Abstract
Study Objective:
The aim of this study is to elaborate the changes of the surgical approach of treatment for uterine myomas in Yangpu Hospital in the past 15 years.
Design:
This was retrospective cohort study.
Setting:
Yangpu Hospital, Tongji University School of Medicine, Shanghai, China.
Materials and Methods:
A total of 4113 patients with symptomatic uterine myomas underwent surgical treatments. Interventions: Eight kinds of different surgeries were involved in the study, including abdominal or laparoscopic surgery, hysterectomy, or uterus-sparing myomectomy.
Measurements:
The study collected patients' clinical data and reviewed surgical access and approach, complications, and the results of following up.
Results:
A total of 1559 cases (37.9%) underwent uterus-sparing myomectomy, 3005 cases (73.1%) performed laparoscopic surgeries. The percentage of laparoscopic surgery was significantly higher than homochronous data of laparotomy after 2003 (P < 0.001). The per year total of uterus-reserved surgery was proved to be negatively correlated with patient's age (R2 = 0.930; P < 0.001). The rate of myomas recurrence was significantly lower in the combined myomectomy and uterine artery occlusion group (4%, 34/910) than in the single myomectomy group (10.5%, 44/420) (P < 0.001).
Conclusions:
Retaining uterus and minimally invasive surgery were the important trends of surgical treatment for symptomatic uterine myomas. Laparoscopic uterus-sparing myomectomy may be an alternative to hysterectomy to manage to appropriate patients with uterine myomas.
Keywords: Laparoscopic uterine artery occlusion, laparoscopy, surgical management, uterine myomas, uterus-sparing myomectomy
INTRODUCTION
Uterine myomas are the most common benign tumor of the uterus, with an estimated incidence of 20%–40% in reproductive-aged women.[1,2] The age and race are thought to be relative to the incidence of myomas. It was showed that the incidence in the age of 35 was 60% and it increased to >80% in the age of 50 among African–American women, while the incidence in Caucasian women was 40% by the age of 35 and almost 70% by the age of 50, according to a study from the USA.[3] The women with myomas are usually affected by symptoms, such as abnormal uterine blood (AUB), pelvic pressure pain, and subfertility or infertility. The standard treatment for symptomatic uterine fibroids has always been surgical, either hysterectomy or the conservative procedure of myomectomy for the women who wish to preserve their uterus. Surgery can be carried out through laparoscopy, vagina, or classical abdominal procedure. Till date, myomas still remain the leading indication for hysterectomy.[4] Although myomectomy allows preservation of the uterus, there is a higher risk of blood loss and greater operative time, when compared with hysterectomy. Fibroids have a 15% recurrence rate, and 10% of women undergoing a myomectomy will eventually require hysterectomy within 5–10 years.[5]
Since 1999, we have tried to carry out laparoscopic myomectomy to treat symptomatic myomas for selected patients. In 2000, we initiated laparoscopic uterine artery occlusion (LUAO) combined with Laparoscopic-assisted myomectomy (LAM) to manage to symptomatic uterine myomas to decrease the risk of intraoperative blood loss. The previous study showed that LAM contributed to not the bleeding reduction but the relief of abnormal symptoms and reduction of uterine volume, as well as the lower myomas recurrence.[6] During the past 15 years, the conservative uterus-sparing surgical therapy by laparoscopy has gradually been alternative to the conventional hysterectomy and became the mainstream for management of symptomatic uterine myomas in our hospital. This study reviewed the clinical data of 4113 patients presenting abnormal symptoms associated with uterine myomas and showed the changes of the approaches of surgical therapy.
MATERIALS AND METHODS
Between January 1999 and December 2013, 4113 patients underwent surgical treatments for uterine myomas in Yangpu Hospital, Tongji University School of Medicine. The retrospective study reviewed the patients' clinical data, including patients' general characteristics, the results of preoperative examinations, surgical approach, complications, and outcomes of following up for the uterus-sparing patients. The study was approved by the ethics committee of Yangpu Hospital (Registration Number: LL-2013-WSJ-009; Date: July 10,2013).
