Abstract
Background and Purpose
Recent evidence has suggested physical therapist involvement in care transitions after hospitalization is associated with reduced rates of hospital readmissions. However, little is known about how physical therapists participate in care transitions for older adults, the content of care communications, and the facilitators and barriers of implementing evidence-based care transitions strategies into practice. Thus, the purpose of this paper is to evaluate participation in care transition activities known to influence readmission risk among older adults, and understand perceptions of and barriers to participation in these activities.
Methods
We developed a survey questionnaire to quantify hospital-based physical therapist participation in care transitions and validated it using cognitive interviewing. It was introduced to a cross-sectional national sample of physical therapists who participate in the Academy of Acute Care Physical Therapy electronic discussion board using a SurveyMonkey™ tool.
Results and Discussion
Over 90% of respondents agreed they routinely recommended a discharge location and provide recommendations for durable medical equipment for patients at the time of hospital discharge. Respondents did not routinely initiate communication with therapists in other care settings, or follow up with patients to determine if recommendations were followed. A majority of respondents agreed their facilities would not consider many key care transition activities to count as productive time.
This survey provides a novel insight into how hospital-based physical therapists participate in care transitions. Communications between rehabilitation providers across care settings are infrequent, even those communications recommended to help reduce readmissions. However, administrative barriers were elucidated in this study that may help explain lack of therapist involvement.
Conclusions
Physical therapists’ communications across healthcare setting about older adults discharging from acute care hospitalization are infrequent, but may represent a meaningful intervention target for future studies. Future research is needed to evaluate best practices for hospital-based physical therapists during care transitions.
Keywords: Care Coordination, Communication, Readmissions, Physical Therapist
INTRODUCTION
Readmissions within 30 days of a hospital discharge are a quality indicator used by the Center for Medicare and Medicaid Services (CMS) to evaluate acute care hospitals; financial penalties are associated with higher than expected rates of unplanned hospitalizations. One risk factor for hospital readmissions is incomplete transfer of information between hospital providers and community providers after hospitalization.1–3 Communication between hospital and community providers during this care transition period is often sporadic, asynchronous, and incomplete. Synchronous (e.g., by telephone) communication occurs only 3% of the time between hospital physicians and community physicians, and discharge summaries were available to community physicians 12% of the time at the time of follow-up.1 Physicians report these omissions impact patient outcomes adversely.3–5
Information about a patient’s limitations in activities of daily living (ADLs) at hospital discharge is commonly omitted from physician discharge summaries. Notably, one study found 53% of physician discharge summaries contained no information about patient safety with mobility, need for assistance, or assistive device needs.6 This is troubling given that limited physical function is a risk factor for hospital readmissions.7–9
Physical therapists (PTs) often assess and intervene upon deficits in physical function in hospital settings. Because impairments in bodily function10 and limited activity participation11 are associated with hospital readmissions, it is imperative that information about rehabilitation progress and physical function are provided to physicians and PTs at the next level of care during a transition of care. Involvement of PTs in care transitions is associated with reduced hospital readmissions.12 However, the extent to which hospital-based PTs communicate with other therapists or physician providers across care settings is incompletely understood, and may represent a target for future quality improvement initiatives.10
Using a national survey, we sought to determine how hospital-based PTs participate in care transitions. The specific aims of our study were to examine: 1) how PTs communicate with patients and providers across care settings; and 2) potential barriers to participation in care transitions. We hypothesized care coordination between PTs across settings is highly infrequent, and acute care PTs would report care transition activities did not contribute to productivity standards required in their facilities.
METHODS
Survey and Participants
An electronic survey (Supplemental Digital Content 1) was developed by the first author (JRF) based on recommended practices for care transitions for typical hospitalized older adult patients.13–15 Questions regarding care communications, perceptions, and care transition activities used a 5-point Likert scale. We also solicited free text responses from therapists regarding the top 5 reasons they felt were associated with readmissions from their perspective. The survey was reviewed by two experienced PTs (KJR and DJM) to ensure face validity. The survey included questions regarding sociodemographic characteristics of survey respondents, as well as questions about working environment, care communications, and perceptions about care transition activities.
A convenience sample of 10 acute care PTs representing 3 US states participated in cognitive interviewing to validate the survey questions. Cognitive interviewing is the process by which survey respondents comprehend questions, retrieve relevant information, and develop survey responses.16 Therapists were asked to take the survey, and then give feedback about content, wording, and perceived value of the questions. The research team modified the survey questions and then formatted into sections regarding discharge planning activities, care communication across settings, perceptions of care transition activities, and perception of how care transition activities aligned with current productivity standards.
