Abstract
Study Objective:
To investigate the use of operative hysteroscopy instead of traditional curettage in women with retained products of conception (RPOC) following first trimester medical abortion, with the aim of reducing post-operative intrauterine adhesions.
Design:
Retrospective study.
Setting:
Gynecology department in a University affiliated hospital.
Patients:
All women treated by hysteroscopy for RPOC following first trimester medical abortion using the mifepristone-misoprostol protocol for pregnancy termination or the misoprostol protocol for early missed abortion from January 2013 to August 2016.
Intervention:
Operative hysteroscopy for removal of RPOC. Post-operative intrauterine adhesions were assessed by diagnostic office hysteroscopy after 6–8 weeks.
Measurements and Main Results:
50 cases were identified. The mean time from medication administration to the operative hysteroscopy was 1.7 ± 0.7 months. Operative hysteroscopy with blunt use of the resectoscopic loop was used to remove all specimens, and all procedures were completed without intra-operative complications. Two patients (4.0%) were readmitted for fever. Pathology confirmed the presence of RPOC in 45 (90.0%) cases. On follow-up office hysteroscopy, a normal uterine cavity without evidence of intrauterine adhesions was seen in 29/29 (100%) women.
Conclusion:
Hysteroscopy for removal of RPOC following medical abortion is associated with low rates of complications and post-operative intrauterine adhesions.
Keywords: abortion, hysteroscopy, intrauterine adhesions, retained products of conception
Introduction
Medical abortion for first trimester pregnancy termination using the mifepristone-misoprostol protocol or for medical treatment of early pregnancy failure (missed abortion) using misoprostol is effective in up to 98% of cases and up to 90% of cases, respectively.1,2,3 For those women with incomplete expulsion of the pregnancy, uterine evacuation may be indicated. This procedure may be performed with suction curettage, or by operative hysteroscopy, which is increasingly used for treatment of retained products of conception (RPOC) following delivery or different types of abortions.4 The advantages of hysteroscopy over curettage in this setting are visualization of the uterine cavity allowing complete removal of the RPOC, “targeted” as opposed to “global” curettage of the uterine walls, and theoretically reduced trauma to the uterine walls leading to reduced rates of post-operative intrauterine adhesions.5 Since many of the patients undergoing medical abortion are young women who will likely wish to conceive in the future, the prevention of intrauterine adhesions which could affect fertility is of prime importance in this population.
Previous studies describing the use of hysteroscopy for treatment of RPOC following different types of deliveries and abortions have included a small number of cases who were treated for RPOC after medical abortion,5,6 but no study to date specifically described the surgical short and long term outcomes of operative hysteroscopy in this group.
The aim of this study is to describe the use of hysteroscopy for removal of RPOC following medical abortion with emphasis on the prevalence of post-operative intrauterine adhesions.
Methods
The department’s computerized database of surgical procedures was searched for cases treated by operative hysteroscopy for removal of RPOC. Of those, we identified cases whose RPOC occurred following medical abortion. Their medical records were reviewed and information on their obstetrical history, clinical presentation, surgical procedure, post-operative follow-up and pathology report was retrieved. All patients were referred for surgery for suspected RPOC after clinical and ultrasound evaluation by their referring gynecologist.
Hysteroscopy for removal of RPOC was performed under general anesthesia. The cervix was dilated with Hegar’s dilators up to 9.5 mm. Using NaCl 0.9% solution as a distension media, the Versapoint resectoscope (Gynecare, Ethicon Endo surgery, Somerville, NJ, USA) fitted with a 2.5 mm or a 4-mm electrosurgical bipolar loop was introduced into the uterine cavity, and the intrauterine findings suspected as RPOC were gently separated from the uterine wall using the loop as a curette. The use of bipolar electro-surgery was minimized as much as possible to avoid causing thermal damage to the endometrium (Supplemental video shows full length procedure). After the mass was separated from the uterine wall completely, a polyp forceps was used to extract it. Perioperative antibiotics were prescribed. All specimens were evaluated for the presence of RPOC by a pathologist (see Fig. 1).
Fig. 1.
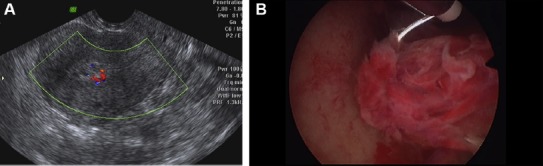
A. Ultrasound exam of a 29 years old gravida 3 para 2 woman, 2 months after medical abortion. An echogenic uterine mass measuring 18*9 mm with color Doppler flow is seen. Pathology confirmed the presence of RPOC. B. Hysteroscopic picture of the same patient. A uterine mass attached to the right uterine wall is seen.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.gmit.2017.05.002
In accordance with our departmental protocol for treatment of RPOC, an office hysteroscopy follow-up (aimed to diagnose postoperative intrauterine adhesions) was recommended 6–8 weeks after the operative hysteroscopy. The timing of the post-operative hysteroscopy was determined according to previous studies on the occurrence of post-operative intrauterine adhesions.7,8 The hysteroscopic findings on that follow up hysteroscopy were classified according to the European Society of Gynecologic Endoscopy (ESGE) classification for intrauterine adhesions.9
Statistical analysis was performed with SPSS software (Version 20, IBM Corp.). Descriptive variables are presented as mean ± standard deviation or as median (range). Frequencies were compared with the Chi square test. Means and medians were compared with the Student T test or with the ANOVA test as appropriate. A p value > 0.05 was considered statistically significant.
