Older adults are the fastest growing demographic in America. From January 1, 2011 to December 31, 2030, an average of approximately 10,000 people are turning 65 every day in the United States (Passel & Cohen, 2008). Although the baby boom has contributed to the aging of the American population, there are more fundamental forces underlying the expected enduring change in the age-structure of American society, including the reduction in birth rate; the reduction in infant, child, and maternal mortality; and the increase in life expectancy (MacArthur Foundation Research Network on an Aging Society, 2009).
The aging of American society has increased the importance of identifying modifiable social, behavioral, and lifestyle factors associated with health and well-being. The modification of these factors has the potential to promote well-being, extend functional lifespan, and help contain health care costs. Longitudinal data on representative samples of middle-age to older adults are particularly useful in this effort. We designed the Chicago Health, Aging, and Social Relations Study (CHASRS) with this objective in mind. CHASRS is a ten-wave longitudinal, population-based (i.e., representative) study of African American, Hispanic, and non-Hispanic White men and women born between 1935 and 1952. The age range for eligibility in the study was selected based on national health statistics, which suggested that most individuals in this age-range would be generally healthy but a significant subset would likely encounter health problems over the next decade. This permitted prospective investigation of the risk factors for and mechanisms underlying changes in health and well-being in an aging population. The Waves of CHASRS were conducted annually, beginning in 2002/2003, with the exception of 2007/2008, when there was a one-year gap between Waves 5 and 6 while funding was secured. Our primary aim here is to describe CHASRS and the de-identified data that are available.
CHASRS was designed as a laboratory rather than a survey study to provide more detailed coverage of the social (e.g., objective social isolation, perceived social isolation or loneliness, social support), dispositional (e.g., Big 5, height, weight), behavioral (e.g., exercise, alcohol consumption, smoking), cognitive (e.g., verbal memory, self-regulation), emotional (e.g., social anxiety, coping strategies), autonomic (e.g., peripheral resistance, blood pressure, heart rate), neuroendocrine (e.g., cortisol, epinephrine, norepinephrine), and molecular (e.g., glycosylated hemoglobin, cholesterol levels) processes underlying psychological (e.g., depressive symptomatology, subjective well-being) and physical health outcomes in older adults (e.g., Charlson Comorbidity Index, self-rated health). The sample size of CHASRS is small by comparison to survey studies such as the Health and Retirement Study (HRS), so CHASRS was designed to complement the HRS (cf. Hughes, Waite, Hawkley, & Cacioppo, 2004) by providing more detailed coverage of the dispositional, biological, and psychological domains to investigate the specificity of and potential causal mechanisms underlying associations between psychological variables and mental or physical health outcomes. The sample size for CHASRS was based on statistical power calculations to permit detection of moderate effect sizes in longitudinal analyses, and the sample size is relatively large given the time and extent of psychological measures, behavioral (e.g., cognitive function) assessments, interviews, tissue collection (urine, blood, saliva), and physiological assessments that were obtained each Wave.
The longitudinal design of CHASRS also permits the use of an array of statistical models, such as cross-lagged panel models (e.g., Cacioppo, Hawkley, & Thisted, 2010), multi-level modeling, latent growth models (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006), and marginal structural models (e.g., VanderWeele, Hawkley, Thisted, & Cacioppo, 2011) to investigate the prospective association and specificity of the association between two variables, as well as to permit investigation of the mechanism(s) underlying specific associations (e.g., loneliness & depressive symptomatology). Attention was also given in the design and selection of measures to permit an evaluation of three general, non-mutually exclusive hypotheses regarding prospective associations of health and well-being: differential exposure, differential reactivity, and differential cumulative load (e.g., see Cacioppo, Berntson, & Hawkley, 2003). According to the differential exposure hypothesis, health outcomes are related to the stimuli or events to which an individual is exposed (e.g., early trauma, life events, quotidian stressors). According to the differential reactivity hypothesis, health outcomes are related to an individual’s reactivity to a given stimulus or event. Finally, according to the differential residual load hypothesis, health outcomes are related to the cumulative wear and tear that accrues over exposures and reactions to stimuli and events to which an individual is exposed.
