Abstract
Context
Women with an unintended birth have an elevated risk of another unintended pregnancy, and multiple unintended pregnancies could exacerbate any negative consequences of such births. This association may stem from variation in postpartum contraception use.
Methods
This analysis uses data from the 2011–15 cycles of the National Survey of Family Growth (NSFG) to compare postpartum contraceptive use across types of birth intendedness (on time/too late, slightly mistimed, seriously mistimed, unwanted). Specifically, with an analytical sample of 2,769 births, the analysis uses life table estimates to demonstrate differences in timing of initial postpartum contraception use and multinomial logistic event history methods to model initial contraceptive uptake and efficacy (highly effective, effective, least effective, or no contraception) by birth intendedness.
Results
Compared to new mothers with on time/too late births, those with seriously mistimed and unwanted births are 1.9 times and 1.7 times as likely, respectively, to first adopt highly effective methods (sterilization, LARCs) than no method. Mothers with unwanted births are also 1.5 times as likely to first use least effective methods (condoms, withdrawal). Mothers with seriously mistimed births are half as likely to use either effective methods (the pill, injectables) or least effective methods than highly effective methods relative to their counterparts with on time/too late births.
Conclusion
The elevated risk of repeat unintended fertility does not seem to be due to mothers’ initial postpartum contraceptive behavior. It remains to be seen whether mothers with unintended births use contraception less consistently, discontinue use sooner, or switch methods more often.
Introduction
Although unintended fertility has declined in recent years, levels and rates remain high in the United States relative to other industrialized countries.1 Nearly half of all pregnancies, and a third of all births, are unintended.1,2 Further, women who have one unintended birth have an elevated risk of subsequent unintended fertility.3,4,5 The high levels, along with the possibility of multiple unintended births among individual women, are concerning given the associations between birth intendedness and maternal, child, and family well-being.6,7,8,9,10 For instance, unintended fertility is linked to maternal depression and parental stress, marital instability, and behavioral problems among children.11,12,13
The vast majority of unintended pregnancies are caused by non-use or inconsistent use of contraception, along with using less effective methods.14 Increasing the use of effective methods of contraception is key to preventing unintended pregnancy, yet the drivers of non-use, inconsistent use, or the use of less effective methods remain unclear. Although preventing all unintended births through increased contraceptive use across the reproductive career is a worthy goal, pregnant women and new mothers are a group uniquely suited for targeted contraceptive counseling to prevent subsequent unintended births. Pregnant and postpartum women may be particularly receptive to information about spacing, planning births, and contraception compared to women at other stages of the reproductive life course. They interact frequently with health care professionals, and both the American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics (AAP) recommend that contraceptive counseling be a primary focus of routine prenatal and postpartum care.15 In recent years, ACOG has initiated programs specifically aimed at increasing the use and efficacy of contraception in the postpartum period.16 Additionally, more than half of unintended births are higher-parity births, indicating that addressing higher-parity births could substantially reduce overall levels of unintended fertility.17
To date, there is a sizeable literature in the public health and medical fields analyzing women’s postpartum contraceptive behavior, largely situated in the literature on rapid repeat pregnancies and post-abortion care and often focused on adolescents in particular.18,19,20,21,22 However, this literature does not explicitly address the question of whether postpartum. contraceptive use varies according to birth intendedness. Given the elevated risk of subsequent unintended fertility among those with an unintended birth, it is important to study postpartum contraceptive behavior as a possible mechanism for this association.
In this paper, we use data from the 2011–15 release of the National Survey of Family Growth (NSFG) to analyze contraceptive uptake, timing, and effectiveness by intendedness of recent births (i.e., on time/too late, slightly mistimed (less than two years too early), seriously mistimed (two or more years too early), or unwanted). The NSFG is uniquely suited for such an analysis, as it collects monthly contraceptive use for up to four years prior to the survey and includes detailed information on all births, including women’s subjective reports of intendedness. We use descriptive statistics, life table analysis, and event history methods to consider how the intendedness of a birth is associated with contraceptive initiation, timing, and method choice (overall efficacy and specific methods).
Background
Reproductive behavior early in the life course is a major focus of family planning programs and policy, as parenthood in the teens and early twenties is often unintended, occurs in less stable relationship contexts, and is potentially disruptive to later achievements and outcomes. Like unintended fertility, early fertility is primarily due to inefficient contraceptive use; sexually active adolescents and young adults use contraception at lower rates, and use less effective methods, than their older counterparts.23,24 However, the overall programmatic focus on early births, particularly the first birth, ignores the fact the majority of births overall are higher -parity births, and thus the majority of unintended births also occur at higher parities.17 Further, elevated rates of rapid repeat pregnancy among adolescent mothers, along with evidence that repeat unintended pregnancies are common across the reproductive years, suggests that ineffective or inconsistent contraceptive use is not limited to nulliparous young women.21,3,4,5 As such, efforts to reduce overall levels of unintended fertility would be well served by better understanding mothers’ contraceptive behavior.
The intention status of the previous birth is one likely predictor of postpartum contraceptive use. To the extent that effective contraceptive use reflects ongoing levels of access to contraception and method adherence, the behavior that leads to an intended or unintended conception may persist after the birth. Women with intended births (those characterized as on time or too late) have demonstrated a planning mentality – that is, they are more likely to have actively wanted and felt prepared to have a child and managed their reproductive behaviors to reach their goals. Conversely, women with unintended births have appear to have some difficulty in managing their reproductive behaviors, perhaps because they are ambivalent about childbearing and do not have clearly formulated plans.25 In any case, these women have births that they themselves identify as occurring when they did not yet feel prepared to do so (slightly or seriously mistimed births) or when they have reached their ideal family size and do not want any, or any more, children (unwanted births). These women, according to their own characterization of their births, exhibited some degree of difficulty aligning their preferences with their actual reproductive behavior in the past. These pre-birth patterns may carry over to postpartum contraceptive use as well.
Existing research on postpartum reproductive behavior suffers from key drawbacks that limit its utility for understanding how postpartum contraceptive use varies by birth intendedness. One, the work focuses heavily on adolescent mothers whose pregnancies are overwhelmingly unintended, making it difficult to consider postpartum contraceptive behavior across the reproductive life course or across intendedness categories.21,26,27 Two, much of it uses small clinical samples or experimental designs, limiting generalizability.22,28 Three, the few large -scale studies on postpartum contraception either do not explicitly consider intendedness or use nonstandard or simplistic measures, making it difficult to align the findings with the extant work on unintended fertility.29,30,31
In this article, we address some of these limitations by analyzing levels of contraceptive use during the postpartum period, timing of postpartum contraceptive initiation, and postpartum method effectiveness among a nationally representative sample. We hypothesize that women with intended births are more likely to use contraception, do so sooner, and adopt more effective methods than their counterparts with unintended births. We do not propose a priori hypotheses about variation across different categories of intended and unintended births (e.g., mistimed vs. unwanted births), but we test for these differences.
