Abstract
Background
Penetrating cardiac injuries (PCIs) are highly lethal, and a sternotomy is considered mandatory for suspected PCI. Recent literature suggests pericardial window (PCW) may be sufficient for superficial cardiac injuries to drain hemopericardium and assess for continued bleeding and instability. This study objective is to review patients with PCI managed with sternotomy and PCW and compare outcomes.
Methods
All patients with penetrating chest trauma from 2000 to 2016 requiring PCW or sternotomy were reviewed. Data were collected for patients who had PCW for hemopericardium managed with only pericardial drain, or underwent sternotomy for cardiac injuries grade 1–3 according to the American Association for the Surgery of Trauma (AAST) Cardiac Organ Injury Scale (OIS). The PCW+drain group was compared with the Sternotomy group using Fisher’s exact and Wilcoxon rank-sum test with P<0.05 considered statistically significant.
Results
Sternotomy was performed in 57 patients for suspected PCI, including 7 with AAST OIS grade 1–3 injuries (Sternotomy group). Four patients had pericardial injuries, three had partial thickness cardiac injuries, two of which were suture-repaired. Average blood drained was 285 mL (100–500 mL). PCW was performed in 37 patients, and 21 had hemopericardium; 16 patients proceeded to sternotomy and 5 were treated with pericardial drainage (PCW+drain group). All PCW+drain patients had suction evacuation of hemopericardium, pericardial lavage, and verified bleeding cessation, followed by pericardial drain placement and admission to intensive care unit (ICU). Average blood drained was 240 mL (40–600 mL), and pericardial drains were removed on postoperative day 3.6 (2–5). There was no significant difference in demographics, injury mechanism, Revised Trauma Score exploratory laparotomies, hospital or ICU length of stay, or ventilator days. No in-hospital mortality occurred in either group.
Conclusions
Hemodynamically stable patients with penetrating chest trauma and hemopericardium may be safely managed with PCW, lavage and drainage with documented cessation of bleeding, and postoperative ICU monitoring.
Level of evidence
Therapeutic study, level IV.
Keywords: chest trauma, cardiac injury, pericardial window, hemopericardium, sternotomy
Background
Penetrating chest trauma is one of the most lethal mechanisms incurred by patients, and penetrating cardiac injuries (PCIs) are among the most fatal.1–3 Up to 94% of patients with PCI die on the scene prior to hospital presentation,4 and the mortality of patients arriving at trauma centers with signs of life ranges from 17% to 58%.3 5 6 Due to the life-threatening physiologic changes caused by these injuries, including pericardial tamponade and hemorrhagic shock, management for PCIs has focused on rapid assessment and therapeutic maneuvres. Due to this potential for rapid hemodynamic decline, the standard management for suspected PCI has been a sternotomy to relieve tamponade and repair any cardiac or great vessel injuries.7
Although many patients die in the field or present in extremis, some patients with PCI have a benign presentation and are hemodynamically stable on arrival to a trauma center.8 These patients have minor cardiac or pericardial injuries resulting in hemopericardium, but bleed very slowly or stop completely. These stable patients allow time for more detailed diagnostic workup and less invasive management strategy. Furthermore, a sternotomy is a highly morbid procedure,4 9 10 and performing one in a trauma patient with benign PCI may subject them to unnecessary complications. Recent studies, including a randomized controlled trial (RCT) performed by Nicol et al,11 have demonstrated that patients with PCI and a benign presentation may be successfully managed with PCW provided they maintain hemodynamic stability and achieve cessation of bleeding.11–14 The pericardial window (PCW) serves to drain the pericardium and relieve any potential tamponade. If bleeding ceases and the patient remains stable, sternotomy may be avoided.
Our trauma center has adopted a selective practice of performing initial PCW, lavage, and drainage for patients with suspected PCI, hemodynamic stability, and pericardial fluid on the cardiac view on the Focused Assessment with Sonography for Trauma (FAST) examination. This report aims to describe our experience in treating this select group of PCI patients and compare outcomes with similarly injured patients undergoing sternotomy. We hypothesized that the stable PCI patients undergoing a PCW and drainage would have no difference in mortality, ventilator days, hospital length of stay (LOS), or intensive care unit (ICU) LOS compared with those who underwent a sternotomy.
