Methamphetamine is a CNS stimulant, and its chronic abuse continues to be a significant problem in the US and worldwide. Powerfully addictive, it has devastating effects on health and other aspects of life. It is a schedule II drug, which can be prescribed only for ADHD, extreme obesity, and narcolepsy. Amphetamine is more often prescribed for these conditions because of its approximately 2-fold lower reinforcing potential. Although amphetamine is less potent than methamphetamine, it can also be neurotoxic when taken at high doses and has the same molecular mechanisms of action as methamphetamine. The mechanisms underlying neurotoxicity are complex, and they ultimately lead to severe dysfunction of dopaminergic and serotonergic neurotransmission. Short of abstinence, there is no treatment for the neurologic complications associated with chronic methamphetamine use.
Understanding the relationship between the molecular mechanisms underlying the neurotoxicity of methamphetamine and related clinical manifestations is imperative to provide more effective treatments for methamphetamine users.
Pharmacology
Methamphetamine is an indirectly acting sympathomimetic amine. It releases dopamine (DA), serotonin, noradrenaline, and adrenaline from nerve terminals, thus increasing their neurotransmission. As a result of its high lipophilicity, methamphetamine easily crosses the blood-brain barrier.
Because its chemical structure is similar to that of monoamines, methamphetamine is recognized as a substrate by DA, serotonin, and the noradrenaline plasma membrane transporter in the brain and transported into neurons and neuronal terminals. Methamphetamine also crosses the neuronal membranes via passive diffusion. Once in the terminals, methamphetamine acts on the monoamine storage vesicles and depletes them of neurotransmitters. In addition, methamphetamine inhibits monoamine metabolism via inhibition of monoamine oxidase. Consequently, intracellular levels of cytoplasmic DA and other monoamines are increased. DA quickly antoxidizes in the cytoplasm and generates reactive oxygen species, leading to degeneration of dopaminergic terminals in most species. Methamphetamine also inhibits and triggers a reversal of the monoamine transporters, which results in a massive release of monoamines into the synaptic cleft.
The net result of the actions of methamphetamine is overstimulation of the monoaminergic pathways in the central and peripheral nervous systems. Higher doses trigger an increase in glutamate in the striatum, which results in excitotoxicity. Methamphetamine interacts with presynaptic DA receptors by competitive antagonism and has minimal effect as an agonist at postsynaptic DA receptors but activates them indirectly via released DA. In addition to damaging dopaminergic and serotonergic terminals, methamphetamine damages neurons in some brain areas (Figure 1).
Figure 1.
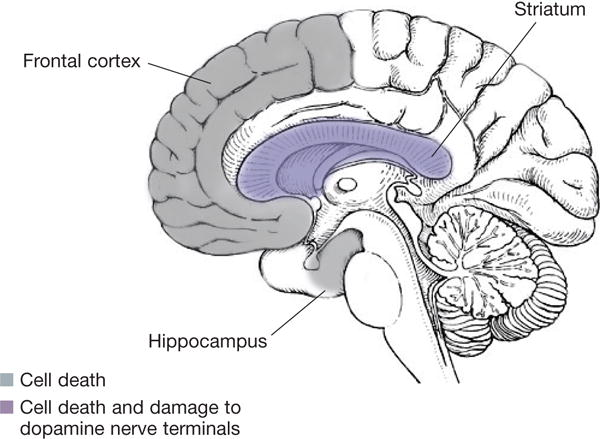
Brain areas affected by methamphetamine neurotoxicity21
Human brain areas corresponding to the mouse brain areas damaged by methamphetamine. Adapted from National Institute on Drug Abuse. 2016.21
Medical use of methamphetamine
Both methamphetamine and amphetamine have active optic isoforms: D-enantiomer and L-enantiomer. The L-isomer contributes more to the peripheral effects, and the D-isomer contributes more to the CNS effects. D-Methamphetamine has 3 to 4 times higher central stimulant effects than L-methamphetamine. Effectiveness and adverse effects are determined not only by the dose but also by the enantiomeric composition of the drug.
