Abstract
Objective
Few data exist regarding physician attitudes and implementation of family-centred rounds (FCR) in cardiovascular care. This study aimed to assess knowledge and attitudes among cardiologists and cardiology fellows regarding barriers and benefits of FCRs.
Methods
An electronic, web-based questionnaire was nationally distributed to cardiology fellows and attending cardiologists.
Results
In total, 118 subjects were surveyed, comprising cardiologists (n=64, 54%) and cardiology fellows (n=54, 46%). Overall, 61% of providers reported participating in FCRs and 64% felt family participation on rounds benefits the patient. Both fellows and cardiologists agreed that family rounds eased family anxiety (fellows, 63%; cardiologists, 56%; p=0.53), improved communication between the medical team and the patient and family (fellows, 78%; cardiologists, 61%; p=0.18) and improved patient safety (fellows, 59%; cardiologists, 47%; p=0.43). Attitudes regarding enhancement of trainee education were similar (fellows, 69%; cardiologists, 55%; p=0.19). Fellows and cardiologists felt that family increased the duration of rounds (fellows, 78%; cardiologists, 80%; p=0.18) and led to less efficient rounds (fellows, 54%; cardiologists, 58%; p=0.27).
Conclusion
The majority of cardiologists and fellows believed that FCRs benefited families, communication and patient safety, but led to reduced efficiency and longer duration of rounds.
Keywords: Perceptions, family, rounds
Key messages.
What is already known about this subject?
Family-centred rounds (FCR) are associated with improved satisfaction for both the family and patient, may ease patient and family anxiety and allow for collaborative information exchange and decision-making.
What does this study add?
Our study is the first to investigate the perceived benefits and barriers of FCRs among cardiovascular medicine physicians. We found that the majority of cardiologists and fellows agreed that FCRs improve workforce communication and nursing satisfaction, ease family anxiety and improve patient safety.
How might this impact on clinical practice?
This study will help facilitate further investigations regarding the merits of FCRs in cardiovascular medicine and in particular in the Cardiac Intensive Care Unit (CICU). Future initiatives will need to highlight the benefits of FCRs and address the potential concerns for optimal outcomes.
Introduction
Family-centred rounds (FCR) are a multidisciplinary process in which patients and/or family members are present and actively participate in rounds and medical decision-making.1 FCRs are associated with improved satisfaction for both the family and the patient as well as the medical staff,2 may ease patient and family anxiety and allow for collaborative information exchange and decision-making.3 Additionally, family-support interventions and inclusivity in the intensive care unit (ICU) is associated with improvement in staff-family communication and decreases ICU length of stay.4 Because of these benefits, the Health and Medicine Division in 2001 advocated for healthcare delivery systems to become more patient centred and tailored to patient preferences.5 In response, national organisations such as the American College of Critical Care Medicine and the American Academy of Pediatrics advocated for FCRs to be an integral part of care, stressing the need to incorporate a patient’s family in the clinical decision-making process of the patient.6 7
Within cardiology, there are fewer guidelines advocating for implementation of FCRs. While the American College of Cardiology (ACC) promotes a patient-centred approach to cardiovascular health in its 2012 healthy policy position paper, it did not specifically advocate for FCRs.8 Because of the lack of information on the impact of FCRs in cardiology, this study aimed to gather data on FCRs in the delivery of cardiovascular care. The primary outcome of the study was to assess knowledge and attitudes among cardiologists and cardiology fellows regarding barriers and benefits of FCRs. The secondary outcome was to evaluate the associations of these attitudes with specific physician characteristics.