Longitudinal studies of older adults can be complicated by the loss of individuals between Waves for various reasons (Given, Keilman, Collins, & Given, 1990; Gustavson, von Soest, Karevold, & Røysamb, 2012). Chatfield, Brayne, and Matthews (2005) performed a systematic review of studies on attrition in longitudinal studies of the elderly, and their multivariate analyses indicated that increasing age and significant cognitive impairment were the two main independent factors that were related to increased attrition. However, the participants in the studies reviewed by Chatfield et al. (2005) were generally much older than the participants in CHASRS, and the response burden was lower than in CHASRS. Our second aim, therefore, is twofold: (a) to extend our understanding of attrition to a population-based sample of older African American, Hispanic, and Non-Hispanic White women and men in a longitudinal laboratory study, and (b) to identify characteristics of respondents that predict attrition to permit evaluation of potential selection biases in secondary analyses of the data. Specifically, we investigate the baseline sociodemographic characteristics of respondents that predict attrition. Knowledge of these characteristics identifies potential selection biases across waves and suggests characteristics for oversampling to ensure adequate representation is maintained in longitudinal laboratory studies. Time-varying health, cognitive, and social factors also contribute to attrition (Powers & Loxton, 2010; Young, Powers, & Bell, 2006). Therefore, we report a second set of regression analyses of attrition that includes baseline measures of cognitive function, loneliness, and social contacts, and an ancillary analysis using the last available measure of these factors (rather than baseline values) to determine whether data from the most recent wave (as opposed to data from baseline) would be predictive of attrition status.
Methods
Participants and Sampling Methodology
Our target sample was selected from the population of English speaking adults born between 1935 and 1952, living in Cook County, Illinois, who were sufficiently ambulatory to come to the University of Chicago for an annual, daylong visit to the Social Neuroscience Laboratory. Potential participants were asked their age, gender, and ethnicity (African American, Hispanic, Non-Hispanic White, Asian/American Indian/Pacific Islander). Citizenship and date of immigration to the U.S. were not among the inclusion criteria, and no questions were asked about these characteristics. Potential participants were classified as African American if they so specified, Hispanic if they so specified, and Non-Hispanic White if they so specified. Given our sampling frame, potential participants who specified they were Asian/American Indian/Pacific Islander were not included in the study. A multi-stage probability sampling design was used to draw a population-based sample.
Stage One: Household Sample
The first stage involved drawing a sample of households, using a sampling frame owned and maintained by GENESYS Sampling Systems. This frame consists of all households with listed phone numbers, augmented by additional households identified through available sources such as voter registration records, school registration records, and magazine subscription lists. The frame used was last updated in September 2001, and contained 57 percent of all households in Cook County. Because of the high costs associated with screening randomly selected households, a subset of households estimated to have high probability of containing at least one adult aged 50–65 was first identified. This subset constituted 24 percent of the total frame, and was identified by GENESYS using a multiple regression model including covariates such as demographic variables, magazine subscription data, and data on purchasing behavior. According to GENESYS, the model is capable of identifying a subset of households with probability 0.6 of containing at least one age-eligible individual.
Once this subset of households was identified, a stratified equal probability of selection sample was drawn. The following three strata were used: (1) households from census tracts in which at least 80 percent of the residents were African American, (2) households for which the associated surname (as listed in GENESYS's records) was among the roughly 13,000 surnames identified by the US Census Department as “Hispanic”, and (3) all remaining households. For the full frame, Stratum (1) contains approximately 80 percent of all African American households in Cook County. Stratum (2) is less effective at targeting Hispanics, as only about 60 percent of persons with Hispanic surnames identify themselves as Hispanic and a similar fraction (60%) of Hispanics have Hispanic surnames. The sample was drawn in replicates, with the proportions from each stratum being varied to achieve an approximately equal distribution among the three racial/ethnic groups in the final sample.
Stage Two: Within-household Selection
Each sampled household was screened by telephone for the presence of at least one age-eligible individual. If a household contained more than one age-eligible individual, the person with the most recent birthday was selected. The selected individual was then screened further in order to exclude those who identified themselves as belonging to a racial/ethnic group other than the three identified above and those not sufficiently ambulatory to come to the University and participate in the study. All remaining individuals were asked to participate in the study. Participants were paid $126 for participating in the first Wave.
To maximize our ability to distinguish between groups and to perform subset analyses, we used a quota sampling strategy at both the household and individual levels to achieve an approximately equal distribution of participants across the six gender by racial/ethnic group combinations. Eligible Hispanic participants were the most difficult to identify (e.g., many age-eligible Hispanics did not speak and read English well enough to participate) and to recruit, and this meant that the final replicates consisted entirely of households from the Hispanic surname stratum. In addition, once the desired number of African American and Non-Hispanic White men and women were recruited, newly sampled households without age-eligible Hispanics were discarded, and the within-household selection was made from among eligible Hispanic participants.
The final sample consisted of 229 individuals who ranged from 50–68 years of age at the time of their participation in Wave 1 (baseline assessment). The characteristics of the sample are summarized in Supplementary Table 1. The study was reviewed and approved by the University of Chicago Institutional Review Board, and all participants gave informed consent each year of their participation.