We distributed the survey to a cross-sectional convenience sample of members of the American Physical Therapy Association (APTA) who were also members of the Academy of Acute Care Physical Therapy (AACPT). The APTA is a professional organization representing more than 95,000 members. The AACPT is a sub-section of the APTA. Members of the AACPT have clinical, administrative, or research interests in acute care practice. Because we were interested in surveying active members of the AACPT, we used an electronic discussion board managed by AACPT to disseminate the survey targeting physical therapist members.
An invitation to participate in the survey and an electronic web link to the survey was posted on the AACPT electronic discussion board. The invitation contained information about the study and the contact information for the principal investigator. Four follow up solicitations were posted over the study period. The initial page of the survey contained information about the risks associated with the study; respondents who continued and answered any subsequent questions represented those who consented to participate. We used a commercial online survey administration platform (SurveyMonkey LLC, Palo Alto, California) to administer the questionnaire. Survey participants were solicited between February 2016 and April 2016. Respondents who only partially completed the survey are included in reported data. We used the Checklist for Reporting Results of Internet E-Surveys17 to guide reporting of findings from the study. The University of Colorado Multiple Institutional Review Board approved this study.
Data Analysis
All statistical analysis was conducted using SAS, version 9.4 (SAS Institute, Inc., Cary, NC). We used descriptive statistics to summarize the distribution of respondents’ responses. The key outcomes of interest were frequency of care transition activities performed and the frequency participants agreed these activities were considered productive time in their facilities.
RESULTS
There were 1409 subscribers to the AACPT electronic discussion board at the time of invitation to participate in the study. Thirty-one survey-related emails sent to discussion board subscribers were returned as undeliverable, and not counted in the total sample. There were 282 physical therapist respondents to the survey (21% response rate). Of these respondents, 18 only completed demographic information and were excluded from further analysis. Demographic information for the survey respondents is reported in Table 1. For reporting purposes, we use the term “routinely” in the text to describe activities respondents reported were done “Almost Always” or “Frequently”, and collapse the terms “Rarely” or “Almost Never” in the text as “rarely”. Similarly, “Strongly Agree” and “Agree” are collapsed as “agree” in the text, and “Disagree” and ‘Strongly Disagree” are collapsed as “disagree”. Free text results were not formally evaluated, but are presented in Supplemental Digital Content 2.
Table 1.
Demographics of Survey Respondents
| Characteristic | n (%) |
|---|---|
| Age, y, mean(SD) | 43.4 (10.6) |
| Female sex | 215 (82) |
| Highest educational level | |
| Certificate | 2 (1) |
| Bachelors | 48 (18) |
| Entry level Masters | 39 (15) |
| Advanced Masters | 22 (8) |
| Doctor of Physical Therapy (DPT) | 143 (54) |
| Advanced Doctorate (e.g. PhD, EdD) | 9 (3) |
| Physical therapy experience | |
| <1 to 3 years | 32 (12) |
| 4–9 years | 39 (15) |
| 10–19 years | 75 (29) |
| 20+ years | 116 (44) |
| Acute care experience | |
| Practiced in acute care within last 3 years | 260 (98) |
| <1 to 3 total years in setting | 36 (14) |
| 4–9 total years in setting | 59 (22) |
| 10–19 total years in setting | 85 (32) |
| 20+ total years in setting | 83 (32) |
| Practice environment | |
| Rural hospital | 58 (23) |
| Teaching hospital | 155 (63) |
| US Census Bureau geographic region | |
| Midwest | 54 (21) |
| Northeast | 48 (19) |
| South | 90 (35) |
| West | 64 (25) |
| Hospital size | |
| <100 beds | 29 (11) |
| 100–249 beds | 61 (24) |
| 250–500 beds | 90 (35) |
| 500+ beds | 77 (30) |
PT Participation in Discharge Planning and Care Transition Activities
Results are summarized in Table 2. Generally, communication between acute care PTs and other in-hospital healthcare providers occurred frequently. Of the respondents surveyed, more than 95% actively participated in discharge planning through routine provision of written discharge recommendations and recommendations for durable medical equipment (DME). Most respondents saw patients routinely on the day of discharge, but a majority did not prepare a formal discharge summary. Respondents were more likely to communicate patient discharge needs with a hospital case manager or social worker than with a treating physician.
Table 2.
