Foot-and-mouth disease (FMD) is a viral disease of livestock with substantial impact on agricultural production and subsistence farming on a global scale. Control of FMD is impeded by the existence of a prolonged asymptomatic carrier phase during which infected cattle shed low quantities of infectious virus in oropharyngeal fluid (OPF) for months to years after infection. The epidemiological significance of FMD virus (FMDV) carriers is unresolved. However, the existence of the FMDV carrier state has substantial impact on international trade in animal products. The current investigation demonstrated that transfer of OPF from persistently infected FMDV carrier cattle to naive cattle led to fulminant clinical FMD. It was thus demonstrated that, although the risk for disease transmission under natural conditions is considered to be low, there is detectable contagion associated with FMDV carrier cattle. This finding is important for optimization of FMD risk mitigation strategies.
KEYWORDS: FMDV, carrier, cow, foot-and-mouth disease, foot-and-mouth disease virus, risk, transmission, virus
ABSTRACT
Control and eradication of foot-and-mouth disease (FMD) are impeded by the existence of a persistent, subclinical phase of infection in ruminants; animals with this status are referred to as carriers. However, the epidemiological significance of these FMD virus (FMDV) carriers is uncertain. In the current investigation, the contagion associated with FMDV carrier cattle was investigated by exposure of susceptible cattle and pigs to oropharyngeal fluid (OPF) samples or tissues harvested from persistently infected cattle. Naive cattle were inoculated through intranasopharyngeal deposition of unprocessed OPF samples that had been collected from FMDV carriers at 30 days postinfection. These inoculated cattle developed clinical FMD, and the severity of disease they developed was similar to that of animals that had been infected with a high-titer inoculum. In contrast, pigs exposed via intraoropharyngeal inoculation of the same OPF samples or via ingestion of nasopharyngeal tissues harvested from the same cohort of persistently infected cattle did not develop FMD. These findings indicate that there is demonstrable contagion associated with FMDV carrier cattle despite the lack of evidence for transmission by direct contact. The findings presented herein provide novel information that should be considered for FMD risk mitigation strategies.
IMPORTANCE Foot-and-mouth disease (FMD) is a viral disease of livestock with substantial impact on agricultural production and subsistence farming on a global scale. Control of FMD is impeded by the existence of a prolonged asymptomatic carrier phase during which infected cattle shed low quantities of infectious virus in oropharyngeal fluid (OPF) for months to years after infection. The epidemiological significance of FMD virus (FMDV) carriers is unresolved. However, the existence of the FMDV carrier state has substantial impact on international trade in animal products. The current investigation demonstrated that transfer of OPF from persistently infected FMDV carrier cattle to naive cattle led to fulminant clinical FMD. It was thus demonstrated that, although the risk for disease transmission under natural conditions is considered to be low, there is detectable contagion associated with FMDV carrier cattle. This finding is important for optimization of FMD risk mitigation strategies.
INTRODUCTION
Foot-and-mouth disease (FMD), caused by infection with FMD virus (FMDV; family Picornaviridae, genus Aphthovirus), is an economically important disease of livestock (1, 2). Large regions of the developed world, including Europe, North America, and Australia, are kept free of FMD through strict regulations on the importation of animals and related products. However, the disease is still endemic in most of Africa and Asia (3–5). FMDV can infect a wide range of cloven-hoofed animals and can cause severe disease in domestic ruminants and pigs (6, 7). The endemic presence of FMD is problematic, as it prevents access to international markets for trade in animal products. Additionally, measures required for disease control, including repeated vaccination campaigns and control of animal movements, are economically and logistically challenging in many affected regions. In countries that are normally free of FMD, incursions of the disease cause major disruptions in agricultural production and severe losses in revenue due to interrupted trade (8–11). Control and eradication of FMD are further impeded by the existence of a subclinical persistent phase of infection in ruminant species (7, 12). This FMDV carrier state has traditionally been defined by detection of infectious FMDV in oropharyngeal fluid (OPF) more than 28 days postinfection (dpi), and it is reported to occur in ≥50% of infected cattle (12). However, recent work has demonstrated that carriers may be identified as early as 15 dpi in vaccinated cattle and 21 dpi in cattle that were not vaccinated (13). Persistent FMDV infection occurs in both vaccinated and naive cattle, regardless of the occurrence of clinical disease (14, 15). This is of particular concern in relation to the use of emergency vaccination to control FMD outbreaks in regions that are normally free of FMD, as infection in vaccinated animals may go unnoticed.
Cattle are highly sensitive to FMDV infection via the respiratory route, and the site of initial virus replication has been localized to specific regions of epithelium of the nasopharyngeal mucosa that contain mucosa-associated lymphoid tissue (MALT) (16–18). The clinical phase of disease includes fever, transient viremia, and the occurrence of characteristic vesicular lesions in and around the mouth, on the feet, and in other areas of nonhaired skin (1). Affected animals may develop severe lameness; in addition, both milk yield and growth rates may be reduced. Mortality rates are low in adult animals, which generally recover from the clinical phase of FMD within approximately 2 weeks. Persistent FMDV infection in cattle has, similar to early infection, also been localized to lymphoid-associated epithelium of the nasopharynx (13, 19). During the persistent phase of infection, FMDV can be detected in nasopharyngeal tissues and in OPF sampled using a probang (sputum) cup (20), but it is usually not detected in oral or nasal swab samples (13, 21, 22).
The existence of the FMDV carrier state has had a profound impact upon legislation concerning international trade in animal products (6, 23). However, there is still uncertainty regarding the actual level of risk associated with FMDV carriers as well as their potential role in the ecology of FMDV in regions where FMD is endemic (24, 25). Historical records have reported FMD outbreaks that were believed to have been seeded by transmission of FMDV from a persistently infected carrier to a susceptible animal (14, 24). However, multiple, small-scale, experimental investigations have failed to demonstrate transmission of FMDV from persistently infected carrier cattle to contact-exposed sentinels (22, 26, 27). A meta-analysis of experimental attempts to transmit FMDV from carrier cattle to naive cattle or pigs demonstrated that transmission had occurred only once among 26 published attempts (28). The original record from that transmission study reported confirmed seroconversion, without clinical signs of FMD, in two pigs after 75 days of contact exposure to carrier cattle (29). It has been speculated that the apparent lack of contagion associated with FMDV carrier cattle may be due to neutralization of virus shed in OPF by secreted anti-FMDV IgA. This theory is supported by a demonstrated increase in infectivity in tissue culture of OPF samples that have been treated with a fluorocarbon compound to dissociate immunoglobulin-bound virus (13, 30). There is experimental evidence that supports transmission from persistently infected African buffalo (Syncerus caffer) to in-contact cattle (31, 32). Additionally, in an experimental investigation from 1968, it was shown that it is possible to infect naive cattle by intrapharyngeal inoculation of OPF samples harvested from FMDV carriers (33). However, the published details of the experiment lack explicit details.
The objective of this current study was to investigate the infectivity of unprocessed OPF samples and pharyngeal tissues harvested from persistently infected FMDV carriers. For this purpose, naive calves and pigs were exposed to OPF samples harvested from FMDV carriers using simulated-natural inoculation systems. Additionally, samples of nasopharyngeal mucosal tissues harvested from the same cohort of FMDV carriers were macerated and fed to naive pigs. The findings presented herein demonstrate that OPF from FMDV carrier cattle is indeed infectious and may, under specific conditions, cause disease in susceptible cattle. Lack of disease in exposed pigs is consistent with previous reports (34) suggesting that higher quantities of virus may be required to infect pigs with FMDV via natural exposure routes.