Amphetamines are prescribed for ADHD, narcolepsy, and severe obesity. Their therapeutic doses range from 5 to 60 mg daily (usually in divided doses). The D-enantiomer has stronger CNS effects, but it is metabolized quicker than the L-enantiomer, which is longer lasting. Better clinical response was seen in children with ADHD who were treated with drugs that contain both enantiomers.1 The initial strong central effect comes from the D-enantiomer, while elongation of the effect is provided by the L-enantiomer. This allows less frequent dosing than a medication containing D-amphetamine only. The maximum therapeutic dose of D-amphetamine and D-methamphetamine is 60 mg daily. However, adverse effects such as insomnia, loss of appetite, and anxiety have occurred with therapeutic doses of amphetamine.2
Short-term behavioral and physiological effects
DA and serotonin pathways regulate a variety of functions and behaviors. Consequently, the repeated release of these monoamines in the CNS (after a methamphetamine binge or chronic abuse of high-dose methamphetamine) is responsible for several neurological problems in methamphetamine users. Short-term behavioral effects of methamphetamine and amphetamine include euphoria, “rush,” alertness, wakefulness, anti-fatigue effect, increased confidence, hyperactivity, and loss of appetite. Higher doses also cause talkativeness, aggressiveness, restlessness, and repetitive behavior.
Very high doses of methamphetamine will trigger some or all of the following symptoms: agitation, confusion, anxiety, irritability, dysphoria, violent behavior, impairment of psychomotor and cognitive skills, stereotypy (punding), auditory hallucinations, panic, formication (delusions of parasites or insects on the skin), and paranoia. During the end stage of the methamphetamine binge, known as “tweaking,” euphoria is gradually replaced by negative feelings (anxiety, feeling of emptiness) and most or all of the symptoms described above. The crash phase follows and is characterized by intense fatigue, uncontrollable sleepiness, and catnapping.
Short-term physiological effects of methamphetamine and amphetamine include loss of appetite, tachycardia, hypertension, tachypnea, mydriasis, and raised body temperature. At higher doses, fever, sweating, headache, blurred vision, dizziness, stomach cramps, muscle fatigue and cramps, chest pains, shaking, dehydration, nausea, and vomiting can occur. Very high doses induce a variety of negative effects such as hyperthermia; hypertension; cardiac arrhythmia; seizures; cerebral hemorrhage; ischemic infarct; renal failure; rhabdomyolysis; and wakefulness to the point of collapse and temporary blindness, coma, or death.
Long-term behavioral and physiological effects
Medically prescribed doses of methamphetamine have some of the adverse effects described above (eg, dysphoria, insomnia, tremors) and can lead to drug addiction. Even the lowest dose (5 mg; 0.06 to 0.08 mg/kg) can result in positive drug effects.
Methamphetamine abuse takes different forms: weekly, daily, and in a binge; via oral, intranasal, or intravenous administration. The recreationally taken methamphetamine dose is estimated to be between 20 and 40 mg. The purity of methamphetamine is currently very high, at 60% to 90%. The illicit methamphetamine is predominantly D-methamphetamine, and commonly abused dosages are 100 to 1000 mg daily—and up to 5000 mg daily in chronic binge use.3 The self-reported chronic methamphetamine dosage was on average 0.25 to 1.6 g daily.4–7
Chronic methamphetamine abuse, particularly at high doses, has a variety of cardiovascular, gastrointestinal, and neurological physiological effects, which include cerebral vasculitis as well as intracerebral, subarachnoid, or intracranial hemorrhage. Behavioral consequences of chronic use include dependence, cognitive impairment, anxiety or depression, violent behavior, insomnia, stereotypy, and psychosis. Cognitive impairments, disturbed sleep or insomnia, depression, and anxiety as well as intense drug craving are the most prominent symptoms of withdrawal; depression and anxiety can lead to suicidal thoughts. In addition, chronic methamphetamine users may be at higher risk for Parkinson disease than non-users because of the toxic effects of the drug in the nigrostriatal DA pathway.
Methamphetamine neurotoxicity in the CNS
There are numerous manifestations of methamphetamine neurotoxicity in the CNS, including psychomotor impairments as well as mental illnesses. The most common cognitive impairments with chronic use are those of episodic memory, executive function, language skills, visuoconstructional abilities, and information processing. Chronic users also display impairments in fine motor skills.
