Abstract
Study objective:
The aim of this study was to compare the surgical outcomes, particularly the specimen retrieval time, between two methods of laparoscopic myomectomy: transumbilical retrieval of the myoma without a morcellator and conventional retrieval of the myoma using a power morcellator via the left lower quadrant.
Design:
Retrospective study.
Setting:
Public hospital.
Patients:
Seventy-four women undergoing laparoscopic myomectomy.
Interventions:
Laparoscopic myomectomy followed by myoma retrieval via transumbilical extraction or electric motorized morcellator extraction.
Measurements and main results:
Seventy-four patients undergoing laparoscopic myomectomy followed by myoma retrieval via transumbilical extraction or electric motorized morcellator extraction were studied. Significant differences were observed in the average weight of the retrieved myomas between the transumbilical and morcellator groups (141.0 vs. 262.8 g, respectively; p < 0.001). Therefore, we chose 27 patients whose total specimen weight was 151–300 g; 13 patients were in the transumbilical extraction group and 14 were in the electric motorized morcellator group. No significant differences were observed in patient characteristics between the two groups. The operative time, blood loss volume, and myoma retrieval time were similar between the two groups.
Conclusion:
Laparoscopic myomectomy with transumbilical extraction for myoma retrieval is a feasible method for specimens weighing up to 300 g.
Keywords: EZ access, Laparoscopic myomectomy, Morcellator, Reduced-port surgery, Transumbilical extraction
Introduction
Laparoscopic myomectomy (LM) is a common procedure. The technique with which the myoma is retrieved after LM is very important because it strongly influences the operative time.
Historically, it was common to use an electric motorized morcellator to retrieve the myoma. However, intracorporeal morcellation is associated with potentially severe complications1 including parasitic myoma and abdominal wall-related injuries. Additionally, the Food and Drug Administration (20140417) stated that intracorporeal morcellation can inadvertently spread cancerous tissue beyond the uterus and into other parts of the body.2,3
After this warning from the Food and Drug Administration, several myoma retrieval procedures were reported, such as in-bag morcellation,4,5 transvaginal extraction,6 transumbilical extraction,7,8,9,10,11 and lower abdominal incision.12 Before this warning, a power morcellator was commonly used in our institution. When the myoma was very small, it was retrieved from the umbilical scar without an electric motorized morcellator. The myoma was contained in a bag and morcellated by scissors and a scalpel. After the warning, we began to retrieve the myoma from the umbilical scar without an electric motorized morcellator during reduced-port surgery. The umbilical scar created during reduced-port surgery is longer (2.5–3.0 cm) than that created during conventional LM.
A few reports have compared the surgical outcomes of reducedport LM using transumbilical myoma extraction without an electric motorized morcellator with the outcomes of conventional LM.8,9 We believe that the specimen retrieval time is important for comparison of these two methods. To the best of our knowledge, only one study has compared the time required for transumbilical extraction without a power morcellator versus extraction with a power morcellator.9 Therefore, in the present study, we compared the surgical outcomes of these two methods with a special focus on the myoma retrieval time.
Aim
The aim of this study was to compare the surgical outcomes of LM using two myoma retrieval techniques: reduced-port transumbilical extraction without a morcellator and conventional extraction with a power morcellator. We paid special attention to the time required for myoma retrieval in each technique. Our goal was to determine whether transumbilical extraction without a morcellator can replace the use of an intracorporeal power morcellator.
Materials and methods
All patients who underwent LM in the Department of Obstetrics and Gynecology at Minoh City Hospital from January 2011 to December 2014 were included in this retrospective study. Institutional review board approval was waived because of the retrospective nature of the study. Informed consent was obtained from all patients prior to surgery and included permission to collect surgical information and use the patients’ specimens for the purpose of any study. The study protocol complied with the Declaration of Helsinki.
Estimation of myoma size
The largest diameter of each myoma was measured immediately before the operation by transvaginal ultrasonography.