Response Rate
The response rate among eligible persons was comparable to those for other well-conducted telephone surveys. This result exceeded expectations given that participation in our study involved spending an entire day at the University. Response rates among both households with an eligible individual and those for which the presence of an eligible individual was unable to be determined (despite repeated phone attempts) were 32 percent for Stratum (1), 27 percent for Stratum (2), and 26 percent for Stratum (3) (28% overall). If we assume that the households for which the presence of an eligible individual was unknown (23 percent of all households) were just as likely to contain an eligible individual as the others, then the implied response rates increase to 50, 51, and 35 percent, respectively (45% overall).
Comparison of our sample to population statistics
The HRS is a nationally representative (population-based), longitudinal survey of persons age 50 and above. At the time CHASRS was launched, the HRS contained measures of economic variables, health behaviors, household and family structure, neighborhood characteristics, health outcomes, self-rated health, chronic diseases and conditions, physical functioning, emotional functioning and cognitive functioning. The distribution of the sample in CHASRS on a number of demographic characteristics (e.g., marital status, working status, self-perceived health) at the time of composition compared closely to that obtained from the HRS (Health and Retirement Study, 2003). For instance, self-rated health was rated as excellent or very good in 48% of 55- to 64-year-olds in HRS and in 40% of the 50- to 68-year-olds in CHASRS (which oversampled African Americans and Hispanics with known poorer self-rated health status than Non-Hispanic Whites). In the U.S. population at that time, 83%–87% of those age 50–64 years were high school graduates or more (Stoops, 2004) and in the first Wave of CHASRS, 84% were high school graduates or more.
Procedure
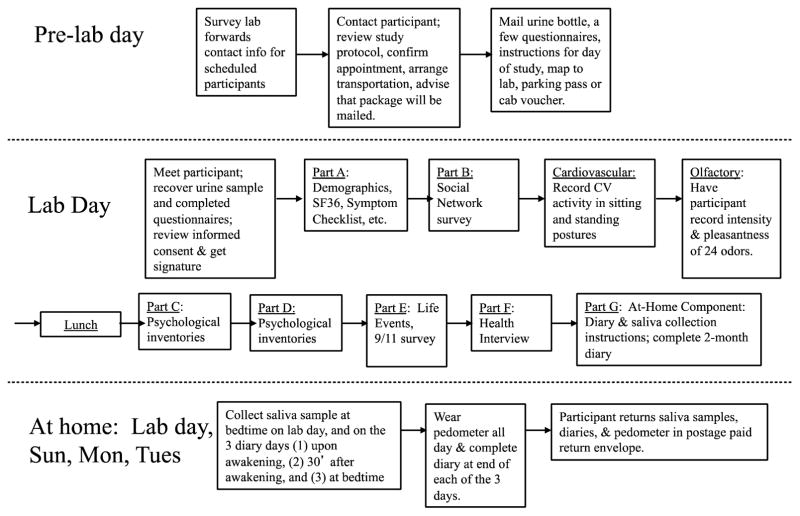
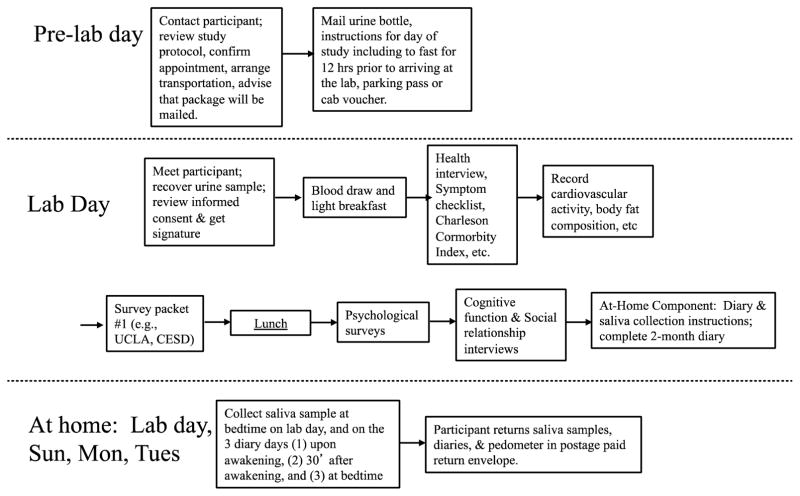
Data collection for Wave 1 of CHASRS occurred in 2002/2003, Wave 2 in 2003/2004, Wave 3 in 2004/2005, Wave 4 in 2005/2006, Wave 5 in 2006/2007, Wave 6 in 2008/2009, Wave 7 in 2009/2010, Wave 8 in 2010/2011, Wave 9 in 2011/2012, and Wave 10 in 2012/2013. The general laboratory protocol for Wave 1 is depicted in Figure 1, and for Wave 2-Wave 10 is depicted in Figure 2. Detailed descriptions of the Materials, Procedures, and Measures are available in Supplementary File 1_Procs_Measures, and a Table of the Waves for which data is available for each measure is available in Supplementary File 2_Measures_Waves.