Methods
Data
We use 2011–15 data from the National Survey of Family Growth (NSFG) (n = 20,621 men and women). The NSFG is a nationally representative cross -sectional survey of men and women aged 15–44 that contains a detailed retrospective history of births and union histories. For women, it also includes detailed monthly contraceptive method histories for up to four years prior to the month of the survey. More specifically, method histories begin in January of the year three years preceding the survey year, so they include three full years of histories plus the partial period covering the year of the interview. For example, if a woman is interviewed in August of 2011, contraceptive method use is available from January 2008 to August 2011 (all of 2008, all of 2009, all of 2010, and part of 2011). Thus, for each respondent, we have between 37 and 48 months of contraception information.
Of the 11,300 women in the sample, 6,208 had at least one live birth. We examine only live births, as abortions are severely underreported in survey data.32 Because most abortions result from unintended pregnancies, differences in contraceptive use depending on pregnancy intendedness may have important implications for post-abortion care that we are unable to measure with our data. Additionally, because contraceptive use is only measured for a limited time period, our analysis is further restricted to those with a birth that occurred in the period between January of the year three years prior to the survey year up to the month of the survey (n =2,467) ; these births could have been conceived prior to this time period, however. Among those mothers, 346 had more than one birth during this time period. For these women, we include all eligible post -birth intervals, and as such, our initial analytical sample is comprised of 2,813 births to 2,467 women.
Measures
Our dependent variable is the first method the respondent reported using after birth. Respondents reported up to four contraceptive methods for each month included in the contraceptive method history. First, for each month, we identified the most effective method reported, using typical failure rates.33 For example, if a respondent reported using both oral contraceptives and condoms, she is coded as using oral contraceptives. Then, because there were over 20 different methods, we collapsed the methods into a four-category indicator of method use and effectiveness for each month using the Centers for Disease Control’s efficacy categorization.34 The four categories were highly effective methods (tubal ligation, hysterectomy, partner vasectomy, hormonal implant, IUD, coil, or loop), effective methods (birth control pills, injectables, contraceptive patch, emergency contraception, diaphragm, or vaginal ring), least effective methods (male or female condom, withdrawal, sponge, foam, jelly or cream, suppository or insert, calendar rhythm/Standard Days/Cycle Beads, or safe period by temperature or cervical mucus test), plus a category for no method if they were not using any contraception during the month (a detailed list of methods and effectiveness is included in Appendix A). After coding contraceptive method use and effectiveness for up to four years preceding the survey, we then linked each recent birth to the method history for the postpartum period to create monthly contraceptive method use and effectiveness for each month starting with the birth month and every month thereafter until the date of the interview. We excluded two women who had a hysterectomy at delivery for medical reasons, reducing the analytical sample to 2,811 births to 2,465 women.
Intendedness was measured based on responses to a series of retrospective questions asked for every birth. Respondents were first asked “Right before you became pregnant, did you yourself want to have a (nother) baby at any time in the future?” Negative answers were characterized as unwanted births. If a woman responded affirmatively, she was asked about the timing of the pregnancy: “So would you say you became pregnant too soon, at about the right time, or later than you wanted?” Births that were identified as occurring too soon were asked a follow-up question: “How much sooner than you wanted did you become pregnant?” As has become standard with NSFG and other research on unintended births, we used two years as a cutoff point to define the extent of mistiming, with less than two years considered as slightly mistimed and births two or more years too soon categorized as seriously mistimed.35,10 This procedure created a four-category variable: on-time or too late (i.e., intended; preliminary analyses indicated these two categories did not differ from each other), slightly mistimed (less than two years too early), seriously mistimed (two or more years too early), and unwanted. This information was missing for 42 births, further reducing the analytical sample to its final size of 2,769 births to 2,435 women.
Analysis
We begin by presenting weighted descriptive statistics of the analytical sample. Then we delineate the overall distribution of first contraceptive used after the focal birth, including information about the mean number of months between birth and contraceptive uptake, indicating significant differences in the mean number of months where appropriate. This descriptive information is followed by a figure showing contraceptive usage by the intendedness of the focal birth; we conducted a global Pearson chi-square significance test but did not test particular contrasts between each type of intendedness and each type of contraceptive method effectiveness. Next, we used life table analysis to examine the timing to contraceptive initiation within the first year following the focal birth, producing a graph indicating the cumulative probability of having used a contraceptive method for each month across each of the four categories of intendedness. We then turn to multivariate models (described below) to examine postpartum contraceptive uptake and efficacy. Finally, to provide a more detailed picture of postpartum contraceptive behavior, we present the breakdown of each specific method within the four categories of intendedness, again using a global Pearson chi-square significance test.
In the multivariate models, we used event history methods to predict the four-category variable indicating contraceptive behavior described above ; supplementary analyses mentioned briefly but not shown used a dichotomous measure of intendedness (on time/too late vs. all other categories). We converted the birth file into a person-birth-month file (n = 13,750), with each month (starting with the month of birth) having an indicator of contraceptive behavior. If contraceptive method use for a particular month was reported as “don’t know” or “refused” (which was rare), the month was not included in the analysis. Women enter the analysis at the month of birth and leave when they begin using a contraceptive method (i.e., when they move from “no method” to any other type of method), become pregnant (since they are no longer at risk of starting contraception), or are censored at the time of interview. Ideally, we would exclude months in which women were trying to conceive from the analysis (i.e., some set of months prior a pregnancy), as some women may not use contraception because they want to become pregnant soon. However, there is no clear and consistent way of measuring pro-conceptive behavior in these data; we return to this issue in discussing results. Note that we include the actual month of birth, as some methods, such as IUD insertion or tubal ligation, can occur during or shortly after delivery. In preliminary models (not shown), we treated pregnancy as a competing risk, but these models showed no variation by birth intendedness in the odds of exiting via pregnancy relative to censoring at the time of interview. We therefore combined these two categories into a single censoring category in the final model. Less than 7% of the analytical sample became pregnant before beginning contraceptive use or the time of the interview; of all censored respondents, 78% were censored at interview rather than pregnancy. On average, there were 22 months between the focal birth and the interview, with a maximum of 45 months. However, as will be demonstrated in the results, overall postpartum contraceptive use is quite high, and the mean number of months of observation is 6 months (including the birth month).