Reported Discharge Planning and Care Transition Activities
| Survey Question, n(%) | Almost Always | Frequently | Sometimes | Rarely | Never |
|---|---|---|---|---|---|
| Actively participates in DC recommendations | 204 (81.6) | 41 (16.4) | 4(1.6) | 1(0.4) | 0 (0.0) |
| Provides a written DC location recommendation | 212 (85.8) | 21 (8.5) | 11 (4.5) | 1(0.4) | 2 (0.8) |
| Sees patients on the day of DC | 49 (19.7) | 99 (39.8) | 92 (37.0) | 8 (3.2) | 1 (0.4) |
| Writes a formal DC summary | 63 (25.3) | 27 (10.8) | 33 (13.3) | 63 (25.3) | 63 (25.3) |
| Communicates with MD regarding DC recommendation | 30 (12.0) | 60 (24.0) | 109 (43.6) | 49 (19.6) | 2 (0.8) |
| Communicates with DC planners regarding DC recommendation | 144 (57.6) | 84 (33.6) | 22 (8.8) | 0(0.0) | 0 (0.0) |
| Provides written DME recommendations | 185 (74.0) | 63 (25.2) | 2 (0.8) | 0(0.0) | 0 (0.0) |
| Follows up with patients about DME | 8 (3.2) | 19 (7.6) | 19 (7.6) | 72 (28.8) | 123 (49.2) |
| Gives contact information to patients at discharge | 25 (10.4) | 32 (13.3) | 57 (23.7) | 62 (25.7) | 65 (27.0) |
| For patients discharged with recommendation for post-acute rehabilitation (e.g. HH, SNF, IRF) | |||||
| Initiates verbal or electronic communication to provide patient information to PTs | 31 (13.1) | 31 (13.1) | 49 (20.8) | 51 (21.6) | 74 (31.4) |
| Initiates verbal or electronic communication to provide patient information to non-rehab staff | 39 (16.6) | 39 (16.6) | 37 (15.7) | 51 (21.7) | 69 (29.3) |
| Contacted by HH PTs about patients | 1 (0.4) | 8 (3.3) | 32 (13.3) | 95 (39.6) | 104 (43.3) |
| Contacted by SNF or IRF PTs about patients | 1 (0.4) | 6 (2.5) | 49 (20.4) | 106 (44.2) | 78 (32.5) |
| For patients discharged with recommendation for outpatient rehabilitation | |||||
| Makes referral to specific clinic | 7 (2.9) | 29 (12.2) | 51 (21.4) | 61 (25.6) | 90 (37.8) |
| Initiates verbal or electronic communication to provide patient information to PTs | 10 (4.2) | 24 (10.1) | 41 (17.2) | 69 (29.0) | 94 (39.5) |
| Initiates verbal or electronic communication to provide patient information to PCPs | 19 (7.9) | 25 (10.5) | 32 (13.5) | 63 (26.5) | 99 (41.6) |
| Follows up to determine if recommendation followed | 5 (2.1) | 0(0.0) | 6 (2.5) | 48 (20.2) | 179 (75.2) |
| Contacted by OP PTs about patients | 0 (0.0) | 4 (1.7) | 31 (12.9) | 86 (35.8) | 119 (49.6) |
| For patients discharged with no skilled rehabilitation needs | |||||
| Initiates verbal or electronic communication to provide patient information to PCPs | 15 (6.3) | 31 (13.1) | 26 (11.0) | 44(18.6) | 121 (51.0) |
| Contacted by patients or family members after hospital discharge | 1 (0.42) | 11 (4.6) | 29 (12.1) | 112(46.9) | 86 (36.0) |
| Contacted by primary care physicians after hospital discharge | 2 (0.8) | 1 (0.4) | 11(4.6) | 58 (24.2) | 168 (70.0) |
DC=Discharge, MD=Physician, DME=Durable Medical Equipment, PT=Physical Therapist, HH=home health, SNF=skilled nursing facility, IRF=inpatient rehabilitation facility, OP=outpatient, PCP=primary care physicians
Communication between in-hospital PTs and post-acute care providers was more infrequent. When asked about the processes for older adults transitioning out of the hospital to other rehabilitation settings, under one-third of respondents reported they routinely initiated communication with post-acute care facility therapists or other clinical staff. Nearly 96% of respondents reported requests for patient information were rarely initiated from post-acute care therapists (home health, skilled nursing, or inpatient rehab).
For patients discharged to outpatient management, the communication frequency was generally lower than for post-acute care settings. When respondents were asked about patients discharged with recommendations for outpatient physical therapy, a majority reported they rarely provided referrals to specific clinics, initiated communication with rehabilitation or primary care providers, or were contacted by outpatient providers about patient care needs.