Methods
We conducted a cross-sectional survey study of cardiology fellows and practising cardiologists across the USA. Physicians were identified via the ACC Board of Governors list-serve, the cardiology programme director list-serve, as well as through community-affiliated cardiovascular specialists in the state of Maryland. An electronic, web-based questionnaire (SurveyMonkey, San Mateo, CA) was sent via email to an estimated 40 000 cardiologists and fellows. The survey instrument’s structure was based on the Consolidated Framework for Implementation Research (CFIR), a widely used comprehensive health services research implementation technique, as well as previously used FCR surveys.2 9 10 CFIR captures five domains: intervention characteristics, outer setting, inner setting, characteristics of individuals and process.9 Our survey included questions from each of the five domains in order to effectively and methodically study cardiologists’ perceptions of FCRs. The questionnaire contained a total of 22 questions utilising Likert scale (1–5) responses, including a section for free-form comments (figure 1).
Figure 1.
Survey questionnaire.
We analysed data and performed descriptive statistics using STATA V.13.1 (StataCorp, College Station, TX). We reported Likert scale responses as proportions and completed univariate analyses of the association between respondent characteristics for each question using Fisher’s exact test, comparing the distribution of all possible answers (agreed, neutral, disagreed and not answered). Additionally, we constructed a Pearson correlation matrix to evaluate the relationship among the continuous variables. Finally, we used pile-sort analysis to assess free-form comments.11
Results
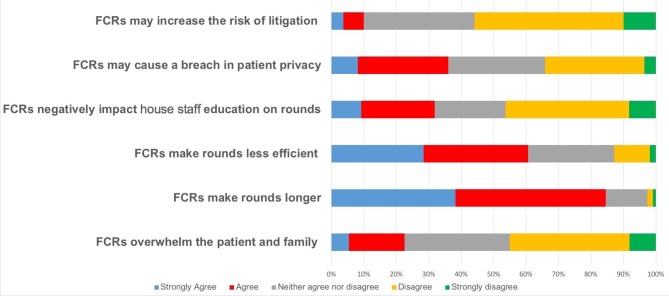
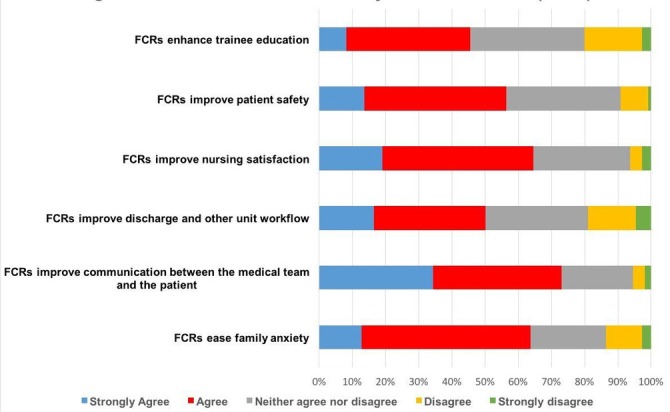
In total, there were 118 respondents with a response rate of<1%, comprising 64 cardiologists (54%) and 54 cardiovascular disease fellows (46%) (table 1). This response rate is typical for internet-based unsolicited surveys. Overall, 61% of providers reported participating in FCRs and 64% felt family participation on rounds benefits the patient. Perceived benefits among all respondents included eased family anxiety (64% agreed or strongly agreed), improved workforce communication (73% agreed or strongly agreed), improved nursing satisfaction (65% agreed or strongly agreed) and improved patient safety (56% agreed or strongly agreed) (figure 2). In contrast, perceived barriers included increased duration of rounds (85% agreed or strongly agreed) and less efficient rounds (61% agreed or strongly agreed) (figure 3).
Table 1.
Baseline characteristics
| Participant characteristics | Frequencies (%) |
| Number of years since completion of general cardiology training | |
| Current fellow | 54 (45.8) |
| 0–5 years | 10 (8.5) |
| 5–10 years | 10 (8.5) |
| 10–15 years | 7 (5.9) |
| >15 years | 37 (31.4) |
| Type of provider | |
| Adult provider | 112 (94.9) |
| Paediatric provider | 3 (2.5) |
| Both | 3 (2.5) |
| In which type of setting do you spend the majority of your time? | |
| University hospital | 77 (65.3) |
| Community hospital | 22 (18.6) |
| Outpatient | 18 (15.3) |
| Is there a residency programme at your institution? | |
| No | 10 (8.5) |
| Yes | 108 (91.5) |
| Is there a cardiology fellowship at your institution? | |
| No | 16 (13.6) |
| Yes | 102 (86.4) |
| I participate in family-centred rounds in my practice. | |
| Never | 39 (33.1) |
| Sometimes | 71 (60.2) |
| Always | 1 (0.9) |
Figure 2.