Analyses control for characteristics associated with both birth intendedness and contraceptive behavior. Time-invariant birth-related factors include parity (1st birth, 2nd, or 3rd or higher birth), prenatal care receipt and timing (1st trimester, 2nd trimester, and 3rd trimester or no care; the latter categories are grouped together due to cell size), and insurance type at delivery (private insurance, Medicaid, or other). We also include a time-varying indicator of breastfeeding during the month. Time-invariant socioeconomic and demographic variables include age at birth, race-ethnicity (categorized as Hispanic, non-Hispanic white, non-Hispanic black, and other), nativity (foreign-born vs. not), and education at the time of interview (which is likely similar to education at the time of the focal birth given the restriction to three-four years prior to the survey).36,37 We also include a time -varying measure of union status (not in a coresidential union, cohabiting, or married). Based on exploratory models, duration since birth is specified as a piecewise nonlinear spline: birth month, 1 month, 2 months, 3 months, 4 months, 5 months, 6 months, 7–12 months, 13–24 months, and 25 or more months after birth. Analyses use the svy commands in Stata 14.2 to account for the complex sampling design and to adjust for the non-independence of outcomes when a single woman has multiple births during the observation period.
Strictly speaking, the unit of analysis in all analyses is a birth, postpartum period, or postpartum person-month. However, because many of the independent variables are characteristics of the women who gave birth, and because the behavioral outcomes are behaviors of women, we sometimes discuss the results in terms of ‘new mothers’ rather than ‘postpartum person-months’ for brevity and clarity.
Results
Descriptive Results
Table 1 shows the characteristics of births in the analytic sample. Of particular note is the distribution of intendedness. The majority (two-thirds) of births were on-time or too late. Among unintended births, unwanted births were the most common, accounting for 14% of all births, followed by seriously mistimed (12%) and slightly mistimed (8%).
Table 1.
Weighted Descriptive Statistics for the Analytical Sample of Births (N = 2,769)
| Intendedness | |
| On time/too late | 66.7% |
| Slightly mistimed | 7.7% |
| Seriously mistimed | 11.5% |
| Unwanted | 14.1% |
| Birth order | |
| 1st birth | 39.1% |
| 2nd birth | 32.8% |
| 3rd or higher | 28.1% |
| Insurance type | |
| Private insurance | 52.0% |
| Medicaid | 43.5% |
| Other | 4.6% |
| Timing of prenatal care | |
| 1st trimester | 89.5% |
| 2nd trimester | 7.7% |
| 3rd trimester or never | 2.9% |
| Started breastfeeding | 72.2% |
| Race-ethnicity | |
| Non-Hispanic white | 55.7% |
| Non-Hispanic black | 14.2% |
| Hispanic | 23.3% |
| Other | 6.9% |
| Foreign-born | 20.0% |
| Age at birth | 28.3 years |
| Union status at birth | |
| Single | 16.1% |
| Cohabiting | 26.1% |
| Married | 57.8% |
| Education | |
| Less than HS | 15.9% |
| HS/GED | 28.0% |
| Some college/AA | 24.6% |
| BA or higher | 31.5% |
May not total 100% due to rounding.
Table 2 shows initial contraceptive behavior after a birth for the sample as a whole, displaying both the effectiveness categories and the specific methods as well as average time to initiation. As seen in the first column, the majority – 82% – of births were followed by the use of some form of contraception after a birth during the period of observation. The modal category of initial postpartum contraception was least effective methods, with 32% of births followed by using such methods. For those whose first method was a least effective method, initiation began, on average, almost three months after birth. By far, the most common of these methods was condoms (accounting for 64% of all least effective method use), followed by withdrawal (28%). Effective methods of contraception were the first type of postpartum method used after 28% of births, occurring about two months on average after a birth. Birth control pills (64%) and injectables (28%) were the most common of the effective methods. Finally, less than a fourth (23%) of births were followed by an initial adoption of a highly effective contraceptive method, occurring slightly more than a month and a half, on average, after the birth. Just under half of these births were followed by sterilization (either male or female), and 44% were followed by the usage of an IUD, coil, or loop. Overall, the more effective the method of first postpartum contraception, the sooner it was adopted. These timing differences are driven in part by the fact that both female sterilization and IUD insertion can occur at the time of the birth.
Table 2.
Weighted Descriptive Information on 1st Contraceptive Use after Birth (N = 2,769)
| AMONG ALL NEW MOTHERS, PERCENT USING | |
| Highly effective methods | 23.3% |
| Mean no. of months until use or censoring (std dev) | 1.63 mos (2.53) |
| Effective methodsA | 27.6% |
| Mean no. of months until use or censoring (std dev) | 1.98 mos (2.59) |
| Least effective methodsA,B | 31.5% |
| Mean no. of months until use or censoring (std dev) | 2.76 mos (3.38) |
| No method | 17.7% |
| Mean no. of months until use or censoring (std dev) | 11.09 mos (10.66) |
| WITHIN EACH METHOD CATEGORY, PERCENT USING | |
| Highly effective methods | |
| Sterilization | 46.2% |
| Implant | 10.0% |
| IUD, coil, or loop | 43.8% |
| Effective methods | |
| Emergency contraception | 1.5% |
| Birth control pills | 63.8% |
| Depo-Provera (injectables) | 27.8% |
| Contraceptive patch | 1.3% |
| Diaphragm | 0.4% |
| Vaginal contraceptive ring | 5.3% |
| Least effective methods | |
| Male or female condom | 64.3% |
| Withdrawal | 28.4% |
| Spermicide/inserts | 1.2% |
| “Natural” methods (safe period, calendar, etc.) | 6.1% |
Mean number of months between birth and initiation of contraception is significantly longer for effective and least effective methods relative to highly effective methods at p≤.05.
Mean number of months between birth and initiation of contraception is significantly longer for least effective methods relative to effective methods at p≤.05.
May not total 100% due to rounding.
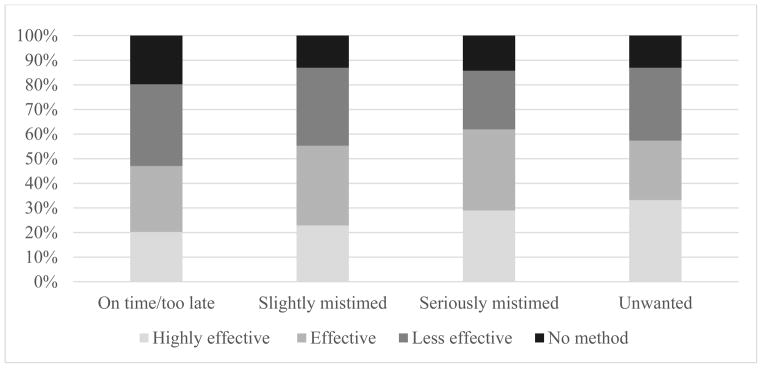
However, as seen in Figure 1, the contraceptive efficacy of the first method used after a birth varies significantly by birth intendedness overall. New mothers with births characterized as on time or too late reported the highest proportions of non-use over the period of observation (20%). A third of those with on time or too late births first used a least effective method, a similar level to that of new mothers with slightly mistimed births (32%) and unwanted births (30%). Among new mothers with unwanted births, the modal category was to use a highly effective method (33%), but 30% first adopted a least effective method, with relatively few using effective methods (24%). Roughly equal proportions of mothers with slightly and seriously mistimed births first reported using effective methods (32% and 33%, respectively), but more mothers with a slightly mistimed birth used a least effective method (33%) than those with a seriously mistimed birth (24%).
