Overview
Introduction
Primary triple arthrodesis is a powerful and reliable procedure for stabilizing and correcting painful rigid flatfoot deformities with a low rate of complications.
Indications & Contraindications
Step 1: Preoperative Planning
Pay careful attention to the history, physical examination, and weight-bearing radiographic studies as they are critical for selecting patients who will benefit from a triple arthrodesis.
Step 2: Room Setup and Patient Positioning
Position the patient supine on the operating table with the toes pointing straight up to the ceiling.
Step 3: Incisions and Exposure
For a standard triple arthrodesis, use 2 incisions: a lateral sinus tarsi incision, which allows exposure of the subtalar joint, CC joint, and lateral aspect of the TN joint, and a medial incision, which provides exposure of the TN joint.
Step 4: Joint Preparation
Ensure that joint preparation is thorough as this is critical for the success of any hindfoot arthrodesis.
Step 5: Reduction of Deformity
Reduce the TN joint first, followed by the subtalar joint, restoring a plantigrade foot and approximately 5° of hindfoot valgus alignment.
Step 6: Joint Fixation
Perform rigid fixation of the subtalar joint first, followed by fixation of the TN and CC joints.
Step 7: Accessory Procedures
Accessory procedures are often required in addition to the triple arthrodesis to ensure that appropriate hindfoot alignment and a plantigrade foot are achieved.
Step 8: Wound Closure
Perform a staged wound closure, taking care to maximize soft-tissue coverage over the involved hindfoot joints.
Step 9: Postoperative Care
Ensure that the patient follows strict non-weight-bearing precautions in the immediate postoperative period to limit micromotion at the arthrodesis sites and allow for timely fusion.
Results
In one of the largest published series of patients managed with triple arthrodesis (111 patients), Pell et al. reported a union rate of 98% at a minimum follow-up of 2 years, with 91% of patients indicating that they would be willing to repeat the procedure under similar circumstances4.
Pitfalls & Challenges
Introduction
Primary triple arthrodesis is a powerful and reliable procedure for stabilizing and correcting painful rigid flatfoot deformities with a low rate of complications.
The first reports of triple arthrodesis date back to the turn of the 20th century1,2, and the modern technique has seen few modifications since the procedure was popularized by Ryerson in 19233. Surgical techniques have been refined over the past decades, with a corresponding improvement in arthrodesis rates and patient satisfaction. The ability to achieve a stable and corrected hindfoot alignment is closely associated with patient outcomes4, and therefore careful patient selection and preoperative evaluation are critical to achieve a successful result. The most common indications for the procedure include hindfoot deformity and degenerative disease associated with chronic posterior tibial tendon dysfunction or posttraumatic or paralytic equinovarus deformity, although the procedure can be used to address more uncommon situations. Pain with bearing weight is the most common symptom in patients with hindfoot arthritis, with sharp pain at the initiation of weight-bearing activity and dull aching pain at the conclusion of activities. Patients may express difficulty when walking over uneven ground because of the increased stress placed across the hindfoot joints with inversion and eversion motion and pain from subfibular impingement laterally. Inspection of soft tissues and careful incision planning are crucial in patients with a history of surgery, trauma, or infection and if a large deformity is to be corrected. Passive inversion and eversion of the subtalar and transverse tarsal joints often demonstrate limited range of motion and may reproduce pain in advanced degenerative conditions. Any residual forefoot deformity noted after correction of the hindfoot must be addressed at the time of surgery to restore a plantigrade foot. Long-standing hindfoot deformity is often associated with a gastrocnemius or Achilles contracture, which can be identified with the Silfverskiöld test. A standing examination is critical to assess the severity of the deformity. Valgus deformity is common in chronic posterior tibial tendon dysfunction, rheumatoid disease, tarsal coalition, and other neuromuscular conditions. Any deformity should be assessed as flexible or rigid, as flexible deformity may be amenable to reconstructive surgical procedures as opposed to arthrodesis. Weight-bearing anteroposterior, lateral, and oblique radiographs of the foot and anteroposterior and mortise views of the ankle are performed in routine evaluation of hindfoot deformity. Standing hindfoot alignment radiographs are often made to identify valgus deformity and assess the degree of symmetry present between the symptomatic and asymptomatic limbs. Advanced imaging techniques such as computed tomography (CT) are frequently unnecessary for diagnostic purposes but may assist in preoperative planning for patients with severe deformity and in accurate assessment of fusion postoperatively.