Perceived benefits to family-centred rounds (FCR).
Figure 3.
Perceived barriers to family-centred rounds (FCR).
When comparing the distribution of responses between fellows and cardiologists, no significant differences were found. Both fellows and cardiologists agreed that FCRs eased family anxiety (fellows, 63% agreed or strongly agreed; cardiologists, 56% agreed or strongly agreed; p=0.53), improved communication between the medical team and the patient and family (fellows, 78% agreed or strongly agreed; cardiologists, 61% agreed or strongly agreed; p=0.18) and improved patient safety (fellows, 59% agreed or strongly agreed; cardiologists, 47% agreed or strongly agreed; p=0.43). Attitudes regarding enhancement of trainee education were similar (fellows, 69% agreed or strongly agreed; cardiologists, 55% agreed or strongly agreed; p=0.19). Fellows and cardiologists felt that barriers to FCRs included longer duration of rounds (fellows, 78% agreed or strongly agreed; cardiologists, 80% agreed or strongly agreed; p=0.18) and less efficient rounds (fellows, 54% agreed or strongly agreed; cardiologists, 58% agreed or strongly agreed; p=0.27).
The perceived benefits and barriers of FCRs were similar between physicians based at different primary practice sites (university hospital vs other). However, practitioners with less than 10 years of experience (junior attendings) had a different distribution of answers to two questions when compared with more experienced practitioners (senior attendings). Senior attendings were more likely to agree that families should be active participants in decision-making during rounds (senior, 43% agreed or strongly agreed; junior, 30% agreed or strongly agreed; p=0.02) and that FCRs ease family anxiety (senior, 59% agreed or strongly agreed; junior, 50% agreed or strongly agreed; p=0.03).
The Pearson correlation matrix of survey answers revealed several findings. The positive aspects of FCRs, as indicated by survey respondents, correlated well with the attitude that FCRs are beneficial (ease family anxiety, r=0.7; improve communication, r=0.79). In contrast, the negative aspects of FCRs had lower correlation with the attitude that family-centred rounds are beneficial (longer rounds, r=0.1; breach of privacy, r=0.28). Although the cardiologists and fellows indicated their perceived barriers of FCRs, they did not have a decisive effect on the overall attitude towards FCRs.
Discussion
Our study is the first to investigate the perceived benefits and barriers of FCRs among cardiovascular medicine physicians. We found that the majority of survey respondents agreed that FCRs improve workforce communication and nursing satisfaction, ease family anxiety and improve patient safety. At the same time, most providers felt that FCRs make rounds longer and less efficient. A minority of cardiologists and fellows also thought that family-centred rounds may cause a breach in patient privacy, negatively impact house staff education or overwhelm patients and families.