All patients underwent the surgical management for the first time without preoperative hormone treatment. The inclusion criteria included symptomatic myoma measuring ≥5 cm or growing quickly myoma based on ultrasonography examination interval of 3–6 months with the increasing diameter ≥3 cm. Preoperative imaging test (ultrasonography/computed tomography/magnetic resonance imaging), serum CA-125, cervical cytology and human papillomavirus (HPV)-DNA test were required for every patient to exclude the risk of malignancy such as leiomyosarcoma and cervical cancer. The choice of surgical approach, in terms of abdominal or laparoscopic route, or hysterectomy or uterus-sparing myomectomy, depended on comprehensive considerations, including patient's condition, age, and desire to retain childbearing or uterus [Figure 1].
Figure 1.
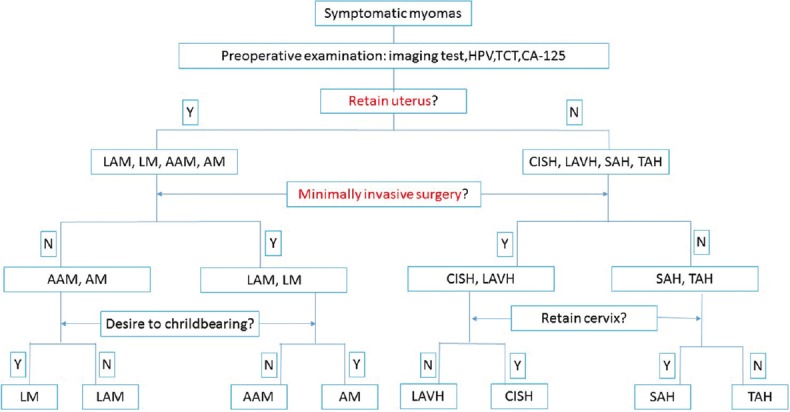
The flow path of surgical approach. CISH: Classic intrafascial supracervical hysterectomy, LM: Laparoscopic myomectomy, LAM: Laparoscopic uterine artery occlusion combined with myomectomy, LAVH: Laparoscopic assisted transvaginal hysterectomy, TAH: Total abdominal hysterectomy, SAH: Subtotal abdominal hysterectomy, AM: Abdominal myomectomy, AAM: Abdominal uterine artery occlusion combined with myomectomy. Y: Yes, N: No
For the women who wanted to preserve uterus but had no wish for childbearing, UAO during myomectomy were recommended. The procedure of UAO was introduced as described in the previous paper.[6] The peritoneum incision was opened in the triangle area surrounded by the round ligament of the uterus, infundibulopelvic ligament and the external iliac vessels. Uterine artery usually originates from the anterior branch of the internal iliac artery with the diameter of about 2–6 mm and the tortuous shape. The ureter goes underneath uterine artery near the paracervical of 2 cm. Bipolar electric coagulation or plasma knife was used to block the initial part of the uterine artery, with the bandwidth of coagulation of 1–1.5 cm.[6]
The number of surgical cases was counted according to the different age group at the interval of 10 years. The correlation analysis between age and surgical approach or access was made. The following up were carried out from January to February in 2015 for the patients who underwent uterus-sparing myomectomy. The symptomatic myomas of ≥3 cm confirmed by ultrasound examination were regarded as myomas recurrence. The recurrence rates of uterine myomas were compared between the groups of UAO plus myomectomy and myomectomy alone. Myomas or uterus specimen were morcellated and took out during laparoscopic surgery. Postoperative pathology examination confirmed the diagnosis of uterine leiomyomas. For the suspicious condition, the specimen was required for the intraoperative frozen pathology examination to exclude the malignancy such as sarcoma and avoid the use of morcellation.
Statistics analysis
The clinical data were presented as a mean ± standard deviation or percentages. Statistical analysis, including survival curve analysis and regression analysis used to statistical software SPSS 18.0 (SPSS Inc., an IBM Company, Chicago, IL). Continuous variables were compared using t-test, and categorical variables were compared using Chi-squared test.