Motor deficits in methamphetamine users typically do not involve alterations in gross motor skills; however, impaired gait and increased risk of Parkinson disease have been reported.8 Other motor impairments include stereotypic behavior, choreoathetoid movements, and dyskinesias that in some cases can persist for a long time after the cessation of methamphetamine use. Anxiety, depression, and psychosis can also persist after cessation of chronic use. Psychosis develops more readily in drug users who take methamphetamine in high doses and for long periods. Moreover, use may trigger underlying psychosis or schizophrenia. In fact, the symptoms of methamphetamine-induced psychosis are similar to those observed in patients with schizophrenia.9,10 Of note, formication is one of the manifestations of methamphetamine-induced paranoia.
In animal models, methamphetamine neurotoxicity manifests with persistent (long-lasting after drug cessation) reductions in dopaminergic and serotonergic markers, morphological and structural abnormalities, apoptosis, and inflammatory response (microglia activation and gliosis). Other neurons, including glutamatergic, GABAergic, and cholinergic, can also be dysregulated by methamphetamine.
In the human brain, the methamphetamine-mediated neurotoxic effects and their manifestations in users are similar to those observed in animals. Studies of autopsied human brains determined that dopaminergic markers and the serotonin transporter are decreased in the caudate and putamen in methamphetamine users.11,12 Moreover, oxidative stress, decreased phospholipid metabolism, and activated glial cells have been detected in the autopsied striatum of chronic methamphetamine users.10,13–15
In vivo imaging (PET and MRI) revealed neuronal alterations that correlate with behavioral neurological consequences of methamphetamine neurotoxicity. Sensitization to methamphetamine psychosis could be related to neurotoxicity because psychiatric symptoms were found to correlate inversely with DA transporter density in the striatum andprefrontal cortex.16 With extended abstinence, methamphetamine neurotoxicity–associated brain abnormalities and neurological problems usually partially recover. Some manifestations of methamphetamine neurotoxicity and related molecular mechanisms are presented in the Table.
TABLE.
Some manifestations of methamphetamine neurotoxicity and related molecular mechanisms17
| Manifestation | Dose | Molecular mechanism |
|---|---|---|
| Anxiety, dysphoria | > 30 mg | Increased adrenergic α1-receptor stimulation in the prefrontal cortex, 5-HT2 receptor, and DA receptor stimulation in the striatum |
| Elevated body temperature | > 30 mg | Increased DA, serotonin, and noradrenaline release in the hypothalamus |
| Talkativeness | > 50 mg | Activation of anterior cingulate cortex and ventral striatum |
| Paranoia | > 55 mg | Increased DA release in the striatum |
| Hallucinations (auditory, visual) | > 55 mg | Auditory: increased activation of thalamus and ventral striatum; visual: increased activation of paralimbic and primary motor cortices |
| Stereotypy (punding) | High | Imbalance between D1 and D2 receptor signaling in the dorsal striatum |
| Choreoathetosis, dyskinesia | High | Overstimulation of D2 receptors in the dorsal striatum |
DA, dopamine.
Implications for treatment
Symptoms can be triggered by acute or chronic methamphetamine administration, binge use, or withdrawal from the drug. When patients with acute symptoms of neurotoxicity present to the emergency department, they are often agitated, violent, combative, and psychotic—and sometimes require physical restraints. These patients can be treated with sedative hypnotics and antipsychotics. Persistent psychosis, anxiety, and depression in current or abstinent methamphetamine users can be treated with antipsychotic, antidepressant, and antianxiety medications. Stereotypic and choreoathetoid movements might be prevented with atypical antipsychotics and haloperidol, respectively.
Methamphetamine is frequently combined with other drugs, including alcohol, marijuana, narcotic analgesics, other stimulants, and depressants. Therefore, it is often difficult to separate the impact of one from another. Logan17 reviewed several studies on the effects of amphetamines coadministered with other drugs. In general, depressants negate the stimulant effect of amphetamines; however, the impairing effects of the drugs would most often be additive.