Multiple approaches to complete a triple arthrodesis have been described. Fixation of the subtalar joint is done with 6.5 or 7.0-mm-diameter screws; cannulated screws are acceptable and facilitate accurate placement, whereas solid-core screws have increased strength. Screws ranging in diameter from 4.0 to 5.5 mm are utilized for the talonavicular (TN) and calcaneocuboid (CC) joints. Headless screws provide a low-profile option and may be less irritating for the patient. Alternatively, nitinol staples and small plates applied in compression may assist in achieving adequate fixation, particularly for the TN and CC joints5,6. Two incisions are utilized to adequately visualize the hindfoot joints. Laterally, an incision is made, starting 2 cm proximal to the tip of the lateral malleolus and extending distally to the base of the fourth metatarsal. The origin of the extensor digitorum brevis (EDB) is identified at the sinus tarsi and is reflected distally. Enhanced exposure of the middle and posterior facets of the subtalar joint may be achieved by placing a lamina spreader between the neck of the talus and the anterior process of the calcaneus. The CC joint is exposed after reflection of the EDB and incision of the joint capsule. Medially, a longitudinal incision is created, starting just distal to the medial malleolus and extending 1 cm beyond the naviculocuneiform joint. Careful subcutaneous dissection is carried down to the TN joint capsule, and the TN joint is exposed and distracted, utilizing a lamina spreader or Hintermann distractor, taking care to avoid crushing the soft bone of the talar head. All remaining cartilage at the various joint surfaces is removed, and the subchondral bone is fenestrated to increase the total surface area of bleeding cancellous bone and enhance fusion. If utilized, bone graft is impacted into the involved joints at this stage. The transverse tarsal joint is manipulated and should achieve approximately 0° to 5° of abduction with the foot demonstrating a plantigrade position. Guidewires are then secured across the TN joint. The calcaneus is rotated to reduce the hindfoot to 5° of valgus. Care should be taken to avoid overcorrecting the hindfoot in varus. Guidewires are then secured across the subtalar joint, originating proximal to the weight-bearing posterior surface of the calcaneus. Through percutaneous incisions made over each guidewire, 6.5-mm cannulated screws are secured across the subtalar joint. Once the subtalar joint is secured, two 5.5-mm cannulated screws or a combination of cannulated screws and a compression plate are secured across the TN joint. The CC joint is evaluated and should not be inferiorly subluxated. Guidewires are secured across the CC joint, while the joint is manually reduced in anatomic alignment and is secured with a combination of 4.0-mm cannulated screws, compression plate and screws, and/or staples. The EDB is repaired over the sinus tarsi, and the TN joint capsule is reapproximated if possible. Subcutaneous tissues and skin are reapproximated with monofilament sutures of the surgeon’s preference. Sterile dressings are applied, and the limb is immobilized in a short leg splint with the ankle held in neutral dorsiflexion. Patients remain non-weight-bearing for a total of 6 weeks, with the postoperative splint worn for the first 2 weeks and a short leg cast or tall walker boot worn for the following 4 weeks. Protected weight-bearing is advanced at 6 weeks in a boot with transition to full weight-bearing in a comfortable shoe by 3 months postoperatively if there is radiographic evidence of fusion.
Indications & Contraindications
Indications
Chronic hindfoot pain with associated primary degenerative disease involving multiple hindfoot joints.
Posttraumatic hindfoot deformity and/or arthritis with involvement of multiple joints (as seen with talar neck fracture-dislocations).
Inflammatory arthropathy involving the hindfoot.
Rigid hindfoot planovalgus deformity.
Flexible hindfoot planovalgus deformity in patients of advanced age.
Symptomatic unresectable or previously resected calcaneonavicular coalition.
Contraindications
Active infection.
Medical comorbidities with an unacceptably high risk of wound-healing complications, infection, or nonunion (uncontrolled diabetes, severe immunocompromise, malnutrition, etc.).
Severe peripheral vascular disease.
Inability of the patient to comply with non-weight-bearing precautions.
Isolated subtalar or TN degenerative joint disease (may be a better candidate for isolated subtalar or TN arthrodesis).
Active nicotine use (a relative contraindication).
Step 1: Preoperative Planning
Pay careful attention to the history, physical examination, and weight-bearing radiographic studies as they are critical for selecting patients who will benefit from a triple arthrodesis.
Perform a thorough clinical examination as it may reveal pain over the involved joints. Palpation over the sinus tarsi and subfibular recess will elicit pain from a degenerative subtalar joint and subfibular impingement, and tenderness over the TN and CC articulations indicates involvement of these joints.
Evaluate for limited ankle range of motion or pain localized to the ankle joint as ankle arthritis or deformity will not be addressed with a triple arthrodesis in isolation.
Be sure to identify any fixed forefoot supination deformity after passive correction of the hindfoot.
Perform a Silfverskiöld test to assess for an Achilles or gastrocnemius contracture, which is often present after a long-standing hindfoot deformity. Address a contracture at the time of surgery with either a gastrocnemius recession or an Achilles lengthening.
Perform a standing evaluation as it is critical for assessing the degree of deformity and any associated lower extremity malalignment (Fig. 1).
Assess all deformity as flexible or rigid, as a flexible deformity may be better addressed with a reconstruction procedure as opposed to arthrodesis.
Perform a sensory examination as it may reveal evidence of peripheral neuropathy, which places patients at increased risk of delayed wound-healing, infection, or other operative complications.
Be sure to identify any impaired arterial inflow to the foot, as it substantially increases wound complication and nonunion rates; if necessary, obtain appropriate vascular imaging studies and/or refer the patient to a vascular surgeon.
Obtain weight-bearing anteroposterior, lateral, and oblique radiographs of the foot and anteroposterior and mortise views of the ankle for the routine evaluation of hindfoot deformity.