RESULTS
Animal experiments.
The experiments reported herein consisted of three distinct phases. Phase I included nine steers that were infected with a high-titer FMDV inoculum and monitored to the persistent phase of infection. Experimental phase II consisted of eight steers that were challenged by intranasopharyngeal inoculation of oropharyngeal fluid (OPF) samples that had been harvested from the persistently infected steers of phase I at 30 days postinfection (dpi). Phase III consisted of two groups of five pigs; one group was challenged by intraoropharyngeal inoculation of the pooled OPF obtained from the phase I cattle, and the other group was fed macerated nasopharyngeal tissues from the same persistently infected cattle.
Clinical progression and infection dynamics in phase I cattle.
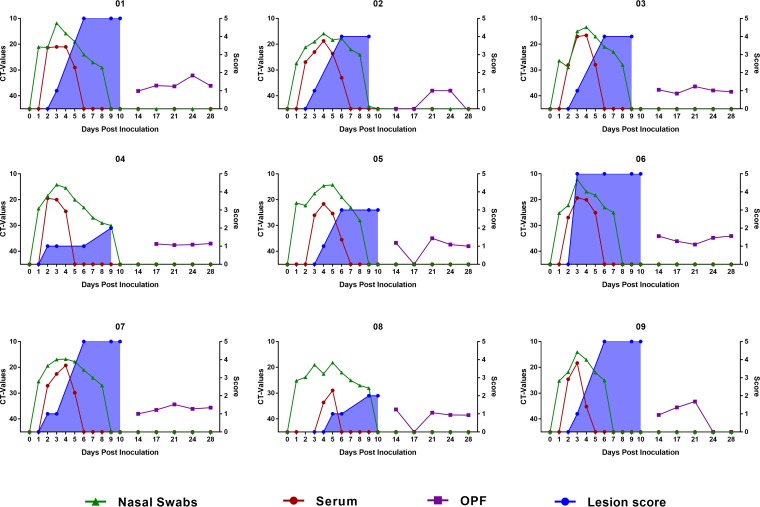
The main purpose of the first phase of the experiment was to produce carrier cattle and harvest appropriate material for inoculation of cattle and pigs in phases II and III. Following intranasopharyngeal (INP) deposition of FMDV A24 Cruzeiro, all nine animals in phase I of the study developed clinical FMD, consistent with previous investigations using the same virus strain, dose, and exposure route (13, 18, 35). Vesicular lesions were observed in the mouth as well as on one or more feet of all animals, with initial detection of lesions occurring between 3 to 6 dpi (Fig. 1). Four animals in phase I reached the maximum lesion score, with lesions in the mouth and on all four feet. The remaining five animals had one or more feet without lesions (Fig. 1). Viremia, defined as detection of FMDV RNA in serum, was apparent in all nine animals and lasted for 2 to 5 days. Abundant quantities of FMDV RNA were detected in nasal fluids throughout the clinical phase of infection. Nasal FMDV detection ceased between 7 and 10 dpi. Low quantities of FMDV RNA were detected in at least two OPF samples in all animals. However, two animals (animals 02 and 09) had two or more FMDV RNA-negative OPF samples, including the sample harvested at 28 dpi (Fig. 1). Therefore, OPF from these two animals was not included in the pooled inoculum that was harvested at 30 dpi and used for challenge of animals in phase II. The persistently infected animals of phase I were euthanized for tissue harvest at 31 dpi.
FIG 1.
FMDV infection dynamics in cattle in phase I of the study. Detection of FMDV RNA by RT-qPCR in nasal swabs and serum and oropharyngeal fluid (OPF) samples collected from cattle infected with 105 TCID50 of FMDV A24 Cruzeiro following intranasopharyngeal inoculation. Time (in days postinoculation) is shown on the x axes, CT values are shown on the left-hand y axes, and lesion scores are shown on the right-hand y axes. The blue shaded area represents cumulative lesion score, which was recorded up to 10 days postinfection (dpi). OPF was collected twice weekly from 14 dpi. Pooled OPF used for challenge of cattle in experimental phase II and pigs in phase III was harvested at 30 dpi, from all animals except animals 02 and 09 (the FMDV carrier status of these two animals was undetermined).
Infectivity of OPF inoculum and pooled tissue macerate.
The titer of FMDV in the unprocessed, pooled OPF (i.e., the material that was used to challenge cattle and pigs in phases II and III, respectively) was 101 50% tissue culture infectious doses (TCID50) per ml on LFBK-αvβ6 cells and below the detection level on BHK-21 cells (Table 1). Trichlorotrifluoroethane (TTE) treatment of the OPF increased the titer to 102.5 TCID50/ml on LFBK-αvβ6 cells, but the infectivity was still below the detection limit when using BHK-21 cells (Table 1). All titrations of the nasopharyngeal tissue macerate were below detection limits for both cell lines. However, infectious virus was isolated when a higher volume (1 ml) of the same tissue macerate was inoculated onto LFBK-αvβ6 cells in unfiltered form (Table 1). Calculating the challenge doses using the titer of the non-TTE-treated OPF derived from the highly sensitive LFBK-αvβ6 cells indicated that cattle in phase II received a dose of 102 TCID50, and the pigs in phase III that were challenged by intraoropharyngeal (IOP) inoculation received 5 × 101 TCID50.
TABLE 1.
FMDV detection in pooled OPF and nasopharyngeal tissues from persistently infected carriers
| Sample | CT value by FMDV RT-qPCR | FMDV isolation in LFBK-αvβ6 cellsa ,b | FMDV titer (TCID50/ml) inb
: |
|||
|---|---|---|---|---|---|---|
| BHK-21 cells |
LFBK-αvβ6 cells |
|||||
| Unprocessed | TTE-treated | Unprocessed | TTE-treated | |||
| OPF | 31.8 | Pos | Neg | Neg | 101 | 102.5 |
| Tissue | 32.0 | Pos | Neg | Neg | Neg | Neg |
Virus isolation on LFBK-αvβ6 cells in T25 flask using unprocessed and unfiltered material.
Pos, positive (observed cytopathic effect [CPE] with FMDV replication confirmed by RT-qPCR); Neg, negative.
Clinical progression and infection dynamics in phase II cattle.