Figure 1.
Contraceptive Efficacy by Birth Intendedness
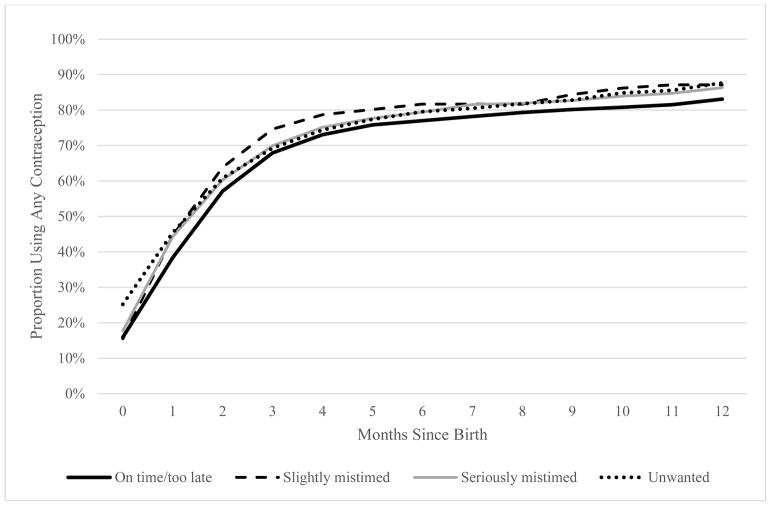
In Figure 2, we display the timing to contraceptive initiation within the first year postpartum by intendedness, drawing from life table analysis. As seen here, the pattern of contraceptive use and initiation was generally similar across all categories of intendedness, with contraceptive uptake increasing sharply from birth through the first three months, increasing more slowly in months three through six, and then largely plateauing (with perhaps a small increase in months ten through twelve). Contraceptive initiation occurred earlier after unwanted births, with the percentage using a method during the same month as birth (26%) higher than the other intendedness categories (15 –18%). By the first month postpartum, women with both slightly and seriously mistimed births were at similar levels of contraceptive use (around 44%), with postpartum use lower following on time/too late births (38%). Usage following slightly mistimed births was higher for months two through six than the other unintended birth categories, but overall, contraceptive use was lower throughout the entire first year postpartum among those with on time and too late births. In sum, the descriptive statistics largely do not support our hypothesis. Instead, we find that new mothers with unintended births adopt contraception more often, do so sooner, and choose more effective methods than those with intended births.
Figure 2.
Contraceptive Use in the First Year after Birth, by Intendedness
Multivariate results
To more thoroughly examine the linkage between birth intendedness and postpartum contraceptive use and consider whether birth and individual characteristics potentially negate the observed bivariate association between intendedness and contraceptive behavior, we turn to multinomial logistic event history models. We begin by presenting the relative risk ratios (RRRs) for each category of efficacy relative to no method, then present the contrasts between each category of method efficacy (Table 3). Looking at intendedness, compared to mothers with on time/too late births, mothers with births that were characterized as seriously mistimed or unwanted were significantly more likely to use a highly effective method rather than no method (RRR = 1.9 and 1.7, respectively), with no differences in effective use relative to no method. Interestingly, as suggested in the descriptive statistics, new mothers with an unwanted birth were also about 50% more likely to use a least effective method than no method compared to their peers with on time/too late births. In the latter columns, which examine the contrast between specific categories of contraceptive efficacy, we see that new mothers with seriously mistimed births were significantly less likely, by about 50%, to use either an effective or least effective method than a highly effective method. Supplementary analyses using a dichotomous indicator of intendedness (not shown) demonstrated that all unintended births increased the risk of using a highly effective method by about 70% rather than no method and decreased the risk of using an effective method relative to a highly effective method by about 40%. In sum, the models generally do not provide support for our hypothesis that unintended births are associated with lower rates of postpartum contraceptive use. Although some of the covariates were significantly associated with contraceptive use (discussed below), they do not explain the link with intendedness observed in descriptive analyses.
Table 3.
Relative Risk Ratios from Multinomial Logistic Event History Models Predicting First Postpartum Contraceptive Use
| Highly effective vs. no method | Effective vs. no method | Least effective vs. no method | Effective vs. highly effective | Least effective vs. highly effective | Least effective vs. effective | |
|---|---|---|---|---|---|---|
| Intendedness | ||||||
| On time/too late | - | - | - | - | - | - |
| Slightly mistimed | 1.25 | 1.31 | 1.15 | 1.05 | 0.92 | 0.88 |
| Seriously mistimed | 1.93*** | 1.00 | 1.02 | 0.52** | 0.53** | 1.02 |
| Unwanted | 1.67** | 1.16 | 1.47* | 0.70 | 0.88 | 1.26 |
| Birth order | ||||||
| 1st birth | - | - | - | - | - | - |
| 2nd birth | 2.02*** | 0.91 | 1.36* | 0.45*** | 0.67* | 1.49 |
| 3rd or higher | 2.75*** | 0.75 | 0.94 | 0.27*** | 0.34*** | 1.26 |
| Insurance type | ||||||
| Private insurance | - | - | - | - | - | - |
| Medicaid | 1.39* | 0.87 | 0.90 | 0.63* | 0.64* | 1.03 |
| Other | 0.81 | 0.39*** | 0.99 | 0.48* | 1.22 | 2.55** |
| Timing of prenatal care | ||||||
| 1st trimester | - | - | - | - | - | - |
| 2nd trimester | 0.66* | 0.96 | 1.01 | 1.47 | 1.53 | 1.04 |
| 3rd trimester or never | 1.34 | 1.72 | 1.45 | 1.28 | 1.08 | 0.85 |
| Breastfeeding during the month | 0.76* | 0.87 | 1.35* | 1.16 | 1.78** | 1.54* |
| Race-ethnicity | ||||||
| Hispanic | 0.89 | 0.99 | 1.06 | 1.12 | 1.19 | 1.06 |
| Non-Hispanic white | - | - | - | - | - | - |
| Non-Hispanic black | 0.62** | 1.09 | 1.07 | 1.75* | 1.72* | 0.98 |
| Other | 0.78 | 0.88 | 1.17 | 1.14 | 1.44 | 1.26 |
| Foreign born | 0.72 | 0.74 | 0.91 | 1.03 | 1.26 | 1.22 |
| Age at birth | 1.01 | 0.95*** | 0.99 | 0.95*** | 0.98 | 1.04 |
| Union status (time-varying) | ||||||
| Single | 0.79 | 0.80 | 0.67* | 1.00 | 0.85 | 0.84 |
| Cohabiting | 0.91 | 1.18 | 0.65* | 1.30 | 0.71 | 0.55* |
| Married | - | - | - | - | - | - |
| Education | ||||||
| Less than HS | 0.91 | 1.43* | 0.67* | 1.58 | 0.73 | 0.47*** |
| HS/GED | - | - | - | - | - | - |
| Some college/AA | 1.13 | 1.35 | 0.74 | 1.20 | 0.66* | 0.55** |
| BA or higher | 0.83 | 1.17 | 0.72 | 1.41 | 0.86 | 0.61 |