Figure 1.
Laboratory Protocol, Wave 1
Figure 2.
Typical Laboratory Protocol, Waves 2–10
Measures for Attrition Analyses
Basic demographic and socioeconomic variables
The basic demographic and socioeconomic variables in the attrition analyses were measured in the Demographic questionnaire. These variables consisted of self-reported age, gender, ethnicity (African American, Hispanic, or non-Hispanic White), education level (Less than high school diploma, High school diploma, College or higher), household income (Twelve response categories ranging from Less than $5,000 up to Over $200,000), retirement status, and marital status.
Health variables
The health variables in the attrition analyses were measured in the Short Form Health Survey and the Health Interview questionnaires. These variables consisted of self-rated health (Poor, Fair, Good, Very Good, Excellent), functional limitation (No limitation, Some limitation, High limitation), and the Charlson comorbidity index (Zero, One, Two or more).
Cognitive function
The measure of cognitive function in the attrition analyses was obtained in the Cognitive Function test, which was administered as part of the Afternoon Interview. Specifically, cognitive function was measured by summing the number of correct answers from a list of eight factual questions (Today’s date, month, year, day of the week, name of the current president and vice president, and etc.), the Immediate Free Recall Test, and the Delayed Free Recall test (see Supplementary File for details). The resulting summary score ranged from 0 to 28 where a higher number indicated better cognitive function.
Loneliness
Loneliness was measured using the 20-item Revised UCLA Loneliness Scale (Russell, 1996; Russell, Peplau, & Cutrona, 1980), which was administered as part of the Main Survey Packet. Examples of the items are ‘‘I lack companionship’’ and ‘‘There are people I can talk to.’’ These items assess the perception that one lacks companionship or has people to talk to (for example) and are to be distinguished from other measures that ask participants how many companions they have and how often they talk to others (see measures of social relationships). The response scale ranges from 1 (never) to 4 (often), and the range of possible scores is 20 to 80, with higher scores signifying greater loneliness.
Social contact
Social contact was measured by the social network index which summarized the participants’ social contacts from seven different social domains. The questions used to create this measure were administered as part of the Demographic questionnaire. One point was assigned to this index for each of the following items endorsed by the respondent: a) is married or living with a partner, b) spoke with one or more relatives at least once every two weeks, c) spoke with one or more friends at least once every two weeks, d) spoke with one or more neighbors at least once every two weeks, e) participated in volunteer work that involves social interactions at least once every two weeks, f) participated in non-religious groups that involves social interactions at least once every two weeks, and g) had a job that involves social interactions at least every two weeks. The response scale ranged from 0 to 7, with higher scores indicating more social contacts.
Attrition Analyses
Participants were recruited originally to participate in a 5-year longitudinal study, and were contacted again for continuous participation after the completion of Wave 5. Following a one-year gap to secure funding, CHASRS was continued for another five years (Wave 6–Wave 10) in the seventh – eleventh year from the beginning of the study. As a preliminary analysis, a discrete time logistic model was used to identify the Waves in which attrition differed. A dummy variable of dropout status was used as the outcome variable in the discrete time model with a fixed effect categorical variable (Wave) indicating each year of the study (reference Wave = Wave 1) as a predictor.
For the primary analyses, survival analyses using Cox stepwise regression were performed to identify measures that predicted number of years in the study. The continuous predictors were standardized, so the resulting coefficients are standardized betas. The dummy and categorical variables (e.g., Wave of the study, retirement status) were not standardized to simplify their interpretation, so their resulting coefficients are not standardized in these analyses.
Seven groups of variables were entered into the model in sequence to investigate their potential effects on attrition, including: 1) Basic demographic variables: age, gender, and ethnicity; 2) Socioeconomic status variables: education level (Less than High School as the reference category) and household income (log transformed category median values); 3) Retirement status (dichotomous where one if retired, otherwise zero); 4) Marital status (dichotomous where one if married or living with a partner, otherwise zero); 5) Health variables: Self-rated health (higher values indicating better health), functional limitation (No limitation as the reference category), and Charlson comorbidity index (zero as the reference group); 6) Cognitive function: Summary of correct answers from eight factual questions, the immediate recall, and the delayed recall tests, with higher scores indicating better cognitive function; and 7) Social function variables: loneliness as measured by the UCLA loneliness scale where a higher value means higher loneliness; and social contacts as measured by the social network index which summarized the participants’ social contacts from seven different social domains (higher values for the measure of social contacts indicate larger social network sizes). Both measures were entered simultaneously (as the seventh variable group) to index social function.
