Abstract
Background:
Behavior change is notoriously difficult to achieve within health care systems. Successful implementation of the I-PASS handoff bundle with subsequent decreases in medical errors and preventable adverse events represents an example of successful transformational change within academic medical centers.
Objective:
We designed a campaign to support and enhance uptake of the I-PASS handoff bundle at 9 study sites from 2011 to 2013.
Methods:
Following Kotter’s model of transformational change, we established urgency using local data and institutional mandates, and site leaders built local guiding coalitions with institutional leaders, key faculty, and Chief Residents. We created and communicated our vision using a branded campaign and empowered others to act by soliciting and acting on feedback and supporting systems changes. Site leaders planned for and created short-term wins by recognizing residents who engaged with I-PASS, consolidated improvements, and institutionalized new approaches.
Results:
Implementation of I-PASS was successful, with achievement of substantial improvements in rates of medical errors and preventable adverse events. Data from the initial I-PASS study have continued to drive a national campaign that has included national recognition by leaders in the field of patient safety and pediatrics. Momentum has increased significantly to support mentored implementation of the I-PASS handoff program at over 35 academic medical centers across North America.
Conclusions:
I-PASS provides an example of transformational change achieved through a combination of educational interventions and change management to address resistance/barriers, supported by a robust campaign. We encourage others in academic medicine to consider using change models, including campaigns, to support health care improvement programs.
INTRODUCTION
Academic medical centers routinely engage in evidence-based practice. However, behavior change is notoriously difficult to achieve.1 Although innovations may diffuse passively within health care systems,2 it has been estimated to take 17 years from the time a discovery is made until universal practice change is achieved.3 Targeted leadership, support, and motivation may be required to drive behavior change among physicians.
Successful models for leading transformational organizational change have been described in the business literature. In Kotter’s 8-step model4 (outlined in Table 1), the key steps in effecting transformational change include establishing a sense of urgency, building a powerful guiding coalition of leaders, creating and communicating the vision, empowering others to act on the vision, planning for and creating short-term wins, consolidating improvements, and institutionalizing new approaches effectively. Within academic medical centers, physician champions and high-level leaders are essential to drive behavior change.1 This change must be aligned with the mission, vision, and values of the institution.
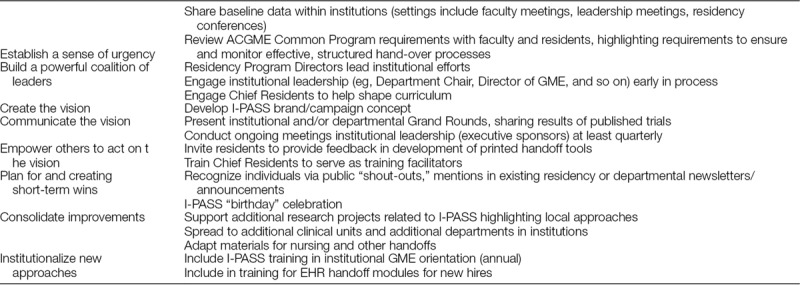
Table 1.
Examples of Specific Techniques from Kotter’s 8-step Model4
In addition to using business change models, medical experts have used campaigns to engage physicians in desirable behaviors. The Choosing Wisely campaign, led by the American Board of Internal Medicine Foundation, has been successful at engaging all major medical specialties to develop specific evidence-based recommendations intended to reduce unnecessary care.5 The Surviving Sepsis campaign sponsored by the Society of Critical Care Medicine has led to implementation of best practices to reduce preventable death from sepsis.6 Similarly the 100,000 Lives Campaign galvanized energy and attention around patient safety with a focus on evidence-based steps to reduce patient deaths.7 In all these campaigns, the purpose was to use process measures (ie, behavior and systems-level changes) to achieve outcome measures (ie, increased value, decreased harms).