Methods
This project was approved by our Institutional Review Board after an expedited review. A waiver of informed consent was obtained. The trauma registry at our American College of Surgeons-verified level 1 trauma center was extracted to create a database including all patients with cardiac injuries from 2000 to 2016. This database was queried for all patients suffering penetrating chest injury who received a PCW, a median sternotomy, or both. Patients who underwent left anterolateral or clamshell thoracotomy, and those who required cardiopulmonary resuscitation prior to intervention, were excluded. A review of the medical records obtained additional details of the operative procedure(s), cardiac injury, quantity of pericardial drainage, and type of drain(s) placed. The Revised Trauma Score (RTS) was calculated retrospectively.15 For patients who underwent sternotomy, the operative details were reviewed and the American Association for the Surgery of Trauma (AAST) Cardiac Organ Injury Scale (OIS) was analyzed retrospectively.16 The AAST Cardiac OIS was unable to be analyzed for patients who only underwent PCW and drainage since the heart was not fully visualized. Postoperative course and hospital resource utilization details, including use of echocardiogram were enumerated for all patients.
Patients who underwent initial PCW were classified as positive on the presence of hemopericardium, or negative for the absence of blood. All patients who had a PCW window and underwent drainage and lavage, but did not require a sternotomy, were included in the PCW+drain group. Patients who underwent both pericardial window and sternotomy were included in the sternotomy group. All PCW+drain patients were hemodynamically stable with systolic blood pressure over 100 mm Hg. Sternotomy patients were classified per their AAST OIS. Patients with AAST OIS 1–3 were included in the Sternotomy group, and patients with OIS 4–6 were excluded. Patients with OIS 1–3 were included because these are not full thickness injuries and may not require surgical repair,13 and were suspected to have similar injury pattern to the PCW+drain group. Patients with extracardiac injuries were included provided they were not immediately fatal and adequate surgical repair was achieved.
All patients in the PCW+drain group had their procedure performed in the operating room under general anesthesia. If hemopericardium was detected during the PCW, a soft 16 F red rubber catheter was inserted into the pericardium, and all blood suctioned out. Output was recorded in the operative dictation, which was reviewed and recorded for this study. After on-table lavage with normal saline and verification that bleeding had ceased, a 19 F fluted, silicone drain was placed in the pericardium and the patient was taken to the ICU for monitoring.
Data were compiled using Microsoft Excel (Microsoft Corp, Redmond, Washington, USA) and statistical analysis was performed using Stata V.11.2 (StataCorp, College Station, Texas, USA). Categorical variables were compared using Fisher’s exact test, and continuous variables were compared with Wilcoxon rank-sum test, with p<0.05 considered statistically significant.
Results
We identified 78 patients who met review criteria, which are summarized in table 1 which includes all patients with penetrating chest trauma undergoing PCW, sternotomy, or both.
Table 1.
All patients with penetrating chest trauma receiving either a pericardial window, sternotomy, or both
| N=78 | |
| Male, n (%) | 73 (93.6) |
| Age (years), median (IQR) | 29 (24–39) |
| Mechanism | |
| Gunshot wound, n (%) | 28 (35.9) |
| Knife stab wound, n (%) | 47 (60.3) |
| Admission vitals | |
| Systolic blood pressure, median (IQR) | 130 (85–149) |
| Heart rate, median (IQR) | 107 (88–121) |
| Glasgow Coma Scale, median (IQR) | 15 (9–15) |
| Exploratory laparotomy, n (%) | 42 (53.8) |
| Hospital LOS (days), median (IQR) | 7 (4–11) |
| ICU LOS (days), median (IQR) | 2 (1–5) |
| Ventilator days (days), median (IQR) | 0 (0–1) |
| Hospital mortality, n (%) | 16 (20.3) |
ICU, intensive care unit; LOS, length of stay.