Communication with patients after hospital discharge was rare. Just over 10% of respondents routinely asked patients if recommended DME was received after hospital discharge, and 2% routinely followed up with patients after discharge to see if recommendations for outpatient care were followed. More than half of respondents reported they rarely provided their contact information to patients at the time of discharge, and even fewer were contacted by caregivers or patients after discharge.
Perception of PT Value in Discharge Planning and Care Transitions
Results are reported in Table 3. Most respondents agreed they prepare patients adequately for discharge and 90% agreed there was a role for acute care PTs in identifying patients at risk and reducing hospital readmissions. A majority of respondents also agreed written evaluation and treatment notes they prepared had value to both rehabilitation and physician providers at the next level of care. Respondents were more uncertain whether the role and responsibility of acute care PTs extended to management of mobility deficits after patient discharge. Most respondents agreed their role in providing discharge recommendations was valued by hospital physicians.
Table 3.
Perceived Value of PTs and PT Communications in Care Transitions
| Survey Question, n(%) | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| I prepare patients adequately for DC | 62 (27.3) | 151 (66.5) | 12 (5.3) | 2(0.9) | 0 (0.0) |
| My DC recommendation valued by MDs | 100 (44.1) | 100 (44.1) | 20 (8.8) | 2 (0.9) | 0 (0.0) |
| Acute care evaluation has value to home health PTs | 68 (30.0) | 115 (50.7) | 32 (14.1) | 9 (4.0) | 3 (1.3) |
| Acute care treatment notes have value to home health PTs | 80 (35.2) | 126 (55.5) | 16 (7.1) | 4 (1.8) | 1 (0.4) |
| Acute care evaluation has value to SNF and IRF PTs | 74 (32.9) | 112 (49.8) | 26 (11.6) | 9 (4.0) | 4 (1.8) |
| Acute care PTs have role managing mobility deficits after DC | 30 (13.5) | 51 (23.0) | 78 (35.1) | 43 (19.4) | 20 (9.0) |
| Acute care PTs have role in reducing hospital readmissions | 97 (42.7) | 107 (47.1) | 21 (9.3) | 2 (0.9) | 0 (0.0) |
| Confident about identifying patients at risk for readmissions | 84 (37.1) | 120 (53.1) | 19 (8.4) | 3 (1.3) | 0 (0.0) |
| Confident that treatment notes are read by hospital MDs | 10 (4.4) | 33 (14.5) | 48 (21.1) | 96 (42.3) | 40 (17.6) |
| Confident that evaluation provided to PCPs | 14 (6.2) | 26 (11.5) | 24 (10.6) | 86 (37.9) | 77 (33.9) |
| Confident that treatment notes provided to PCPs | 12(5.3) | 23 (10.2) | 23 (10.2) | 86 (38.1) | 82 (36.3) |
| Confident that evaluation provided to post-acute PTs | 24 (10.8) | 70 (31.3) | 46 (20.6) | 60 (26.9) | 23 (10.3) |
| Confident that treatment notes provided to post-acute PTs | 17 (7.6) | 63 (28.1) | 56 (25.0) | 65 (29.0) | 23 (10.3) |
| Confident that evaluation is provided to outpatient PTs | 7 (3.1) | 25 (11.0) | 40 (17.6) | 98 (43.2) | 57 (25.1) |
| Confident that treatment notes provided to outpatient PTs | 8 (3.5) | 23 (10.1) | 40 (17.6) | 94 (41.4) | 62 (27.3) |
| PTs in my facility are involved in readmission reduction | 33 (14.9) | 70 (31.5) | 37 (16.7) | 46 (20.7) | 36 (16.2) |
| How often do you feel MDs review information you document about: | Almost Always | Frequently | Sometimes | Rarely | Never |
| Discharge recommendations | 59 (26.3) | 88 (39.3) | 58 (25.9) | 18 (8.0) | 1 (0.5) |
| Physical therapy outcome measures | 1 (0.5) | 21 (9.4) | 67 (30.0) | 91 (40.8) | 43 (19.3) |