A significant percentage of methamphetamine users are HIV-positive and are being treated with antiretroviral agents. Findings from in vitro and in vivo studies indicate that HIV infection and methamphetamine potentiate each other’s neurotoxic effects.18,19 Moreover, the combination may be fatal.20 Antiretroviral protease inhibitors are substrates as well as inhibitors of CYP2D6 and may increase methamphetamine concentration in the plasma. Betulinic acid and its derivatives might potentiate neurotoxicity in high-dose methamphetamine users via potentiation of mitochondrial dysfunction, as seen in rats (Figure 2).19 Consequently, caution must be exercised when prescribing anti-HIV medications to methamphetamine users.
Figure 2.
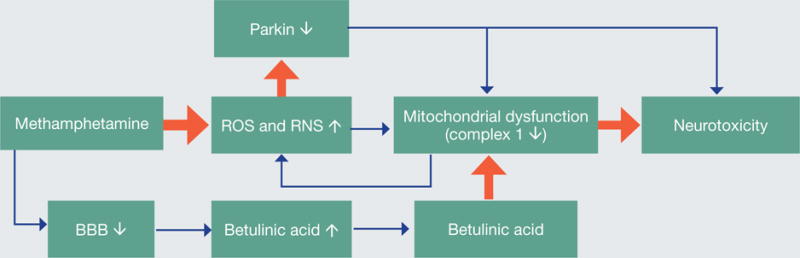
Synergistic neurotoxicity of methamphetamine (METH) and betulinic acid (BA) to monoaminergic terminals in the rat striatum of male late adolescent rats19
Methamphetamine binge increases the production of reactive oxygen and nitrogen species in brain areas containing dopamine (DA), particularly in the DA-rich striatum; decreases the levels of neuroprotective E3 ligase parkin; and increases permeability of the blood-brain barrier to drugs—including betulinic acid.
ROS, reactive oxygen species; RNS, reactive nitrogen species; BBB, blood-brain barrier.
There is no effective pharmacological treatment for methamphetamine dependence, short of prolonged abstinence, although some drug candidates against methamphetamine addiction are in clinical trials. Currently, standard therapies aimed to combat dependence on the drug include cognitive-behavioral therapies and contingency management interventions, support groups, and step-treatment programs.18
SIGNIFICANCE FOR THE PRACTICING PSYCHIATRIST.
Understanding the relationship between the molecular mechanisms underlying the neurotoxicity of methamphetamine and related clinical manifestations is imperative to provide more effective treatments. This article highlights:
-
◗
Neurobiology of methamphetamine toxicity
-
◗
Clinical manifestations of methamphetamine neurotoxicity
-
◗
Implications for treatment of chronic methamphetamine users
Footnotes
Dr. Moszczynska reports no conflicts of interest concerning the subject matter of this article.
References
- 1.Patrick KS, Straughn AB, Perkins JS, González MA. Evolution of stimulants to treat ADHD: transdermal methylphenidate. Hum Psychopharmacol. 2009;24:1–17. doi: 10.1002/hup.992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medscape. Methamphetamine toxicity. http://emedicine.medscape.com/article/820918-overview. Accessed August 2, 2016.
- 3.National Highway Traffic Safety Administration. Methamphetamine (and amphetamine) http://www.nhtsa.gov/people/injury/research/job185drugs/methamphetamine.htm. Accessed July 29, 2016.
- 4.Chang L, Alicata D, Ernst T, Volkow N. Structural and metabolic brain changes in the striatum associated with methamphetamine abuse. Addiction. 2007;102(suppl 1):16–32. doi: 10.1111/j.1360-0443.2006.01782.x. [DOI] [PubMed] [Google Scholar]
- 5.Volkow ND, Chang L, Wang GJ, et al. Loss of dopamine transporters in methamphetamine abusers recovers with protracted abstinence. J Neurosci. 2001;21:9414–9418. doi: 10.1523/JNEUROSCI.21-23-09414.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volkow ND, Wang GJ, Smith L, et al. Recovery of dopamine transporters with methamphetamine detoxification is not linked to changes in dopamine release. Neuroimage. 2015;121:20–28. doi: 10.1016/j.neuroimage.2015.07.035. [DOI] [PubMed] [Google Scholar]
- 7.Kilmer B, Pacula R. Estimating the size of the global drug market: a demand side approach, report 2. Report 2. 2009 http://www.rand.org/content/dam/rand/pubs/technical_reports/2009/RAND_TR711.pdf. Accessed July 27, 2016.