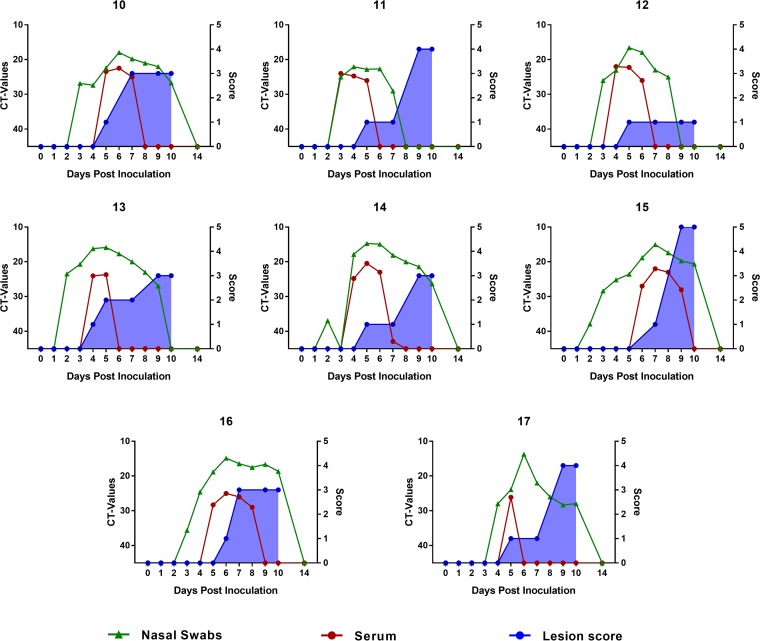
The second phase of the experiment included eight cattle that were challenged by INP deposition of 10 ml of pooled OPF that had been harvested at 30 dpi from seven phase I animals that had been identified as being persistently infected carriers. The first sign of FMD in the phase II cohort consisted of a large vesicle on the tongue of animal 13 at 4 dpi (Fig. 2). On the subsequent day, an interdigital cleft lesion was detected in this same animal, and oral vesicles were observed in five additional animals (Fig. 2). The remaining two cattle had developed oral lesions by day 6 and 7, respectively. Seven out of the eight animals developed lesions on one or more feet subsequent to the initial oral lesions. All animals became viremic, although FMDV RNA was detected in only one serum sample from animal 17. High quantities of FMDV RNA were detected in nasal secretions from all eight cattle starting from 2 to 4 dpi until 7 to 10 dpi (Fig. 2). The severity and progression of clinical FMD were similar to those observed in phase I cattle.
FIG 2.
FMDV infection dynamics in cattle in phase II of the study. Detection of FMDV RNA by RT-qPCR in nasal swabs and serum samples in cattle infected through intranasopharyngeal inoculation of pooled OPF obtained from cattle in experimental phase I at 30 dpi. The blue shaded area represents cumulative lesion score, which was recorded up to 10 days postinfection (dpi). The challenge dose was determined to have been 102 TCID50 per animal.
Clinical monitoring and infection dynamics in phase III pigs.
The pigs in the third phase of the study were challenged by either intraoropharyngeal deposition (n = 5) of the same pooled OPF as was used to challenge cattle in phase II or by feeding macerated nasopharyngeal tissues (n = 5) harvested from the persistently infected carriers of phase I at 31 dpi. There were no signs of FMD in any of the pigs included in the third phase of the experiment. Similarly, FMDV RNA was not detected in any oropharyngeal (OP) swabs or serum samples (not shown), and no antibodies against FMDV were detected in sera from each of these pigs collected at 14 dpi (not shown).
FMDV sequence analysis.
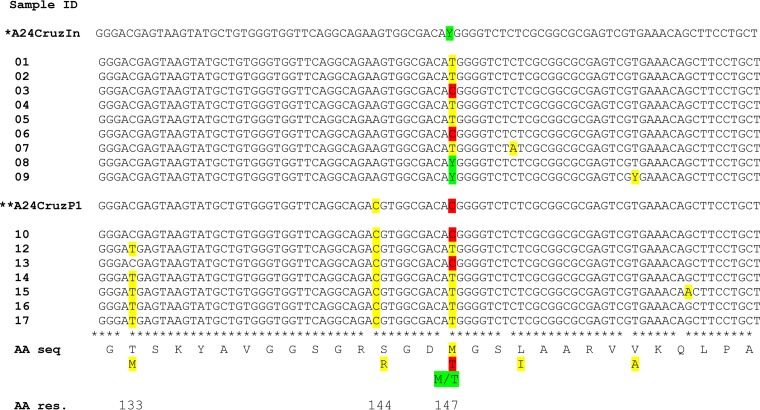
In order to assess the region specificity of genomic changes during the course of these studies, near-complete FMDV genome sequences were acquired from the original virus inoculum, as well as from nasal swab samples obtained during the clinical phase of infection from one calf from experimental phase I and from one calf from phase II (not shown). The majority of the observed changes within the genome occurred within the VP1 coding region. On this basis, further genomic analysis was focused upon the VP1-2A coding sequence in FMDV RNA derived from nasal swab samples from all animals in phase I and almost all animals from phase II (not including one animal). Samples for sequence analysis ranged from 3 to 4 dpi for phase I and 6 to 7 dpi for phase II. Specific samples were selected based on the presence of high levels of FMDV RNA (as judged by a low threshold cycle [CT] value in real-time quantitative PCR [RT-qPCR] assays) and corresponded to the peak of clinical FMD for both phase I animals and phase II animals. Nonsynonymous changes in the coding sequence were found predominantly at amino acid residues 133, 144, and 147 (Fig. 3) of VP1 which includes the integrin-binding motif (RGD) within the G-H loop. While the original inoculum and all phase I samples included amino acid sequences RSGDM or RSGDT at this site, all samples from the phase II animals were either RRGDM or RRGDT (Fig. 3). Due to low RNA content, it was not possible to obtain the VP1 coding sequence from the pooled OPF inoculum used for challenge of phase II cattle without one passage of the virus in tissue culture. However, the passaged phase II inoculum had a sequence encoding RRGDT at the specified site, indicating that the S-to-R substitution at residue 144 had occurred during the later stages of infection of the phase I cattle. Additionally, the sequences obtained from the phase II samples suggested that infection of this group was seeded by at least two major viral variants; one with methionine (M) at residues 133 and 147 and another with threonine (T) at both of these sites. The two variants at residue 147 had been present in different cattle in phase I. This suggested that virus from at least two different cattle from phase I initiated infection in phase II.
FIG 3.
Nucleotide sequences encoding part of the VP1 capsid protein of FMDVs derived from infected cattle in phase I and phase II of the study. Partial VP1 coding sequence obtained from nasal swab samples collected during the clinical phase of FMD from cattle of experimental phases I (animal identifiers [IDs] 01 to 09) at 3 or 4 dpi and phase II (animal IDs 10 to 17) at 6 or 7 dpi. The top row (*A24CruzIn for A24 Cruzeiro given INP) represents the consensus sequence of the inoculum used to infect cattle in phase I. The middle row (**A24CruzP1) is the consensus sequence of the pooled OPF inoculum (as determined after a single passage in cell culture; see text) that was used to infect cattle in phase II. Nucleotide changes and the corresponding amino acid substitutions are marked using the same color code. The variations in coding sequence suggest that the inoculums used for both phase I and II consisted of heterogeneous viral populations. Additionally, the sequences obtained from phase II animals suggest that infection of this group of animals was seeded by at least two different virus populations, as the samples from animals 10 and 13 are distinct from the remaining samples at amino acid residues 133 and 147 of VP1. Y = mixture of C and T (pyrimidines). AA seq, amino acid sequence; AA res., amino acid residue.
DISCUSSION
Although the FMDV carrier state was first described in cattle almost 60 years ago (36), the epidemiological significance of FMDV carriers remains undetermined and controversial. Although numerous reports have characterized the carrier state under natural and laboratory conditions, the crucial issue of whether carrier cattle pose a significant risk of contagion remains incompletely resolved. Despite a lack of substantiated experimental evidence of transmission from FMDV carrier cattle (28), the FMDV carrier state has had an impact upon the regulation of global trade in animal products (24, 37). The objective of this current investigation was to use recent knowledge about the initial and persistent sites of virus replication (13, 18) to investigate the potential risk of disease transmission associated with biological materials (OPF samples and tissues) from persistently infected FMDV carrier cattle.