| ADL status | 7 (3.1) | 55 (24.6) | 84 (37.5) | 62 (27.7) | 16 (7.1) |
| Trajectory of recovery | 8 (3.6) | 22 (9.9) | 88 (39.5) | 76 (34.1) | 29 (13.0) |
| Recommended DME | 28 (12.6) | 79 (35.4) | 78 (35.0) | 28 (12.6) | 10 (4.5) |
| Cognitive status | 8 (3.6) | 31 (13.9) | 92 (41.3) | 71 (31.8) | 21 (9.4) |
| Patient participation in therapy | 17 (7.6) | 52 (23.2) | 98 (43.8) | 49 (21.9) | 8 (3.6) |
| Confident MD discharge summaries include | |||||
| Discharge recommendations | 58 (25.8) | 83 (36.9) | 61 (27.1) | 16 (7.1) | 7 (3.1) |
| Physical therapy treatment outcomes | 3 (1.33) | 6 (2.7) | 31 (13.7) | 73 (32.3) | 113 (50.0) |
| ADL status | 5 (2.21) | 20 (8.9) | 66 (29.2) | 83 (36.7) | 52 (23.0) |
| Trajectory of recovery | 4 (1.8) | 30 (13.3) | 69 (30.5) | 77 (34.1) | 46 (20.4) |
| Recommended DME | 17 (7.5) | 41 (18.1) | 72 (31.9) | 55 (24.3) | 41 (18.1) |
| Cognitive status | 11 (4.9) | 54 (24.0) | 90 (40.0) | 48 (21.3) | 22 (9.8) |
| Patient participation in therapy | 5 (2.2) | 22 (9.8) | 71 (31.60 | 82 (36.4) | 45 (20.0) |
| Fall risk | 8 (3.5) | 33 (14.6) | 84 (37.2) | 76 (33.6) | 25 (11.0) |
DC=Discharge, MD=Physician, DME=Durable Medical Equipment, PT=Physical Therapist, SNF=skilled nursing facility, IRF=inpatient rehabilitation facility, OP=outpatient, PCP=primary care physicians, ADL=activities of daily living
Respondents reported greater uncertainty about whether clinical information documented was routinely reviewed by hospital physicians. Most respondents did not generally agree outcome measures generated by physical therapists were routinely reviewed by hospital physicians. However, a majority of respondents agreed PTs recommendations for discharge location were routinely reviewed. Participants reported mixed agreement and disagreement as to whether physicians routinely reviewed PT-generated information, such as DME recommendations.
When asked if they believed evaluation and treatment notes were provided to providers outside the hospital after patient discharges, most respondents disagreed notes were routinely provided to primary care physicians or outpatient providers. Nearly half of respondents disagreed these documents were routinely provided to any post-acute care providers in home health, skilled nursing, or inpatient rehabilitation facility settings (Table 3).
Barriers to Effective PT Participation in Care Transitions
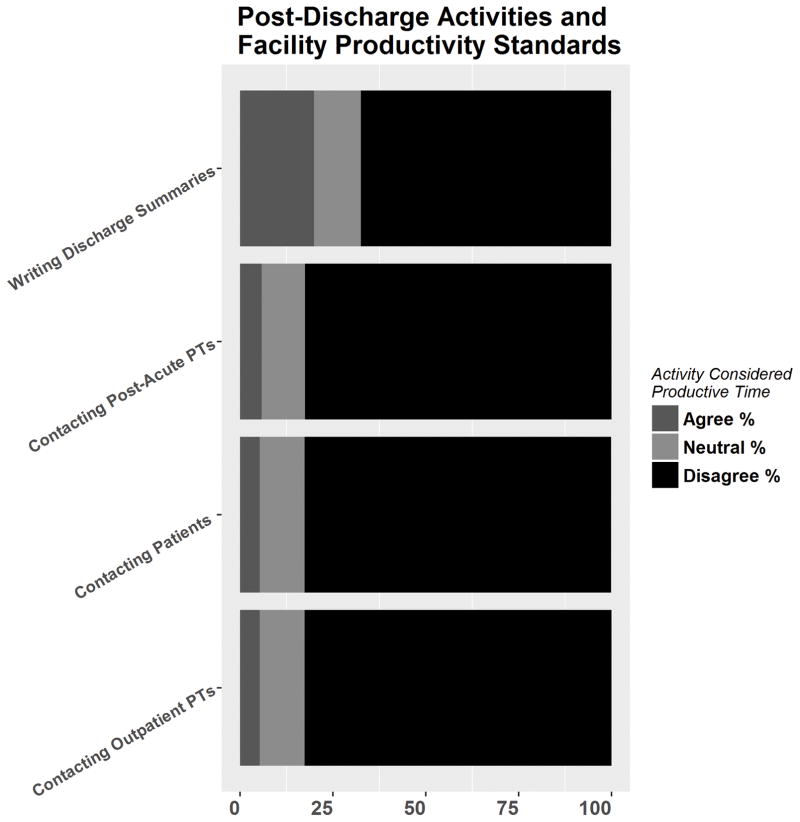
Less than half of therapists agreed PTs in their facilities were involved in readmission reduction efforts as part of a formal hospital committee or task force. Productivity standards were also identified as a potential barrier. While the definition of productivity varies slightly across facilities, it refers, in this context, to activities hospital administrators define as meaningful uses of therapist time. For example, these activities may be defined in some facilities as billable units, and in others as “hands-on” time with patients. In our study, therapists reported the average facility productivity standard was 68% of their day; though how this was defined varied substantially. Most respondents disagreed their facilities would consider contacting patients or other PTs in different settings as activities counting toward hospital productivity standards; similarly, a majority of respondents disagreed that preparing physical therapy discharge summaries for patients would be considered productive time within their facilities (Figure 1).