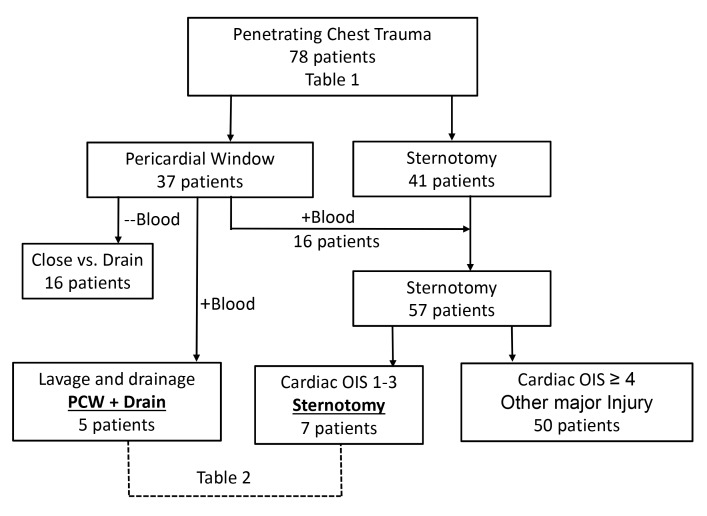
Sternotomy was performed immediately in 41 patients. PCW was performed in 37 patients. PCW was negative in 16 patients, and positive in 21 patients. Of the 21 patients with hemopericardium, 16 patients proceeded to sternotomy for a total of 57 patients undergoing sternotomy. Five patients did not undergo sternotomy, and instead underwent pericardial drainage and lavage, and comprise the PCW+drain group. All PCW+drain patients had suction evacuation of hemopericardium pericardial lavage, and documented cessation of intraoperative bleeding, followed by pericardial drain placement and admission to ICU. Of the 57 patients who required sternotomy, 50 patients had cardiac OIS of 4–6 or suffered other major injuries, and were excluded from the sternotomy comparison group. The pathway describing the patients reviewed for this study is illustrated in figure 1. Details of injuries to this group include 26 patients with OIS 4, 16 patients with OIS 5, 5 patients with OIS 6, and 2 patients with OIS 0 but had major thoracic vessel injuries (one inferior vena cava, one aorta).
Figure 1.
Flow chart of patients reviewed, including all patients who underwent sternotomy or pericardialwindow for suspected penetrating cardiac injury. OIS, Organ Injury Scale; PCW+drain, pericardial window, lavage, and drainage.
Comparisons between the PCW+drain and Sternotomy groups are shown in table 2.
Table 2.
Comparison between patients undergoing PCW+drain after positive PCW and those undergoing sternotomy for cardiac OIS of 1–3. Median and IQR displayed for continuous variables, and quantity (%) for categorical variables. omparison using Fisher’s exact test and Wilcoxon rank-sum with p<0.05 was considered statistically significant
| PCW+drain N=5 |
Sternotomy N=7 |
P values | |
| Age (years), median | 29 (25–51) | 35 (17–52) | 0.63 |
| Male, n (%) | 4 (80%) | 7 (100%) | 0.42 |
| Knife stab wound, n (%) | 5 (100%) | 6 (86%) | 1.0 |
| Exploratory laparotomy, n (%) | 2 (40%) | 3 (43%) | 1.0 |
| Systolic blood pressure, median (IQR) | 144 (138–149) | 127 (71–145) | 0.57 |
| Heart rate, median (IQR) | 99 (93–110) | 98 (88–111) | 0.81 |
| Glasgow Coma Scale, median (IQR) | 15 (15–15) | 15 (15–15) | 0.40 |
| Revised Trauma Score, median (IQR) | 12 (11–12) | 12 (10–12) | 1.0 |
| Hospital LOS (days), median (IQR) | 5 (5–12) | 7 (4–20) | 0.63 |
| ICU LOS (days), median (IQR) | 4 (3–4) | 2 (2–3) | 0.18 |
| Ventilator days (days), median (IQR) | 1 (0–2) | 0 (0–1) | 0.36 |
| Hospital mortality, n (%) | 0 (0%) | 0 (0%) | - |
ICU, intensive care unit; LOS, length of stay; PCW+drain, pericardial window, lavage, and drainage.
There was no significant difference in age, gender, injury mechanism, exploratory laparotomies, presentation vital signs and Glasgow Coma Scale, and RTS. Outcome measures including hospital or ICU LOS, and ventilator days were also similar between groups. ICU LOS in the PCW+drain group was 4 days compared with 2 days in the sternotomy group, although this was not statistically significant (p=0.18). No patients died prior to hospital discharge in either group.