| Months since birth | ||||||
| Birth month | 0.97 | 0.33*** | 0.49*** | 0.34*** | 0.50** | 1.45 |
| 1 mon after birth | - | - | - | - | - | - |
| 2 mos after birth | 1.09 | 0.93 | 1.74** | 0.85 | 1.59 | 1.87* |
| 3 mos after birth | 0.88 | 0.46** | 1.73** | 0.52 | 1.98* | 3.81*** |
| 4 mos after birth | 0.44** | 0.48** | 0.99 | 1.10 | 2.26* | 2.06* |
| 5 mos after birth | 0.42 | 0.21*** | 0.50* | 0.51 | 1.18 | 2.33 |
| 6 mos after birth | 0.10*** | 0.08*** | 0.42* | 0.77 | 4.24* | 5.54** |
| 7–12 mos after birth | 0.06*** | 0.09*** | 0.27*** | 1.46 | 4.35*** | 2.97** |
| 13–24 mos after birth | 0.04*** | 0.01*** | 0.10*** | 0.41 | 2.81* | 6.86*** |
| 25+ mos after birth | 0.01*** | 0.02*** | 0.08*** | 1.95 | 9.04 | 4.62 |
| Constant | 0.05*** | 0.78 | 0.19** | 15.62*** | 3.82 | 0.24* |
| Person-birth-months | 13,750 | |||||
| Births | 2,769 | |||||
| Women | 2,435 | |||||
p≤.05
p≤.01
p≤.001
Looking at the birth-related covariates, parity was associated with postpartum contraceptive initiation and efficacy. Compared to first -time mothers, those with a higher-parity birth were significantly more likely to use a highly effective method than any of the other method categories; interestingly, mothers having a second birth were also more likely to use a least effective method than no method (RRR = 1. 4). New mothers whose birth was paid for by Medicaid were more likely to use a highly effective method than no method, an effective method, or a least effective method than their peers whose birth was paid for by private insurance. Mothers who reported using neither private insurance nor Medicaid were less likely to use an effective method than no method or a highly effective method and more likely to use a least effective method. Compared to mothers who initiated prenatal care in the 1st trimester, beginning prenatal care in the 2nd trimester decreased the chances of using a highly effective method relative to no method by about a third. Breastfeeding mothers had an elevated risk of using a least effective method rather than no method (RRR = 1.4), an effective method (RRR = 1.5), or a highly effective method (RRR = 1.8). Age was somewhat related to contraceptive use, with increasing age at birth linked to lower chances of using an effective method relative to no method.
Net of birth-related characteristics, relatively few socioeconomic and demographic covariates were associated with initiation of contraception after a birth in the multivariate models. Non-Hispanic black mothers were about 40%less likely to use a highly effective method than no method and about 75% more likely to use an effective or least effective method relative to non-Hispanic white mothers. Compared to new mothers with a high school degree at the time of interview, women without a high school degree were about 40% less likely to use a least effective method than no method and 50% less likely to use a least effective method than an effective method. Mothers with some college were more likely to use an effective method than no method and less likely to use a least effective method than a highly effective method or an effective method. Relative to their married counterparts, single and cohabiting mothers were about a third as likely to use a least effective method than no method, and cohabiting mothers were also about half as likely to use a least effective method than an effective method.
Finally, time since birth was a strong predictor of contraceptive uptake. In general, new mothers are less likely to begin contracepting in the same month as their birth compared to the first month after birth, except when the first method adopted was a highly effective method. Relative to the first month, there were also no differences in initiating a highly effective or effective method (rather than no method) in the second month. The first and second months almost certainly account for the bulk of new mothers’ first postpartum check-ups, in which contraceptive counseling may occur. For highly effective methods relative to no method, the chances of initiating such methods does not begin to decline significantly until the fourth month (RRR = 0.4). For effective methods relative to no method, the decline in initiation begins with the third month (compared to the first month postpartum). Initiating least effective methods relative to no method spikes by about 70% in months three and four and then declines. With the exception of the birth month, there are no differences in the timing of initiation of effective methods rather than highly effective methods; however, the odds of initiating in later months is higher for mothers using least effective methods than highly effective or effective methods.
To provide a more nuanced examination of which methods new mothers are specifically using by the intendedness of their birth, we turn to Table 4. There were indeed differences in specific methods, and we highlight a few particularly interesting examples. The multivariate analysis showed that both mothers with seriously mistimed births and those with unwanted births were more likely to adopt a highly effective method; however, among mothers within this group, those with seriously mistimed births were predominantly using LARCs whereas those with unwanted births were predominantly using sterilization (either male or female). As suggested in both the bivariate statistics and the multivariate analysis, though, there appears to be a sizeable group of mothers with unwanted births who were using least effective methods – a tenth of all mothers with unwanted births used withdrawal as their first postpartum contraceptive method.
Table 4.