The study was approved by the Institutional Review Boards. Since this was a retrospective study reviewing data from medical records, patients’ informed consent was not required.
Results
The study included 50 patients, of whom 26 were treated for RPOC following first trimester medical abortion with mifepristone-misoprosol and 24 were treated for RPOC following misoprostol treatment for early pregnancy failure. Their demographic, gynecologic and clinical characteristics are shown in Table 1. Women in the RPOC following early pregnancy failure group were significantly older than women in the RPOC following medical induced abortion group, but their gravidity and parity were similar (Table 1). The mean time from medication administration to the operative hysteroscopy for RPOC removal was 1.7 ± 0.8 months. At time of surgery, 33 (66.0%) patients reported persistent vaginal bleeding, 4 (8.0%) were hospitalized for fever and suspected pelvic inflammatory disease, and 13 (26.0%) were asymptomatic. Those 4 patients who presented with fever were hospitalized for treatment with intravenous antibiotics, while the remaining cases were treated as outpatients.
Table 1.
The demographic, gynecologic, and clinical characteristics of the study patients.
| Parameter | Whole cohort (N = 50) | RPOC following medical pregnancy termination (N = 26)a | RPOC following medical treatment of early pregnancy failure (N = 24)b | p value |
|---|---|---|---|---|
| Age (years) | 27.8 ± 7.7 | 23.5 ± 6.7 | 32.5 ± 5.6 | <0.01 |
| Gravidity | 2 (1–8) | 1 (1–8) | 2 (1–5) | 0.1 |
| Parity | 0 (0–6) | 0 (0–6) | 1 (0–4) | 0.07 |
| Past cesarean section | 8 (16.0) | 2 (7.7) | 6 (25.0) | 0.1 |
| Vaginal bleeding | 33 (66.0) | 17 (65.4) | 16 (66.7) | 0.6 |
| Clinical presentation | ||||
| Fever | 4 (8.0) | 3 (11.5) | 1 (4.2) | 0.3 |
| Asymptomatic | 13 (26.0) | 6 (23.1) | 7 (29.2) | 0.4 |
| Size of RPOC finding on hysteroscopy (cm) | 2.1 ± 0.1 | 2.1 ± 0.6 | 2.1 ± 0.9 | 0.8 |
Data is presented as mean ± standard deviation, median (range) or number (%).
a Retained products of conception (RPOC) diagnosed after medical treatment with mifepristone-misoprostol for first trimester pregnancy termination.
b RPOC diagnosed following treatment with misoprostol for early pregnancy failure (early missed abortion).
All findings were removed hysteroscopically, and no intra-operative complications occurred. The mean RPOC specimen size on hysteroscopy was 2.1 ± 0.1 cm (Table 1). The post-operative complications included two (4.0%) re-admissions for postoperative fever. Both patients were discharged after a short course of intravenous antibiotics. On pathology, RPOC were confirmed in 45/90 (90.0%) cases. Twenty-nine patients presented for follow up office hysteroscopy. A normal uterine cavity without evidence of intrauterine adhesions was seen in all cases.
Discussion
The main drawback of the medical treatment for early induced abortion (using the mifepristone-misoprostol protocol) and for early pregnancy failure (using the misoprostol protocol) is the need for uterine curettage in cases of incomplete abortion, which may be required in up 5% of cases.1,2,3 This surgical procedure may be associated with immediate complications (i.e. infection, bleeding and rarely uterine perforation) and with the long term complication of intrauterine adhesions, which in severe cases may cause infertility. To date, the rate of intrauterine adhesions following curettage for incomplete medical abortion is unknown. However, curettage performed in the setting of RPOC (following delivery or abortion) may be complicated by intrauterine adhesions in 40%–60% of cases.10,11 In young women who are likely to desire future pregnancies, this complication with its implications on fertility could be significant. In this study, we described low rates of complications and post-procedure intrauterine adhesions in a small cohort of patients in whom post-abortion RPOC were removed hysteroscopically.
The recommended timing for uterine evacuation in cases of incomplete expulsion of pregnancy following medical abortion varies widely in the literature.12 In low resources areas where ultrasound follow up is not available, clinical and/or human chorionic gonadotropin measurements are used to determine pregnancy expulsion and RPOC may not be diagnosed at all in this setting. In other countries where clinical and ultrasound follow up are widely available, different follow up periods to determine post-abortion RPOC were suggested, ranging from 6 weeks after medication administration to much longer periods of several months.