RESULTS
Preoperative assessment and surgical treatment
The general characteristics of the patients, including mean age (age of onset and accepting surgery), symptoms resulting from myoma, numbers of myomas, mean myoma diameter, and patient's parity are described in Table 1, and the data were recorded and compared between the groups of laparoscopy and laparotomy, uterus-sparing myomectomy and hysterectomy. Eight kinds of different operative procedures were involved in the study [Table 2]. 15 cases of laparoscopic surgeries had to convert laparotomy due to heavy pelvic adhesions.
Table 1.
The general characteristics of the patients
| Laparoscopy (n=3005), n (%) | Laparotomy (n=1108), n (%) | P | Uterus-sparing myomectomy (n=1559), n (%) | Hysterectomy (n=2554), n (%) | P | |
|---|---|---|---|---|---|---|
| Age (years olds) | ||||||
| Onset age | 35±1.63 | 35±1.29 | 0.792 | 35±1.43 | 35±1.70 | 0.779 |
| Surgical age | 45±1.32 | 46±2.30 | 0.075 | 44±2.55 | 47±2.78 | 0.008 |
| Symptoms | ||||||
| AUB | 992 (33.0) | 332 (29.7) | 0.954 | 492 (31.6) | 832 (32.6) | 0.912 |
| Pelvic pressure | 1200 (39.9) | 527 (47.6) | 0.080 | 648 (41.6) | 1079 (42.2) | 0.858 |
| Dysmenorrhea | 940 (31.3) | 368 (33.2) | 0.878 | 489 (31.4) | 819 (32.1) | 0.945 |
| Urinary incontinence | 832 (27.7) | 325 (29.3) | 0.554 | 471 (30.2) | 686 (26.9) | 0.790 |
| Infertility/subfertility | 78 (2.60) | 25 (2.26) | 0.958 | 103 (6.61) | 0 | / |
| Parity | 1.68±0.83 | 1.90±0.74 | 0.437 | 1.40±0.70 | 1.69±0.70 | 0.320 |
| Myomas | ||||||
| Single myoma | 1560 (51.9) | 558 (50.4) | 0.781 | 927 (59.5) | 1065 (41.7) | 0.635 |
| Multi-myomas | 1445 (48.1) | 550 (49.6) | / | 632 (40.5) | 1489 (58.3) | / |
| Diameter | 7.33±1.56 | 6.70±1.34 | 0.251 | 7.10±1.20 | 6.63±1.31 | 0.362 |
Laparoscopy includes CISH, LM, LAM, and LAVH, Laparotomy includes TAH, SAH, AM, and AAM. Uterus-sparing myomectomy means LM, LAM, AM and AAM, Hysterectomy means CISH, LAVH, TAH, and SAH. CISH: Classic intrafascial supracervical hysterectomy, LAM: Laparoscopic assisted myomectomy, LM: Laparoscopic myomectomy, TAH: Total abdominal hysterectomy, SAH: Subtotal abdominal hysterectomy, AM: Abdominal myomectomy, AAM: Abdominal uterine artery occlusion combined with myomectomy
Table 2.
Surgical approaches
| Surgical access and procedure | n (%) |
|---|---|
| Laparoscopy | 3005 (73.1) |
| CISH | 1638 (54.5) |
| LM | 276 (9.2) |
| LAM | 1016 (33.8) |
| LAVH | 75 (2.5) |
| Laparotomy | 1108 (26.9) |
| TAH | 352 (31.8) |
| SAH | 489 (44.1) |
| AM | 258 (23.3) |
| AAM | 9 (0.8) |
CISH: Classic intrafascial supracervical hysterectomy, LAM: Laparoscopic uterine artery occlusion combined with myomectomy, LM: Laparoscopic myomectomy, TAH: Total abdominal hysterectomy, SAH: Subtotal abdominal hysterectomy, AM: Abdominal myomectomy, AAM: Abdominal uterine artery occlusion combined with myomectomy, LAVH: Laparoscopic assisted transvaginal hysterectomy
Eight cases (8/4113, 1.95‰), including 5 LAM and 3 abdominal myomectomy encountered malignant transformation, endometrial stromal sarcoma, which were confirmed by intraoperative frozen pathology examination. All of them received timely sub-radical hysterectomy by laparotomy plus pelvic lymphadenectomy. None of cervical cancer or leiomyosarcoma after primary surgery was found.