Detailed Distribution of 1st Contraceptive Method by Intendedness
| Sterilization | Implant | IUD, coil, or loop |
Depo- Provera |
Birth control pills |
Cont. patch |
Vaginal ring |
Diaphragm | Spermicide /inserts |
Emer- gency cont. |
Male or female condom |
With- drawal |
“Natural” methods |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| On time/ | 12.2% | 2.4% | 10.6% | 6.9% | 24.1% | 0.3% | 1.5% | 0.2% | 0.5% | 0.5% | 25.6% | 12.1% | 3.2% |
| Slightly mistimed | 6.6% | 1.4% | 18.2% | 14.2% | 17.4% | 0.8% | 4.7% | 0.0% | 0.7% | 0.2% | 25.4% | 7.7% | 2.6% |
| Seriously mistimed | 8.7% | 6.6% | 18.4% | 14.0% | 20.2% | 1.3% | 2.1% | 0.3% | 0.0% | 0.4% | 21.0% | 6.6% | 0.2% |
| Unwanted | 24.0% | 2.2% | 12.0% | 13.1% | 12.5% | 0.2% | 1.0% | 0.0% | 0.7% | 0.9% | 22.7% | 10.5% | 0.2% |
| Total | 13.1% | 2.8% | 12.4% | 9.3% | 21.4% | 0.4% | 1.8% | 0.1% | 0.5% | 0.5% | 24.6% | 10.9% | 2.3% |
Withdrawal was more often used as the first postpartum method among those with on time or too late births (12%) than among new mothers with mistimed births (7–8%). Among those with on time/too late births, new mothers most commonly first used condoms (26%) followed by the pill (24%). In fact, condoms were the modal category of first method use for new mothers with on time/too late (26%), slightly mistimed births (25%), and (just barely) seriously mistimed (21%); for the latter, the pill was close behind, lagging by only 0.8 percentage points. Using ‘natural’ methods, such as the calendar rhythm or safe periods, was very uncommon among mothers with seriously mistimed or unwanted births (0.2% for both groups) whereas 3% of mothers with on time/too late and slightly mistimed births first adopted this method. Twice as many mothers with any type of unintended birth used injectables (13 –14% across all three categories) as mothers with on time/too late births (7%). Vaginal rings and implants were fairly rare overall (2% and 3%, respectively), but about 5% of mothers with slightly mistimed births first used a vaginal ring, and 7% of those with a seriously mistimed birth used an implant.
Discussion
Women with an unintended pregnancy are at an elevated risk of experiencing a subsequent unintended pregnancy. One potential explanation is that these women differ in their postpartum contraceptive behavior– uptake, timing, and method choice. In this paper, we used rich data with detailed histories of contraceptive behavior and birth intendedness to examine women’s experiences of postpartum contraception. We posited one key hypothesis:based on prior research and arguments that mothers with intended births are better able to manage their reproductive and contraceptive behavior, we expected that postpartum contraception would occur more often, sooner, and involve more effective methods among those with intended births than those with unintended births.
Our results strongly contradict our hypothesis. New mothers with intended births (those characterized as on time or too late) had lower rates of contraceptive use during the period of observation, tended to start using a method later, and more often relied on less effective methods. New mothers with unintended births – particularly those with seriously mistimed and unwanted births – were more likely to use highly effective methods than no method, and mothers with seriously mistimed births were also more likely to use highly effective methods than less effective methods. For those using highly effective methods, new mothers with unwanted births more often used sterilization whereas those with seriously mistimed births tended to opt for LARCs. As such, it seems that new mothers with births arising from the more ‘severe’ types of unintended pregnancies take actions to better control their future fertility. However, it is worth noting that there is also a subset of mothers with unwanted births whose initial contraceptive method was one of the least effective methods (primarily condoms and withdrawal).
There are two possible explanations as to why new mothers with unintended births may be adopting methods sooner and using more effective methods than mothers with intended births. First, to the extent that all women, regardless of birth intendedness, have some level of both prenatal and postpartum care, then all women likely receive some level of family planning counseling. In fact, this is one of the goals of the postpartum care visit, and women who have such visits are more likely to use contraception.21,38 Second, it could be that new mothers with an unintended birth are more motivated to avoid a subsequent birth, at least in the short-term. Mothers with intended births are most likely to feel prepared to meet the needs of parenting an infant and have entered, or are still in, a family-building stage, whereas mothers with an unintended birth may view the birth as highly disruptive to educational, occupational, or relational statuses and goals.39 The perceived shock to current and future statuses may spur this group of new mothers to become more explicit about their reproductive and contraceptive preferences, goals, and behaviors.40
The earlier uptake of more effective methods among mothers after an unintended birth suggests that the elevated chances of subsequent unintended fertility among these women are not driven by contraceptive method uptake, timing, or type choice in the short term. The question then arises, what explains the higher risk of repeat unintended fertility? Mothers with unintended births may differ in their method adherence compared to their peers with intended births. Perhaps such women discontinue or switch their methods more frequently or sooner or, for methods that entail more user effort (like condoms or daily pills), use the method less consistently. It is also possible that the earlier documented link between one unintended birth and the risk of subsequent unintended births has attenuated or disappeared. The growing availability and acceptability of LARCs in recent years, for instance, thanks to both marketing campaigns and insurance coverage provided through the Affordable Care Act, may have made more effective methods more accessible to those with an unintended birth than in the past. Moreover, public health efforts to reduce both unintended and teen fertility, along with the movement away from abstinence-only programs to comprehensive sex education in recent years, may have helped women better understand how to control their fertility.41
Limitations
A possible limitation of the analysis is the inability to fully account for whether new mothers anticipate having another birth after the focal birth. If new mothers, particularly those with intended births, are already planning on having another child within a year or two, they may not use any contraception or avoid using more effective methods in favor of methods that are easy to discontinue and have no lingering effects on fecundity. We did explore models in which we dropped person-birth-months based on questions about whether respondents were trying at the time of the survey to get pregnant and for how long. In these exploratory models, we also dropped, for those with a subsequent pregnancy during the observation period, the six months prior to the next pregnancy (though only if it was intended); it is worth noting that we do not actually know how long these women were trying to get pregnant, so the six months is just an assumption. Because so few new mothers (n = 13) were either trying to get pregnant or had an intended subsequent pregnancy without first using contraception after the focal birth, the results were virtually identical, leading us to conclude that anticipation of continued childbearing in the short term is unlikely to explain the observed differences. The analysis also did not control for contraceptive use prior to the focal birth, although new mothers’ postpartum contraceptive choice could reflect a return to pre -pregnancy methods. Many women discontinue contraception explicitly to get pregnant (along with other reasons), but because we have no information on how long women were trying to conceive the focal birth, it is not clear when would be the appropriate pre-pregnancy month to capture earlier contraceptive behavior. And, of course, the data only include only a limited time frame of detailed contraceptive method use. Another limitation is that we did not examine the duration of new mothers’ first method choice in this current analysis nor could we analyze method consistency or adherence. Finally, we were unable to examine post-abortion contraceptive behaviors due to concerns over the quality of the abortion reports in the NSFG.32 Most abortions result from unintended pregnancies, but differences in contraceptive use between mistimed and unwanted pregnancies could have important implications for post-abortion care.