Surgical technique
For conventional LM, two 12-mm trocars were placed in the umbilicus and left lower quadrant, and two 5-mm trocars were placed in the right lower quadrant and left upper quadrant. All resected myomas were morcellated and retrieved via the left lower quadrant trocar using the power morcellator (Ethicon Inc., NJ, USA) (Fig.1).
Fig. 1.
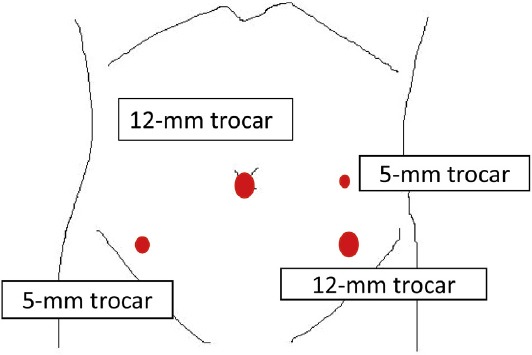
Conventional laparoscopic myomectomy.
For transumbilical retrieval, we used an EZ Access (Hakko Medical, Nagano, Japan), which has a silicon cap for the wound retractor (LAP PROTECTOR™; Hakko Medical) that makes it possible to insert multiple trocars without air leakage. The skin incision for insertion of the LAP PROTECTOR™ was 20–30 mm long. In single-port LM, three 5-mm trocars were inserted through the EZ Access; in two-port LM, two 5-mm trocars were inserted through the EZ Access and a 5-mm trocar was inserted in the left lower quadrant; and in three-port LM, two 5-mm trocars were inserted through the EZ Access and two 5-mm trocars were inserted in the right and left lower quadrants (Fig. 2).
Fig. 2.
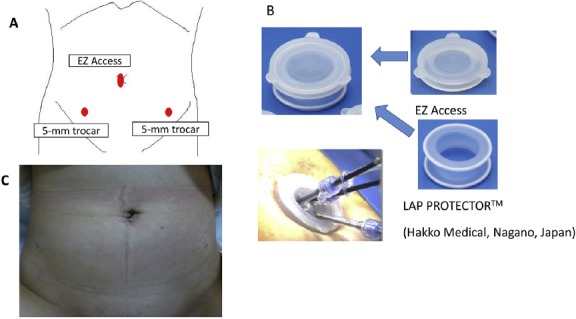
Single-, two-, or three-port laparoscopic myomectomy. (A) Trocar positions. (B) The LAP PROTECTOR™ is a wound retractor that requires a skin incision of 20–30 mm. The EZ Access (Hakko Medical, Nagano, Japan) is a silicon cap for the LAP PROTECTOR™ that makes it possible to insert multiple trocars without air leakage. (C) The umbilical and right and left lower quadrant incisions 1 month after laparoscopic myomectomy.
The detached myomas were contained in a specimen bag (EZ Purse; Hakko Medical) that was exteriorized at the umbilicus, morcellated with scissors and a scalpel, and retrieved through the umbilical incision.
The retrieval time was obtained from the nurse records and surgical videos. For morcellator extraction, it was defined as the duration of time from the start to end of morcellator use. For transumbilical extraction, it was defined as the duration of time from insertion of the specimen bag via the umbilical incision to retrieval of both the myomas and the specimen bag from the umbilical incision. The C-reactive protein concentration was measured on days 1 and 4 postoperatively, and the higher concentration was used in the analysis.
Statistical analysis
Statistical analysis was performed with Statcel 4 software (OMS Publishing, Saitama, Japan). The t test and Mann–Whitney U test were used to compare continuous variables sampled from a normal or non-normal distribution, respectively. Statistical significance was assumed when p < 0.05.
