Abstract
Ureteral involvement is rare, with an estimated frequency of 10–14% in cases of deep infiltrating endometriosis. An important complication of ureteral involvement is asymptomatic loss of renal function. We reported that a 49-year-oId woman presented with chronic pelvic pain due to severe dysmenorrhea and without any urological symptoms. Magnetic resonance imaging (MRI) identified a 7 cm endometrioma compressing and infiltrating the rectal wall, and chronic left hydronephrosis. Isotope renogram decreased 14% function in the left kidney. We performed adhesiolysis, freeing of the uterus and appendages, hysterectomy, bilateral oophorectomy. However, we performed only to resect a part of left deep infiltrating endometriosis with ureteral involvement to avoid ureteral injury. After surgery, hydronephrosis was improved and those endometriosis left was not enlarged after 1 years of follow-up. We have to consider bilateral oophorectomy since endometriosis develops by the estrogen-dependent and it may decrease reproductive hormone derived from ovary.
Keywords: Deep infiltrating endometriosis, Hydronephrosis, Laparoscopy, Peri-menopausal women
Introduction
Endometriosis is a common condition that affects as many as 10%–20% of women of reproductive age.1 Endometrial implants are observed most commonly on the ovaries, and in the anterior and posterior cul-de-sacs, broad ligaments, and uterosacral ligaments.2 Commonly, most patients have pelvic pain. However, urinary tract complications are uncommon, occurring in approximately 1–2% of affected patients.3 Medical treatment of fibrotic tissue secondary to endometriosis is ineffective. Laparoscopy is a reasonable choice for treatment of severe pelvic endometriosis, assuming that the surgeon is highly skilled in this technique as laparoscopic radical hysterectomy.4 We report a patient with hydronephrosis by severe left urinary tract endometriosis and asymptomatic loss of renal function that was initially managed laparoscopically.
Case report
This case report was approved by Nasu red cross hospital institutional review board. The informed consent of this case report and associated images was obtained from the patient for the publication.
A 49-year-old woman, gravida 2, para 0, came to our hospital for the screening of uterine cervical cancer once a year. Her menstrual cycle is regular. She chronically had symptoms of pelvic pain, dysmenorrhea and hypermenorrhea. T2-weighted magnetic resonance imaging (MRI) showed a 8 cm uterine fibroid, a 7 cm left ovarian endometrioma and uterosacral ligament endometriosis infiltrating the rectal wall (Fig. 1). Coronal section T1-weighted MRI with fat-saturation after contrast medium enhancement showed a left hydroureter (Fig. 1). There was no ascites. Her serum level of both cancer antigen (CA) 125; 115.0 U/ml and 19-9; 76.1 U/ml was elevated. Computed tomography (CT) of the abdomen revealed the left ureter and hydronephrosis (Fig. 1). 3D volume rendered images created from CT urography showed left proximal ureteral obstruction (Fig. 1). The renogram (99mTc-MAG3) showed a residual renal function of 14% in the left kidney and 86% in the right kidney (Fig. 1). Endometriotic lesion was suspected of causing periureteral compression. Cystourethroscopy showed external compression 2 cm above the ureteral orifice. There was no evidence of disease within the urinary tract itself. A ureteral catheter was inserted with mild difficulty.
Fig. 1.
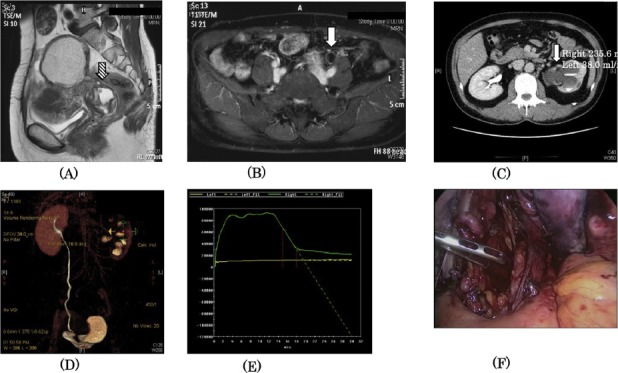
Colonel T2-W1 MRI shows (A) endometrioma and strong adhesion between posterior wall of uterus and rectum (hatched arrow) and (B) the left hydroureter (white arrow). (C) CT scan axial view shows hydronephrosis (white arrow) in left kidney. (D) 3D volume rendered images created from Computed tomography urography doesn’t show the imaging of left ureter, however detects left renal cortex. (E) In 99mTc-mercaptoacetyltriglycine (99mTc-MAG3) renogram, the effective renal plasma flow of the left kidney markedly decreased and showed no peak curve. (F) Laparoscopic view demonstrating left ureter (white arrow) above the level of the uterosacral ligament (hatched arrow), which is infiltrated by endometriosis.