Although the manner of transfer of OPF samples to naive cattle used herein could not occur under natural conditions, the finding of transmission of FMD from unprocessed OPF samples from carrier cattle indicates that the potential risk of disease outbreaks being initiated from these animals is real and cannot be discounted. Naive cattle and pigs were exposed to OPF samples from persistently infected carriers via direct intranasopharyngeal (INP) (cattle) or intraoropharyngeal (IOP) (pigs) deposition. These challenge systems have been developed to simulate natural, species-specific, exposure conditions while maintaining control of the dose and timing of virus challenge (38, 39). These challenge systems are needle-free inoculation systems that do not breach the mucosal barrier but rely on natural mechanisms of virus entry into susceptible cells at the documented primary infection sites. Additionally, one group of pigs was fed nasopharyngeal tissues from FMDV carriers to test the hypothesis that feeding pigs offal from persistently infected animals may constitute a risk for initiation of FMD outbreaks.
Titrations of the pooled OPF on highly sensitive LFBK-αvβ6 cells suggested that the INP-challenged cattle had each received a total dose of 102 TCID50, whereas the IOP-challenged pigs had each received a dose of 5 × 101 TCID50. However, the infectivity of the pooled OPF was below the detection limit when titration was attempted using the cell line most commonly used for isolation of FMDV (BHK-21 cells). The small (twofold) difference in inoculation dose between cattle and pigs was purely a practical consequence of not being able to deposit a larger volume of fluid onto the porcine tonsil of the soft palate. It was not possible to measure an infectivity titer in the macerated tissue that was fed to the pigs in experimental phase III. However, RT-qPCR analysis and successful virus isolation on LFBK-αvβ6 cells indicated the presence of low quantities of infectious FMDV in this material.
Viral sequence analysis was utilized to determine whether multiple animals had been infected by the phase II inoculum, as opposed to a single animal being infected by inoculation and subsequently transmitting the disease to the other phase II animals. The predicted VP1 amino acid sequence encoded by the FMDV RNA isolated from nasal swab samples obtained from the clinical phase of cattle in phase II indicated that infection of that group of cattle was seeded by at least two distinct viral variants. Specifically, the viral sequence obtained from animal 13, which had developed clinical FMD 1 day earlier than the majority of animals of the group, was similar to only one other sample obtained from that group (animal 10). This suggests that animals 12, 14, 15, 16, and 17 were not infected by animal 13, but rather through at least one additional distinct primary infection directly from the inoculum. Interestingly, all sequences obtained from phase II samples differed from the phase I samples within the integrin-binding region of the G-H loop (RSGD in phase I samples versus RRGD in phase II samples). However, since only samples from the clinical phase of infection were included in this analysis, it is likely that this substitution had occurred during the later stages of infection of the phase I animals, as suggested by the sequence obtained from the pooled OPF inoculum (Fig. 3).
The use of OPF and the simulated natural INP system in this study had advantages but also intrinsic limitations. Under natural conditions, the probability that a sufficient quantity of FMDV shed from a carrier animal would reach the susceptible cells within the nasopharynx of a naive animal is likely very small. However, the successful transmission under these experimental conditions substantiates the perceived risk of contagion associated with persistently infected FMDV carrier cattle. Furthermore, these findings confirm that the infectious dose of FMDV required to infect cattle through nasopharyngeal exposure is very low.
There has been speculation on the mechanisms responsible for the low infectiousness of FMDV carrier cattle, but the mechanisms have not been definitively elucidated. It has been postulated that FMDV in OPF from persistently infected animals may be shed either as immunoglobulin-bound (cell-free) virus or within detached cells or cellular debris (2). Oropharyngeal fluid samples from FMDV carriers contain secreted anti-FMDV IgA (13, 40, 41), which may decrease infectivity. Furthermore, it has been demonstrated that the apparent infectivity of OPF samples increases substantially for tissue culture cells if these samples are pretreated with a fluorocarbon compound (1,1,2-trichlorotrifluoroethane or trichlorotrifluoroethane [TTE]), which is believed to dissociate immunoglobulins bound to FMDV (30, 42). The advantages of using TTE treatment of OPF samples prior to virus isolation have been utilized in multiple large-scale investigations (13, 19, 43, 44) and were confirmed in this investigation by an increased titer measured in the TTE-treated OPF. However, it is also possible that the increased virus titers detected after TTE treatment of OPF may be caused by disruption of cellular membranes and thereby release of virus from cells or cellular debris present within the OPF. Shedding of persistent FMDV in association with sloughing of superficial nasopharyngeal epithelial cells is consistent with findings from investigations using immunomicroscopy in our laboratory (13). Additionally, previous in vitro investigations have suggested that FMDV may be released from infected cells within “cytoplasmic blebs” (45). This may be similar to the nonlytic cellular escape mechanisms that have been described for other picornaviruses (46). Specifically, hepatitis A virus and some members of the Enterovirus genus have been reported to be released from infected cells in a “quasi-enveloped” state within membranous vesicles (47–49). To our knowledge, such nonlytic cellular escape of FMDV has not yet been described in vivo. Although the mechanism of shedding of FMDV into OPF in persistently infected animals is not known, the possible release of virus within membranous compartments could potentially prevent immediate binding of secreted IgA to FMDV and thus protect the infectivity of shed virus.
The pigs exposed to the OPF from the carrier cattle in this investigation did not become infected. This is in agreement with previous reports that have concluded that higher infectious doses are required to initiate FMD in this species (2, 34). Feeding unprocessed food waste to pigs has been associated with initiation of FMD epidemics (50). However, the current findings suggest that the amounts of FMDV present in OPF or nasopharyngeal tissues of FMDV carriers may not be sufficient for disease dissemination to pigs to occur readily via this route. Further investigations are necessary to determine a minimum infectious dose to infect pigs via oropharyngeal exposure.
Conclusions.
This current investigation demonstrated that it is possible to transmit FMDV from persistently infected cattle to naive recipient cattle via mechanical transfer of unprocessed oropharyngeal fluid. Pigs exposed to the same material, under similar conditions, did not develop FMD, which suggests that a higher infectious dose and/or distinct mechanisms are required to infect this species by this route. These results contribute to improved understanding of the FMDV carrier state and provide novel information that is relevant for FMD risk analyses.
MATERIALS AND METHODS
Virus.
The virus used for this investigation was an isolate of FMDV strain A24 Cruzeiro that had been passaged twice in cattle as used previously (13).
Authentication of cell lines.
The cell lines used for virus isolation were LFBK-αvβ6 (51), which are porcine kidney cells transfected with a bovine integrin receptor, and BHK-21 cells originally obtained from ATCC (Manassas, VA, USA). Species specificity and absence of cross-contamination of cell lines were confirmed by validated conventional PCR assays detecting DNA from pig, cow, hamster, and monkey, corresponding to the species origin of cell lines routinely used in the laboratory.
Animals.