Evaluate the anteroposterior radiograph of the foot to identify degenerative conditions of the TN joint and provide a rapid assessment for abduction or adduction of the forefoot.
Use the oblique and lateral foot radiographs to identify degenerative changes at the TN and CC joints.
Evaluate the lateral talar-first metatarsal angle to assess the arch height, with a planovalgus foot demonstrating a negative angle (apex plantar).
Note that as the posterior and middle facets of the subtalar joint are aligned in parallel at 45° to the sole of the foot, the lateral radiograph may not identify subtle or early degenerative changes at these facets.
Use the ankle radiographs to identify concomitant tibiotalar joint deformity or arthritis, which require further intervention beyond correction of the hindfoot deformity.
Obtain standing hindfoot alignment radiographs to quantify valgus deformity and assess the degree of symmetry between the symptomatic and asymptomatic limbs (Fig. 1).
Advanced imaging techniques such as CT are frequently unnecessary for diagnostic purposes but may assist in preoperative planning in severe deformity and accurate assessment of fusion postoperatively. Magnetic resonance imaging (MRI) may identify concomitant intra-articular ankle joint pathology or evidence of deltoid injury but is not routinely performed preoperatively unless additional pathology outside the hindfoot area of interest is suspected.
Fig. 1.

Preoperative evaluation includes careful inspection of hindfoot alignment with the patient standing. A hindfoot alignment radiograph can assist in assessing deformity, especially in the setting of bilateral deformity or prior surgery.
Step 2: Room Setup and Patient Positioning
Position the patient supine on the operating table with the toes pointing straight up to the ceiling.
Use general anesthesia, typically with preoperative popliteal and/or sciatic and saphenous nerve blocks.
Position the patient supine on the operating table with the foot near, but not extending beyond, the end of the table.
Place a bump under the ipsilateral hip to internally rotate the involved limb to direct the toes straight up toward the ceiling (Fig. 2).
Administer preoperative antibiotics within 1 hour before the surgical incision.
To provide adequate visualization, use a mini C-arm, which should be positioned on the same side of the table as the involved limb. A large C-arm may also be utilized and is helpful if operating without an assistant.
Prepare and drape the involved limb in standard fashion. An occlusive dressing is placed over the toes to limit bacterial contamination (Fig. 3).
Inflate a thigh tourniquet to between 250 and 300 mm Hg after Esmarch exsanguination of the limb.
Fig. 2.
A beanbag or bolster is utilized under the ipsilateral hip to rotate the limb and position the toes so that they are pointing to the ceiling.
Fig. 3.

A sponge and occlusive dressing (e.g., Ioban surgical drape [3M Medical]) are placed over the toes to limit infection risk.
Step 3: Incisions and Exposure
For a standard triple arthrodesis, use 2 incisions: a lateral sinus tarsi incision, which allows exposure of the subtalar joint, CC joint, and lateral aspect of the TN joint, and a medial incision, which provides exposure of the TN joint.
Laterally, make an incision starting at the distal tip of the fibula and extending distally toward the base of the fourth metatarsal (Fig. 4 and Video 1).
Protect the crossing branches of the sural nerve to the intermediate branch of the superficial peroneal nerve throughout the case.
Identify the origin of the EDB at the sinus tarsi and reflect it distally (Fig. 5).
The peroneal tendon sheath runs near the plantar aspect of the incision. Use a Cobb elevator to elevate the peroneal sheath and surrounding soft tissues away from the lateral aspect of the posterior facet of the subtalar joint near the tip of the distal end of the fibula. A bent Hohmann retractor may be placed around the posterolateral aspect of the subtalar joint to protect soft tissues during the joint preparation (Fig. 6).
Excise the interosseous ligaments of the sinus tarsi to allow visualization of the subtalar joint.
Incise the joint capsule along the lateral aspect of the posterior facet of the subtalar joint.
To improve exposure of the posterior and middle facets, place a lamina spreader into the sinus tarsi, between the plantar neck of the talus and the anterior body of the calcaneus.
Expose the CC joint after reflection of the EDB distally.
Sweep a knife vertically through the CC joint and rotate it dorsally through the bifurcate ligament (Fig. 7 and Video 2).
Improve visualization with plantar flexion and supination of the midfoot and placement of a lamina spreader within the joint.
Medially, make a longitudinal incision centered over the TN joint, starting just distal to the medial malleolus and extending 1 cm distal to the naviculocuneiform joint (Fig. 8 and Video 3).
Use an interval between the anterior tibial and posterior tibial tendons, taking care to protect the saphenous vein and nerve.
Carry out subperiosteal dissection over the TN joint with a Cobb elevator.
Incise the TN joint capsule, and further expose the joint with a small lamina spreader placed into the joint (Fig. 9).
Visualize the lateral aspect of the TN joint through the lateral incision.
Fig. 4.