The preoperative diagnosis was left ovarian endometrioma with deep infiltrating endometriosis and a leiomyoma.
The patient was evaluated and discussed by a multidisciplinary team including urology. The proposed treatment was a laparoscopic approach to perform adhesiolysis, liberation and resection of the uterus and appendages, the rectovaginal septum nodule. When it is difficult to preserve left ureter laparoscopically, left nephrectomy would be additionally performed. The patient was informed of the risks of the procedure and she received informed consent. She was made aware of the possible need for nephrectomy, depending upon the extent of disease.
During laparoscopy, we found a frozen pelvis with significant adherence syndrome. The left ureter was entrapped by an endometriotic nodule that also affected the left uterosacral ligament (Fig. 1). The left uterosacral ligament had dense adhesions which were separated by blunt dissection. The retroperitoneal space was opened above the ureter and ureterolysis was performed by blunt dissection. The uterosacral ligament and a pararectal space were identified. The ureter was pushed downward and laterally. The uterine artery was also identified to prevent injury during ureterolysis. Ureterolysis was performed to a point below the uterine artery, but this creation of a ureteral tunnel had to be stopped because of injury to the descending uterine vessels. The bleeding was stopped by bipolar electrocauterization. It was extremely difficult to divide the space of where left ureter was involved into deep infiltrating endometriosis because of the intensive adhesion because there are two reasons why we estimated that its endometriosis might be regressed by the bilateral oophorectomy and needed to avoid ureteral injury.
We also resected the left endometrioma and uterus including leiomyoma. The resected specimen was delivered through the opened vaginal vault. The incised vaginal vault was closed with laparoscopically placed absorbable sutures. The patient was hospitalized for a total of seven days and her subsequent clinical course was excellent.
Postoperatively, the ureteral catheter was removed 2 months postoperatively. Then, CT scan revealed the improvement of hydronephrosis, so called mild hydronephrosis, compared to preoperation (Fig. 2). While mild hydronephrosis was left, that was not enlarged after 1 years of follow-up.
Fig. 2.

CT scan axial view improves hydronephrosis (white arrow) in left kidney.
Discussion
Deep infiltrating endometriosis is defined as lesions penetrating surrounding tissue by 5 mm or more5 and is likely of multifactorial origin. It can affect both genital and extragenital organs. Of these, the most frequently involved are the large intestine and urinary tract. Patients usually present with multiple symptoms including abdominal pain, dysmenorrhea, chronic pelvic pain, dyspareunia, dyschezia and other digestive and urinary symptoms. The goal of treatment is to improve the patient’s quality of life.
The surgical approach is often complex for various reasons, including the intrinsic difficulty of treating endometriosis and the previous (often laparoscopic) surgeries resulting in adhesions and anatomic distortion. This requires the participation of expert laparoscopic surgeons with wide experience in this disease. In our case, there was hypermenorrhea and dysmenorrhea. On the other hand, there were no symptoms as any urinary trouble despite of loss of renal function. Jadoul et al reported that the risk of loss of renal function in cases of ureteral endometriosis is 11.5%.6 Whereas, there are some cases reported with silent ureteral involvement in the context of deep infiltrating endometriosis,7,8 as occurred in our patient. When renal function is below 14%, there is a risk of pyelonephritis and renovascular hypertension, and nephrectomy is recommended. Our patient had a left renal function of 14%. It is important to call the attention of professionals who treat these patients with deep infiltrating endometriosis to the possibility of silent ureteral involvement, using imaging tests to diagnose this eventuality and resolving the obstruction surgically before loss of renal function. Generally, MRI is very useful for guiding laparoscopy, and fat-saturation MRI is more accurate in the diagnosis of pelvic endometriosis.9,10 Our patient had irregular infiltration of the pelvic sidewall with strong enhancement, indicating peritoneal endometriosis, a finding confirmed at laparoscopy. Deeply penetrating endometriosis generally requires surgery. Chapron and Dubuisson reported that laparoscopic surgery is efficacious for the treatment of deep infiltrating endometriosis.4 However, they also cautioned that retroperitoneal infiltration may substantially modify the normal anatomic relationships and, hence, laparoscopy must be performed with great care. In fact, they could extend the ureterolysis below the uterine artery and completely remove deep infiltrating endometriosis. In further severe cases, if stenosis is evident but limited to the ovarian fossa and distal ureter can be preserved, then ureteral resection and end-to-end anastomosis can be performed over a ureteral stent. Surgical approach is changed if the ureteral stenosis is close to the vesicoureteral junction and is extensive. The ureter is resected before the area of disease, and the proximal end is reimplanted into the bladder. However, advanced surgical techniques that are comparable with laparoscopic radical hysterectomy are required.