Two sets of analyses were performed. The first set of analyses utilized variable group 1 to 4, which contained the participants’ sociodemographic information. This set of analyses aimed to identify likely sources of attrition among the variables that are available to the researchers at the initial stage of data collection. Variable groups were entered into the model sequentially and non-significant variables were dropped before adding new group of variables. The resulting model was then compared with the model with full list of covariate variables to identify influential variables that did not survive the stepwise procedure. If such variables exist, an additional model was run in which these variables were added to the last stepwise regression model. The likelihood ratio test was then used to decide the statistically preferred final sociodemographic model.
The final sociodemographic model served as the starting model for the second set of analyses. Following the same stepwise regression and model selection procedures, variable groups 5 to 7 were next entered sequentially into the model. Variable group 5 to 7 contained health, cognitive, and social measures that might contribute to attrition in a longitudinal study. For this set of variables, additional ancillary analyses were conducted to investigate whether data from the most recent wave (as opposed to data from baseline) would be predictive of attrition status.
Lastly, the reasons for attrition were analyzed. The research project managers documented the reasons for attrition based on the last phone conversation with the participants inquiring about the details behind their decisions, before sending out official end letters to thank them for the participation. In the case of death, the participation was terminated after we received news from family members. Reasons for attrition were grouped into four categories – the death of the participant, loss of contact with the participant, chose not to continue, or were dropped by the study team. Loss of contact occurred when we couldn't reach the participants either by phone or mail, which included situations when no one answered the phone, a number became invalid, when we were told the person has moved but wasn't provided with the new contact information, or when the mails sent to the participants were returned without forwarding address.
Results
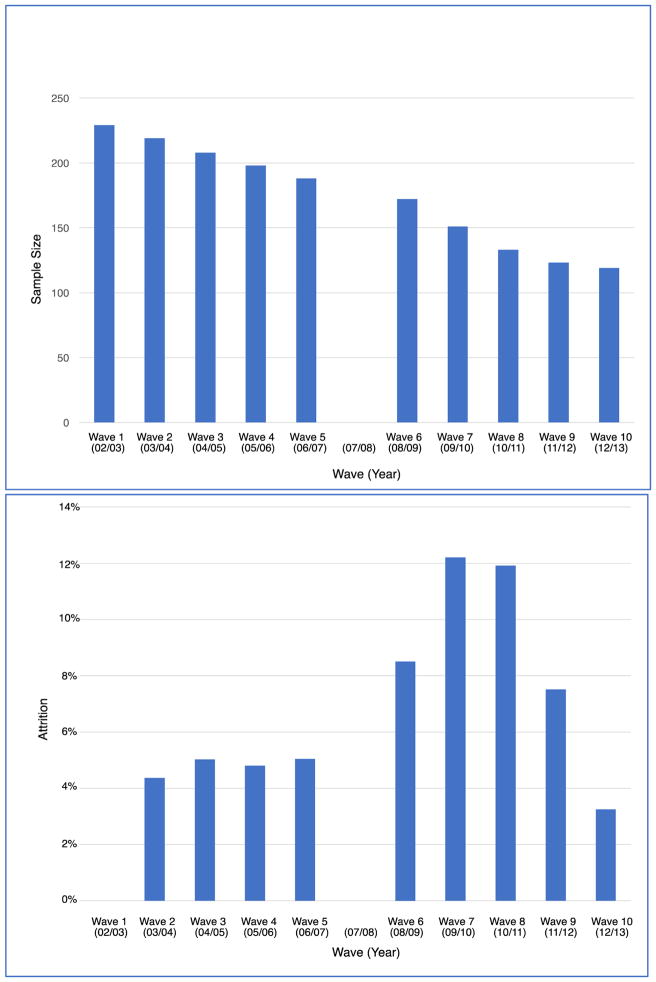
The sample size for each Wave of the study is illustrated in the top panel of Figure 3, and the annual attrition rate over the ten years of CHASRS is depicted in the bottom panel of Figure 3. The attrition rate was stable at around 4.8% for the first 4 years of the study. It started to trend up in Wave 6 (8.5%), and reached its highest levels in Wave 7 and Wave 8 (around 12% in both years). The attrition rate then declined to reach around 3% by Wave 10. Although attrition averaged 6.96% across the ten waves of CHASRS, the cumulative effect on the sample size was to reduce the sample from 229 in Wave 1 to 119 in Wave 10 (see Figure 3). Discrete time survival model confirmed the odds of dropping out was higher in Waves 6 (β = 0.71, SE = 0.42, p = .087, Odds ratio = 2.04), 7 (β = 1.11, SE = 0.40, p = .005, Odds ratio = 3.05) and 8 (β = 1.09, SE = 0.41, p = .008, Odds ratio = 2.96) than in the other Waves.