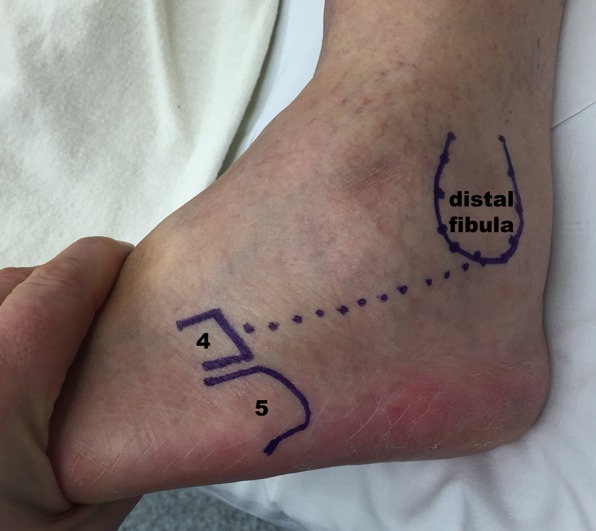
The lateral exposure is performed through an incision extending from the tip of the distal end of the fibula toward the base of the fourth metatarsal.
Fig. 5.

After reflection of the EDB muscle, the sinus tarsi and posterior facet of the subtalar joint are exposed. The interosseous ligament is identified within the sinus tarsi and incised to allow adequate distraction and exposure of the subtalar joint.
Fig. 6.

A Hohmann retractor is placed around the posterolateral subtalar joint to protect the peroneal tendons. A lamina spreader is placed within the sinus tarsi to allow exposure of the entire posterior facet of the subtalar joint.
Fig. 7.

As dissection is carried out distally, the bifurcate ligament and CC joint capsule are incised to expose the CC joint.
Fig. 8.

The medial exposure is performed through an incision starting just distal to the tip of the medial malleolus (med. mall.) and extending over the TN joint beyond the navicular tuberosity (navic.). ATT = anterior tibial tendon, and PTT = posterior tibial tendon.
Fig. 9.
The TN joint is exposed through an interval between the anterior tibial and posterior tibial tendons (top images). After the TN joint capsule is incised, thorough debridement of the remaining chondral tissue is completed (bottom images).
Video 1.
The lateral approach and subtalar joint exposure.
Video 2.
Exposure of the CC joint.
Video 3.
The medial approach and TN joint exposure.
Step 4: Joint Preparation
Ensure that joint preparation is thorough as this is critical for the success of any hindfoot arthrodesis.
Starting with the subtalar joint, and progressing to the CC and TN joints, remove all remaining chondral tissue from the joint surfaces with a combination of osteotome, curet, or rongeur (Fig. 10 and Videos 4 and 5).
Copiously irrigate the wounds to flush out all remaining chondral debris.
The goal of joint preparation is to create bleeding cancellous bone surfaces and increase the surface area of bone across the joints to enhance healing.
Use a 6-mm curved osteotome to “fish-scale” both sides of each joint, penetrating through the subchondral plates.
Use a 2.0-mm drill-bit to perforate the subchondral bone if it is sclerotic and difficult to penetrate with the osteotome.
Be careful not to break the tip of the drill-bit during joint preparation. A tissue protector and/or drill guide is helpful to access deep portions of each joint while limiting the risk of breaking the drill-tip.
The use of bone graft is not universally indicated as high fusion rates have been demonstrated both with and without supplemental autograft or allograft.
Address large defects or bone loss with allograft chips or cancellous graft harvested from the anterior aspect of the calcaneus, distal tibial metadiaphysis, proximal tibial metadiaphysis, or iliac crest. Donor site morbidity must be considered prior to harvesting autograft.
The use of bone graft in patients with a higher risk of nonunion (diabetes mellitus, active or recent nicotine use, etc.) is left to the discretion of the surgeon (Fig. 11).
Fig. 10.

A curet and/or osteotome may be utilized to thoroughly debride the chondral tissues on both sides of the entire subtalar joint.
Fig. 11.

Bone graft is utilized at the discretion of the individual surgeon, but may be helpful in patients at risk for poor or delayed bone-healing.
Video 4.
Subtalar and CC joint preparation.
Video 5.
TN joint preparation.
Step 5: Reduction of Deformity
Reduce the TN joint first, followed by the subtalar joint, restoring a plantigrade foot and approximately 5° of hindfoot valgus alignment.
It is rare that a bone wedge needs to be resected from the subtalar or CC joints to achieve corrected hindfoot alignment.
In a long-standing planovalgus deformity, the talar head may collapse and a small wedge may need to be removed from the TN joint medially to allow correction of midfoot abduction.
Reduce the TN joint first as it is typically the apex of deformity in a severe flatfoot deformity (Video 6).
In a flatfoot deformity, pronate, adduct, and plantar flex the forefoot around the talar head while pressure is applied posteromedially along the talar neck.
The transverse tarsal joint should demonstrate approximately 0° to 5° of abduction with the foot resting in a plantigrade position after reduction of the TN joint.
Place guidewires across the TN joint for provisional fixation.
Advance 1 guidewire through the incision, starting at the edge of the naviculocuneiform joint and advancing across the TN joint into the body of the talus.
If utilized, advance a second guidewire in percutaneous fashion starting at the distal and dorsolateral aspect of the navicular and advancing into the medial talar body.
Obtain anteroposterior and lateral foot and anteroposterior ankle fluoroscopic views to confirm reduction of the TN joint and positioning of the guidewires.
