy with severely depressed left ventricular systolic function by catheter ablation with mechanical hemodynamic support: a case report. Clin Case Rep. 2016;4:232–235. doi: 10.1002/ccr3.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shannon M. Life-threatening events after theophylline overdose: a 10-year prospective analysis. Arch Intern Med. 1999;159:989–994. doi: 10.1001/archinte.159.9.989. [DOI] [PubMed] [Google Scholar]
- 6.Jhang W.K., Lee S.C., Seo D.M., Park J.J. Mechanical circulatory support to control medically intractable arrhythmias in pediatric patients after cardiac surgery. Korean Circ J. 2010;40:471–474. doi: 10.4070/kcj.2010.40.9.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faulds D., Chrisp P., Buckley M.M. Adenosine. An evaluation of its use in cardiac diagnostic procedures, and in the treatment of paroxysmal supraventricular tachycardia. Drugs. 1991;41:596–624. doi: 10.2165/00003495-199141040-00007. [DOI] [PubMed] [Google Scholar]
- 8.Mallet M.L. Proarrhythmic effects of adenosine: a review of the literature. EMJ. 2004;21:408–410. doi: 10.1136/emj.2004.016048. [DOI] [PMC free article] [PubMed] [Google Scholar]