To the Editor,
We present a case of a 47-year-old, nulliparous woman who underwent a maximal debulking surgery and adjuvant chemotherapy with Taxol–carboplatin for ovarian malignancy, and subsequently had a secondary laparotomic debulking surgery 8 months later due to tumor recurrence. However, after this surgery, the patient refused to take subsequent chemotherapy due to its discomforts. Her wound healing was optimum; however, a small mass developed over the scar and was felt 6 months after the last surgery and it progressed since then to 4 cm × 5 cm in size. The mass is irregular in contour, with erosion and bleeding over the previous laparotomy scar below the umbilicus.
Abdominopelvic computed tomography (CT) showed extensive carcinomatosis. In addition, it showed a 5.1-cm subcutaneous mass in the midline of the abdominal wall, just adhered to and above the abdominal fascia (Figure 1).
Figure 1.
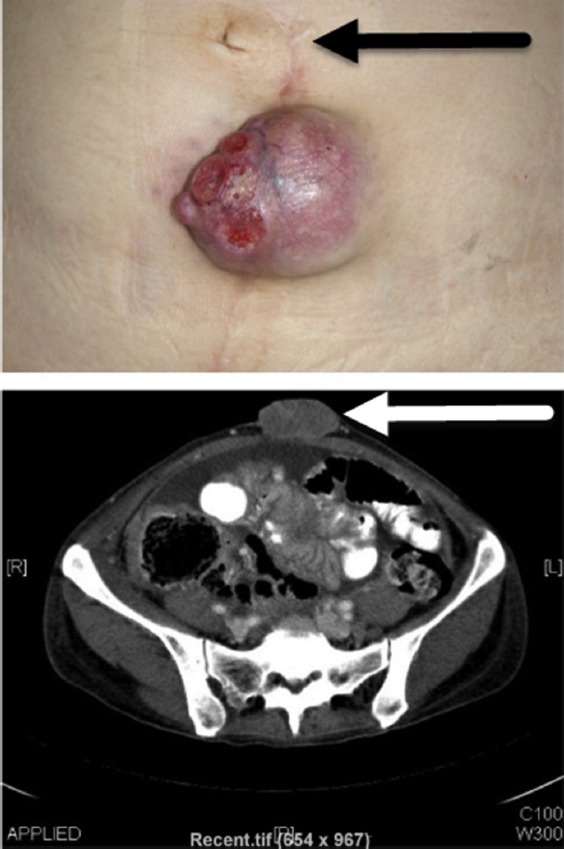
(Above) Small mass with erosion over the previous Laparotomy Scar. (Below) Abdominopelvic CT showing a 5.1 cm subcutaneous mass in midline abdominal wall.
Following hospice palliative care, this patient expired 7 months after the first presentation of abdominal wound metastasis.
Cutaneous metastasis in ovarian cancer is quite rare. In a case series of nine patients from over 200 treated at a single center in Italy, Cormio et al1 in 2003 detected a rate of 3.5% for metastasis to the skin presenting as nodular lesions, commonly on the abdomen or thorax and particularly on abdominal wall incisions, either laparotomy or laparoscopy scars. He also concluded that there is poor prognosis for ovarian cancers with skin metastasis with a survival rate ranging between 2 months and 65 months.2
V. Manvelyan et al (2016) in their article review, points out that in the development of port-site (scar) metastases, the major role is played by biologically aggressive diseases, tumor manipulation, wound contamination, and surgery-related factors.3
Thus in conclusion, the skin metastasis in ovarian cancer is seen not only in laparoscopic port sites but can occur also in laparotomy scars.
Acknowledgments
We thank the Asia-Pacific Association for Gynecologic Endoscopy and Minimal Invasive Therapy (APAGE) for providing International Fellowship in Endoscopy training program at Chang Gung Memorial Hospital, Taiwan for Dr Vijal Modi.
Footnotes
Conflicts of interest: We, the authors, do not have any conflicts of interest and have nothing to disclose.
References
- 1.Cormio G, Capotort M, Di Vagno G, et al. Skin metastases in ovarian carcinoma: a report of nine cases and a review of the literature. Gynecol Oncol. 2003;90(3):682–685. doi: 10.1016/s0090-8258(03)00400-1. [DOI] [PubMed] [Google Scholar]
- 2.Cowan LJ, Roller JI, Connelly PJ, Nahhas WA. Extraovarian stage IV peritoneal serous papillary carcinoma presenting as an asymptomatic skin lesion–a case report and literature review. Gynecol Oncol. 1995;57(3):433–435. doi: 10.1006/gyno.1995.1169. [DOI] [PubMed] [Google Scholar]
- 3.Manvelyan V, Khemarangsan V, Huang K-G, Adlan A-S, Lee C-L. Port-site metastasis in laparoscopic gynecological oncology surgery: an overview. GMIT. 2016 Feb;5(1):1–6. [Google Scholar]