Details of patient presentation, workup, surgical approach and outcomes are shown in online supplementary table 1. For the PCW+drain patients, the average age was 29 years, and 80% were male. All were injured by stab wounds. FAST was performed in four patients (80%) and was positive in three. Patient 5 had an initial negative FAST, but developed a pericardial effusion on hospital day 7 and PCW was done. Average volume of blood drained was 240 mL (range 40–600 mL). Drains were removed on average postoperative day 3.6 (range 2–5). Three patients underwent intraoperative transesophageal echocardiography (TEE), all of which showed resolution of pericardial fluid after surgical therapy. The median stay in the ICU after the procedure was 4 days, hospital LOS was 5 days, and median 1 ventilator day. No patients died prior to hospital discharge, and all patients were discharged home.
tsaco-2018-000187supp001.docx (17.6KB, docx)
Details of the seven sternotomy patients for AAST cardiac OIS 1–3 are also shown in online supplementary table 1. Median age was 35 years (range 17–52) and all were male. One patient was injured by gunshot wound (GSW), the other six by knife stab wound (KSW). Two patients had no ultrasound prior to sternotomy, two underwent FAST which was positive, three underwent formal echocardiogram (two Trans-thoracic Echocardiogram (TTE), one TEE) all of which showed pericardial fluid. Three patients also underwent laparotomy, and these three had a PCW prior to their sternotomy; one was subxiphoid and two transdiaphragmatic. The operative dictations of five patients listed specific volumes of blood drained from the pericardium, with an average 285 mL (range 100–500 mL); the volume of pericardial fluid of the two remaining patients’ drainage was described (figure 2) as ‘significant’ and ‘moderate’. The cardiac OIS was 1 in four patients, 2 in two patients, and 3 in one patient. Three patients underwent intraoperative TEE which confirmed resolution of pericardial fluid. All patients in the sternotomy group had pericardial drains placed, including size 32 F (French) in six patients and 36 F in one patient. The pericardial drain was removed 2–5 days after operation. Two patients required a ventilator, one for 1 day, and another for 27 days, the remaining five patients did not require a ventilator. Median ICU stay was 2 days (range 1–28 days) and median hospital LOS was 7 days (range 3–28 days). All patients in this group survived to discharge. Patient 1 was discharged to a skilled nursing facility, and the remaining six patients were discharged home.
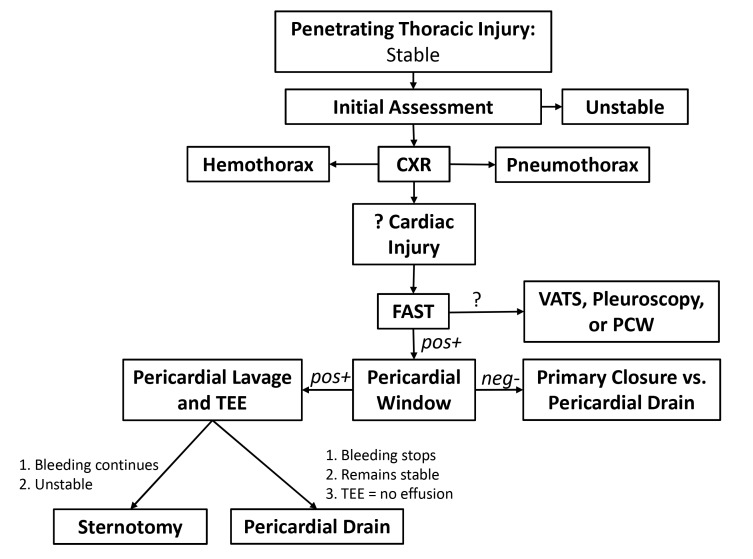
Figure 2.
Suggested modification to the Western Trauma Association’s management strategy for stable patients with penetrating thoracic injury. FAST, Focused Assessment with Sonography for Trauma; PCW, pericardial window; TEE, transesophageal echocardiography, VATS = Video Assisted Thoracic Surgery, CXR = Chest X-Ray.
Laparotomy was performed in two of the PCW+drain patients. Patient 2 underwent laparotomy for multiple abdominal KSWs, but had no internal injuries. Patient 5 underwent initial exploratory laparotomy for multiple KSWs with only minor injuries to the liver and spleen, and a small diaphragm laceration which was repaired. Three patients in the Sternotomy group required laparotomy. Patient 6 was injured by GSW and underwent exploratory laparotomy, splenorrhaphy and colon resection, patient 7 had laparotomy with no internal injuries, and patient 8 had laparotomy with control of liver bleeding.
Cardiac and pericardial repair was performed only in patients undergoing sternotomy. Patient 6 had a partial thickness right ventricle (RV) laceration which was sutured, and patient 11 also had a partial thickness RV laceration which was irrigated but not sutured. Patient 12 had a tangential left ventricle injury which was suture-repaired. Patients 7, 8, 9, and 10 all had injuries to the pericardium but no injury to the heart itself.