Conclusion
Despite modest declines in unintended fertility in recent years, continued efforts to examine how women manage their fertility careers is warranted. This research simultaneously provides insight and raises more questions. Our analysis shows significant variation in contraceptive use among new mothers depending on the reported intendedness of the previous birth. These results demonstrate the importance of understanding contraceptive decision-making as part of a series of linked reproductive outcomes, rather than simply an isolated event. The findings also point to the potential role of contraceptive counseling and service provision during prenatal and immediate postpartum care in reducing inequalities in access to family planning services. Studies show that less advantaged women benefit more from prenatal and postpartum contraceptive counseling in terms of postpartum contraceptive use, yet there is some evidence to suggest these women are less likely to attend a postpartum care visit and that such visits often occur after individuals have already resumed sexual activity.42,43 Still, our finding that women with unintended births are more likely to use highly effective methods afterbirth than women with intended births suggests that postpartum care can address and even reverse gaps in access to and use of contraception. It is not clear how the broader range of family planning services to non-pregnant women might adapt in order to become similarly effective; it is possible that the way prenatal and postpartum services are organized and funded makes them more accessible, but it may also be the case that it is inherently easier to provide care over a clearly defined time period and for a specific purpose. More research explicitly identifying the barriers less advantaged women – who are more likely to experience unintended fertility – have in accessing and using family planning services to manage their reproductive careers is needed.
Acknowledgments
This research was partially supported from center grants to Bowling Green State University’s Center for Family and Demographic Research (P2C-HD050959) and Ohio State University’s Institute for Population Research (P2C-HD058484).
Appendix A. Contraceptive Efficacy Categorization, Methods, and Failure Rates
| Categorization | Specific Methods | Typical Failure Rates (one year) |
|---|---|---|
| Highly effective | Tubal ligation, hysterectomy | 0.50% |
| Less than 1 pregnancy per 100 women in a year | Vasectomy | 0.15% |
| Hormonal implant | 0.05% | |
| IUD, coil, or loopA | 0.2–0.8% (depending on type) | |
| Effective | Emergency contraception B | |
| 6–12 pregnancies per 100 women in a year | Birth control pills | 9% |
| Depo-Provera (injectables) | 6% | |
| Contraceptive patch | 9% | |
| Diaphragm | 9% | |
| Vaginal contraceptive ring | 9% | |
| Least effective | Condom | 18% |
| 18–28 pregnancies per 100 women in a year | Female condom | 21% |
| Withdrawal | 22% | |
| Sponge | 12–22% (nulliparous & parous women, respectively) | |
| Foam | 28% | |
| Jelly or cream | 28% | |
| Suppository or insert | 28% | |
| Calendar rhythm, Standard days, or Cycle Beads | 24% | |
| Safe period by temperature or cervical mucus test | 24% | |
| No method | ||
| 85 pregnancies per 100 women in a year | ||
These three methods were grouped together in the original question in the NSFG survey.
Emergency contraception (EC) failure rates are generally not calculated in the same manner as other methods, as they are linked to specific experiences of unprotected sex. If EC was the only form of contraception used for an entire year, the risk of getting pregnant would range from 20% to 35%44. However, for a single instance, EC lowers the risk of pregnancy by 65%–95% in the case of oral pills (depending on formulation and when the pills were taken relative to unprotected sex) and up to 99% when a copper IUD is inserted.
Footnotes
An earlier version of this paper was presented at the 2017 annual meeting of the American Sociological Association in Montreal, Canada.
Contributor Information
Karen Benjamin Guzzo, Bowling Green State University.
Kasey Eickmeyer, Bowling Green State University.
Sarah R. Hayford, Ohio State University
References
- 1.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. New England Journal of Medicine. 2016;374(9):843–852. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Child Trends. Child Trends Databank. Washington, DC: Child Trends; 2013. [Accessed 1/10/17]. Unintended births. http://www.childtrends.org/?indicators=unintended-births. [Google Scholar]
- 3.Guzzo KB, Hayford SR. Fertility following an unintended first birth. Demography. 2011;48(4):1493–1516. doi: 10.1007/s13524-011-0059-7. [DOI] [PubMed] [Google Scholar]
- 4.Rajan S, Morgan SP, Harris KM, Guilkey D, Hayford SR, Guzzo KB. Trajectories of Unintended Fertility. Population Research and Policy Review. 2017;36(6):903–928. doi: 10.1007/s11113-017-9443-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wildsmith E, Guzzo KB, Hayford SR. Repeat unintended, unwanted and seriously mistimed childbearing in the United States. Perspectives on Sexual and Reproductive Health. 2010;42(1):14–22. doi: 10.1363/4201410. [DOI] [PubMed] [Google Scholar]
- 6.Guzzo KB, Hayford SR. Unintended fertility and the stability of coresidential relationships. Social Science Research. 2012;41(5):1138–1151. doi: 10.1016/j.ssresearch.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herd P, Higgins J, Sicinski K, Merkurieva I. The implications of unintended pregnancies for mental health in later life. American Journal of Public Health. 2016;106(3):421–429. doi: 10.2105/AJPH.2015.302973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCrory C, McNally S. The effect of pregnancy intention on maternal prenatal behaviours and parent and child health: results of an Irish cohort study. Paediatric and Perinatal Epidemiology. 2013;27(2):208–215. doi: 10.1111/ppe.12027. [DOI] [PubMed] [Google Scholar]
- 9.Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography. 2015;52(1):83–111. doi: 10.1007/s13524-014-0359-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindberg L, Maddow-Zimet I, Kost K, Lincoln A. Pregnancy intentions and maternal and child health: An analysis of longitudinal data in Oklahoma. Maternal and Child Health Journal. 2015;19(5):1087–1096. doi: 10.1007/s10995-014-1609-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller WB, Sable MR, Beckmeyer JJ. Preconception motivation and pregnancy wantedness: Pathways to toddler attachment security. Journal of Marriage and Family. 2009;71(5):1174–1192. [Google Scholar]
- 12.Maddow-Zimet I, Lindberg L, Kost K, Lincoln A. Are pregnancy intentions associated with transitions into and out of marriage? Perspectives on sexual and reproductive health. 2016;48(1):35–43. doi: 10.1363/48e8116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barber J, East PL. Children’s experiences after the unintended birth of a sibling. Demography. 2011;48:101–125. doi: 10.1007/s13524-010-0011-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sonfield A, Hasstedt K, Gold RB. Moving Forward: Family Planning in the Era of Health Reform. New York: Guttmacher Institute; 2014. [Google Scholar]
- 15.Kilpatrick SJ, Papile LA, Macones GA. Guidelines for Perinatal Care. 8. American Academy of Pediatrics; 2017. [Google Scholar]
- 16.American College of Obstetrics and Gynecologists. [Accessed 3/12/18];Committee Opinion: Immediate Postpartum Long-Acting Reversible Contraception. 2016 Aug;(670) https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Immediate-Postpartum-Long-Acting-Reversible-Contraception.