Figure 3.
CHASRS Yearly Sample Size (top panel) and Attrition Rate (bottom panel). The attrition rate is specified for data collection Waves 2–10 because it represents the difference in sample size in Waven minus Waven−1.
The Cox stepwise regression analyses on the socioeconomic items at baseline indicated that, in the final model (Model 6, see Supplementary Table 2), age, education, household income, and retirement status were significantly related to attrition. Specifically, attrition was higher for older participants (β = 0.30, SE = 0.10, p < .01), and lower for people with more years of education (high school diploma, β = −0.51, SE = 0.25, p < .05; college or more, β = −0.59, SE = 0.30, p < .05), higher household income (β = −0.22, SE = 0.10, p < .05), and among retirees (β = −1.18, SE = 0.21, p < .001). Although not significant, there was a tendency for attrition to be higher for Hispanic participants (β = 0.45, SE = 0.24, p = .07). Hazard ratios for these predictors are provided in Table 1A (top panel). Details of the Cox regression analyses of demographic predictors are provided in Supplementary Table 2.
Table 1.
Hazard Ratios for Significant Predictors of Attrition
| A. Model with significant sociodemographic predictors | |||
|---|---|---|---|
| Hazard Ratio | SE | P | |
| Age | 1.35 | 0.14 | < .01 |
| Ethnicity | |||
| Black | 1.12 | 0.27 | 0.65 |
| Hispanic | 1.56 | 0.38 | 0.07 |
| Education | |||
| HS diploma | 0.60 | 0.15 | < .05 |
| College + | 0.56 | 0.17 | < .05 |
| Household income | 0.80 | 0.08 | < .05 |
| Retirement status | 0.31 | 0.07 | < .01 |
| B. Final model | |||
|---|---|---|---|
| Hazard Ratio | SE | P | |
| Age | 1.26 | 0.13 | < .05 |
| Retirement status | 0.30 | 0.06 | < .01 |
| Cognitive function | 0.74 | 0.07 | < .01 |
| Social contacts | 0.72 | 0.07 | < .01 |
When health, cognitive, and social predictors at baseline were added as predictors, the only sociodemographic measures that remained significant predictors of attrition were age (β = 0.23, SE = 0.10, p < .05) and retirement status (β = −1.19, SE = 0.21, p < .001). In addition, better cognitive function (β = −0.30, SE = 0.10, p < .01) and more social contacts (β = −0.33, SE = 0.09, p < .001) were also significant predictors of lower attrition. Hazard ratios for these predictors are provided in Table 1B (bottom panel). Details of the Cox regression analyses of demographic, health, cognitive, and social predictors are provided in Supplementary Table 3.
Finally, ancillary analyses were performed using the latest available values rather than baseline values for time−varying (i.e., cognitive & social) predictors. The final model was unchanged: age (β = 0.21, SE = 0.10, p < .05), retirement status (β = −1.13, SE = 0.21, p < .001), cognitive function (β = −0.32, SE = 0.07, p < .01), social contacts (β = −0.34, SE = 0.09, p < .001) were significant predictors of attrition. Details of these ancillary analyses are provided in Supplementary Table 4.
Analyses of the reasons identified for attrition indicated that, among the 110 people who dropped out of the study, 9 died, 33 could not be reached, 70 chose not to continue, and 3 were dropped by the study-team. The death of participants occurred relative evenly across the study and we did not see more death clustered at the later years of the study. There were no significant moderators (e.g., age, ethnicity, or gender patterns) for this category of attrition. The most common reasons given for choosing to no longer continue in the study (mentioned by 55 of the 70 participants) were: “don't want to any more,” “busy with other obligations,” or “not worth the time.” Of the remaining 15 participants, 10 cited health issues, 2 cited difficulties in scheduling, 2 cited a spouse passing away, and 1 did not like the content of the questionnaires. Finally, 3 people were dropped by the study team: one due to language barriers not detected at prescreening, one due to inappropriate behaviors toward the study team, and one due to internally inconsistent survey responses.