Follow-up echocardiograms were performed as clinically indicated and are summarized in online supplementary table 2. Four patients in the PCW+drain group had a postoperative TTE, and all showed either no or trivial pericardial effusion, along with other physiologic findings. Three patients in the Sternotomy group had follow-up TTE. Patients 10 and 12 had one follow-up echo each, and both showed no evidence of effusion with other findings. Patient 6, who had a long ICU stay had multiple TTE studies which showed a progressively enlarging pericardial effusion which ultimately improved without intervention.
tsaco-2018-000187supp002.docx (14.1KB, docx)
Discussion
Penetrating injuries to the chest can be rapidly fatal, and this is demonstrated by the high mortality seen with PCIs. It is with this high lethality in mind that current management strategies have evolved. Early in the management of penetrating chest trauma, a PCW was the gold standard for evaluation of possible hemopericardium. At that time, penetrating chest injury with hemopericardium on PCW mandated sternotomy to locate and repair the site of injury. With the development of the FAST examination, which can be performed rapidly at the bedside in any patient with penetrating chest injury, the PCW procedure is rarely performed in the current era.5 17 The current Western Trauma Association (WTA) algorithm for penetrating chest trauma recommends sternotomy for patients with penetrating chest injury with positive cardiac FAST examination.8
Although a sternotomy allows for a thorough cardiac examination, it is a highly morbid procedure. Complications include sternal instability and deep sternal wound infections, which occur in 0.75% to 3% of patients post cardiac surgery.4 10 11 Although uncommon, these complications carry significant morbidity and possible mortality. Although no literature exists about the risks posed specifically to trauma patients requiring sternotomy, one study does list emergency operation as an independent risk factor for sternal wound infection in cardiac surgery patients.10 Significant complications from sternotomies were noted in previous studies on this topic, including death from iatrogenic internal mammary artery injury and mediastinitis requiring sternal debridement and advancement flaps in the RCT performed by Nicol et al. Thorson et al describe a patient undergoing a non-therapeutic sternotomy who suffered an iatrogenic pulmonary injury and developed an infected pericardial effusion. Even without complications, a sternotomy requires several weeks of recovery, and as such should not be considered a benign procedure.
There are several previously published works which have demonstrated a similar management strategy to what we have proposed here.7 12–14 Nagy et al 14 reported using echocardiography to determine presence of hemopericardium after penetrating injury to the box in stable patients, followed by subxiphoid PCW. Thorson7 reported three cases of hemopericardium from traumatic injury (two blunt, one penetrating) managed with PCW and drainage. The strongest and most recent is the work of Nicol12 who performed a prospective RCT, and showed that stable patients with penetrating chest injuries and positive PCW had equivalent outcomes when randomized to sternotomy and pericardial drainage alone. Furthermore, 93% of patients randomized to sternotomy had either a tangential injury or no cardiac injury at all.12 Our study found no hospital deaths in either group, whereas Nicol reported only one death from iatrogenic injury during sternotomy. Thorson’s review of 21 non-therapeutic sternotomies included four deaths, but none from cardiac causes.
In our center, this management strategy was adopted with the utmost consideration for safety, and so the following principles were followed: (1) Only patients hemodynamically stable without evidence of tamponade physiology would be considered for initial PCW. (2) The PCW must be performed in the operating room with the option to rapidly convert to sternotomy. (3) All pericardial blood must be suctioned and lavaged until clear. (4) Cessation of bleeding must be verified prior to leaving the operating room. (5) A pericardial drain is placed to drain any residual fluid and monitor for delayed bleeding. (6) The patients are monitored in the ICU after the procedure.
Several points deserve emphasis. First, in unstable patients with cardiac arrest or tamponade physiology, sternotomy or anterolateral thoracotomy should be performed for immediate chest access. Second, all current literature on this topic comes from high-volume level I trauma centers, with inhouse trauma surgeons and experienced ICU nurses to monitor patients closely for physiologic changes or deterioration. Third, the on-table lavage and observation is imperative, since the goal of lavage is to disrupt any unstable clot which may have formed and could possibly cause delayed bleed.
This management strategy is similar to that employed in managing complications from implantable electronic device (IED) placement. A full-thickness myocardial perforation is a known complication of IED lead placement resulting in hemopericardium. Although unstable patients require open heart surgery to repair perforation, stable patients are routinely managed with observation, pericardiocentesis, and lead extraction and replacement.17 18 Although the injury patterns associated with PCI in our series are clearly higher energy injuries than IED lead perforation, it is worthy to note that this is a well-accepted management strategy to deal with full-thickness myocardial perforation resulting in hemopericardium.