- 17.Guzzo KB. Family Profiles, FP-17-08. Bowling Green, OH: National Center for Family & Marriage Research; 2017. A quarter century of change in unintended births. [Google Scholar]
- 18.de Bocanegra HT, Chang R, Howell M, Darney P. Interpregnancy intervals: impact of postpartum contraceptive effectiveness and coverage. American Journal of Obstetrics and Gynecology. 2014;210(4):311–e1. doi: 10.1016/j.ajog.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 19.Langston AM, Joslin-Roher SL, Westhoff CL. Immediate postabortion access to IUDs, implants and DMPA reduces repeat pregnancy within 1 year in a New York City practice. Contraception. 2014;89(2):103–108. doi: 10.1016/j.contraception.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Matulich M, Cansino C, Culwell KR, Creinin MD. Understanding women’s desires for contraceptive counseling at the time of first-trimester surgical abortion. Contraception. 2014;89(1):36–41. doi: 10.1016/j.contraception.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Chacko MR, Wiemann CM, Buzi RS, Kozinetz CA, Peskin M, Smith PB. Choice of postpartum contraception: Factors predisposing pregnant adolescents to choose less effective methods over long-acting reversible contraception. Journal of Adolescent Health. 2016;58(6):628–635. doi: 10.1016/j.jadohealth.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Damle LF, Gohari AC, McEvoy AK, Desale SY, Gomez-Lobo V. Early initiation of postpartum contraception: does it decrease rapid repeat pregnancy in adolescents? Journal of Pediatric and Adolescent Gynecology. 2015;28(1):57–62. doi: 10.1016/j.jpag.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Jones J, Mosher D, Daniels K. National Health Statistics Reports. Hyattsville, MD: National Center for Health Statistics; 2012. Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995; p. 60. [PubMed] [Google Scholar]
- 24.Daniels K, Daugherty J, Jones J, Mosher W. National Health Statistics Reports. Hyattsville, MD: National Center for Health Statistics; 2015. Current contraceptive use and variation by selected characteristics among women aged 15–44: United States, 2011–2013; p. 86. [PubMed] [Google Scholar]
- 25.Borrero S, Nikolajski C, Steinberg JR, Freedman L, Akers AY, Ibrahim S, Schwarz EB. “It just happens”: a qualitative study exploring low-income women’s perspectives on pregnancy intention and planning. Contraception. 2015;91(2):150–156. doi: 10.1016/j.contraception.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coles MS, Makino KK, Stanwood NL. Contraceptive experiences among adolescents who experience unintended birth. Contraception. 2011;84(6):578–584. doi: 10.1016/j.contraception.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson EK, Fowler CI, Koo HP. Postpartum contraceptive use among adolescent mothers in seven states. Journal of Adolescent Health. 2013;52(3):278–283. doi: 10.1016/j.jadohealth.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Potter JE, Hopkins K, Aiken AR, Hubert C, Stevenson AJ, White K, Grossman D. Unmet demand for highly effective postpartum contraception in Texas. Contraception. 2014;90(5):488–495. doi: 10.1016/j.contraception.2014.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White K, Potter JE, Hopkins K, Grossman D. Variation in postpartum contraceptive method use: results from the Pregnancy Risk Assessment Monitoring System (PRAMS) Contraception. 2014;89(1):57–62. doi: 10.1016/j.contraception.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hernandez LE, Sappenfield WM, Goodman D, Pooler J. Is effective contraceptive use conceived prenatally in Florida? The association between prenatal contraceptive counseling and postpartum contraceptive use. Maternal and Child Health Journal. 2012;16(2):423–429. doi: 10.1007/s10995-010-0738-9. [DOI] [PubMed] [Google Scholar]
- 31.Zapata LB, Tregear SJ, Tiller M, Pazol K, Mautone-Smith N, Gavin LE. Impact of reminder systems in clinical settings to improve family planning outcomes: a systematic review. American Journal of Preventive Medicine. 2015;49(2):S57–S64. doi: 10.1016/j.amepre.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones RK, Kost K. Reporting of induced and spontaneous abortion in the 2002 National Survey of Family Growth. Presented at the National Center for Health Statistics National Survey of Family Growth Research Conference; Bethesda, MD. October 19th–20th.2006. [Google Scholar]
- 33.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control. [Accessed 1/9/17];Effectiveness of Family Planning Methods. 2016 https://www.cdc.gov/reproductivehealth/contraception/unintendedpregnancy/pdf/contraceptive_methods_508.pdf.
- 35.Mosher WD, Jones J, Abma JC. National Health Statistics Reports. Hyattsville, MD: National Center for Health Statistics; 2012. Intended and unintended births in the United States: 1982–2010; p. 55. [PubMed] [Google Scholar]
- 36.Augustine JM. Exploring New Life Course Patterns of Mother’s Continuing Secondary and College Education. Population Research and Policy Review. 2016;35(6):727–755. doi: 10.1007/s11113-016-9401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gault B, Reichlin L, Reynolds E, Froehner M. IWPR #C424. Institute for Women’s Policy Research; George Washington, D.C: 2014. 4.8 million college students are raising children. [Google Scholar]
- 38.Masho SW, Cha S, Charles R, McGee E, Karjane N, Hines L, Kornstein SG. Postpartum visit attendance increases the use of modern contraceptives. Journal of Pregnancy. 2016 doi: 10.1155/2016/2058127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kavanaugh ML, Kost K, Frohwirth L, Maddow-Zimet I, Gor V. Parents’ experience of unintended childbearing: A qualitative study of factors that mitigate or exacerbate effects. Social Science & Medicine. 2017;174:133–141. doi: 10.1016/j.socscimed.2016.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edin K, Kefalas M. Promises I can keep: Why poor women put motherhood ahead of marriage. Berkeley, CA: University of California Press; 2005. [Google Scholar]
- 41.Donovan M. The looming threat to sex education: A resurgence of federal funding for abstinence-only programs? Guttmacher Policy Review. 2017;20:44–47. [Google Scholar]
- 42.Zapata LB, Murtaza S, Whiteman MK, Jamieson DJ, Robbins CL, Marchbanks PA, D’Angelo DV, Curtis KM. Contraceptive counseling and postpartum contraceptive use. American Journal of Obstetrics & Gynecology. 2015;212(2):171–e1. doi: 10.1016/j.ajog.2014.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Henderson V, Stumbras K, Caskey R, Haider S, Rankin K, Handler A. Understanding factors associated with postpartum visit attendance and contraception choices: listening to low-income postpartum women and health care providers. Maternal and child health journal. 2016;20(1):132–143. doi: 10.1007/s10995-016-2044-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Trussell J, Raymond EG, Cleland K. Working paper published by the Office of Population Research. Princeton University; 2017. [Accessed 8/1/17]. Emergency contraception: A last chance to prevent pregnancy. http://ec.princeton.edu/questions/ec-review.pdf#page=3. [Google Scholar]