Discussion
The loss of individuals between waves in longitudinal studies of older adults can have implications for what are appropriate research questions, analyses, and interpretations. One aim in this study, therefore, was to identify the characteristics of respondents that predicted attrition over the ten waves of CHASRS. We first focused on sociodemographic characteristics at baseline as predictors (Models 1–4). In a second set of analyses, we added measures of health, cognitive, and social functioning (Models 5–7) at baseline. Multivariate analysis of the prior literature on attrition in longitudinal studies of older adults revealed that the two main factors that predicted attrition were age and significant cognitive impairment (Chatfield et al., 2005). The attrition analyses in CHASRS produced similar results: the final predictive model indicated that age was associated with higher attrition, whereas better cognitive function and social contact at baseline were associated with lower attrition. Analyses using the latest available values rather than baseline values produced comparable results, suggesting that the predictors of attrition are not time-varying in population-based samples of older adults.
The comparability of our results and those reviewed by Chatfield et al. (2005) is notable in light of the differences between CHASRS and most prior research on attrition in older adults. First, the participants in most of the studies reviewed by Chatfield et al. (2005) were substantially older than the participants in CHASRS, with the minimum age at baseline in the vast majority of these studies being 65 years. In contrast, the participants in CHASRS ranged in age from 50–68 years at baseline. Second, the sample size of the studies reviewed by Chatfield et al. (2005) was many times greater (ranging from 1,045 to more than 13,000) than in CHASRS, yet there was remarkable similarity in the results. Finally, and perhaps most notably, the response burden in CHASRS was significantly greater than in the studies reviewed by Chatfield et al. (2005). For instance, participation in CHASRS were asked to complete a long set of surveys and an overnight urine sample prior to a number of annual assessments; travel to and a day-long visit to the laboratory for an extensive series of physiological assessments, interviews, and surveys; and complete and return a take-home packet that in some years included three days of daily surveys and multiple salivary samples. Indeed, the modal reasons given for attrition were “busy with other obligations,” “not worth the time,” or “don't want to any more,” and many complained that the compensation for traveling to and spending the day in a university laboratory was insufficient.
Despite generally modest annual rates of attrition, the sample size for CHASRS was nearly halved over the ten waves of the study. Analyses of attrition showed that age was the only demographic factor that significantly predicted attrition, suggesting that the demographic characteristics of the final sample in CHASRS was similar to the baseline sample. The demographic composition of the U.S. population also changed over the eleven-year period of the study. These demographic changes were foreseeable, however, and we oversampled African American and Hispanic participants when recruiting for Wave 1 of CHASRS.
Analyses of attrition across the ten waves of CHASRS revealed that attrition was significantly higher in Waves 6–8 than in the remaining waves. We can only speculate about the causes of the higher attrition in Waves 6–8, but three factors which coincided with the beginning of Wave 6 may have been contributing factors: (a) the respondents’ initial 5-year commitment to CHASRS had been completed, (b) there was an unexpected one-year gap between Waves 5 and 6 while funding was secured, and (c) the global banking crisis in September 2008 erupted as data collection for Wave 6 was beginning. Despite the elevated attrition rates in Waves 6–8, the predictors of attrition in CHASRS were stable across years. These findings, together with the similarity in our results to those of prior studies, indicate that age and cognitive function are stable and generalizable predictors of attrition and point to social contact as a third potentially factor to consider in longitudinal studies of older adults, especially for studies in which the response burden is high.
Our primary focus in CHASRS has been to investigate the association between social isolation (objective & perceived, or loneliness) and health outcomes (e.g., depressive symptomatology, e.g., Cacioppo et al., 2010; physical activity, e.g. Hawkley, Thisted, & Cacioppo, 2009; blood pressure, e.g., Hawkley, Thisted, Masi, & Cacioppo, 2010; morning rise in cortisol, e.g., Adam et al., 2006) as well as the transduction pathways through which social isolation may influence age-related changes in health (e.g., see recent reviews by J. T. Cacioppo, Cacioppo, Capitanio, & Cole, 2015; S. Cacioppo, Capitanio, & Cacioppo, 2014; S. Cacioppo, Grippo, London, Goossens, & Cacoppo, 2015; Cole, Hawkley, Arevalo, & Cacioppo, 2011). However, CHASRS is suitable for a wide range of investigations of older adults, including narrowly focused hypothesis testing, exploratory analyses and pilot research, and sample size calculation.1
In sum, American society is in the midst of an enduring change in demographic composition. For instance, according to the U.S. Census, people aged 65 years or older represented less than 5.4% of the American population in 1930, had grown to 12.4% of the population by 2000 (shortly before Wave 1 of CHASRS) and are projected to reach 20% by 2030 (MacArthur Foundation Research Network on an Aging Society, 2009). Investigations of modifiable social, behavioral, and lifestyle factors that influence the health and well-being of this growing demographic have an important role to play in the health and welfare of these individuals and of industrialized societies more generally. Our hope is that the data available in CHASRS provides a valuable resource in such investigations.