- 8.Moratalla R, Khairnar A, Simola N, et al. Amphetamine-related drugs neurotoxicity in humans and in experimental animals: main mechanisms. Prog Neurobiol. 2016 doi: 10.1016/j.pneurobio.2015.09.011. In press. [DOI] [PubMed] [Google Scholar]
- 9.Rusyniak DE. Neurologic manifestations of chronic methamphetamine abuse. Psychiatr Clin North Am. 2013;36:261–275. doi: 10.1016/j.psc.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tong J, Fitzmaurice P, Furukawa Y, et al. Is brain gliosis a characteristic of chronic methamphetamine use in the human? Neurobiol Dis. 2014;67:107–118. doi: 10.1016/j.nbd.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Wilson JM, Kalasinsky KS, Levey AI, et al. Striatal dopamine nerve terminal markers in human, chronic methamphetamine users. Nat Med. 1996;2:699–703. doi: 10.1038/nm0696-699. [DOI] [PubMed] [Google Scholar]
- 12.Kish SJ, Fitzmaurice PS, Boileau I, et al. Brain serotonin transporter in human methamphetamine users. Psychopharmacol (Berl) 2009;202:649–661. doi: 10.1007/s00213-008-1346-x. [DOI] [PubMed] [Google Scholar]
- 13.Mirecki A, Fitzmaurice P, Ang L, et al. Brain antioxidant systems in human methamphetamine users. J Neurochem. 2005;89:1396–1408. doi: 10.1111/j.1471-4159.2004.02434.x. [DOI] [PubMed] [Google Scholar]
- 14.Ross BM, Moszczynska A, Peretti FJ, et al. Decreased activity of brain phospholipid metabolic enzymes in human users of cocaine and methamphetamine. Drug Alcohol Depend. 2002;67:73–79. doi: 10.1016/s0376-8716(02)00022-4. [DOI] [PubMed] [Google Scholar]
- 15.Fitzmaurice PS, Tong J, Yazdanpanah M, et al. Levels of 4-hydroxynonenal and malondialdehyde are increased in brain of human chronic users of methamphetamine. J Pharmacol Exp Ther. 2006;319:703–709. doi: 10.1124/jpet.106.109173. [DOI] [PubMed] [Google Scholar]
- 16.Sekine Y, Minabe Y, Ouchi Y, et al. Association of dopamine transporter loss in the orbitofrontal and dorsolateral prefrontal cortices with methamphetamine-related psychiatric symptoms. Am J Psychiatry. 2003;160:1699–1701. doi: 10.1176/appi.ajp.160.9.1699. [DOI] [PubMed] [Google Scholar]
- 17.Logan BK. Methamphetamine: effects on human performance and behavior. Forensic Sci Rev. 2002;14:133–151. [PubMed] [Google Scholar]
- 18.Courtney KE, Ray LA. Methamphetamine: an update on epidemiology, pharmacology, clinical phenomenology, and treatment literature. Drug Alcohol Depend. 2014;143:11–21. doi: 10.1016/j.drugalcdep.2014.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Killinger BA, Shah M, Moszczynska A. Co-administration of betulinic acid and methamphetamine causes toxicity to dopaminergic and serotonergic nerve terminals in the striatum of late adolescent rats. J Neurochem. 2014;128:764–775. doi: 10.1111/jnc.12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Urbina A, Jones K. Crystal methamphetamine, its analogues, and HIV infection: medical and psychiatric aspects of a new epidemic. Clin Infect Dis. 2004;38:890–894. doi: 10.1086/381975. [DOI] [PubMed] [Google Scholar]
- 21.National Institute on Drug Abuse. Methamphetamine. 2016 https://www.drugabuse.gov/drugsabuse/methamphetamine. Accessed July 27, 2016.