I-PASS is an evidence-based handoff bundle,8 which was implemented and rigorously studied on non-ICU inpatient “medical-surgical” units at 9 North American pediatrics residency programs. The handoff bundle is centered on the I-PASS mnemonic (illness severity, patient summary, action list, situation awareness and contingency plans, and synthesis by receiver) and includes teamwork training adapted from TeamSTEPPS,9 and changes to printed and verbal handoffs. The study was approved by the institutional review boards at all participating institutions. Successful implementation of the bundle was associated with significant changes in handoff processes, and a 23% reduction in medical errors and a 30% reduction in preventable adverse events (harms) to patients, without lengthening the time spent on handoffs.10
Implementation of the I-PASS handoff bundle required institutions to achieve transformational change in both processes (eg, communication practices, team work) and structures (eg, physical space, computerized templates). Here, we describe the importance of incorporating a campaign as a key element of the I-PASS bundle. The I-PASS campaign, framed using Kotter’s model (Table 1), was a key element of the I-PASS bundle and helped overcome barriers to drive transformational change efforts at the study sites.
CREATING THE CLIMATE FOR CHANGE
We began by analyzing our target audience via needs assessments with stakeholders at 9 pediatrics institutions.11 Stakeholders included residents, chief residents, front-line faculty, and program directors. Our needs assessment revealed significant variation in handoff content and process (eg, majority of institutions did not train residents in handoffs, did not provide supervision, and did not use a structured handoff mnemonic), and also identified a large population of physicians who would potentially benefit from an improved handoff process. Based on this needs assessment, we designed core curricula to include all key stakeholders and focused a campaign on engaging these stakeholders over the 2011–2013 study period. The implementation process was designed following Kotter’s 8 steps4: Establish a sense of urgency; Build a powerful coalition of leaders; Create the vision; Communicating the vision; Empower others to act on the vision; Plan for and creating short-term wins; Consolidate improvements; Institutionalize new approaches.
We established a sense of urgency by sharing data on current gaps in care including the alarmingly high rates of handoff-related medical errors and miscommunications described by the Institute of Medicine,12 including the consistently high levels of communication failures13 and the lack of improvement over time.14 We also shared pilot data to demonstrate that meaningful change was possible.15 These data were generally shared in single meetings with high-level leaders, at division faculty meetings (generally with monthly updates/check-ins), individual stakeholder meetings and at institutional Grand Rounds presentations.
From the outset of our project, we identified the importance of forming a powerful guiding coalition to help tailor the message to multiple audiences. Although the primary audience for the change was front-line providers, specifically residents and faculty, we sought early engagement of high-level leaders, including the Chief Executive Officers and the Chairs of Pediatrics. Other high-level leaders, such as Chief Medical Officers, Patient Safety Officers, Chief Nurses, and Program Directors, contributed to our guiding coalition. At each site, we also identified champions to do the bulk of the training and lead implementation efforts.
When resistance to change was encountered, as was the case to varying degrees at all sites, we reinforced pilot data, needs assessment data, and high-level mandates for change. These efforts benefited from the contemporaneously establishment by the Accreditation Council for Graduate Medical Education (ACGME) of new requirements to teach and monitor transitions of care. At that time, none of the 9 sites we surveyed had a standardized approach to teaching and monitoring handoffs.16
Chief Residents can be key drivers of the hidden curriculum17 and can therefore role model early adoption of new innovations within residency programs. We engaged Chief Residents at a very early stage by inviting them to provide feedback on the bundle. They identified barriers to change and suggested strategies for effective change management at their institutions. Among the barriers identified were challenges with getting all providers trained, existing parallel signouts by level rather than group signouts, and most importantly overall” buy-in” to the potential benefits of the change. The Chief Residents also helped develop the national branding strategy for the I-PASS campaign, including participation in a competition to identify the tagline, which would ultimately accompany the curriculum and campaign (“Better Handoffs. Safer Care.”).