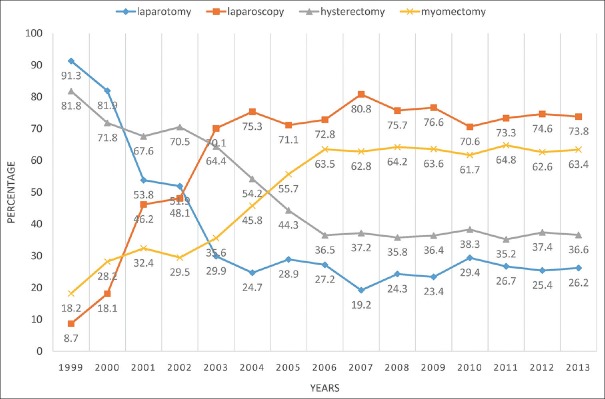
The changes of surgical approach
During the past 15 years, the total number of laparoscopic surgery for uterine myomas added up to 3005 cases (3005/4113, 73.1%), and laparotomy was 1108 case (1108/4113, 26.9%). From 2003 the rate of laparoscopy had got the level of >70% and been higher than the proportion of laparotomy [Figure 2]. 2554 cases (62.1%) underwent hysterectomy, and 1559 cases (37.9%) accepted uterus-sparing myomectomy. After 2005, the cases of uterus-reserved surgery have been more than that of hysterectomy [Figure 2], and the mean proportion was 62.5%/year. In addition, 1016 cases were performed LUAO, which accounted for 78.6% of the total of laparoscopic uterus-sparing myomectomy (1016/1292).
Figure 2.
The rates of surgical access (laparotomy or laparoscopy) and surgical approach (hysterectomy or myomectomy)
Myomectomy was responsible for the most of surgeries in younger group of <45 years, and conversely, hysterectomy was the main surgical approach in the group of ≥45 years [Figure 3]. Based on the result of linear regression analysis of data, uterus retention was negatively correlated with age ([y = −3.0x + 191.0], R2 = 0.930; P < 0.001).
Figure 3.
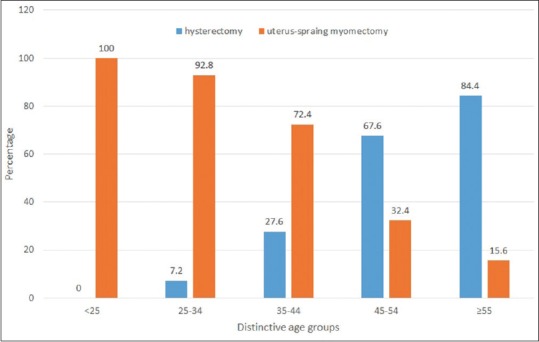
The proportion of different surgical approach in different age of groups
Laparoscopy was primary surgical access in the younger group, which accounted for more than 80% of cases in 25–44 age of the group. It was down to 55.8% at the age of over 55 years old. The rate of laparoscopic route appeared to decrease as the increasing of patient's age (P > 0.05).
Complications
Six cases (0.2%, 6/3005) of laparoscopic surgeries involved the complication: one case of classic intrafascial supracervical hysterectomy (CISH) occurred intestinal trauma due to severe pelvic adhesions, which was repaired by laparotomy on the 3rd day; 3 cases of CISH encountered intraoperative bladder injuries, and accepted the repairing surgery timely; 1 case of LAM suffered intestine incarceration in abdominal incision resulting in small intestine necrosis and had to be performed partial bowel resection; 1 case of laparoscopic assisted transvaginal hysterectomy underwent heavy bleeding after 4 h postoperatively which attributed to ligature slippage of the right uterine artery stump, the patient was timely rescued. In addition, 1 case of CISH accepted transvaginal cervix resection because of cervical myomas after 1 year; 1 case of CISH was performed radical cervix resection after 18 months owing to cervical stump cancer.