Figure 1. Productivity of Care Transition Activities for Hospital-Based Physical Therapists.
Figure 1 demonstrates how frequently physical therapists agreed that the listed care transition activities would count towards productivity standards within their hospital facilities. Darker shading indicates a greater level of disagreement that these activites were productive time.
DISCUSSION
The results of our survey suggest acute care PTs are highly involved in discharge planning, including recommendations of discharge location and DME needs. These findings are consistent with previous research on acute care physical therapy practice.18–20 Our study suggests communication about impairments in bodily function and activity limitations is often limited across care settings; this suggests valuable information may be lost during care transitions. Because of strong relationships between impairments in bodily function, activity limitation, participation restriction, and adverse health outcomes after hospitalization,8,9,11,21 these communication breakdowns are concerning because critical information may not reach providers managing patients after hospital discharge. This may limit opportunities to alter the trajectory of disability commonly observed after hospital discharge,22 and perhaps leave patients vulnerable to higher rates of hospital readmission and death.23
The findings in our study related to care handoffs are in stark contrast to best practices in care transitions supported by Agency for Healthcare Research and Quality (AHRQ) recommendations and Joint Commission guidelines. The AHRQ describes care coordination as “deliberately organizing patient care activities and sharing information among all of the participants concerned with a patient’s care to achieve safer and more effective care.” 24 The Joint Commission similarly suggests clinicians should be actively involved in all steps of the care transition, and should participate in timely follow up with patients to ensure adequate resources and knowledge are available to carry out care plans.25
Based on these guidelines, we feel it is concerning so many therapists feel their facilities would not support many care transition activities as productive time, in spite of evidence suggesting these communications may contribute to improved patient outcomes.6,12 A lack of communication about impairments in a patient’s bodily function is perhaps most notable when considering patients who are discharged to home health or outpatient rehabilitation settings. Medicare statutory guidelines allow for periods of 48 hours between hospital discharge and initiation of home health services, and no guidelines exist for outpatient providers seeing patients after hospitalization. Because any decline in physical function during or after hospitalization increases risk of hospital readmission, nursing home admission, or death,23,26,27 timely communication about patients at high risk is especially critical.
The paucity of formal written discharge summaries written in the acute care settings is an unanticipated finding of this study. The American Physical Therapy Association guidelines for clinical documentation recommend therapists complete discharge summaries at the end of each physical therapy episode of care to summarize progress towards goals and plan for further care.28 Yet, in our study, less than half of therapists routinely write a discharge summary. The reasons for this are not clear from the findings, but we posit many therapists may treat each individual visit as a reassessment in acute care and thus include more thorough documentation in each visit note about progress towards goals and discharge recommendations. Writing discharge summaries also was not considered productive time for many of the survey respondents which may further disincentive preparing these documents. This may be an area of future study.
Less than half of respondents reported they were actively involved in readmission reduction programs at their hospital facilities, though nearly all felt acute-care PTs have a role in reducing hospital readmissions. This gap may represent an opportunity for hospital-based PTs to increase involvement in hospital readmission reduction efforts and contribute to development of standardized processes which improve communications about physical function and rehabilitation plans of care across care settings.10
A future direction from this work should be a careful examination of how to align physical therapy productivity standards in hospital settings with best practices for care coordination. Most currently used measures of hospital-based therapist productivity assess primarily the amount of time PTs spend directly delivering interventions to hospitalized patients.