Faculty leaders formed a second group of early adopters as they were engaged both as participants and champions. Faculty champions on inpatient care teams participated in trainings alongside residents to serve as models, and subsequently observed handoffs and gave feedback to residents. Many faculty were hesitant to commit to the extra time required to observe resident handoffs, especially early morning and end-of-day. We encouraged alternative strategies such as observing preclinic handoffs, and engaging nocturnists to help. In addition, faculty were incentivized with Maintenance of Certification Part 4 Credit from the American Board of Pediatrics.18
Finally, we applied for and received support from the Initiative for Innovation in Pediatric Education.19 This recognition by our field’s education leaders elevated the project’s status within our institutions and among peers and provided additional support to our guiding coalition.
Drawing on lessons from both medical and nonmedical fields, we created and communicated our vision in the form of a branded campaign. We hired a graphic designer to create an I-PASS logo (Fig. 1). The logo was based on an infinity loop to reinforce the continuous passage of information without breaks. Using this logo, items such as posters, pocket cards, monitor frames, and lanyards were developed to provide visual reinforcement.20 The message was further communicated through “Just in Time” reinforcement modules (20-minute presentations focusing on single topics/domains), daily I-PASS tips, and custom fortune cookies with I-PASS-themed fortunes (Fig. 2). Most importantly, direct reinforcement via faculty observation of residents was recommended at least twice per 4-week block.
Fig. 1.

I-PASS logo and tagline.
Fig. 2.
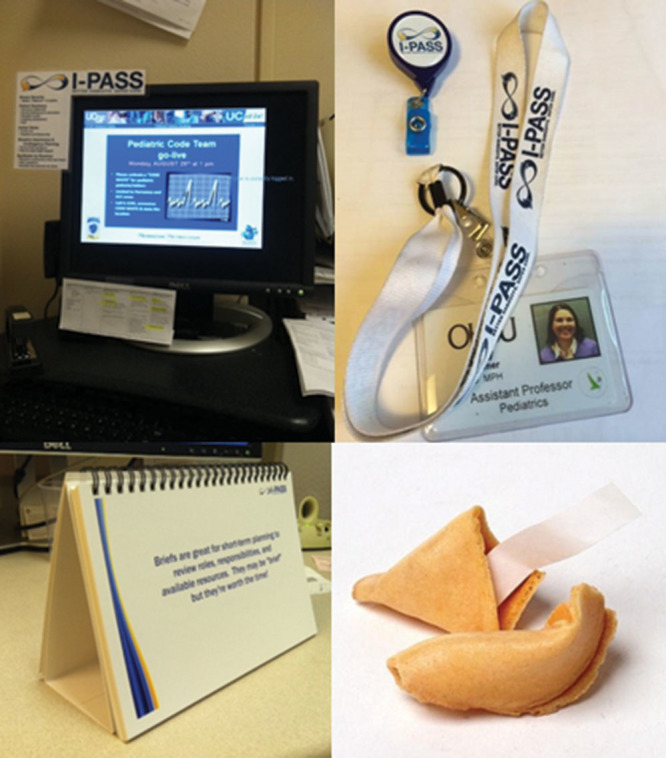
I-PASS campaign materials including screen frames, ID badge clips/lanyards, daily tip booklet, and fortune cookies.
In communicating the vision, the importance of the launch at the time of initial institutional rollout cannot be underestimated. We were training residents and faculty with a formal curriculum, but we were also aware of the potential for hidden curricula in academic medical centers17—specifically the notion that if residents were not supported at the organizational level, they were unlikely to adopt and/or sustain I-PASS. Site-launches included presenting the evidence and the I-PASS handoff program at departmental Grand Rounds, initial meetings with faculty champions (generally at Division faculty meetings) and front-line providers (residents and NPs at other teaching conferences), the actual trainings, and the campaign materials. Over the course of the implementation, most site leads met or otherwise communicated with champions on a monthly basis to support observations, and most checked in with front-line provider teams more than once per month.