The follow-up results
The total number of patient undergoing uterus-preserved myomectomy surgery was 1559 cases. 1330 patients participated in follow-up survey with the follow-up rate of 85.3%. 910 cases were carried out UAO and other 420 cases were done myomectomy alone. The span of follow-up was from 22 to 108 months, with an average interval of 36.4 ± 0.7 months. 34 recurrence cases (4%, 34/910) were found in UAO group with the average follow-up of 25.4 ± 0.8 months. 18 cases of them did the second myomectomy surgeries; 16 cases did the total hysterectomy due to the age >48 years. 44 cases (10.5%, 44/420) in single myomectomy group were recurrent with the follow-up of 19.5 ± 0.5 months. 29 patients performed the myomectomy combined with UAO; 15 cases chose hysterectomy because of perimenopausal age. The difference of recurrence rate between two groups was significant (P < 0.001) [Figure 4].
Figure 4.
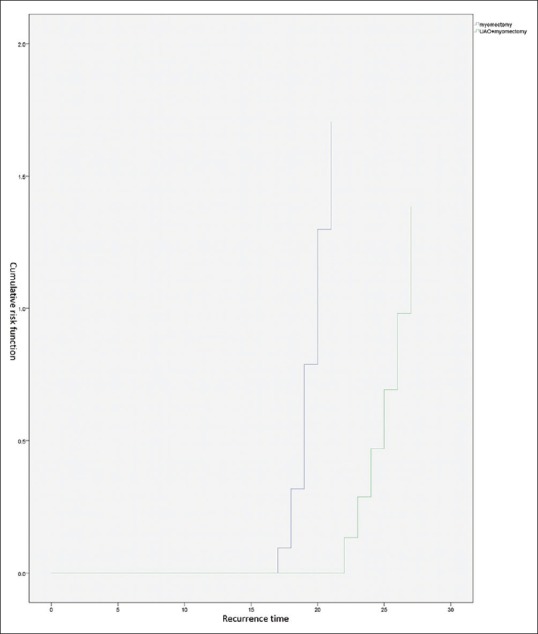
Comparing of the risk of recurrence between UAO combined with myomectomy group and single myomectomy group. UAO: Uterine artery occlusion
DISCUSSION
Minimally invasive access and uterus-sparing surgery
Although minimally invasive technique emerged in China in the late 1990s, the development of endoscopic surgeries was very fast. The study showed that the rate of laparoscopic surgeries maintained the level of 70%–80% after 2003 and reached the peak value of 80.8% in 2007. CISH surgery was the most common procedure of hysterectomy in our study, which was accounted for 95.6% (1638/1713) of removing-uterus approach. In 1996, Dr. Semm came to China and introduced CISH surgery. After that, the majority of appropriated patients with myomas received CISH in our hospital. Our results showed that CISH was safety and feasible for selected women with the low risk of injuries to ureters, bowel and bladder (0.2%, 4/1628) similarly to the results reported by literature (0.2%–0.75%).[7,8] Randomized studies showed that laparoscopic supracervical hysterectomy (LSH) compared with total abdominal hysterectomy has no significant differences in postoperative risk of complications, including urinary tract injury, bowel obstruction, pain score, or pelvic organ prolapse.[9,10,11,12] Hence, the increasing of CISH/LSH in the study was more attributed to the development of laparoscopy techniques and equipment, as well as the surgeon's bias for minimally invasive technology.