Results
Of 76 patients undergoing laparoscopic myomectomy, 2 were excluded because the weight of the largest myoma or the retrieval time was unknown. Thus, 74 patients were analyzed. Forty-five patients underwent transumbilical retrieval of the specimen without a power morcellator, and 29 patients underwent power morcellation. Fig. 3 shows the distribution of the specimen weights in the two groups. Among all 74 patients, the weight of the retrieved specimen and the weight of the largest myoma were significantly heavier and the size of the largest myoma was significantly larger in the power morcellation group than transumbilical group (p < 0.001) (Table 1). Table 2 shows the surgical outcomes of the 74 patients. The operative time and myoma retrieval time were significantly longer and the blood loss volume was significantly greater in the power morcellation group.
Fig. 3.
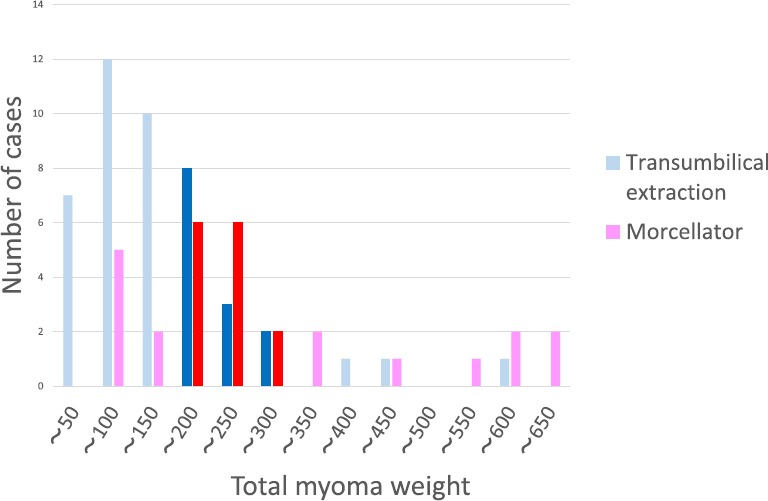
Number of cases according to weight of specimen.
Table 1.
Characteristics of all patients.
| U (n = 45) | M (n = 29) | p value | |
|---|---|---|---|
| Age (years) | 37.8 ± 5.1 (25–49) | 38.7 ± 4.4 (31–46) | 0.43 |
| Body mass index (kg/m2) | 22.0 ± 4.5 (17.2–42.3) | 21.3 ± 3.18 (17–27.6) | 0.63 |
| Weight of specimen (g) | 141.0 ± 111.1 (6–580) | 262.8 ± 173.3 (58–646) | p < 0.001 |
| Size of largest myoma (mm) | 60.3 ± 16.2 (6–90) | 74.7 ± 15.5 (50–100) | p < 0.001 |
| Weight of largest myoma (g) | 116.5 ± 80.5 (6–395) | 233.6 ± 142.9 (58–646) | p < 0.001 |
| Number of myomas | 2.13 ± 1.5 (1–7) | 2.3 ± 1.7 (1–7) | 0.60 |
Data are expressed as mean ± standard deviation (range).
M = power morcellator group.
U = transumbilical extraction group.
Table 2.
Surgery-related outcomes in all patients.
| U (n = 45) | M (n = 29) | p value | |
|---|---|---|---|
| Operative time (min) | 160.9 ± 65.5 (44–311) | 209.8 ± 55.7 (118–350) | 0.001 |
| Estimated blood loss (ml) | 155.4 ± 230.5 (10–967) | 287.5 ± 282.4 (5–1100) | 0.009 |
| Myoma retrieval time (min) | 18.1 ± 25.6 (1–172) | 28.37 ± 19.7 (6–69) | 0.002 |
| Postoperative CRP (mg/dl) | 2.78 ± 2.49 (0.15–11.5) | 3.30 ± 2.07 (0.75–11.0) | 0.055 |
Data are expressed as mean ± standard deviation (range).
M = power morcellator group.
U = transumbilical extraction group.
CRP = C-reactive protein.