Program Directors were given the responsibility of leading the trainings, whereas Chief Residents were engaged as small group facilitators to highlight them as early adopters. Two hundred sixty seven total faculty participated in resident trainings or completed observations across the 9 institutions, with most sites having 2–3 identified site leaders. Sites were strongly encouraged to ensure that all faculty were trained and participated in observations, though it is likely that there were some faculty who supervised residents but were neither trained nor participated in observations. Eight hundred eighty-five residents were trained, representing 91% of pediatrics residents at the 9 institutions. Site leaders and champions were publically identified and praised. As part of the launch, campaign elements were placed in workspaces and champions supported teams and encouraged a “buzz” about the curriculum.
ENGAGING AND ENABLING THE ORGANIZATION
Well-communicated plans and a guiding coalition are necessary but not sufficient. Institutional obstacles need to be overcome to empower others to act on the vision. It was important that residents were supported as they made adaptations to their workflow—even small obstacles could have easily been perceived as major impediments. Where possible, we worked closely with medical informatics teams to make changes in our electronic health records (EHRs) so that printed handoff documents could be aligned with I-PASS, and therefore help facilitate rather than impede uptake. These modifications to EHRs required institutional support and proved quite challenging at some sites. Notably, since the publication of the study, major EHR vendors including EPiC have integrated I-PASS-based handoff modules. Two institutions did not have EHRs with integrated handoff modules and thus used an I-PASS template in MS-Word.
Though we felt that a handoff involving all members of the resident team was ideal (versus handoffs in parallel), we were not prescriptive in this area because we recognized that varying work flows might make this ideal very challenging.
We celebrated short-term wins using I-PASS “shout-outs” in program newsletters or via e-mail to recognize residents who had performed an excellent I-PASS handoff, prizes for teams with high I-PASS performance, and at 1 site, an I-PASS birthday party to celebrate 1 year of implementation.
IMPLEMENTING AND SUSTAINING CHANGE
After implementation at the study sites, both the study group as a whole and individuals at their respective institutions worked to consolidate improvement and institutionalize the I-PASS approach. Site leaders and champions spread I-PASS throughout their institution by highlighting successes within pilot units and helping implement the program in other specialties such as obstetrics and gynecology and internal medicine. Pilot changes to the EHR were pushed system-wide. One site incorporated the framework into the nurse to nurse handoff and another incorporated it into transitions of care between units within the hospital.21,22 All these efforts took place as I-PASS training and faculty observation/feedback became the standard for pediatric residents at the study sites, well beyond the study timeline.
Locally, sustainability requires annual training of new residents (and therefore time during orientation), and ongoing direct observations of handoffs with feedback, all of which require significant efforts on behalf of local champion—a potential barrier if these efforts are not recognized and supported. If observations are documented on paper or electronic forms, administrative staff must be provided with time to process these data.
Sustainment need not mean 100% compliance with all elements of the handoff—in the multi-site residents used key elements of the verbal handoff only about 60% of the time and still observed significant decreases in medical errors and adverse events. From follow-up studies, we have learned that pediatrics residents from study sites are most likely to use I-PASS when signing out new patients, complex patients, or when directly observed by faculty,23 further highlighting value of faculty engagement. This faculty engagement via observations and feedback is essential to reinforce the importance of standardized handoffs.
In addition to site-specific efforts, the study group presented the I-PASS curriculum at national meetings. Workshop participants and platform attendees were given I-PASS campaign materials including lanyards, badge-clips, pocket cards, and business cards referencing the study website, all designed to support broader dissemination.
DISCUSSION
The I-PASS Campaign used principles of transformational change adapted from the business literature to create a multifaceted campaign to implement a structured handoff program. A structured process including a robust campaign provided a key framework for both local implementation and national and international dissemination.5–7
Many campaigns focus on behavior change and/or improving processes with the vision of improving outcomes. I-PASS is supported by a strong evidence-base, and integrating this evidence into the campaign has elevated the campaign to a higher level. Successful implementation of the I-PASS handoff program was associated with a 23% reduction in medical errors and a 30% reduction in preventable adverse events (harms) to patients.10 Time motion studies demonstrated that residents spent no additional time performing an I-PASS handoff when compared with their baseline handoff techniques.10 Embedded process metrics showing improved verbal and written handoffs provided evidence that behavior change had in fact occurred. These data support a true comparative advantage of I-PASS over traditional handoff practices and helped elevate the campaign by providing meaningful evidence of improvements in patient outcomes.