The survey views are largely supportive of FCRs, which is important, since FCRs are recognised as the standard of care within the ICU.1 In particular, the Society of Critical Care Medicine endorses the option of participating in interdisciplinary team rounds to improve satisfaction with communication and increase family engagement,6 because FCRs ease family anxiety, increase family and staff satisfaction, improve communication between provider and family, improve staff workflow, improve time management, improve trainee education and improve patient safety.2 3 10 12 13 Outside of the ICU, there are no guidelines specifically advocating for FCRs for cardiac patients, although the ACC does advocate for patient-centred care.8
Perhaps our survey respondents thought favourably of FCRs, because they perceived improved communication and patient safety (73%, 56%) as a result of implementing FCRs, which has been noted by physicians in other disciplines.14 In one particular initiative led by cardiac surgeons, FCRs resulted in increased staff satisfaction, including nurses, and a reduction in surgical mortality rates.15 16 In other prospective studies, FCRs were associated with high satisfaction among both patients and families, including a study on an internal medicine ward which revealed high rates of staff, patient and family satisfaction (83%, 96% and 97%, respectively).3 17–19 Likely FCRs lead to high satisfaction rates because they allow participants increase opportunities to hear and contribute new information, as well as listen and participate in clinical decisions.3 Finally, our survey respondents thought that FCRs ease family anxiety, perhaps because a structured daily routine in which the family is able to listen and participate in staff discussions can alleviate festering family concerns.3
Survey respondents also noted barriers, and were especially concerned about the perceived increase in rounds duration and in inefficiency, both of which have been noted in other studies.10 However, several time-impact studies have found minimal changes on rounds duration after implementing FCRs,10 20 and one study found a decrease in rounding time.2 In addition, 32% of survey participants felt that FCRs could negatively affect house staff teaching and education. Fewer studies have evaluated the impact on education, although one prior study described similar concerns for decreases in didactic teaching and efficiency.2 Interestingly, one study found no objective changes in medical student performance on shelf exams after implementation of FCRs.21
While our study revealed no differences in perceptions of FCRs between fellows and practising cardiologists, our study is the first to note distinctions between less and more experienced practitioners. A greater proportion of more experienced practitioners felt that families should be active participants in decision-making and that FCRs ease family anxiety. Although this finding may seem counterintuitive, given that FCRs are a relatively recent phenomenon, perhaps the senior attendings’ greater clinical experience shaped their perceptions about the role of family input. Additionally, senior attendings are more likely to have experienced the patient side of medicine, which may have also affected their perspectives of FCRs.
Our findings and conclusions have several limitations. The small sample size limits the ability to generalise our results to the entire cardiovascular community. Furthermore, our survey study has an inherent voluntary response bias, as it only assessed willing respondents who may have an inherent interest in FCRs. Although our survey instrument was based on prior FCR-related studies, it was not independently validated. Finally, we limited the number of questions to maintain a 3 min survey completion time, and thus not all perceived benefits and barriers were studied. Despite these limitations, our study findings remain important, and can help buttress future initiatives that advocate for FCRs.
Conclusions
The majority of cardiologists and fellows believed that FCRs benefit families, enhance communication and improve patient safety. However, many also felt that FCRs reduce efficiency and increase the duration of rounds. While we encourage strategies to implement and evaluate FCRs in cardiovascular care, future initiatives will need to highlight the benefits and address the potential concerns for optimal outcomes.
Footnotes
Contributors: All the authors were actively involved in the planning, conduct and reporting of this original work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: This study was granted exempt status by the Institutional Review Board of the University of Maryland, Baltimore.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data collected in our study which are not highlighted in our manuscript are available for review by contacting the corresponding author.