Among patients whose specimen weight ranged from 101 to 300 g (n = 39), the weight (mean ± standard deviation) of the largest myoma was significantly heavier in the power morcellation group (194.0 ± 37.5 g; range, 120–254 g; n = 16) than in the transumbilical group (150.7 ± 60.5 g; range, 83–282 g; n = 23) (p = 0.02). The weight of the retrieved specimen (p = 0.06) and the size of the largest myoma (p = 0.10) were not significantly different between the two groups. With respect to perioperative details of the patients whose specimen weight ranged from 101 to 300 g, the operative time was significantly longer in the power morcellation group (208.8 ± 54.2 min; range, 139–350 min) than in the transumbilical group (169.8 ± 58.9 min; range, 44–298 min) (p = 0.04). There were no significant differences in blood loss volume, postoperative C-reactive protein concentration, or specimen retrieval time.
Among patients whose specimen weight ranged from 151 to 300 g, there were no significant differences in any demographic parameters or specimen weights between the groups at baseline (Table 3).
Table 3.
Characteristics of patients with a specimen weight of 151–300 g.
| U (n = 13) | M (n = 14) | p value | |
|---|---|---|---|
| Age (years) | 37.6 ± 4.1 (30–43) | 38.1 ± 4.2 (33–45) | 0.85 |
| Body mass index (kg/m2) | 20.8 ± 2.1 (17.2–23.8) | 21.1 ± 3.4 (17–31) | 0.80 |
| Weight of specimen (g) | 204.9 ± 41.6 (151–289) | 209.1 ± 32.1 (75.5–280) | 0.78 |
| Size of largest myoma (mm) | 72.5 ± 9.95 (61–90) | 75.5 ± 12.5 (50–96) | 0.52 |
| Weight of largest myoma (g) | 178.4 ± 64.8 (83–282) | 202.6 ± 29.7 (162–254) | 0.25 |
| Number of myomas | 3.15 ± 1.8 (1–7) | 2.43 ± 1.3 (1–6) | 0.23 |
Data are expressed as mean ± standard deviation (range).
M = power morcellator group.
U = transumbilical extraction group.
Our goal was to compare groups in which the weight of the retrieved myomas and weight and size of the largest myoma were not significantly different. Therefore, we chose patients whose specimen weight ranged from 151 to 300 g, not 101–300 g. This resulted in 13 patients in the transumbilical group and 14 patients in the power morcellation group. The diameter and weight of the largest myoma were 61–90 mm and 83–282 g in the transumbilical group and 50–96 mm and 162–254 g in the power morcellation group, respectively.
Table 4 shows the perioperative details. There were no significant differences in the operative time, blood loss volume, postoperative C-reactive protein concentration, or specimen retrieval time. No intraoperative or postoperative complications occurred in either group.
Table 4.
Surgery-related outcomes of patients with a specimen weight of 151–300 g.
| U (n = 13) | M (n = 14) | p value | |
|---|---|---|---|
| Operative time (min) | 189.0 ± 57.6 (87–298) | 211.1 ± 55.6 (151–350) | 0.38 |
| Estimated blood loss (ml) | 200.2 ± 250.6 (10–800) | 254.7 ± 255.4 (10–850) | 0.56 |
| Myoma retrieval time (min) | 21.5 ± 9.99 (7–41) | 21.1 ± 9.72 (7–43) | 0.92 |
| Postoperative CRP (mg/dl) | 2.40 ± 1.48 (0.28–3.31) | 3.03 ± 1.23 (0.75–5.07) | 0.26 |
Data are expressed as mean ± standard deviation (range).
M = power morcellator group.
U = transumbilical extraction group.
CRP = C-reactive protein.
Discussion
This study evaluated two approaches for myoma retrieval after LM. When the weight of the retrieved myomas was 151–300 g, the myoma retrieval time was not significantly different between the transumbilical and morcellation groups. Additionally, the surgical outcomes were similar between two- or three-port surgery using the EZ access to retrieve the specimen with a 2.5–3.0-cm umbilical incision and conventional LM with power morcellation.