All animal experiments were performed in the CL3Ag FMDV research facility on Lindholm Island, which is part of the National Veterinary Institute of the Technical University of Denmark (DTU). This study was conducted with approval from the Danish Animal Experimentation Inspectorate (license 201415-0201-00173) in accordance with Danish and European Union (EU) legislation (Consolidation Act 474 15/05/2014 and EU Directive 2010/63/EU). Cattle were Holstein bull calves weighing approximately 150 to 200 kg upon arrival. Pigs were conventionally bred Landrace/Yorkshire mixed males and females weighing approximately 20 kg at delivery. All animals were allowed 1 week of acclimatization in the facility before the start of the experiments.
Study design.
Phases I and II of the study were carried out sequentially, using separate isolation units, while phase III was performed several weeks later after cleaning, disinfection, and fumigation of the unit.
Phase I.
The first phase of the experiments included nine cattle that were inoculated with 105 infectious doses (titrated in bovine tongue epithelium) of FMDV A24 via intranasopharyngeal (INP) inoculation as previously described (38). Briefly, cattle were sedated and placed in sternal recumbency, and the virus inoculum (2 ml), diluted in minimal essential medium (MEM) with 25 mM HEPES, was deposited within the nasopharynx using a flexible 30-cm catheter. The cattle in the first phase of the study were monitored for 30 days postinfection (dpi). Oropharyngeal fluid (OPF) samples for challenge of cattle and pigs in phases II and III were collected at 30 dpi, and tissues for challenge of pigs in phase III were harvested at 31 dpi immediately after euthanasia. Nasopharyngeal tissue samples for feeding to pigs consisted of the dorsal surface of the soft palate and the dorsal surface of the nasopharynx as previously described (13, 16). Tissue samples were macerated using forceps and scissors to facilitate feeding to pigs in phase III. Clinical monitoring and sample collection were carried out as described below.
Phase II.
The second phase of the experiment included eight cattle that were subjected to INP inoculation as described above, but with each animal receiving 10 ml of pooled OPF that had been harvested at 30 dpi from seven phase I animals that had been identified as being persistently infected carriers. Prior to inoculation of phase II animals, the pooled OPF was homogenized using a 16-gauge metal cannula attached to a 50-ml syringe in order to disrupt mucous and potential epithelium within the sample. There was no further processing or freezing of this material prior to inoculation of the phase II cattle. Challenge of phase II cattle (0 dpi) was performed on the same day as the OPF samples were harvested from phase I animals (30 dpi). Animals in this second phase of the experiment were monitored for a further 14 days.
Phase III.
The third phase of the investigation included two groups of five pigs each. The pigs in the first group were inoculated with OPF from the phase I carrier cattle (stored at −80°C following collection) by intraoropharyngeal (IOP) inoculation as previously described (39). Briefly, sedated pigs were placed in dorsal recumbency, and the inoculum (5 ml) was deposited onto the surface of the tonsil of the soft palate using a blunt-ended metal cannula. Pigs were kept on their backs for approximately 1 min before they were placed in sternal position and left to recover from the sedation. The pigs in the second group were each fed approximately 45 g of nasopharyngeal tissue harvested from the phase I cattle. The macerated tissues were mixed with a small amount of the pig’s standard feed, and each pig received the measured ration in a separate feeding bucket. Both groups of pigs were monitored for the following 14 days.
Clinical monitoring and sample collection.
Samples collected to evaluate infection dynamics in cattle were nasal swabs and blood and OPF samples. Nasal swabs were collected using tampons inserted into each nostril, and blood samples were collected through jugular venipuncture. Blood samples and tampons were centrifuged at 2,075 × g for 10 min to harvest serum and nasal fluid, respectively. Blood samples were collected daily from 0 to 10 dpi, and once per week thereafter. Nasal swabs were collected daily from 0 to 10 dpi and twice per week thereafter. OPF was collected using a probang cup. Probang sampling of phase I animals was conducted twice weekly from 14 to 28 dpi, with an additional final sampling at 30 dpi in order to harvest OPF for challenge of phase II animals. The OPF was diluted with an equal volume of MEM with 25 mM HEPES, except for the 30 dpi sample for which the amount of added medium was reduced to half (giving a 2:1 ratio). OPF samples were homogenized using a syringe and cannula as described above. FMDV carrier status of phase I animals was determined on the basis of consistent detection (by real-time quantitative PCR [RT-qPCR]) of FMDV RNA in OPF from 14 dpi to 28 dpi. At 30 dpi, OPF samples were collected only from the seven cattle that had been identified as FMDV carriers.
Samples collected from pigs were whole blood and oropharyngeal (OP) swabs as previously described (39). The OP swab samples were harvested using a large cotton swab applied to the tonsil of the soft palate and subsequently immersed in MEM (2 ml) with 25 mM HEPES. Swabs and blood samples were centrifuged as described above to retrieve the OPF and serum. Swabs were collected daily from 0 to 10 dpi and again at 14 dpi. Blood samples were collected on 0, 2, 3, 4, 6, 8, 10, and 14 dpi.
Daily clinical examinations of both cattle and pigs included monitoring for any signs of FMD, such as fever, lameness, and vesicular lesions. The occurrence and progression of clinical FMD were recorded using a cumulative lesion score for which any lesion on the head contributed 1 point and foot lesions contributed 1 point per affected foot, giving a maximum score of 5. For cattle, the head and oral cavity were inspected daily from 0 to 10 dpi. Feet were inspected twice weekly in sedated cattle (0, 3, 6 and 10 dpi for phase I cattle and 0, 3, 5, 7, and 10 dpi for phase II cattle). For pigs, the head and feet were examined daily from 0 to 10 dpi and again after euthanasia at 14 dpi.
FMDV RNA detection.
Total RNA was extracted from serum, nasal fluid, and OPF samples using a MagNA Pure LC total nucleic acid isolation kit (product no. 03038505001; Roche) with an automated robotic workstation (Roche), according to the manufacturer’s instructions. The level of FMDV RNA in serum and nasal fluid samples was determined using a one-step quantitative RT-PCR assay targeting the 3D-coding region of the FMDV genome (52) as modified by Vandenbussche et al. (53). OPF samples were analyzed using similar primers and probes, but in a two-step assay. Briefly, cDNA was produced using reverse transcriptase (TaqMan reverse transcriptase; Applied Biosystems) with random hexamer primers (Roche). The quantitative PCR was performed using AmpliTaq (Applied Biosystems) using the primers and probes described by Callahan et al. (52).
Quantitation of infectivity in OPF and tissue macerate.
The in vitro infectivity of the OPF and nasopharyngeal tissue samples obtained from the seven persistently infected carriers at 30 dpi was evaluated through titration on BHK-21 and LFBK-αvβ6 cells (51) as previously described (17). Two aliquots of 30 mg of tissue macerate were thawed, MEM (900 µl) and two steel beads (catalog no. 69989; Qiagen) were added to each aliquot, and the samples were homogenized using a TissueLyser bead beater (Qiagen) (2 min; frequency, 22/s). The processed macerates were pooled and clarified through centrifugation at 1,000 × g for 2 min at 4°C. For both the processed tissue macerate and the pooled OPF sample, one aliquot (1 ml) was treated with 1,1,2-trichlorotrifluoroethane (TTE) for dissociation of immunocomplex-bound virus as previously described (54). All four sample aliquots (TTE-treated and nontreated OPF and processed tissue macerate) were cleared of debris and potential bacterial contamination by centrifugation through Spin-X filter columns (pore size, 0.45 μm; catalog no. 8163; Costar) and were subsequently inoculated onto the two different cell types. Calculations of infectivity (as 50% tissue culture infectious doses [TCID50] per milliliter) were performed by standard methods (55). An additional attempt to isolate FMDV from the tissue macerate was performed by inoculating T25 flasks of both LFBK-αvβ6 and BHK-21 cells with 1 ml of non-TTE-treated and nonfiltered macerate. All supernatants were analyzed by RT-qPCR to determine the occurrence of FMDV replication.