As attention is next turned to the subtalar joint, rotate the calcaneus to reduce the hindfoot into 5° of valgus.
Opening a lamina spreader within the sinus tarsi may assist with reducing the subtalar joint, but take care to avoid overcorrecting the hindfoot in varus.
Accomplish temporary fixation of the subtalar joint with a guidewire advanced through a percutaneous incision just proximal to the posterior weight-bearing surface of the calcaneus.
Advance the guidewire across the posterior facet into the body of the talus, and direct it from slightly lateral to medial.
Take care not to advance the tip of the guidewire beyond the subchondral bone of the talar dome to avoid damage to the talar cartilage.
Obtain lateral foot, axial hindfoot, and anteroposterior ankle fluoroscopic views to confirm reduction of the subtalar joint and positioning of the guidewires.
Reduce the CC joint, which is performed typically after fixation of the subtalar and TN joints.
The cuboid has a tendency to subluxate plantarward once the hindfoot deformity is corrected. Apply manual pressure under the plantar aspect of the cuboid to dorsally translate the cuboid and reduce the CC joint (Figs. 12-A and 12-B).
Pack any remaining gaps noted along the visualized joints with bone graft to maximize the joint surface available for fusion.
Figs. 12-A and 12-B The order of fixation of the subtalar and TN joints frequently dictates the reduction of the CC joint.
Fig. 12-A.

If the subtalar joint is stabilized first (left image), the cuboid frequently subluxates inferiorly, potentially leading to lateral overload and pain if not reduced prior to fixation. Reducing and stabilizing the TN joint first (right image) reliably maintains reduction of the CC joint.
Fig. 12-B.
If subluxation of the CC joint is noted after securing both the TN and subtalar joints (left image), dorsal pressure is placed under the cuboid while the joint is secured (central and right images).
Video 6.
Reduction of the hindfoot and fixation of the subtalar and TN joints.
Step 6: Joint Fixation
Perform rigid fixation of the subtalar joint first, followed by fixation of the TN and CC joints.
Secure the subtalar joint first, utilizing 2 screws to improve rotational stability and compression (Fig. 13). Due to the rigidity of the hindfoot after fixation of all 3 joints, many surgeons utilize only 1 screw for subtalar joint fixation, although this is not our preferred method.
Typically, 6.5 to 7.0-mm screws are utilized.
Use partially threaded screws or fully threaded screws in compression mode by overdrilling the calcaneus.
Advance the first screw over the guidewire placed for temporary stabilization.
A second diverging screw may be placed in a similar manner from the posterior aspect of the calcaneus into the talar body.
Alternatively, a second screw can be directed in a percutaneous manner from the dorsal talar neck into the calcaneal body. Advance the screw between the anterior tibial and extensor hallucis longus tendons.
While this approach allows more threads of the screw to engage across the joint, take care to countersink the head of the screw to limit anterior ankle impingement in terminal dorsiflexion.
Secure the TN joint with a 5.5-mm cannulated, partially threaded screw advanced over the guidewire running from the medial aspect of the navicular into the lateral talar body (Fig. 14).
Ensure that the head of the screw is advanced to sit flush with the naviculocuneiform joint to limit prominence and future hardware irritation.
A second 5.5-mm cannulated screw may be advanced over the dorsal guidewire to complete TN joint fixation.
Alternatively, use a dorsal 2-hole locking compression plate, depending on the quality of the bone and purchase achieved by the first screw. The proximal screw may be advanced across the subtalar joint into the anterior aspect of the calcaneus for added purchase.
Use a 5.5-mm screw for fixation across the CC joint. The screw may be advanced in antegrade or retrograde fashion (Video 7).
If the screw is placed from proximal to distal, create a small lateral notch behind the anterior process of the calcaneus 1 cm proximal to the CC joint to recess the screw head (Fig. 15).
If limited purchase of the screw or poor compression is achieved across the joint, apply a 2-hole or 4-hole compression plate across the joint for added stability and compression.
If a gap of >2 mm is evident at the CC joint after fixation of the subtalar and TN joints, a bone block arthrodesis is required. A small tricortical wedge of bone may be utilized to provide osseous contact and achieve arthrodesis. A compression plate is most useful to provide fixation in this circumstance.
Fig. 13.

A bump may be utilized to assist in placing the subtalar screws. A mini C-arm is versatile and easily manipulated in the operating room to guide screw placement, but a large C-arm may also be set in a stable position to allow for rapid placement of guidewires and screws. Care should be taken to avoid penetrating the chondral surface of the talar dome while advancing the guidewires and screws across the posterior facet of the subtalar joint.
Fig. 14.

The TN joint may be secured with a variety of methods. A partially threaded cannulated screw is typically advanced from the navicular tuberosity across the joint into the talar neck and body (left image). The dorsal aspect of the TN joint is additionally compressed with a second screw or small compression plate with screws (right image).
Fig. 15.

Prior to placing a screw from proximal to distal across the CC joint, a small notch is made in the anterior neck of the calcaneus to prevent fracture of the anterior process while securing the CC joint.
Video 7.
Fixation of the CC joint.