Our implementation and subsequent data collection have some important limitations that should be considered. Implementation efforts varied among sites based in part on readiness to change. Needs assessments identified variation, such as baseline engagement by faculty in the handoff process. We did not quantify the efforts at each site (eg, number of meetings with faculty), though all sites met the minimum standard of at least 1 Grand Rounds and at least 1 faculty meeting presentation. Direct observations of handoffs with subsequent feedback were recommended to be at least twice monthly, though there was variation between sites and likely some sites did not adhere to this suggested standard. Also, we did not track the total number of faculty who may have been involved in supervising residents, nor their total weeks of service, so it is possible that observations were performed by a limited subset of faculty. Nonetheless, our process data, based on a sample of 207 observations on a subset of the 875 residents who participated in the study, demonstrated significant uptake.
Disseminating this evidence of success has been extremely important in the change process and has facilitated acceptance by potential skeptics. Highlighting the comparative advantage through robust improvements in patient safety metrics with minimal workflow changes have become a central component of ongoing marketing as I-PASS leaders continue to communicate the vision at new institutions. Concurrently, ACGME Clinical Learning Environment Review (CLER) requirements for improving Transitions of Care24 have created external pressures and a renewed sense of urgency for academic medical centers to standardize processes for transitions of care. I-PASS provides a robust solution to this need.
Perhaps most significantly, as leading academic institutions have adopted I-PASS, we have created a social pressure for peer institutions to follow suit. The selection of I-PASS as a finalist in the Harvard Business School/Harvard Medical School Health Acceleration Challenge,25 and as the winner of the Pediatric Hospital Medicine Quality and Safety Award and the 2016 John M. Eisenberg Award for Patient Safety and Quality sponsored by the National Quality Forum and the Joint Commission provided additional credibility, which has continued to support the social marketing and diffusion of I-PASS. I-PASS curriculum materials have been downloaded over 3000 times by individuals in all 50 states and over 40 countries, and over 80% are from medical fields outside pediatrics. In 2014, the I-PASS team received additional funding to study mentored implementation of the I-PASS bundle at 32 additional institutions (a public call for study sites received applications from 87 institutions, reflecting the growing momentum of I-PASS.) The evidence, peer pressure, and academic recognition continue to enable the work to spread within institutions, nationally, and internationally.
CONCLUSIONS
The I-PASS Campaign is an example of using a transformational change model in academic medical centers to improve patient safety. A structured process including a robust campaign to support diffusion of this important innovation was a key component of our successful local implementation and national and international dissemination. We encourage others in academic medicine to consider the use of campaigns to support improvement programs in health care institutions.
ACKNOWLEDGEMENTS
The authors acknowledge the efforts of the residents, Chief Residents, and faculty champions at all of our sites. Christian Ledford, PhD, and Patricia O’Sullivan, EdD, provided valuable guidance in the framing of this article. The I-PASS Campaign Subcommittee operated within the I-PASS Education Executive Committee, which included the following additional members: I-PASS Study Education Executive Committee: Boston Children’s Hospital/Harvard Medical School (primary site): Christopher P. Landrigan, MD, MPH, Theodore C. Sectish, MD, Amy J. Starmer, MD, MPH; Boston Children’s Hospital: Elizabeth L. Noble, Lisa L. Tse; Cincinnati Children’s Hospital Medical Center/University of Cincinnati College of Medicine: Jennifer K. O’Toole, MD, MEd; Hospital for Sick Children/University of Toronto: Zia Bismilla, MD, FRCPC, Maitreya Coffey, MD, FRCPC; Lucile Packard Children’s Hospital/Stanford University School of Medicine: Lauren A. Destino, MD, Jennifer L. Everhart, MD, Shilpa J. Patel, MD (currently at Kapi’olani Children’s Medical Center for Women and Children/University of Hawai’i at Mānoa John A. Burns School of Medicine); OHSU Doernbecher Children’s Hospital/Oregon Health and Science University: Amy J. Starmer, MD, MPH (currently at Boston Children’s Hospital/Harvard Medical School); Primary Children’s Hospital/Intermountain Healthcare/University of Utah School of Medicine: James F. Bale, Jr., MD, Rajendu Srivastava, MD, MPH, FRCPC, Adam T. Stevenson, MD; St. Louis Children’s Hospital/Washington University School of Medicine in St. Louis: F. Sessions Cole, MD; St. Christopher’s Hospital for Children/Drexel University College of Medicine: Sharon Calaman, MD, Nancy D. Spector, MD; UCSF Benioff Children’s Hospital/University of California, San Francisco, School of Medicine: Glenn Rosenbluth, MD, Daniel C. West, MD; Walter Reed National Military Medical Center/Uniformed Services University of the Health Sciences: Jennifer H. Hepps, MD, Joseph O. Lopreiato, MD, MPH, Clifton E. Yu, MD.