Detection of anti-FMDV antibodies in serum.
Serum samples obtained at 0 and 14 dpi from the pigs in experimental phase III were analyzed for the presence of anti-FMDV antibodies using a solid-phase blocking enzyme-linked immunosorbent assay (ELISA) as previously described (56).
FMDV sequence assembly and analysis.
RNA was extracted from nasal swab samples from individual calves (collected on preselected days) and also from the FMDV A24 inoculum using the MagNA Pure system (Roche) as described by the manufacturer. The cDNA synthesis was carried out using Ready-To-Go You-Prime First-Strand beads (GE Healthcare Life Sciences, Uppsala, Sweden) with a mixture of random hexamer primers [pd(N)6] and oligo(dT). The cDNA was diluted to 150 µl from which an aliquot (5 µl) was used to amplify the VP1 coding region using primers 10-PPN6 (5′-TAGCGCCGGCAAAGACTTTGA) and 1-OPN20 (5′-GACATGTCCTCCTGCATCTG). The products (ca. 810 bp) were purified using a QIAquick gel extraction and purification kit (Qiagen, Hilden, Germany) and quantified using a Nanodrop 1000 spectrophotometer (Fisher Scientific, Waltham, MA, USA). Sequencing of the PCR products was performed using a BigDye Terminator v 3.1 cycle sequencing kit (Applied Biosystems, Foster City, CA, USA), using the same primers as used in the PCRs, according to the manufacturer’s instructions, and ran on an automated DNA sequencer (ABI PRISM 3730 DNA analyzer; Applied Biosystems, Foster City, CA, USA). The resulting consensus sequences were compared to others using MUSCLE (https://www.ebi.ac.uk/Tools/msa/muscle/) and translated into amino acid sequences using ExPASy (https://web.expasy.org/cgi-bin/translate/dna_aa). Near-full-length genome sequences, from selected samples, were assembled using Seqman Pro 14 based on the production and sequencing of 15 separate PCR products, using primers (Table 2) to produce overlapping amplicons.
TABLE 2.
Primers used for RT-PCRs and sequencing
| Primer | Primer sequence (5′–3')a | Orientation | Location (nt)b |
|---|---|---|---|
| 8-APN35 | GAGAAAXGGGACGTCXGCGC | Forward | 522 |
| 8-APN2 | GTCXCCTATTCAGGCXTAGAAG | Reverse | 990 |
| 8-APN3 | GGCTAAGGATGCCCTTCAG | Forward | 894 |
| 9-XPN18 | TTXGAXAACCAXTCXTTXTTXTGXGTGTT | Reverse | 1832 |
| 14-CPN63 | CCGTTGGAGGTGACACACG | Reverse | 1503 |
| 14-CPN7 | ATGCCATCAGTGGAGGCTCC | Forward | 1773 |
| 14-CPN6 | GTCCAACAGGTTGGTGAAGC | Reverse | 2679 |
| 14-CPN5 | ATGGCAAGGTGTACAACCCG | Forward | 2637 |
| 11-FPN35 | GAARGGCCCRGGGTTGGAC | Reverse | 3898 |
| 14-CPN61 | GGAGGCGCAACTCAAAGTC | Reverse | 3185 |
| 14-CPN3 | TACAACAAGGCACCATTCACG | Forward | 3542 |
| 11-SPN3 | ACACTGTCGCCAGCACACG | Reverse | 3593 |
| 14-CPN4 | CCAGACCGCTGTTGGCAATAG | Forward | 3783 |
| 8-APN45 | GGAAGAAACTCGAGGCGAC | Reverse | 4316 |
| 8-APN22 | AAGGACCCXGTCCTTGTGGC | Forward | 4151 |
| 1-XPN28 | GTTGTAGCCGTCXAAGTGGTC | Reverse | 4808 |
| 8-APN46 | TGGTCGTTTGCCTCCGTGG | Forward | 4683 |
| 8-APN87 | CTCAAAGAATTCAATTGCTGC | Reverse | 5387 |
| 8-APN13 | GCXCTTCTXAACGGXATGGC | Forward | 5171 |
| 8-APN68 | GGGTCCTTCAGCTGGTGG | Reverse | 5774 |
| 8-APN113 | CGCGAXACTCGCAAGAGAC | Forward | 5555 |
| 9-XPN11 | AGCATGTCCTGTCCTTTTACT | Reverse | 6223 |
| 14-CPN2 | CCATTTGCTGTGCTACTGGA | Forward | 6084 |
| 8-APN114 | CAGGGTTGAACACACCGTG | Reverse | 6716 |
| 9-XPN2 | AATGAAGGCACACXTXGAXCCXGA | Forward | 6601 |
| 14-CPN1 | AGGGTTACAACCGACCGCG | Reverse | 7276 |
| 8-APN17 | CTGAAGGACGAXXTXCGXCC | Forward | 7124 |
| 8-APN52 | GGAXTGACCAAGAACAAAACC | Reverse | 7754 |
| 9-XPN23 | TGGACACXTACACCATGATCTC | Forward | 7620 |
| NVT27 | TTTTTTTTTTTTTTTTTTTTTTTTTTTVN | Reverse | 8140 |
X = inosine.
The primer locations are based on the sequence of FMDV A24 Cruzeiro (accession no. AY593768.1). For forward primers, the 5′-terminal nucleotide (nt) is used, while for the reverse primers, the position of the nt that is complementary to the 3′ nt of the primer is given.
Accession number(s).
The sequence of the inoculum used to infect the animals, and to which all other sequences were compared, is available at GenBank under accession no. MH746921.
ACKNOWLEDGMENTS
This work was funded by the U.S. Department of Agriculture Agricultural Research Service CRIS project 1940-32000-061-00D and an interagency agreement with the Science and Technology Directorate of the U.S. Department of Homeland Security under award HSHQDC-11-X-00131.
None of the funding sources had any role in study design, interpretation of results, or decision to publish.
Preben Normann, Jani Christiansen, and Ethan Hartwig are thanked for processing of samples. Henrik Andersen, Janni Oxfeldt, and Heidi Lehman are thanked for animal handling and technical support through the experiments. Amaresh Das is thanked for optimizing and performing the cell line authentication assays.