References
- 1. Committee on Hospital Care. American Academy of P. Family-centered care and the pediatrician’s role. Pediatrics 2003;112:691–7. [PubMed] [Google Scholar]
- 2. Rappaport DI, Ketterer TA, Nilforoshan V, et al. Family-centered rounds: views of families, nurses, trainees, and attending physicians. Clin Pediatr 2012;51:260–6. 10.1177/0009922811421002 [DOI] [PubMed] [Google Scholar]
- 3. Davidson JE. Family presence on rounds in neonatal, pediatric, and adult intensive care units. Ann Am Thorac Soc 2013;10:152–6. 10.1513/AnnalsATS.201301-006PS [DOI] [PubMed] [Google Scholar]
- 4. White DB, Angus DC, Shields AM. A Randomized trial of a family-support intervention in intensive care un Units. N Engl J Med 2018;378:2365–75. 10.1056/NEJMoa1802637 [DOI] [PubMed] [Google Scholar]
- 5. Institute of M. Crossing the quality chasm: a new health system for the 21st century, 2011. [PubMed] [Google Scholar]
- 6. Davidson JE, Aslakson RA, Long AC. Guidelines for family-centered care in the neonatal, pediatric, and adultGuidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Crit Care Med 2017;45:103–28. 10.1097/CCM.0000000000002169 [DOI] [PubMed] [Google Scholar]
- 7. Schor EL. American Academy of Pediatrics Task Force on the F. Family pediatrics: report of the Task Force on the Family. Pediatrics 2003;111:1541–71. [PubMed] [Google Scholar]
- 8. Walsh MN, Bove AA, Cross RR, et al. ACCF 2012 health policy statement on patient-centered care in cardiovascular medicine: a report of the American College of Cardiology Foundation Clinical Quality Committee. J Am Coll Cardiol 2012;59:2125–43. 10.1016/j.jacc.2012.03.016 [DOI] [PubMed] [Google Scholar]
- 9. Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:504–50. 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mittal VS, Sigrest T, Ottolini MC, et al. Family-centered rounds on pediatric wards: a PRIS network survey of US and Canadian hospitalists. Pediatrics 2010;126:37–43. 10.1542/peds.2009-2364 [DOI] [PubMed] [Google Scholar]
- 11. Bernard HR, Ryan GW. Classes of and F. Analyzing qualitative data: systematic approaches. Los Angeles Calif. Sage 2010. [Google Scholar]
- 12. Rappaport DI, Cellucci MF, Leffler MG. Implementing family-centered rounds: pediatric residents’ perceptions. Clin Pediatr 2010;49:228–34. 10.1177/0009922809346568 [DOI] [PubMed] [Google Scholar]
- 13. Mittal V. Family-centered rounds: a decade of growth. Hosp Pediatr 2014;4:6–8. 10.1542/hpeds.2013-0100 [DOI] [PubMed] [Google Scholar]
- 14. Rosen P, Stenger E, Bochkoris M, et al. Family-centered multidisciplinary rounds enhance the team approach in pediatrics. Pediatrics 2009;123:e603–e608. 10.1542/peds.2008-2238 [DOI] [PubMed] [Google Scholar]
- 15. Kendall EM. Improving patient care with collaborative rounds. Am J Health Syst Pharm 2003;60:132–5. [DOI] [PubMed] [Google Scholar]
- 16. Uhlig PN, Brown J, Nason AK. John M. Eisenberg patient safety awards. System innovation: Concord hospital. Jt Comm J Qual Improv 2002;28:666–72. [DOI] [PubMed] [Google Scholar]
- 17. Landry MA, Lafrenaye S, Roy MC, et al. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics 2007;120:275–80. 10.1542/peds.2007-0107 [DOI] [PubMed] [Google Scholar]
- 18. Lewis C, Knopf D, Chastain-Lorber K, et al. Patient, parent, and physician perspectives on pediatric oncology rounds. J Pediatr 1988;112:378–84. 10.1016/S0022-3476(88)80316-0 [DOI] [PubMed] [Google Scholar]
- 19. Rotman-Pikielny P, Rabin B, Amoyal S, et al. Participation of family members in ward rounds: Attitude of medical staff, patients and relatives. Patient Educ Couns 2007;65:166–70. 10.1016/j.pec.2006.07.003 [DOI] [PubMed] [Google Scholar]
- 20. Aronson PL, Yau J, Helfaer MA, et al. Impact of family presence during pediatric intensive care unit rounds on the family and medical team. Pediatrics 2009;124:1119–25. 10.1542/peds.2009-0369 [DOI] [PubMed] [Google Scholar]
- 21. Kimbrough TN, Heh V, Wijesooriya NR, et al. Family-centered rounds and medical student performance on the NBME pediatrics subject (shelf) examination: a retrospective cohort study. Med Educ Online 2016;21:30919 10.3402/meo.v21.30919 [DOI] [PMC free article] [PubMed] [Google Scholar]