In this series, five cases are reported in which we spared the recommended sternotomy for PCI and hemopericardium, and thus avoided the potential morbidity and extended recovery of this approach. To compare against similar patients undergoing sternotomy, we selected only patients with cardiac OIS 1–3. This includes patients who have injuries to the pericardium, and tangential/partial thickness injuries to the heart muscle itself. This requires the assumption that the injury pattern of the patients in the PCW+drain group matches that of the sternotomy group. Four of the seven patients in the sternotomy group had no cardiac injury. Three patients had cardiac injury, two had suture repair and one had already stopped bleeding at the time of exploration. We think the injury severity is similar, and is, thus, the closest possible comparison available.
The PCW+drain patients had statistically equivalent, but numerically greater, ICU LOS than sternotomy patients (4 vs. 2, P=0.18). This contrasts with the findings of the Nicol’s study, who found a shorter ICU LOS in patients undergoing PCW. This is likely from overly cautious ICU monitoring of patients in the PCW+drain group, whose injuries were never directly visualized. Furthermore, the patients in both groups had other injuries, and so the increased LOS may be unrelated to their PCI. Nonetheless, we suspect that with greater experience with this strategy, the ICU stay should decrease.
This study has weaknesses. Both patient groups are small, so statistical comparison is difficult. This single institution study at a level 1 trauma center may lack generalizability, and the retrospective study design carries inherent inaccuracies. There was no standardized plan for follow-up echocardiogram, and attempts to obtain outpatient echocardiograms have been hindered by patient relocation, poor follow-up, and lack of insurance coverage. This limits our ability to comment on long-term sequelae and outcomes such as delayed mortality. Furthermore, the cardiac injuries in the PCW+drain group were never directly visualized, so it is impossible to be certain if the injury patterns were similar. Since this was not a randomized study, the groups were created at the discretion of the authors. This introduces selection bias, and could affect our results and conclusions.
Although we think that our results are encouraging and suggest a potential change in management for stable patients with suspected PCI, the authors still urge caution if choosing to adopt this management strategy. There are still many issues to address, including the amount of PCW drainage to trigger a sternotomy, timing of pericardial drain removal, length of monitoring in ICU, and frequency of delayed pericardial bleed. Other diagnostic tools deserve evaluation, including on-table flexible mediastinoscopy to evaluate the cardiac injury after PCW.
The current algorithm published by the Western Trauma Association8 for penetrating chest trauma recommends stable patients with suspected cardiac injury undergo a FAST examination. Equivocal or inconclusive examinations may undergo further diagnostic workup, including PCW, whereas patients with positive FAST are recommended to undergo sternotomy. In this setting, the FAST examination has diminished the role of the PCW to detect the presence of cardiac injuries, and this decline in the PCW has been recognized by other authors.5 19 However, in the discussion of management of PCIs, the WTA acknowledges the increasing experience of avoiding sternotomy if the window is ‘mildly’ positive.8 Options discussed include direct cardiac observation, mediastinoscopy or thoracoscopy to inspect the cardiac surface, or application of biologic glues over the surface of the heart in partial thickness injuries.
There is historical context for other injuries which posed diagnostic dilemmas, but now are managed through less invasive means. Laparotomy was originally the gold standard for evaluation in blunt abdominal trauma. This was followed by direct visualization of the abdomen through a needlescope,20 then diagnostic peritoneal lavage (DPL),21 22 followed by CT scanning.23 24 In the current era, CT scanning is the gold standard for evaluation of the abdomen in stable patients, and DPL is rarely performed. We think that in stable patients, the PCW and lavage should function in similar capacity to DPL by ruling out patients with suspected PCI who do not require sternotomy.
In light of this and other studies’ findings demonstrating good outcomes for this management strategy,11–14 the authors propose a modification to WTA’s algorithm for penetrating chest trauma8 in stable patients (figure 2). If cardiac injury is suspected and the patient is hemodynamically stable, FAST is performed. If positive, PCW should be done in the operating room. If the PCW is negative for blood, no further operative intervention is warranted. If the PCW is positive for blood, on-table pericardial lavage should be performed although closely monitoring the bloody return and patient hemodynamics. With continued bleeding, or instability, a sternotomy and exploration should be done. If stable and the bleeding stops, a pericardial drain should be placed and the patient admitted to the ICU. On-table TEE should be performed when available, and a follow-up echocardiogram should be obtained in the immediate postoperative period to monitor for recurrent pericardial fluid. In selected patients, we think this strategy could help avoid the unnecessary morbidity of sternotomy in patients who do not need it, although identifying those who should undergo more invasive exploration to identify their injuries.