Dr. Victor Bonney firstly described myomectomy in 1931 by laparotomy[13] and German Gynecologist Dr. Semm completed the first case of laparoscopic myomectomy in 1979.[14] However, its the fact that hysterectomy is yet the leading place for treatment of symptomatic uterine myomas and now takes up 85.9% of surgical management in the USA.[15] In earlier years, many facts were responsible for the result: the limitation of surgical skills, transfusion and antibiotics application, as well as the introduction of cervical screening programs. The literature supported that hysterectomy was negatively correlated to the incidence of cervical carcinoma, resulting in the steadily increasing rate of total hysterectomy although the death rate of cervical cancer gradually decreased.[16] Today, with the improvement of surgeon's skills and the developments of endoscopy devices, clinicians can perform more precise and complex procedure under laparoscopy. For the women who want to preserve uterus and anatomic integrity whether she has or has not the desire for future childbearing, LM is indicated.[17,18] LM is evidence-based beneficial alternative therapy for symptomatic uterine myomas with reduction of morbidity and recovery time in comparison with AM.[19] A prospective study of 235 patients undergoing LM for symptomatic myomas showed no conversions to laparotomy and in 3 years, only 1.2% of patients had a second LM for recurrent myomas. By 48 h after surgery, 86.3% of the patients were discharged.[20,21]
In the study, the rate of myomectomy has been over the hysterectomy since 2005 and got the peak of 64.8% in 2011 [Figure 2]. Only 8 cases (8/4113, 1.95%) encountered sarcoma during myomectomy. Intraoperative pathology examination was performed to confirm the malignant diagnosis and morcellation was avoided to use. Due to the preoperative excluded examinations and intraoperative pathology confirmation for the suspicious lesion, there are not malignant cases found after operation and morcellation risks do not happen in the study. The introduction of endoscopic surgery has led surgical management of symptomatic uterine myomas into the current era of fertility-preserving or uterus-sparing approach.[22]
Onset age and surgical age
The incidence of uterine myomas was linked to the patient's age, which is 40% to 60% at the age of 35 and >70% after the age of 50.[20] The study showed that the mean age of onset was 35 ± 6.7 years and the mean age of surgery was 45.8 ± 7.7 years. The surgical age was nearly later 10 years than the diagnosed age and the average interval of tumor-bearing was 10 ± 5.3 years. When the patient with no symptoms is not appropriate to recommend surgery, medical management, medical insurance and additional outpatient physician visits are often required, which further increase patients' psychological burden and annual costs.[15] It is necessary for these patients to take part in follow-up. For seeing the change of size of the myomas, we often require patients to come back outpatient for the imaging examination at an interval of 3–6 months.
Our data showed the probability of uterine retention was negatively correlated with patient's age (P = 0.000). The surgical age was 44 ± 2.55 years in retaining uterus group and 47 ± 2.78 years in removing uterus group (P = 0.008). It suggested that younger patients tended to the approach of preserving the uterus. The surgical management of uterine myomas is individual and associated with the patient's age and the desire. However, patients undergoing myomectomy were adequately informed of the risk that the symptoms would persist and that the leiomyomas may recur and require further surgery.
Laparoscopic uterine artery occlusion
Since 1999, we tried to perform LUAO before LM for the initial consideration of reducing intraoperative blood loss. In another article of 566 patients performed LAM, it was showed that the intraoperative blood loss was 88.2 ± 52.7 ml. The other clinic data including postoperative morbidity, uterine volume reduction, and relief rate of AUB were reported as following 5.7%, 48.9%, and 97%.[4] The clinical results were satisfying. The similar outcomes were reported by other documents.[23,24,25] Its well known that leiomyoma originates from unicellular growth, and the nucleus of fibroid cell can be very small, and 77%–80% patients are the cases of multi-leiomyomas.[26] Small residual myomas which could not be removed totally during myomectomy are the important cause of myomas recurrence. UAO helped to the excision of residual myomas due to hypoxia,[27] which significantly reduces the risk of fibroid recurrence. In this context, the recurrent rate was significantly lower in UAO group than in myomectomy alone (4% vs. 10.5%, P < 0.001) with the follow-up of 36.4 months. In the study, 1016 cases received LAM, accounting for 65.2% of “uterus-sparing” surgeries. No severe intraoperative and postoperative complications occurred. Its regarded as an important fact to promote the development of uterus-sparing surgery.
Although the concept of retaining uterus for the patients with uterine myomas has been widely accepted, there have been few data to show the changes of surgical approach. This study analyzed retrospectively surgical managements of 4113 patients with uterine myomas in the past 15 years and elaborated the development of surgical treatment of uterine myomas. Retaining uterus and minimally invasive approach were the most important changes. Endoscopic surgery appeared to replace gradually traditional laparotomy. LUAO technique greatly promoted the development of laparoscopic uterus-sparing surgery.