DISCLOSURE
Drs. Landrigan, Sectish, Spector, and Starmer co-founded and hold equity interest in the I-PASS Institute, a company which aims to assist institutions in the implementation of the I-PASS Handoff Program. Dr. Landrigan is supported by the Children’s Hospital Association for his work as Executive Council member of the PRIS Network. Dr. Rosenbluth has received consulting fees from the I-PASS Institute. Dr. Destino declares no conflicting interests.
Footnotes
Published online July 20, 2018.
The I-PASS Study Group has presented brief descriptions of the I-PASS campaign in national and international academic presentations. However, this comprehensive overview of the campaign has not previously been presented or published.
Supported by U.S. Department of Health and Human Services, Office of the A Assistant Secretary for Planning and Evaluation (1R18AE000029-01), the Agency for Healthcare Research and Quality/Oregon Comparative Effectiveness Research K12 Program (1K12HS019456-01, to Dr. Starmer), the Medical Research Foundation of Oregon, and the Physician Services Incorporated Foundation (of Ontario, Canada) and by an unrestricted medical education grant from Pfizer.
Members of I-PASS Campaign Committee: April D. Allen, MPA, Sharon Calaman, MD, Lauren A. Destino, MD, Jennifer L. Everhart, MD, Jennifer H. Hepps, MD, Christopher P. Landrigan, MD, MPH, Jennifer K. O’Toole, MD, MEd, Shilpa J. Patel, MD, Glenn Rosenbluth, MD, Theodore C. Sectish, MD, Nancy D. Spector, MD, Amy J. Starmer, MD, MPH, Adam T. Stevenson, MD, Clifton E. Yu, MD
To cite: Rosenbluth G, Destino LA, Starmer AJ, Landrigan CJ, Spector ND, Sectish TC. I-PASS Handoff Program: Use of a Campaign to Effect Transformational Change. Pediatr Qual Saf 2018;3:088.
REFERENCES
- 1.Reinertsen JLGA, Rupp W, Whittington JW.Engaging Physicians in a Shared Quality Agenda 2007. 2007. Cambridge, Mass.: IHI Innovation Series white paper. [Google Scholar]
- 2.Rogers E.Diffusion of Innovations. 20035th ed New York: Simon and Schuster; [Google Scholar]
- 3.Westfall JM, Mold J, Fagnan L.Practice-based research—“Blue Highways” on the NIH roadmap. JAMA. 2007;297:403–406.. [DOI] [PubMed] [Google Scholar]
- 4.Kotter JP.Leading change: why transformation efforts fail. Harvard Business Review. 1995 (March-April):59–67.. [Google Scholar]
- 5.ABIM Foundation. Choosing wisely. 2016. Available at http://www.choosingwisely.org/. Accessed August 13, 2016.
- 6.Society of Critical Care Medicine. Surviving sepsis campaign. Available at http://www.survivingsepsis.org. Accessed August 13, 2016.