Conclusions
Patients presenting with penetrating chest injuries and pericardial effusion, who are hemodynamically stable, may safely undergo an initial PCW, lavage and drainage. Patients with continued bleeding or instability should be explored by sternotomy. These ideas should be studied on a larger scale with the expectation to develop algorithms to limit sternotomy to patients in whom it is necessary.
Acknowledgments
The authors thank Kimberly Cerasoli and Elizabeth Snavely, Trauma Registrars at University Medical Center of Southern Nevada, for their help with this project.
Footnotes
Presented at: Presented on March 7, 2017 at the 47th Annual Meeting of the Western Trauma Association at the Cliff Lodge in Snowbird, Utah.
Contributors: All authors made significant contributions to the completion of this project, and have had input in the final article submission. PJC: Study inception and design, data collection and analysis, creating tables and figures, drafting and critical revisions of the article. CFM: Data collection and analysis, creating tables and figures, drafting and critical revisions of the article. DRF: Data analysis, drafting and critical revisions of the article. PPP: Data collection and analysis DAK: Drafting and critical revisions of the article. EC: Data collection, critical revisions of the article. JJF: Sponsored project, final revision and approval of the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: University Medical Center Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Asensio JA, Soto SN, Forno W, Roldan G, Petrone P, Salim A, Rowe V, Demetriades D. Penetrating cardiac injuries: a complex challenge. Injury 2001;32:533–43. 10.1016/S0020-1383(01)00068-7 [DOI] [PubMed] [Google Scholar]
- 2. Asensio JA, Murray J, Demetriades D, Berne J, Cornwell E, Velmahos G, Gomez H, Berne TV. Penetrating cardiac injuries: a prospective study of variables predicting outcomes. J Am Coll Surg 1998;186:24–34. 10.1016/S1072-7515(97)00144-0 [DOI] [PubMed] [Google Scholar]
- 3. Pereira BM, Nogueira VB, Calderan TR, Villaça MP, Petrucci O, Fraga GP. Penetrating cardiac trauma: 20-y experience from a university teaching hospital. J Surg Res 2013;183:792–7. 10.1016/j.jss.2013.02.015 [DOI] [PubMed] [Google Scholar]
- 4. Ståhle E, Tammelin A, Bergström R, Hambreus A, Nyström SO, Hansson HE. Sternal wound complications–incidence, microbiology and risk factors. Eur J Cardiothorac Surg 1997;11:1146–53. 10.1016/S1010-7940(97)01210-4 [DOI] [PubMed] [Google Scholar]
- 5. Morse BC, Mina MJ, Carr JS, Jhunjhunwala R, Dente CJ, Zink JU, Nicholas JM, Wyrzykowski AD, Salomone JP, Vercruysse GA, et al. . Penetrating cardiac injuries: a 36-year perspective at an urban, Level I trauma center. J Trauma Acute Care Surg 2016;81:623–31. 10.1097/TA.0000000000001165 [DOI] [PubMed] [Google Scholar]
- 6. Rhee PM, Foy H, Kaufmann C, Areola C, Boyle E, Maier RV, Jurkovich G. Penetrating cardiac injuries: a population-based study. J Trauma 1998;45:366–70. [DOI] [PubMed] [Google Scholar]
- 7. Karmy-Jones R, Namias N, Coimbra R, Moore EE, Schreiber M, McIntyre R, Croce M, Livingston DH, Sperry JL, Malhotra AK, et al. . Western Trauma Association critical decisions in trauma: penetrating chest trauma. J Trauma Acute Care Surg 2014;77:994–1002. 10.1097/TA.0000000000000426 [DOI] [PubMed] [Google Scholar]
- 8. Saadia R, Levy RD, Degiannis E, Velmahos GC. Penetrating cardiac injuries: clinical classification and management strategy. Br J Surg 1994;81:1572–5. 10.1002/bjs.1800811106 [DOI] [PubMed] [Google Scholar]