REFERENCES
- 1.Grubman MJ, Baxt B. 2004. Foot-and-mouth disease. Clin Microbiol Rev 17:465–493. doi: 10.1128/CMR.17.2.465-493.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexandersen S, Zhang Z, Donaldson AI, Garland AJM. 2003. The pathogenesis and diagnosis of foot-and-mouth disease. J Comp Pathol 129:1–36. doi: 10.1016/S0021-9975(03)00041-0. [DOI] [PubMed] [Google Scholar]
- 3.Brito BP, Rodriguez LL, Hammond JM, Pinto J, Perez AM. 2017. Review of the global distribution of foot-and-mouth disease virus from 2007 to 2014. Transbound Emerg Dis 64:316–332. doi: 10.1111/tbed.12373. [DOI] [PubMed] [Google Scholar]
- 4.Jamal SM, Belsham GJ. 2013. Foot-and-mouth disease: past, present and future. Vet Res 44:116. doi: 10.1186/1297-9716-44-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jamal SM, Belsham GJ. 2018. Molecular epidemiology, evolution and phylogeny of foot-and-mouth disease virus. Infect Genet Evol 59:84–98. doi: 10.1016/j.meegid.2018.01.020. [DOI] [PubMed] [Google Scholar]
- 6.Arzt J, Baxt B, Grubman MJ, Jackson T, Juleff N, Rhyan J, Rieder E, Waters R, Rodriguez LL. 2011. The pathogenesis of foot-and-mouth disease II: viral pathways in swine, small ruminants, and wildlife; myotropism, chronic syndromes, and molecular virus-host interactions. Transbound Emerg Dis 58:305–326. doi: 10.1111/j.1865-1682.2011.01236.x. [DOI] [PubMed] [Google Scholar]
- 7.Arzt J, Juleff N, Zhang Z, Rodriguez LL. 2011. The pathogenesis of foot-and-mouth disease I: viral pathways in cattle. Transbound Emerg Dis 58:291–304. doi: 10.1111/j.1865-1682.2011.01204.x. [DOI] [PubMed] [Google Scholar]
- 8.Muroga N, Hayama Y, Yamamoto T, Kurogi A, Tsuda T, Tsutsui T. 2012. The 2010 foot-and-mouth disease epidemic in Japan. J Vet Med Sci 74:399–404. doi: 10.1292/jvms.11-0271. [DOI] [PubMed] [Google Scholar]
- 9.Park JH, Lee KN, Ko YJ, Kim SM, Lee HS, Park JY, Yeh JY, Kim MJ, Lee YH, Sohn HJ, Moon JS, Cho IS, Kim B. 2014. Outbreaks and diagnosis of foot-and-mouth disease serotype O in the Republic of Korea, April-June 2010. Transbound Emerg Dis 61:277–284. doi: 10.1111/tbed.12029. [DOI] [PubMed] [Google Scholar]
- 10.Yoon H, Yoon SS, Kim YJ, Moon OK, Wee SH, Joo YS, Kim B. 2015. Epidemiology of the foot-and-mouth disease serotype O epidemic of November 2010 to April 2011 in the Republic of Korea. Transbound Emerg Dis 62:252–263. doi: 10.1111/tbed.12109. [DOI] [PubMed] [Google Scholar]
- 11.Samuel AR, Knowles NJ. 2001. Foot-and-mouth disease virus: cause of the recent crisis for the UK livestock industry. Trends Genet 17:421–424. doi: 10.1016/S0168-9525(01)02374-5. [DOI] [PubMed] [Google Scholar]
- 12.World Organisation for Animal Health (OIE). 2016. Terrestrial Animal Health Code, Chapter 8.8. Infection with foot and mouth disease virus. World Organisation for Animal Health (OIE), Paris, France: http://www.oie.int/fileadmin/Home/eng/Health_standards/tahc/current/chapitre_fmd.pdf. Accessed 14 July 2016. [Google Scholar]
- 13.Stenfeldt C, Eschbaumer M, Rekant SI, Pacheco JM, Smoliga GR, Hartwig EJ, Rodriguez LL, Arzt J. 2016. The foot-and-mouth disease carrier state divergence in cattle. J Virol 90:6344–6364. doi: 10.1128/JVI.00388-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alexandersen S, Zhang Z, Donaldson AI. 2002. Aspects of the persistence of foot-and-mouth disease virus in animals–the carrier problem. Microbes Infect 4:1099–1110. doi: 10.1016/S1286-4579(02)01634-9. [DOI] [PubMed] [Google Scholar]
- 15.Moonen P, Schrijver R. 2000. Carriers of foot-and-mouth disease virus: a review. Vet Q 22:193–197. doi: 10.1080/01652176.2000.9695056. [DOI] [PubMed] [Google Scholar]
- 16.Arzt J, Pacheco JM, Rodriguez LL. 2010. The early pathogenesis of foot-and-mouth disease in cattle after aerosol inoculation: identification of the nasopharynx as the primary site of infection. Vet Pathol 47:1048–1063. doi: 10.1177/0300985810372509. [DOI] [PubMed] [Google Scholar]
- 17.Pacheco JM, Arzt J, Rodriguez LL. 2010. Early events in the pathogenesis of foot-and-mouth disease in cattle after controlled aerosol exposure. Vet J 183:46–53. doi: 10.1016/j.tvjl.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 18.Stenfeldt C, Eschbaumer M, Pacheco JM, Rekant SI, Rodriguez LL, Arzt J. 2015. Pathogenesis of primary foot-and-mouth disease virus infection in the nasopharynx of vaccinated and non-vaccinated cattle. PLoS One 10:e0143666. doi: 10.1371/journal.pone.0143666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pacheco JM, Smoliga GR, O’Donnell V, Brito BP, Stenfeldt C, Rodriguez LL, Arzt J. 2015. Persistent foot-and-mouth disease virus infection in the nasopharynx of cattle; tissue-specific distribution and local cytokine expression. PLoS One 10:e0125698. doi: 10.1371/journal.pone.0125698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutmoller P, Gaggero A. 1965. Foot-and mouth diseases carriers. Vet Rec 77:968–969. doi: 10.1136/vr.77.33.968. [DOI] [PubMed] [Google Scholar]
- 21.Stenfeldt C, Lohse L, Belsham GJ. 2013. The comparative utility of oral swabs and probang samples for detection of foot-and-mouth disease virus infection in cattle and pigs. Vet Microbiol 162:330–337. doi: 10.1016/j.vetmic.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 22.Parthiban AB, Mahapatra M, Gubbins S, Parida S. 2015. Virus excretion from foot-and-mouth disease virus carrier cattle and their potential role in causing new outbreaks. PLoS One 10:e0128815. doi: 10.1371/journal.pone.0128815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garland AJ, de Clercq K. 2011. Cattle, sheep and pigs vaccinated against foot and mouth disease: does trade in these animals and their products present a risk of transmitting the disease? Rev Sci Tech 30:189–206. doi: 10.20506/rst.30.1.2023. [DOI] [PubMed] [Google Scholar]
- 24.Sutmoller P, Casas OR. 2002. Unapparent foot and mouth disease infection (sub-clinical infections and carriers): implications for control. Rev Sci Tech 21:519–529. doi: 10.20506/rst.21.3.1366. [DOI] [PubMed] [Google Scholar]