The AACPT Position Statement on Value vs Productivity Measurement in Acute Care Physical Therapy notes:
Productivity, when measured solely as a percentage of daily staff time engaged in direct interventions, holds little value for the stakeholders of physical therapist services. Focusing on these specific interventions may actually impede the physical therapist’s ability to meet the goals of the patients/clients, families, significant others, and caregivers, the healthcare system and society29
The findings of our study suggest current productivity standards for PTs often do not credit care coordination activities shown to be valuable.13,15,30 We feel facilities which do not value therapist time spent in care coordination are not only failing to modify care delivery to meet the best evidence, but potentially increasing risk of adverse outcomes for their patients. New ways to assess productivity take into account the value of verbal and written communications with other providers, patients, and caregivers both within and across care settings are needed.
Limitations
The main limitation of our study is selection bias which may reduce generalizability of our findings. Surveying only AACPT members who are active participants in the discussion board may not have accurately represented acute care physical therapy community, as this sample may have been more motivated to participate or be more engaged with evidence based practice than non-participants. Also, this study of acute care physical therapists only represents their perceptions about patients they see, and not hospital populations in general.
With a response rate of 21%, there is a potential lack of generalizability in the survey results across acute care PTs representing the AACPT. However, this response rate is likely conservative, given the survey targeted only PTs, and physical therapist assistants also participate in the discussion board but the respective numbers of PTs vs assistants were unable to be ascertained accurately from the discussion board administrators. We were also underpowered to determine whether survey responses differed across key demographic or hospital characteristics, which may be a fruitful area for future research. In addition, previous research soliciting participants using an electronic discussion board managed by the AACPT was conducted in this manner with a similar response rate.31 Lastly, because hospital PTs often use shared computers, individual IP addresses were allowed to submit multiple surveys raising the possibility respondents could have completed multiple surveys. However, analysis of the results did not reveal any identical entries.
CONCLUSIONS
The overall results of our survey suggest there are gaps in communication between PTs across care settings when managing older adults after acute hospitalization. These gaps, when considered in combination with other documented gaps in communication surrounding impairments in bodily function and activity limitations,6 may contribute to increased hospital readmission rates. Physical therapist communication breakdowns across care settings appear to be exacerbated by facility regulations on what is considered productive time in acute care facilities; notably, many communication and handoff procedures recommended by consensus guidelines24,25 are considered unproductive time. Future research should identify the extent to which these gaps are modifiable, design quality improvement initiatives including both physicians and physical therapists as stakeholders, and measure the resultant impact on patient and facility outcomes.
Supplementary Material
Acknowledgments
Grant Funding: This work was supported by a Promotion of Doctoral Studies II Scholarship from the Foundation for Physical Therapy, the National Institute on Aging T32AG000279-15 & F31AG056069, and a research grant from the Health Policy and Administration Section of the American Physical Therapy Association.
Footnotes
Conflicts of Interest: Jason Falvey and Kyle Ridgeway receive royalty payments from Medbridge Education for development of continuing education coursework on hospital readmissions.
References
- 1.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 2.Witherington E, Pirzada O, Avery A. Communication gaps and readmissions to hospital for patients aged 75 years and older: observational study. Qual Saf Health Care. 2008;17(1):71–75. doi: 10.1136/qshc.2006.020842. [DOI] [PubMed] [Google Scholar]
- 3.Roy CL, Kachalia A, Woolf S, et al. Hospital readmissions: physician awareness and communication practices. J Gen Intern Med. 2009;24(3):374–380. doi: 10.1007/s11606-008-0848-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradley EH, Curry L, Horwitz LI, et al. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. J Am Coll Cardiol. 2012;60(7):607–614. doi: 10.1016/j.jacc.2012.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradley EH, Sipsma H, Horwitz LI, et al. Hospital strategy uptake and reductions in unplanned readmission rates for patients with heart failure: a prospective study. J Gen Intern Med. 2015;30(5):605–611. doi: 10.1007/s11606-014-3105-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polnaszek B, Mirr J, Roiland R, et al. Omission of physical therapy recommendations for high-risk patients transitioning from the hospital to subacute care facilities. Arch Phys Med Rehabil. 2015;96(11):1966–1972. e1963. doi: 10.1016/j.apmr.2015.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher SR, Kuo Y-F, Sharma G, et al. Mobility after hospital discharge as a marker for 30-day readmission. J Gerontol A Biol Sci Med Sci. 2012;68(7):805–810. doi: 10.1093/gerona/gls252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DePalma G, Xu H, Covinsky KE, et al. Hospital readmission among older adults who return home with unmet need for ADL disability. Gerontologist. 2013;53(3):454–461. doi: 10.1093/geront/gns103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen HQ, Chu L, Amy Liu I-L, et al. Associations between physical activity and 30-day readmission risk in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11(5):695–705. doi: 10.1513/AnnalsATS.201401-017OC. [DOI] [PubMed] [Google Scholar]