- 7.Berwick DM, Calkins DR, McCannon CJ, et al. The 100,000 lives campaign: setting a goal and a deadline for improving health care quality. JAMA. 2006;295:324–327.. [DOI] [PubMed] [Google Scholar]
- 8.Starmer AJ, O’Toole JK, Rosenbluth G, et al. I-PASS Study Education Executive Committee. Development, implementation, and dissemination of the I-PASS handoff curriculum: a multisite educational intervention to improve patient handoffs. Acad Med. 2014;89:876–884.. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services AfHRaQ. TeamSTEPPS home. Available at http://teamstepps.ahrq.gov/. Accessed June 8, 2015. [DOI] [PubMed]
- 10.Starmer AJ, Spector ND, Srivastava R, et al. I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371:1803–1812.. [DOI] [PubMed] [Google Scholar]
- 11.Starmer AJ, Spector ND, Landrigan CP, et al. Resident Sign-out Practices: Results from a Multisite Needs Assessment. Association of Pediatric Program Directors Annual Meeting; April 21, 2011; Miami, FL. [Google Scholar]
- 12.Kohn L, Corrigan J, Donaldson M.To Err Is Human: Building a Safer Health System. 1999Washington, D.C.: National Academy Press; [PubMed] [Google Scholar]
- 13.The Joint Commission. Sentinel event data—root causes by event type. 2015. Available at http://www.jointcommission.org/assets/1/18/Root_Causes_by_Event_Type_2004-2Q_2014.pdf. Accessed April 13, 2015.
- 14.Landrigan CP, Parry GJ, Bones CB, et al. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363:2124–2134.. [DOI] [PubMed] [Google Scholar]
- 15.Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310:2262–2270.. [DOI] [PubMed] [Google Scholar]
- 16.Accreditation Council for Graduate Medical Education. Common program requirements. 2011. Available at http://acgme.org/acgmeweb/tabid/429/ProgramandInstitutionalAccreditation/CommonProgramRequirements.aspx. Accessed May 11, 2015.
- 17.Hafferty FW.Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med. 1998;73:403–407.. [DOI] [PubMed] [Google Scholar]
- 18.Rosenbluth G, Tabas JA, Baron RB.What’s in it for me? Maintenance of certification as an incentive for faculty supervision of resident quality improvement projects. Acad Med. 2016;91:56–59.. [DOI] [PubMed] [Google Scholar]
- 19.Carraccio C, Englander R.Innovation in pediatric education: the path to transforming pediatric graduate medical education. Pediatrics. 2010;125:617–618.. [DOI] [PubMed] [Google Scholar]
- 20.Rosenbluth G, Patel SJ, Everhart JL, et al. I-PASS handoff curriculum: campaign toolkit. MedEdPORTAL Publications. 2013;9397 Available at http://doi.org/10.15766/mep_2374-8265.9397. Accessed July 12, 2018. [Google Scholar]
- 21.Caruso TJ, Marquez JL, Wu DS, et al. Implementation of a standardized postanesthesia care handoff increases information transfer without increasing handoff duration. Jt Comm J Qual Patient Saf. 2015;41:35–42.. [DOI] [PubMed] [Google Scholar]
- 22.Sheth S, McCarthy E, Kipps AK, et al. Changes in efficiency and safety culture after integration of an I-PASS-supported handoff process. Pediatrics. 2016;137:e20150166. [DOI] [PubMed] [Google Scholar]
- 23.Coffey M, Thomson K, Li SA, et al. Resident experiences with implementation of the I-PASS handoff bundle. J Grad Med Educ. 2017;9:313–320.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.CLER Pathways to Excellence. 2014. Available at http://www.acgme.org/acgmeweb/Portals/0/PDFs/CLER/CLER_Brochure.pdf. Accessed April 23, 2014.
- 25.Harvard Business School, Harvard Medical School. Health acceleration challenge—2015 finalists. 2016. Available at http://forumonhealthcareinnovation.org/2014-15-finalists. Accessed August 24, 2016.