In the present study, the specimen retrieval time was not significantly different between the two groups. In previous comparisons of specimen retrieval procedures, the operation time was usually assessed.7,8 We found only three studies in which the retrieval time was also assessed. In these studies, transvaginal retrieval,6 transumbilical retrieval during single-site myomectomy,9 and retrieval from a lower abdominal incision12 without a power morcellator were compared with power morcellation. In the latter two studies,9,12 the retrieval time was similar in the two groups and the size of the myomas was assessed using the diameter. Myomas are usually assessed using the maximum diameter of the largest myoma. However, myomas are not spherical in shape; therefore, it is difficult to compare the myoma volume using the diameter. In our study, the specimens were estimated by weight. We believe that use of the weight is more reliable.
The weight of a myoma cannot be practically determined preoperatively; therefore, the diameter of the largest myoma may be more useful than the weight of the specimen. In the present study, the diameter of the largest myoma was also analyzed. When the specimen weight was ≤300 g, the maximum diameter of the largest myoma was 96 mm. Therefore, we believe that our transumbilical method is useful when the diameter of the largest myoma is ≤9 cm. Preoperative assessment of the volume of a myoma is difficult. To the best of our knowledge, only one study estimated the uterine weight preoperatively.13 The study revealed a strong correlation between the weight of the removed uterus and the value of a × b × c for each individual uterus, where a = the maximum longitudinal diameter in the sagittal section, b = the maximum lateral diameter, and c = the maximum longitudinal diameter in the transverse section. Further investigation is necessary for preoperative assessment of the myoma volume.
Previous studies have shown no significant difference in surgical outcomes between single-port myomectomy and conventional LM.7,9 In the present study, there were no significant differences in surgical outcomes between reduced-port myomectomy (two- or three-port technique), which involved retrieval of the specimen through the EZ Access and a 2.5–3.0-cm umbilical incision, and conventional LM with power morcellation (four-port technique). In one study, single-site LM was technically more challenging for surgeons than conventional laparoscopy; therefore, the authors did not recommend routine performance of single-site LM.9 However, in contrast to single-port surgery, the operator’s forceps do not interfere with each other in two- or three-port surgery. Therefore, two- or three-port surgery does not require a degree of skill as high as that required in single-port myomectomy. In three-port surgery, the assistant can use forceps and assist the operator. Pulling myomas from an umbilical port makes it easier to enucleate them than pulling them from a lower abdominal port. The expected benefit of transumbilical myoma retrieval through a LAP PROTECTOR is easier specimen extraction. In addition, scissors or scalpel morcellation within a bag decreases the risk of specimen dissemination.9
The Food and Drug Administration (20140417) stated that intracorporeal morcellation can inadvertently spread cancerous tissue beyond the uterus and into other parts of the body.2,3 A previous meta-analysis showed a significant correlation between uterine morcellation and an increased risk of intra-abdominal recurrence in patients affected by unexpected uterine leiomyosarcoma.14 Recently published studies have revealed potential detrimental effects of morcellation not only for leiomyosarcoma but also for smooth muscle tumors of uncertain malignancy.15,16 A preoperative diagnosis of uterine sarcoma is important. However, it is currently impossible to diagnose unexpected uterine sarcoma with 100% accuracy.17 Therefore, based on the currently available data, intra-abdominal morcellation should be avoided. However, minimally invasive surgery should not be banned.18,19 It is necessary to devise better myoma retrieval methods that can replace intra-abdominal power morcellation.
Identification of the optimal myoma retrieval method is a crucial problem. Many methods have been described, including the conventional method using power morcellation, in-bag morcellation at the umbilical site,4,5 and transvaginal retrieval with or without a power morcellator.6 Some studies have reviewed transvaginal specimen retrieval after operative laparoscopy.20,21 In comparison of the transumbilical and transvaginal techniques, the transvaginal approach for specimen removal after laparoscopic resection of adnexal masses offers the advantage of less postoperative pain than that associated with transumbilical retrieval.20 A previous retrospective analysis and systematic review of the literature reported that transvaginal specimen retrieval after operative laparoscopy is a safe, feasible, and applicable technique.21 However, we prefer transumbilical specimen retrieval because with transvaginal retrieval, an additional wound is needed and the visual field is less adequate. Our data suggest that transumbilical myoma retrieval is easy and safe.