- 10.Falvey JR, Burke RE, Malone D, et al. Role of physical therapists in reducing hospital readmissions: Optimizing outcomes for older adults during care transitions from hospital to community. Phys Ther. 2016;96(8):1125–1134. doi: 10.2522/ptj.20150526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greysen SR, Cenzer IS, Auerbach AD, et al. Functional impairment and hospital readmission in Medicare seniors. JAMA intern med. 2015;175(4):559–565. doi: 10.1001/jamainternmed.2014.7756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kadivar Z, English A, Marx BD. Understanding the relationship between physical therapy participation in interdisciplinary rounds and hospital readmission rates: A preliminary study. Phys Ther. 2016;96(11):1705–1713. doi: 10.2522/ptj.20150243. [DOI] [PubMed] [Google Scholar]
- 13.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 14.Burke RE, Kripalani S, Vasilevskis EE, et al. Moving beyond readmission penalties: creating an ideal process to improve transitional care. J Hosp Med. 2013;8(2):102–109. doi: 10.1002/jhm.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radwin LE, Castonguay D, Keenan CB, et al. An expanded theoretical framework of care coordination across transitions in care settings. J Nurs Care Qual. 2016;31(3):269–274. doi: 10.1097/NCQ.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 16.Willis GB. Cognitive interviewing and questionnaire design: a training manual. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 1994. [Google Scholar]
- 17.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES) J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jette DU, Grover L, Keck CP. A qualitative study of clinical decision making in recommending discharge placement from the acute care setting. Phys Ther. 2003;83(3):224–236. [PubMed] [Google Scholar]
- 19.Jette DU, Brown R, Collette N, et al. Physical therapists’ management of patients in the acute care setting: an observational study. Phys Ther. 2009;89(11):1158–81. doi: 10.2522/ptj.20080338. [DOI] [PubMed] [Google Scholar]
- 20.Masley PM, Havrilko C-L, Mahnensmith MR, et al. Physical therapist practice in the acute care setting: a qualitative study. Phys Ther. 2011;91(6):906–919. doi: 10.2522/ptj.20100296. [DOI] [PubMed] [Google Scholar]
- 21.Burke RE, Whitfield EA, Hittle D, et al. Hospital readmission from post-acute care facilities: risk factors, timing, and outcomes. J Am Med Dir Assoc. 2016;17(3):249–255. doi: 10.1016/j.jamda.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gill TM, Allore HG, Gahbauer EA, et al. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304(17):1919–1928. doi: 10.1001/jama.2010.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Volpato S, Cavalieri M, Sioulis F, et al. Predictive value of the Short Physical Performance Battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011;66(1):89–96. doi: 10.1093/gerona/glq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality. Improving primary care practice: care coordination. Retrieved December 1st, 2016 from http://www.ahrq.gov/professionals/prevention-chronic-care/improve/index.html.
- 25.The Joint Commission. Transitions of care portal. Retrieved December 3rd, 2016 from https://www.jointcommission.org/assets/1/18/Hot_Topics_Transitions_of_Care.pDf.evention-chronic-care/improve/index.html.
- 26.Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171–2179. doi: 10.1111/j.1532-5415.2008.02023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rudberg MA, Sager MA, Zhang J. Risk factors for nursing home use after hospitalization for medical illness. J Gerontol A Biol Sci Med Sci. 1996;51(5):M189–M194. doi: 10.1093/gerona/51a.5.m189. [DOI] [PubMed] [Google Scholar]
- 28.American Physical Therapy Association. Physical therapy documentation of patient/client management (BOD G03-05-16-41) Retrieved November 28th, 2017 from http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Practice/DocumentationPatientClientManagement.pdf.
- 29.Academy of Acute Care Physical Therapy. Position statement on value vs. productivity measurement in acute care physical therapy. Retrieved February 2nd, 2017 from http://c.ymcdn.com/sites/acutept.siteym.com/resource/resmgr/Files/2014-11_Productivity_Value_B.pdf.
- 30.Jones CD, Vu MB, O’Donnell CM, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417–424. doi: 10.1007/s11606-014-3056-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olkowski BF, Stolfi AM. Safe patient handling perceptions and practices: a survey of acute care physical therapists. Phys Ther. 2014;94(5):682–695. doi: 10.2522/ptj.20120539. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.