- 9. Heilmann C, Stahl R, Schneider C, Sukhodolya T, Siepe M, Olschewski M, Beyersdorf F. Wound complications after median sternotomy: a single-centre study. Interact Cardiovasc Thorac Surg 2013;16:643–8. 10.1093/icvts/ivs554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Borger MA, Rao V, Weisel RD, Ivanov J, Cohen G, Scully HE, David TE. Deep sternal wound infection: risk factors and outcomes. Ann Thorac Surg 1998;65:1050–6. 10.1016/S0003-4975(98)00063-0 [DOI] [PubMed] [Google Scholar]
- 11. Nicol AJ, Navsaria PH, Hommes M, Ball CG, Edu S, Kahn D. Sternotomy or drainage for a hemopericardium after penetrating trauma: a randomized controlled trial. Ann Surg 2014;259:438–42. 10.1097/SLA.0b013e31829069a1 [DOI] [PubMed] [Google Scholar]
- 12. Thorson CM, Namias N, Van Haren RM, Guarch GA, Ginzburg E, Salerno TA, Schulman CI, Livingstone AS, Proctor KG. Does hemopericardium after chest trauma mandate sternotomy? J Trauma Acute Care Surg 2012;72:1518–25. 10.1097/TA.0b013e318254306e [DOI] [PubMed] [Google Scholar]
- 13. Navsaria PH, Nicol AJ. Haemopericardium in stable patients after penetrating injury: is subxiphoid pericardial window and drainage enough? A prospective study. Injury 2005;36:745–50. 10.1016/j.injury.2004.08.005 [DOI] [PubMed] [Google Scholar]
- 14. Nagy KK, Lohmann C, Kim DO, Barrett J. Role of echocardiography in the diagnosis of occult penetrating cardiac injury. J Trauma 1995;38:859–62. 10.1097/00005373-199506000-00004 [DOI] [PubMed] [Google Scholar]
- 15. Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma 1989;29:623–9. 10.1097/00005373-198905000-00017 [DOI] [PubMed] [Google Scholar]
- 16. Moore EE, Malangoni MA, Cogbill TH, Shackford SR, Champion HR, Jurkovich GJ, McAninch JW, Trafton PG. Organ injury scaling. IV: thoracic vascular, lung, cardiac, and diaphragm. J Trauma 1994;36:299–300. [PubMed] [Google Scholar]
- 17. Ohlow MA, Lauer B, Brunelli M, Geller JC. Incidence and predictors of pericardial effusion after permanent heart rhythm device implantation: prospective evaluation of 968 consecutive patients. Circ J 2013;77:975–81. [DOI] [PubMed] [Google Scholar]
- 18. Huang XM, Fu HX, Zhong L, Osborn MJ, Asirvatham SJ, Sinak LJ, Cao J, Friedman PA, Cha YM. Outcomes of lead revision for myocardial perforation after cardiac implantable electronic device placement. J Cardiovasc Electrophysiol 2014;25:1119–24. 10.1111/jce.12457 [DOI] [PubMed] [Google Scholar]
- 19. Kang N, Hsee L, Rizoli S, Alison P. Penetrating cardiac injury: overcoming the limits set by Nature. Injury 2009;40:919–27. 10.1016/j.injury.2008.12.008 [DOI] [PubMed] [Google Scholar]
- 20. McSwain NE. Visual examination for blunt abdominal trauma. JACEP 1977;6:56–7. 10.1016/S0361-1124(77)80034-8 [DOI] [PubMed] [Google Scholar]
- 21. Engrav LH, Benjamin CI, Strate RG, Perry JF. Diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma 1975;15:854–9. 10.1097/00005373-197510000-00003 [DOI] [PubMed] [Google Scholar]
- 22. Olsen WR, Hildreth DH. Abdominal paracentesis and peritoneal lavage in blunt abdominal trauma. J Trauma 1971;11:824–9. 10.1097/00005373-197110000-00002 [DOI] [PubMed] [Google Scholar]
- 23. Schreiber MA, Gentilello LM, Rhee P, Jurkovich GJ, Maier RV. Limiting computed tomography to patients with peritoneal lavage-positive results reduces cost and unnecessary celiotomies in blunt trauma. Arch Surg 1996;131:954–9. 10.1001/archsurg.1996.01430210052010 [DOI] [PubMed] [Google Scholar]
- 24. Meyer DM, Thal ER, Weigelt JA, Redman HC. Evaluation of computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma 1989;29:1168–72. 10.1097/00005373-198908000-00017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2018-000187supp001.docx (17.6KB, docx)
tsaco-2018-000187supp002.docx (14.1KB, docx)