Step 7: Accessory Procedures
Accessory procedures are often required in addition to the triple arthrodesis to ensure that appropriate hindfoot alignment and a plantigrade foot are achieved.
Perform a Silfverskiöld test to assess for an Achilles or gastrocnemius contracture, which is often present after a long-standing hindfoot deformity.
If an isolated gastrocnemius contracture is evident, a gastrocnemius lengthening procedure is indicated and is typically performed at the beginning of the surgical procedure.
Address an Achilles contracture either with a percutaneous lengthening or with an open Z-lengthening of the Achilles tendon.
In the setting of chronic valgus hindfoot malalignment, the forefoot develops a compensatory supination deformity, which is accentuated after correction of the hindfoot. To maintain a plantigrade foot and limit the risk of recurrent hindfoot deformity, it is necessary to perform a first metatarsal dorsal opening-wedge osteotomy, plantar flexion arthrodesis of the first tarsometatarsal joint, or medial cuneiform dorsal opening-wedge (Cotton) osteotomy (Fig. 16).
Patients with severe midfoot abduction (uncoverage of >50% of the talar head) have a contracted peroneus brevis, which can limit the ability to correct the hindfoot malalignment or lead to recurrent deformity.
In this scenario, consider performing a tenodesis, or transfer, of the peroneus brevis to the peroneus longus, which reduces the abduction and eversion forces imparted by the brevis and can also assist the longus in plantar flexing the first ray and limit residual forefoot supination.
If necessary, address continued plantar subluxation of the first tarsometatarsal or naviculocuneiform joint with an extended medial column fusion. In general, arthrodesis of the first tarsometatarsal joint is adequate to stabilize the medial column and allows preservation of NC joint motion.
Alternatives to the traditional triple arthrodesis, including an “all-medial” triple arthrodesis7,8 or “double arthrodesis,”9-12 in which the CC joint is spared, have been described with successful results, but they remain beyond the scope of this technique article.
A medial displacement calcaneal osteotomy, in addition to a triple arthrodesis, will improve the mechanical balance at the level of the ankle in patients with a rigid planovalgus deformity with associated deltoid laxity or rupture.
If necessary, perform a medial displacement calcaneal osteotomy through a separate oblique incision directly over the posterolateral calcaneal tuberosity. Advance the screws across both the osteotomy and the subtalar joint for fixation.
With valgus alignment but limited arthritis at the ankle joint, a deltoid ligament reconstruction can be performed in addition to the above procedures. Eversion stress anteroposterior fluoroscopic views of the ankle may be performed after final correction of the hindfoot to determine the competency of the deltoid ligament.
If ankle arthritis is present, consider a tibiotalocalcaneal or pantalar arthrodesis. Alternatively, a total ankle arthroplasty can be performed in a staged manner once the hindfoot is appropriately balanced.
Fig. 16.
After correction of the hindfoot deformity, attention is turned to the midfoot and forefoot. In long-standing hindfoot valgus deformity, compensatory forefoot supination becomes evident when the hindfoot is corrected. This must be addressed with concomitant procedures; otherwise the foot will not be plantigrade and recurrent deformity of the ankle and hindfoot is inevitable. A plantar flexion medial cuneiform osteotomy was performed in this patient to correct the residual forefoot supination.
Step 8: Wound Closure
Perform a staged wound closure, taking care to maximize soft-tissue coverage over the involved hindfoot joints.
Complete a thorough irrigation of the hindfoot wounds.
Release the thigh tourniquet at this time and achieve hemostasis with Bovie electrocautery.
Reapproximate the EDB muscle and fascia over the sinus tarsi with 2-0 braided absorbable suture (Video 8).
Reapproximate the TN joint capsule with 2-0 braided absorbable suture.
Reapproximate subdermal tissues for all incisions with a 3-0 absorbable monofilament suture.
Reapproximate skin for all incisions with a 3-0 nonabsorbable monofilament suture.
Apply Xeroform (Kendall) and sterile dressings.
Place the limb in a well-padded short leg splint with a posterior slab and stirrups.
Video 8.
EDB and lateral wound closure.
Step 9: Postoperative Care
Ensure that the patient follows strict non-weight-bearing precautions in the immediate postoperative period to limit micromotion at the arthrodesis sites and allow for timely fusion.
Immobilize the leg in a short leg splint for 2 weeks postoperatively.
At 2 weeks following surgery, remove the sutures.
The patient may transition to a short leg cast or tall walker boot.
If the patient is managed with immobilization in a boot, encourage him or her to remove the boot 3 times a day for active ankle dorsiflexion and plantar flexion range-of-motion exercises to minimize disuse atrophy and stiffness.
Advise patients that they may also remove the boot for daily hygiene and application of ice around the foot and ankle, but should keep the boot on at all other times.
Ensure that the patient remains strictly non-weight-bearing for 6 weeks postoperatively.
If managed with a cast, the patient may transition to a tall walker boot at 6 weeks postoperatively.
After 6 weeks postoperatively, the patient may remove the boot at night and while at rest.
Advise the patient to begin advancing weight-bearing, at a rate of 25% of body weight per week.