Supplementary Material
Acknowledgments
This research is supported by Grants P01AG18911, RO1AG034052, and R37AG033590 from the National Institute on Aging. We thank Hsi Yuan Chen, Ron Thisted, Linda Waite, Martha McClintock, Louise Hawkley, Tyler Lorig, Christopher Masi, Phil Schumm, and the staff of CHASRS for their assistance in this work.
Footnotes
Please see the policy and procedures of the Archives of Scientific Psychology for access to the CHASRS data (http://www.apa.org/pubs/journals/arc/data-access.aspx).
The authors have made available for use by others the data that underlie the analyses presented in this paper (see Cacioppo and Cacioppo, 2017), thus allowing replication and potential extensions of this work by qualified researchers. Next users are obligated to involve the data originators in their publication plans, if the originators so desire.
Contributor Information
John T. Cacioppo, University of Chicago
Stephanie Cacioppo, University of Chicago Pritzker School of Medicine.
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience-cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry AE. How attrition impacts the internal and external validity of longitudinal research. The Journal of school health. 2005;75(7):267–270. doi: 10.1111/j.1746-1561.2005.00035.x. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S, Capitanio JP, Cole SW. The neuroendocrinology of social isolation. Annual Review of Psychology. 2015;66:733–767. doi: 10.1146/annurev-psych-010814-015240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S. The Population-Based Longitudinal Chicago Health, Aging, and Social Relations Study (CHASRS): Study Description and Predictors of Attrition in Older Adults) (ICPSR36950-v1) [Data set] Ann Arbor, MI: Inter-University Consortium for Political and Social Research; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG. The anatomy of loneliness. Current Directions in Psychological Science. 2003;12:71–74. [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: Five year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross sectional and longitudinal analyses. Psychology and Aging. 2006;21:140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Cacioppo S, Capitanio JP, Cacioppo JT. Toward a neurology of loneliness. Psychological Bulletin. 2014;140:1464–1504. doi: 10.1037/a0037618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: Clinical import and interventions. Perspectives on Psychological Science. 2015;10:238–249. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. Journal of Clinical Epidemiology. 2005;58:13–19. doi: 10.1016/j.jclinepi.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JMG, Cacioppo JT. Transcript origin analysis identifies antigen presenting cells as primary targets of socially regulated leukocyte gene expression. Proceedings of the National Academy of Sciences. 2011;108:3080–3085. doi: 10.1073/pnas.1014218108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givens BA, Keilman LJ, Collins C, Given CW. Strategies to minimize attrition in longitudinal studies. Nursing Research. 1990;39(3):184–186. doi: 10.1097/00006199-199005000-00018. [DOI] [PubMed] [Google Scholar]
- Gustavson K, von Soest T, Karevold E, Røysamb E. Attrition and generalizability in longitudinal studies: findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Public Health. 2012;12(1):918. doi: 10.1186/1471-2458-12-918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: Cross-sectional and longitudinal analyses. Health Psychology. 2009;28:354–363. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: Five-year cross-lagged analyses in middle-aged and older adults. Psychology and Aging. 2010;25:132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study. Sample size and response rates. 2003 Retrieved October 13, 2003, from www.umich.edu/~hrswww/studydet/techdet/sample.html.
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacArthur Foundation Research Network on an Aging Society. Facts and fictions about an aging America. Contexts. 2009;8(4):16–21. doi: 10.1525/ctx.2009.8.4.16. [DOI] [Google Scholar]
- Passel JS, Cohn D. U.S. Population Projections: 2005 – 2050. Social and Demographic Trends. 2008:2005–2050. [Google Scholar]
- Powers J, Loxton D. The impact of attrition in an 11-year prospective longitudinal study of younger women. Annals of Epidemiology. 2010;20(4):318–321. doi: 10.1016/j.annepidem.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Russell D. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology. 1980;39:472–80. doi: 10.1037/0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Stoops N. Educational attainment in the United States: 2003. Population characteristics. Washington, D.C: US Department of Commerce; 2004. https://www.census.gov/prod/2004pubs/p20-550.pdf. [Google Scholar]
- VanderWeele TJ, Hawkley LC, Thisted RA, Cacioppo JT. A marginal structural model analysis for loneliness: Implications for intervention trials and clinical practice. Journal of Clinical and Consulting Psychology. 2011;79:225–235. doi: 10.1037/a0022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AF, Powers JR, Bell SL. Attrition in longitudinal studies: who do you lose? Australian and New Zealand Journal of Public Health. 2006;30(4):353–361. doi: 10.1111/j.1467-842X.2006.tb00849.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.