CONCLUSION
Although the concept of retaining uterus for the patients with uterine myomas has been widely accepted, there have been few data to show the changes of surgical approach. This study analyzed retrospectively surgical managements of 4113 patients with uterine myomas in the past 15 years and elaborated the development of surgical treatment of uterine myomas. Retaining uterus and minimally invasive approach were the most important changes. Endoscopic surgery appeared to replace gradually traditional laparotomy. LUAO technique greatly promoted the development of laparoscopic uterus-sparing surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ryan GL, Syrop CH, Van Voorhis BJ. Role, epidemiology, and natural history of benign uterine mass lesions. Clin Obstet Gynecol. 2005;48:312–24. doi: 10.1097/01.grf.0000159538.27221.8c. [DOI] [PubMed] [Google Scholar]
- 2.Wallach EE, Vlahos NF. Uterine myomas: An overview of development, clinical features, and management. Obstet Gynecol. 2004;104:393–406. doi: 10.1097/01.AOG.0000136079.62513.39. [DOI] [PubMed] [Google Scholar]
- 3.Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: Ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–7. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 4.Bulun SE. Uterine fibroids. N Engl J Med. 2013;369:1344–55. doi: 10.1056/NEJMra1209993. [DOI] [PubMed] [Google Scholar]
- 5.Vilos GA, Allaire C, Laberge PY, Leyland N Special Contributors. The management of uterine leiomyomas. J Obstet Gynaecol Can. 2015;37:157–78. doi: 10.1016/S1701-2163(15)30338-8. [DOI] [PubMed] [Google Scholar]
- 6.Cheng Z, Yang W, Dai H, Hu L, Qu X, Kang L, et al. Laparoscopic uterine artery occlusion combined with myomectomy for uterine myomas. J Minim Invasive Gynecol. 2008;15:346–9. doi: 10.1016/j.jmig.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Erian J, Hassan M, Pachydakis A, Chandakas S, Wissa I, Hill N, et al. Efficacy of laparoscopic subtotal hysterectomy in the management of menorrhagia: 400 consecutive cases. BJOG. 2008;115:742–8. doi: 10.1111/j.1471-0528.2008.01698.x. [DOI] [PubMed] [Google Scholar]
- 8.Donnez O, Jadoul P, Squifflet J, Donnez J. A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: Evaluation of complications compared with vaginal and abdominal procedures. BJOG. 2009;116:492–500. doi: 10.1111/j.1471-0528.2008.01966.x. [DOI] [PubMed] [Google Scholar]
- 9.Gimbel H, Zobbe V, Andersen BM, Filtenborg T, Gluud C, Tabor A, et al. Randomised controlled trial of total compared with subtotal hysterectomy with one-year follow up results. BJOG. 2003;110:1088–98. [PubMed] [Google Scholar]
- 10.Learman LA, Summitt RL, Jr, Varner RE, McNeeley SG, Goodman-Gruen D, Richter HE. A randomized comparison of total or supracervical hysterectomy: Surgical complications and clinical outcomes. Obstet Gynecol. 2003;102:453–62. doi: 10.1016/s0029-7844(03)00664-1. [DOI] [PubMed] [Google Scholar]
- 11.Thakar R, Ayers S, Clarkson P, Stanton S, Manyonda I. Outcomes after total versus subtotal abdominal hysterectomy. N Engl J Med. 2002;347:1318–25. doi: 10.1056/NEJMoa013336. [DOI] [PubMed] [Google Scholar]
- 12.Gorlero F, Lijoi D, Biamonti M, Lorenzi P, Pullè A, Dellacasa I, et al. Hysterectomy and women satisfaction: Total versus subtotal technique. Arch Gynecol Obstet. 2008;278:405–10. doi: 10.1007/s00404-008-0615-6. [DOI] [PubMed] [Google Scholar]