The hysteroscopic morcellator has been recently studied as an alternative surgical treatment option for women with RPOC.13 This procedure has been advocated as “safer” than the traditional operative hysteroscopy. Hamerlynck et al13 reported the outcomes of 105 RPOC cases managed with hysteroscopic morcellation. In their cohort, 6 adverse events occurred, including 4 uterine perforations. Thus, further studies are needed to compare the outcomes of hysteroscopic morcellation and operative hysteroscopy.
The current study is limited by its small number of cases and its retrospective design. In addition, operative hysteroscopy may not be available to all patients requiring uterine evacuation for incomplete medical abortion, because of its high cost and need for surgeon’s experience. Thus, our findings may not be applicable to many women undergoing medical abortion in low resources areas.
In conclusion, hysteroscopy allows for removal of RPOC following medical abortion. This procedure is associated with low rates of intra- and post-operative complications as well as low rates of post-procedure intrauterine adhesions.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest relevant to this article.
References
- 1.Raymond EG, Shannon C, Weaver MA, Winikoff B. First-trimester medical abortion with mifepristone 200 mg and misoprostol: a systematic review. Contraception. 2013;8:26–37. doi: 10.1016/j.contraception.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 2.Spitz IM, Bardin CW, Benton L, Robbins A. Early pregnancy termination with mifepristone and misoprostol in the United States. N Engl J Med. 1998;338:1241–1247. doi: 10.1056/NEJM199804303381801. [DOI] [PubMed] [Google Scholar]
- 3.Colleselli V, Nell T, Bartosik T, et al. Marked improvement in the success rate of medical management of early pregnancy failure following the implementation of a novel institutional protocol and treatment guidelines: a follow-up study. Arch Gynecol Obstet. 2016;294:1265–1272. doi: 10.1007/s00404-016-4179-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smorgick N, Barel O, Fuchs N, Ben-Ami I, Pansky M, Vaknin Z. Hysteroscopic management of retained products of conception: meta-analysis and literature review. Eur J Obstet Gynecol Reprod Biol. 2014;173:19–22. doi: 10.1016/j.ejogrb.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 5.Barel O, Krakov A, Pansky M, Vaknin Z, Halperin R, Smorgick N. Intrauterine adhesions after hysteroscopic treatment for retained products of conception: what are the risk factors? Fertil Steril. 2015;103:775–779. doi: 10.1016/j.fertnstert.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 6.Golan A, Dishi M, Shalev A, Keidar R, Ginath S, Sagiv R. Operative hysteroscopy to remove retained products of conception: novel treatment of an old problem. J Minim Invasive Gynecol. 2011;18:100–103. doi: 10.1016/j.jmig.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Kim T, Ahn KH, Choi DS, et al. A randomized, multi-center, clinical trial to assess the efficacy and safety of alginate carboxymethylcellulose hyaluronic acid compared to carboxymethylcellulose hyaluronic acid to prevent postoperative intrauterine adhesion. J Minim Invasive Gynecol. 2012;19:731–736. doi: 10.1016/j.jmig.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Thubert T, Dussaux C, Demoulin G, Rivain AL, Trichot C, Deffieux X. Influence of auto-cross-linked hyaluronic acid gel on pregnancy rate and hysteroscopic outcomes following surgical removal of intra-uterine adhesions. Eur J Obstet Gynecol Reprod Biol. 2015;193:65–69. doi: 10.1016/j.ejogrb.2015.06.025. [DOI] [PubMed] [Google Scholar]
- 9.Nasr AL, Al-Inany HG, Thabet SM, Aboulghar M. A clinicohysteroscopic scoring system of intrauterine adhesions. Gynecol Obstet Investig. 2000;50:178–181. doi: 10.1159/000010305. [DOI] [PubMed] [Google Scholar]
- 10.Westendorp IC, Ankum WM, Mol BW, Vonk J. Prevalence of Asherman's syndrome after secondary removal of placental remnants or a repeat curettage for incomplete abortion. Hum Reprod. 1998;13:3347–3350. doi: 10.1093/humrep/13.12.3347. [DOI] [PubMed] [Google Scholar]
- 11.Guida M, Cipullo LMA, Iovieno R, et al. Office hysteroscopic treatment of a vanishing external uterine orifice in a postmenopausal woman with an obstetrical history of 44 abortions. Gynecol Minim Invasive Ther. 2014;4:146–148. [Google Scholar]
- 12.Lemmers M, Verschoor MA, Oude Rengerink K, et al. MisoREST: surgical versus expectant management in women with an incomplete evacuation of the uterus after misoprostol treatment for miscarriage: a randomized controlled trial. Hum Reprod. 2016;31:2421–2427. doi: 10.1093/humrep/dew221. [DOI] [PubMed] [Google Scholar]
- 13.Hamerlynck TW, Blikkendaal MD, Schoot BC, Hanstede MM, Jansen FW. An alternative approach for removal of placental remnants: hysteroscopic morcellation. J Minim Invasive Gynecol. 2013;20:796–802. doi: 10.1016/j.jmig.2013.04.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