In our case, we created a pararectal space to identify the uterosacral ligament, and the uterine artery was also carefully identified to prevent injury. However, we could not extend the ureterolysis below the uterine artery as their procedure. We did not try to remove whole deep infiltrating endometriosis for the purpose of avoiding nephrectomy because we inferred that deep infiltrating endometriosis would be diminished by the influence of bilateral ovarian resection which means that reproductive hormone is lacked such as menopause. Optionally, that patient didn’t hope to take any medication after surgery though we could choose to resect only left endometrioma and use hormone therapy such as dienogest after surgery. Consequently, we technically made an effort to preserve the left urinary tract to avoid nephrectomy.
In conclusion, our case illustrates that even in the absence of symptoms, deep infiltrating endometriosis may seriously affect surrounding structures, in particular the urinary tract. MRI and the renogram may help to diagnose pelvic endometriosis and the renal function before surgery. While laparoscopy may be adequate in the hands of a skilled operator, chronic inflammation with fibrosis may not be amenable to this less invasive technique. In patient without fertile preservation, we do not dare to try to resect whole endometriosis completely because endometriosis left would be degraded by the bilateral oophorectomy that decrease the level of reproductive hormone such as menopause.
Footnotes
Conflict of interest: The authors have no conflict of interest relevant to this article.
References
- 1.Frenna V, Santos L, Ohana E, Bailey C, Wattiez A. Laparoscopic management of ureteral endometriosis: our experience. J Minim Invasive Gynecol. 2007;14:169–171. doi: 10.1016/j.jmig.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Adamson GD. Diagnosis and clinical presentation of endometriosis. Am J Obstet Gynecol. 1990;162:568–569. doi: 10.1016/0002-9378(90)90431-6. [DOI] [PubMed] [Google Scholar]
- 3.Denes FT, Pompeo AC, Montelatto NI, Lopes RN. Ureteral endometriosis. Int Urol Nephrol. 1980;12:205–209. doi: 10.1007/BF02217137. [DOI] [PubMed] [Google Scholar]
- 4.Chapron C, Dubuisson JB. Laparoscopic treatment of deep endometriosis located on the uterosacral ligaments. Hum Reprod. 1996;11:868–873. doi: 10.1093/oxfordjournals.humrep.a019268. [DOI] [PubMed] [Google Scholar]
- 5.Cornillie FJ, Oosterlynck D, Lauweryns JM, Koninckx PR. Deeply infiltrating pelvic endometriosis: histology and clinical significance. Fertil Steril. 1990;53:978–983. doi: 10.1016/s0015-0282(16)53570-5. [DOI] [PubMed] [Google Scholar]
- 6.Jadoul P, Feyaerts A, Squifflet J, Donnez J. Combined laparoscopic and vaginal approach for nephrectomy, ureterectomy, and removal of a large rectovaginal endometriotic nodule causing loss of renal function. J Minim Invasive Gynecol. 2007;14:256–259. doi: 10.1016/j.jmig.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Seracchioli R, Mabrouk M, Manuzzi L, et al. Importance of retroperitoneal ureteric evaluation in cases of deep infiltrating endometriosis. J Minim Invasive Gynecol. 2008;15:435–439. doi: 10.1016/j.jmig.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Carmignani L, Vercellini P, Spinelli M, Fontana E, Frontino G, Fedele L. Pelvic endometriosis and hydroureteronephrosis. Fertil Steril. 2010;93:1741–1744. doi: 10.1016/j.fertnstert.2008.12.038. [DOI] [PubMed] [Google Scholar]
- 9.Zanardi R, Del Frate C, Zuiani C, Del Frate G, Bazzocchi M. Staging of pelvic endometriosis using magnetic resonance imaging compared with the laparoscopic classification of the American Fertility Society: a prospective study. Radiol Med. 2003;105:326–338. [PubMed] [Google Scholar]
- 10.Ha HK, Lim YT, Kim HS, Suh TS, Song HH, Kim SJ. Diagnosis of pelvic endometriosis: fat-suppressed T1-weighted vs conventional MR images. AJR Am J Roentgenol. 1994;163:127–131. doi: 10.2214/ajr.163.1.8010198. [DOI] [PubMed] [Google Scholar]