This was a retrospective study, and the number of cases was small. Additionally, the retrieval time of one myoma should be compared. However, there were no records for individual myomas; therefore, the retrieval time of all specimens was compared. The operation time and blood loss volume differed according to the weight, number, and position of the myomas. Additionally, the number of ports (two-port or three-port LM) and operators (these operations were performed by four operators) may have affected the perioperative outcomes. In the present study, however, these conditions were not considered.
In conclusion, two or three-port LM with the EZ Access and transumbilical retrieval of specimens weighing 151–300 g provides perioperative outcomes similar to those of the conventional method with power morcellation. Transumbilical retrieval reduces the risk of tissue dissemination and is cost-effective. The American Association of Gynecologic Laparoscopists Position Statement recommended improvement, not abandonment, of power morcellation.22 However, a randomized study comparing transumbilical retrieval and intracorporeal power morcellation is almost impossible. We believe that the herein-described technique of LM with the EZ Access is a feasible method for specimens weighing up to 300 g and can replace intracorporeal power morcellation.
Footnotes
Conflicts of interest: The authors have no conflicts of interest relevant to this article.
References
- 1.Buckley VA, Nesbitt-Hawes EM, Atkinson P, et al. Laparoscopic myomectomy: clinical outcomes and comparative evidence. J Minim Invasive Gynecol. 2015;22:11–25. doi: 10.1016/j.jmig.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Lieng M, Berner E, Berner E, Busund B. Risk of morcellation of uterine leiomyosarcomas in laparoscopic supracervical hysterectomy and laparoscopic myomectomy, a retrospective trial including 4791 women. J Minim Invasive Gynecol. 2015;22:410–414. doi: 10.1016/j.jmig.2014.10.022. [DOI] [PubMed] [Google Scholar]
- 3.Chin H, Ng XHA, Chern SMB. Power morcellation-An emerging risk complicating minimally invasive surgery for uterine mesenchymal neoplasms. Gynecol Minim Invasive Ther. 2016;5:109–111. [Google Scholar]
- 4.Kanadae TT, McKenna JB, Choi S, et al. Sydney contained in bag morcellation for laparoscopic myomectomy. J Minim Invasive Gynecol. 2014;21:981. doi: 10.1016/j.jmig.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Vargas MV, Cohen SL, Fuchs-Weizman N, et al. Open power morcellation versus contained power morcellation within an insufflated isolation bag: comparison of perioperative outcomes. J Minim Invasive Gynecol. 2015;22:433–438. doi: 10.1016/j.jmig.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Bogani G, Uccella S, Cromi A, et al. Electric motorized morcellator versus transvaginal extraction for myoma retrieval after laparoscopic myomectomy: a propensity-matched analysis. J Minim Invasive Gynecol. 2014;21:928–934. doi: 10.1016/j.jmig.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Kim SK, Lee JH, Lee JR, et al. Laparoendoscopic single-site myomectomy versus conventional laparoscopic myomectomy: a comparison of surgical outcomes. J Minim Invasive Gynecol. 2014;21:775–781. doi: 10.1016/j.jmig.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Kim JY, Kim KH, Choi JS, Lee JH. A prospective matched case-control study of laparoendoscopic single-site vs conventional laparoscopic myomectomy. J Minim Invasive Gynecol. 2014;21:1036–1040. doi: 10.1016/j.jmig.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 9.Song T, Kim TJ, Lee SH, Kim TH, Kim WY. Laparoendoscopic single-site myomectomy compared with conventional laparoscopic myomectomy: a multicenter, randomized, controlled trial. Fertil Steril. 2015;104:1324–1331. doi: 10.1016/j.fertnstert.2015.07.1137. [DOI] [PubMed] [Google Scholar]