At 12 weeks postoperatively, the patient should be bearing full weight in the boot and may transition into a supportive shoe if there is radiographic evidence of fusion. Activity is advanced as tolerated.
Accommodative orthotics may be required postoperatively on the basis of the patient’s alignment and comfort.
Obtain postoperative radiographs of the foot and ankle at 2 weeks, 6 weeks, and 3 months postoperatively, and subsequently as needed until adequate bone bridging is noted across the fusion sites.
Obtain a CT scan of the hindfoot with thin cuts, reconstruction views, and metal suppression after 3 months postoperatively if there is persistent pain with weight-bearing activity or concern for delayed bone bridging across the arthrodesis sites on radiographs.
Caution patients that it may take up to 1 year for maximum recovery of motor strength and balance in the operatively treated extremity.
For patients with neuropathy, diabetes mellitus, or other compromising medical comorbidity that may delay healing, restrict weight-bearing on the operatively treated foot for 12 weeks postoperatively.
Results
In one of the largest published series of patients managed with triple arthrodesis (111 patients), Pell et al. reported a union rate of 98% at a minimum follow-up of 2 years, with 91% of patients indicating that they would be willing to repeat the procedure under similar circumstances4. Bone graft was required in less than half of the feet. No difference in outcomes was reported on the basis of the preoperative diagnosis. Patient satisfaction was closely associated with the ability to correct the hindfoot deformity intraoperatively. Rosenfeld et al. corroborated these outcomes with a 4% nonunion rate and good to excellent results after triple arthrodesis in 75% of 100 feet13. Saltzman et al. reported outcomes for 67 feet in 57 patients at an average of 24 and 44 years following triple arthrodesis14. Union rates of 81% were reported. Thirty of the 57 patients did not report any pain at the final follow-up, and 15 did not demonstrate any residual deformity. Rates of good results and the ability to walk at least 1 mile declined between the 2 follow-up periods. All ankles in the study demonstrated progressive radiographic degenerative disease. Despite the decline in function and reported good results at the long-term follow-up, 95% of the patients were satisfied with the result of the procedure and 91% would recommend the procedure to others.
Hardware design and surgical techniques have advanced throughout the years, with corresponding improvements in fusion rates and patient satisfaction. Throughout the recent literature, patient satisfaction rates of >85% have been reported and most stated that they would undergo the procedure again if indicated4,5,13-18. Most patients can return to unrestricted work duties16.
Nonunion remains the most commonly reported complication following triple arthrodesis, with rates historically ranging from 10% to 23%14,15,17,19,20. With improved hardware fixation and attention to joint preparation, fusion rates in the recent literature have exceeded 95%4,5,13,16,18. Most nonunions are noted at the TN joint, although the rates of CC joint nonunion are as high as 20%9,13-21. Development of ankle arthritis remains a concern and has been reported to occur in a few as 40% and as many as 100% of patients with long enough follow-up15,21. Midfoot arthritis is also common and has been reported to occur in nearly 50% of patients4,5,14,15,21. Concern over adjacent joint degenerative disease has led to the popularity of limited arthrodesis techniques, which are beyond the scope of this paper. Other complications such as hardware irritation13,16,17, infection13-17, osteonecrosis15, malunion13,14,16,18, deep-vein thrombosis13,16, and iatrogenic nerve injury4,15 remain quite rare.
Pitfalls & Challenges
Careful debridement and preparation of the joint surfaces is critical to the success of the arthrodesis.
Minimal bone resection should be the goal, as shortening of the foot and malunion can occur when resecting bone wedges from the involved joints. Correction of deformity is achieved with translation and rotation at each joint, not bone resection.
Small locking compression plates may be used to supplement fixation in patients with soft bone or when screw purchase is tenuous.
Headless compression screws may be desirable to limit the prominence of screw heads along the posterior aspect of the calcaneus or at the naviculocuneiform joint.
The TN joint is typically reduced first, followed by the subtalar joint. If the subtalar joint is reduced and stabilized first, the TN joint has a tendency to “overcorrect.”
The exception to this rule occurs with severe fixed valgus deformity of the subtalar joint. In this situation, the subtalar joint is reduced first, followed by the TN joint, which must be adducted and plantar flexed.
The sural nerve is encountered near the posterior aspect of the sinus tarsi incision and often has an anterior branch that crosses the incision site; aggressive retraction should be avoided to protect the nerve and prevent neuroma formation.
Failure to recognize and reduce an inferiorly subluxated CC joint will lead to fixed rotation of the transverse tarsal joint and pain from overload underneath the cuboid.
The position of the first ray must be assessed after correction of the hindfoot, and a plantar flexion osteotomy or arthrodesis may be required to establish a plantigrade foot.
Correction of a flatfoot deformity in the obese patient is difficult because of the increased girth of the thighs leading to valgus thrust on the foot. The foot must be fused in a slightly greater degree of valgus to limit lateral overload and pain.
Footnotes
Published outcomes of this procedure can be found at: J Bone Joint Surg Am. 2000 Jan;82(1):47-57
Investigation performed at Twin Cities Orthopedics, Edina, Minnesota
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work.