- 13.Bonney V. The technique and results of myomectomy. Lancet. 1931;217:171–7. [Google Scholar]
- 14.Semm K. New methods of pelviscopy (gynecologic laparoscopy) for myomectomy, ovariectomy, tubectomy and adnectomy. Endoscopy. 1979;11:85–93. doi: 10.1055/s-0028-1098329. [DOI] [PubMed] [Google Scholar]
- 15.Cardozo ER, Clark AD, Banks NK, Henne MB, Stegmann BJ, Segars JH, et al. The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol. 2012;206:211e1–9. doi: 10.1016/j.ajog.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyons TL. Laparoscopic supracervical hysterectomy. Obstet Gynecol Clin North Am. 2000;27:441–50, ix. doi: 10.1016/s0889-8545(00)80034-0. [DOI] [PubMed] [Google Scholar]
- 17.Luciano AA. Myomectomy. Clin Obstet Gynecol. 2009;52:362–71. doi: 10.1097/GRF.0b013e3181b0bdcd. [DOI] [PubMed] [Google Scholar]
- 18.Sami Walid M, Heaton RL. The role of laparoscopic myomectomy in the management of uterine fibroids. Curr Opin Obstet Gynecol. 2011;23:273–7. doi: 10.1097/GCO.0b013e328348a245. [DOI] [PubMed] [Google Scholar]
- 19.van der Kooij SM, Ankum WM, Hehenkamp WJ. Review of nonsurgical/minimally invasive treatments for uterine fibroids. Curr Opin Obstet Gynecol. 2012;24:368–75. doi: 10.1097/GCO.0b013e328359f10a. [DOI] [PubMed] [Google Scholar]
- 20.Tinelli A, Hurst BS, Hudelist G, Tsin DA, Stark M, Mettler L, et al. Laparoscopic myomectomy focusing on the myoma pseudocapsule: Technical and outcome reports. Hum Reprod. 2012;27:427–35. doi: 10.1093/humrep/der369. [DOI] [PubMed] [Google Scholar]
- 21.Khan AT, Shehmar M, Gupta JK. Uterine fibroids: Current perspectives. Int J Womens Health. 2014;6:95–114. doi: 10.2147/IJWH.S51083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rossetti A, Sizzi O, Soranna L, Cucinelli F, Mancuso S, Lanzone A, et al. Long-term results of laparoscopic myomectomy: Recurrence rate in comparison with abdominal myomectomy. Hum Reprod. 2001;16:770–4. doi: 10.1093/humrep/16.4.770. [DOI] [PubMed] [Google Scholar]
- 23.Yen YK, Liu WM, Yuan CC, Ng HT. Laparoscopic bipolar coagulation of uterine vessels to treat symptomatic myomas in women with elevated Ca 125. J Am Assoc Gynecol Laparosc. 2001;8:241–6. doi: 10.1016/s1074-3804(05)60584-1. [DOI] [PubMed] [Google Scholar]
- 24.Mara M, Kubinova K, Maskova J, Horak P, Belsan T, Kuzel D, et al. Uterine artery embolization versus laparoscopic uterine artery occlusion: The outcomes of a prospective, nonrandomized clinical trial. Cardiovasc Intervent Radiol. 2012;35:1041–52. doi: 10.1007/s00270-012-0388-y. [DOI] [PubMed] [Google Scholar]
- 25.Helal A, Mashaly Ael-M, Amer T. Uterine artery occlusion for treatment of symptomatic uterine myomas. JSLS. 2010;14:386–90. doi: 10.4293/108680810X12924466007403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burbank F, Hutchins FL., Jr Uterine artery occlusion by embolization or surgery for the treatment of fibroids: A unifying hypothesis-transient uterine ischemia. J Am Assoc Gynecol Laparosc. 2000;7:S1–49. [Google Scholar]
- 27.Cheng ZP, Tao X, Gong J, Dai H, Hu LP, Yang WH, et al. Early-stage morphological observations of myoma and myometrium after laparoscopic uterine artery occlusion treatment. Eur J Obstet Gynecol Reprod Biol. 2009;145:113–6. doi: 10.1016/j.ejogrb.2009.03.027. [DOI] [PubMed] [Google Scholar]