- 10.Yuk JS, Ji HY, Kim KH, Lee JH. Single-port laparoscopically assisted-transumbilical ultraminilaparotomic myomectomy (SPLA-TUM) versus single port laparoscopic myomectomy: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2015;188:83–87. doi: 10.1016/j.ejogrb.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Lee JR, Lee JG, Kim JY, Chang HJ, Suh CS, Kim SH. Single port laparoscopic myomectomy with intracorporeal suture-tying and transumbilical morcellation. Eur J Obstet Gynecol Reprod Biol. 2014;181:200–204. doi: 10.1016/j.ejogrb.2014.07.051. [DOI] [PubMed] [Google Scholar]
- 12.Venturella R, Rocca ML, Lico D, et al. In-bag manual versus uncontained power morcellation for laparoscopic myomectomy: randomized controlled trial. Fertil Steril. 2016;105:1369–1376. doi: 10.1016/j.fertnstert.2015.12.133. [DOI] [PubMed] [Google Scholar]
- 13.Shiota M, Kotani Y, Umemoto M, TObiue T, Hoshiai H. Estimation of preoperative uterine weight in uterine myoma and uterine adenomyosis. Asian J Endosc Surg. 2012;3:123–125. doi: 10.1111/j.1758-5910.2011.00130.x. [DOI] [PubMed] [Google Scholar]
- 14.Bogani G, Cibly WA, Aletti GD. Impact of morcellation on survival outcomes of patients with unexpected uterine leiomyosarcoma: a systematic review and meta-analysis. Gynecol Oncol. 2015;137:167–172. doi: 10.1016/j.ygyno.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Bogani G, Ditto A, Martinelli F, et al. Morcellator's port-site metastasis of a uterine smooth muscle tumor of uncertain malignant potential after minimally invasive myomectomy. J Minim Invasive Gynecol. 2016;23:647–649. doi: 10.1016/j.jmig.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 16.Raspagliesi F, Maltese G, Bogani G, et al. Morcellation worsens survival outcomes in patients with undiagnosed uterine leiomyosarcomas: a retrospective MITO group study. Gynecol Oncol. 2017;144:90–95. doi: 10.1016/j.ygyno.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Bogani G, Chiappa V, Ditto A, et al. Morcellation of undiagnosed uterine sarcoma: a critical review. Crit Rev Oncol Hematol. 2016;98:302–308. doi: 10.1016/j.critrevonc.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 18.Bogani G, Chiappa V, Ditto A, et al. Morcellation of apparent benign uterine yoma: assessing risk to benefit ratio. J Gynecol Oncol. 2016;27:e37. doi: 10.3802/jgo.2016.27.e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bogani G, Serati M, Uccella S, Chezzi F. In-bag morcellation for presumed myoma retrieval at laparoscopy. Cancer. 2014;24:4004–4005. doi: 10.1002/cncr.28959. [DOI] [PubMed] [Google Scholar]
- 20.Ghezzi F, Cromi A, Ucella S, Bogani G, Serati M, Bolis P. Transumbilical versus transvaginal retrieval of surgical specimens at laparoscopy: a randomized trial. Am J Obstet Gynecol. 2012;207:112.e1–112.e6. doi: 10.1016/j.ajog.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 21.Ucella S, Cromi A, Bogani G, Casarin J, Serati M, Ghezzi F. Transvaginal specimen extraction at laparoscopy without concomitant hysterectomy: our experience and systematic review of the literature. J Minim Invasive Gynecol. 2013;20:583–590. doi: 10.1016/j.jmig.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 22.Brown J. AAGL advancing minimally invasive gynecology worldwide: Statement to the FDA on power morcellation. J Minim Invasive Gynecol. 2014;21:970–971. doi: 10.1016/j.jmig.2014.08.780. [DOI] [PubMed] [Google Scholar]