References
- 1. Wülker N, Stukenborg C, Savory KM, Alfke D. Hindfoot motion after isolated and combined arthrodeses: measurements in anatomic specimens. Foot Ankle Int. 2000. November;21(11):921-7. [DOI] [PubMed] [Google Scholar]
- 2. Hoke M. An operation for stabilizing paralytic feet. Am J Orthop Surg. 1921;3:494-507. [Google Scholar]
- 3. Ryerson E. Arthrodesing operations on the feet. J Bone Joint Surg Am. 1923;5:453-71. [Google Scholar]
- 4. Pell RF, 4th, Myerson MS, Schon LC. Clinical outcome after primary triple arthrodesis. J Bone Joint Surg Am. 2000. January;82(1):47-57. [DOI] [PubMed] [Google Scholar]
- 5. Knupp M, Skoog A, Törnkvist H, Ponzer S. Triple arthrodesis in rheumatoid arthritis. Foot Ankle Int. 2008. March;29(3):293-7. [DOI] [PubMed] [Google Scholar]
- 6. Seybold JD, Zide JR, Myerson MS. Hindfoot fusions in the flatfoot deformity: when and what techniques to use in late stage II and stage III deformities. Tech Foot & Ankle. 2014;13(1):29-38. [Google Scholar]
- 7. Vora AM, Myerson MS, Jeng CL. The medial approach to triple arthrodesis: indications and technique for management of rigid valgus deformities in high-risk patients. Tech Foot Ankle Surg. 2005;4(4):258-62. [DOI] [PubMed] [Google Scholar]
- 8. Jeng CL, Vora AM, Myerson MS. The medial approach to triple arthrodesis. Indications and technique for management of rigid valgus deformities in high-risk patients. Foot Ankle Clin. 2005. September;10(3):515-21, vi-vii. [DOI] [PubMed] [Google Scholar]
- 9. Sammarco VJ, Magur EG, Sammarco GJ, Bagwe MR. Arthrodesis of the subtalar and talonavicular joints for correction of symptomatic hindfoot malalignment. Foot Ankle Int. 2006. September;27(9):661-6. [DOI] [PubMed] [Google Scholar]
- 10. Anand P, Nunley JA, DeOrio JK. Single-incision medial approach for double arthrodesis of hindfoot in posterior tibialis tendon dysfunction. Foot Ankle Int. 2013. March;34(3):338-44. [DOI] [PubMed] [Google Scholar]
- 11. Knupp M, Schuh R, Stufkens SA, Bolliger L, Hintermann B. Subtalar and talonavicular arthrodesis through a single medial approach for the correction of severe planovalgus deformity. J Bone Joint Surg Br. 2009. May;91(5):612-5. [DOI] [PubMed] [Google Scholar]
- 12. Brilhault J. Single medial approach to modified double arthrodesis in rigid flatfoot with lateral deficient skin. Foot Ankle Int. 2009. January;30(1):21-6. [DOI] [PubMed] [Google Scholar]
- 13. Rosenfeld PF, Budgen SA, Saxby TS. Triple arthrodesis: is bone grafting necessary? The results in 100 consecutive cases. J Bone Joint Surg Br. 2005. February;87(2):175-8. [DOI] [PubMed] [Google Scholar]
- 14. Saltzman CL, Fehrle MJ, Cooper RR, Spencer EC, Ponseti IV. Triple arthrodesis: twenty-five and forty-four-year average follow-up of the same patients. J Bone Joint Surg Am. 1999. October;81(10):1391-402. [PubMed] [Google Scholar]
- 15. Angus PD, Cowell HR. Triple arthrodesis. A critical long-term review. J Bone Joint Surg Br. 1986. March;68(2):260-5. [DOI] [PubMed] [Google Scholar]
- 16. Bednarz PA, Monroe MT, Manoli A., 2nd Triple arthrodesis in adults using rigid internal fixation: an assessment of outcome. Foot Ankle Int. 1999. June;20(6):356-63. [DOI] [PubMed] [Google Scholar]
- 17. Graves SC, Mann RA, Graves KO. Triple arthrodesis in older adults. Results after long-term follow-up. J Bone Joint Surg Am. 1993. March;75(3):355-62. [DOI] [PubMed] [Google Scholar]
- 18. Sangeorzan BJ, Smith D, Veith R, Hansen ST., Jr Triple arthrodesis using internal fixation in treatment of adult foot disorders. Clin Orthop Relat Res. 1993. September;294:299-307. [PubMed] [Google Scholar]
- 19. Friedenberg ZB. Arthrodesis of the tarsal bones; a study of failure of fusions. Arch Surg. 1948. July;57(1):162-70. [DOI] [PubMed] [Google Scholar]
- 20. Wilson FC, Jr, Fay GF, Lamotte P, Williams JC. Triple arthrodesis. A study of the factors affecting fusion after three hundred and one procedures. J Bone Joint Surg Am. 1965. March;47:340-8. [PubMed] [Google Scholar]
- 21. Bennett GL, Graham CE, Mauldin DM. Triple arthrodesis in adults. Foot Ankle. 1991. December;12(3):138-43. [DOI] [PubMed] [Google Scholar]