- 25.Bronsvoort BM, Handel IG, Nfon CK, Sorensen KJ, Malirat V, Bergmann I, Tanya VN, Morgan KL. 2016. Redefining the "carrier" state for foot-and-mouth disease from the dynamics of virus persistence in endemically affected cattle populations. Sci Rep 6:29059. doi: 10.1038/srep29059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ilott MC, Salt JS, Gaskell RM, Kitching RP. 1997. Dexamethasone inhibits virus production and the secretory IgA response in oesophageal-pharyngeal fluid in cattle persistently infected with foot-and-mouth disease virus. Epidemiol Infect 118:181–187. doi: 10.1017/S0950268896007376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bertram M, Vu LT, Pauszek JR, Brito B, Hartwig E, Smoliga G, Hoang BH, Phuong NT, Stenfeldt C, Fish IH, Hung VV, Delgado A, VanderWaal K, Rodriguez LL, Long NT, Dung DH, Arzt J. 2018. Lack of transmission of foot-and-mouth disease virus from persistently infected cattle to naïve cattle under field conditions in Vietnam. Front Vet Sci 5:174. doi: 10.3389/fvets.2018.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tenzin, Dekker A, Vernooij H, Bouma A, Stegeman A. 2008. Rate of foot-and-mouth disease virus transmission by carriers quantified from experimental data. Risk Anal 28:303–309. [DOI] [PubMed] [Google Scholar]
- 29.Sutmoller P, McVicar JW, Cottral GE. 1967. Foot-and-mouth disease virus carrier studies at the Plum Island Animal Disease Laboratory. European Commission for the control of foot-and-mouth disease Standing Technical Committee working paper no. 11. European Commission, Brussels. Belgium. [Google Scholar]
- 30.Sutmoller P, Cottral GE. 1967. Improved techniques for the detection of foot-and-mouth disease virus in carrier cattle. Arch Gesamte Virusforsch 21:170–177. doi: 10.1007/BF01241441. [DOI] [PubMed] [Google Scholar]
- 31.Dawe PS, Flanagan FO, Madekurozwa RL, Sorensen KJ, Anderson EC, Foggin CM, Ferris NP, Knowles NJ. 1994. Natural transmission of foot-and-mouth-disease virus from African buffalo (Syncerus caffer) to cattle in a wildlife area of Zimbabwe. Vet Rec 134:230–232. doi: 10.1136/vr.134.10.230. [DOI] [PubMed] [Google Scholar]
- 32.Dawe PS, Sorensen K, Ferris NP, Barnett ITR, Armstrong RM, Knowles NJ. 1994. Experimental transmission of foot-and-mouth-disease virus from carrier African buffalo (Syncerus caffer) to cattle in Zimbabwe. Vet Rec 134:211–215. doi: 10.1136/vr.134.9.211. [DOI] [PubMed] [Google Scholar]
- 33.Sutmoller P, McVicar JW, Cottral GE. 1968. The epizootiological importance of foot-and-mouth disease carriers. I. Experimentally produced foot-and-mouth disease carriers in susceptible and immune cattle. Arch Gesamte Virusforsch 23:227–235. doi: 10.1007/BF01241895. [DOI] [PubMed] [Google Scholar]
- 34.Sellers RF. 1971. Quantitative aspects of the spread of foot and mouth disease. Vet Bull 41:431–439. [Google Scholar]
- 35.Eschbaumer M, Stenfeldt C, Rekant SI, Pacheco JM, Hartwig EJ, Smoliga GR, Kenney MA, Golde WT, Rodriguez LL, Arzt J. 2016. Systemic immune response and virus persistence after foot-and-mouth disease virus infection of naive cattle and cattle vaccinated with a homologous adenovirus-vectored vaccine. BMC Vet Res 12:205. doi: 10.1186/s12917-016-0838-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Bekkum JG, Frenkel HS, Frederiks HHJ, Frenkel S. 1959. Observations on the carrier state of cattle exposed to foot-and-mouth disease virus. Tijdschr Diergeneeskd 84:1159–1164. [Google Scholar]
- 37.Geale DW, Barnett PV, Clarke GW, Davis J, Kasari TR. 2015. A review of OIE country status recovery using vaccinate-to-live versus vaccinate-to-die foot-and-mouth disease response policies II: waiting periods after emergency vaccination in FMD free countries. Transbound Emerg Dis 62:388–406. doi: 10.1111/tbed.12165. [DOI] [PubMed] [Google Scholar]
- 38.Pacheco JM, Stenfeldt C, Rodriguez LL, Arzt J. 2016. Infection dynamics of foot-and-mouth disease virus in cattle following intranasopharyngeal inoculation or contact exposure. J Comp Pathol 155:314–325. doi: 10.1016/j.jcpa.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 39.Stenfeldt C, Pacheco JM, Rodriguez LL, Arzt J. 2014. Infection dynamics of foot-and-mouth disease virus in pigs using two novel simulated-natural inoculation methods. Res Vet Sci 96:396–405. doi: 10.1016/j.rvsc.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 40.Parida S, Anderson J, Cox SJ, Barnett PV, Paton DJ. 2006. Secretory IgA as an indicator of oro-pharyngeal foot-and-mouth disease virus replication and as a tool for post vaccination surveillance. Vaccine 24:1107–1116. doi: 10.1016/j.vaccine.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 41.Francis MJ, Ouldridge EJ, Black L. 1983. Antibody-response in bovine pharyngeal fluid following foot-and-mouth-disease vaccination and, or, exposure to live virus. Res Vet Sci 35:206–210. [PubMed] [Google Scholar]
- 42.Brown F, Cartwright B. 1960. Purification of the virus of foot-and-mouth disease by fluorocarbon treatment and its dissociation from neutralizing antibody. J Immunol 85:309–313. [Google Scholar]
- 43.Brito B, Pauszek SJ, Eschbaumer M, Stenfeldt C, de Carvalho Ferreira HC, Vu LT, Phuong NT, Hoang BH, Tho ND, Dong PV, Minh PQ, Long NT, King DP, Knowles NJ, Dung DH, Rodriguez LL, Arzt J. 2017. Phylodynamics of foot-and-mouth disease virus O/PanAsia in Vietnam 2010–2014. Vet Res 48:24. doi: 10.1186/s13567-017-0424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Carvalho Ferreira HC, Pauszek SJ, Ludi A, Huston CL, Pacheco JM, Le VT, Nguyen PT, Bui HH, Nguyen TD, Nguyen T, Nguyen TT, Ngo LT, Do DH, Rodriguez L, Arzt J. 2017. An integrative analysis of foot-and-mouth disease virus carriers in Vietnam achieved through targeted surveillance and molecular epidemiology. Transbound Emerg Dis 64:547–563. doi: 10.1111/tbed.12403. [DOI] [PubMed] [Google Scholar]
- 45.Yilma T, McVicar JW, Breese SS. 1978. Pre-lytic release of foot-and-mouth disease virus in cytoplasmic blebs. J Gen Virol 41:105–114. doi: 10.1099/0022-1317-41-1-105. [DOI] [PubMed] [Google Scholar]
- 46.Bird SW, Kirkegaard K. 2015. Escape of non-enveloped virus from intact cells. Virology 479–480:444–449. doi: 10.1016/j.virol.2015.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McKnight KL, Xie L, Gonzalez-Lopez O, Rivera-Serrano EE, Chen X, Lemon SM. 2017. Protein composition of the hepatitis A virus quasi-envelope. Proc Natl Acad Sci U S A 114:6587–6592. doi: 10.1073/pnas.1619519114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hirai-Yuki A, Hensley L, Whitmire JK, Lemon SM. 2016. Biliary secretion of quasi-enveloped human hepatitis A virus. mBio 7:e01998-16. doi: 10.1128/mBio.01998-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robinson SM, Tsueng G, Sin J, Mangale V, Rahawi S, McIntyre LL, Williams W, Kha N, Cruz C, Hancock BM, Nguyen DP, Sayen MR, Hilton BJ, Doran KS, Segall AM, Wolkowicz R, Cornell CT, Whitton JL, Gottlieb RA, Feuer R. 2014. Coxsackievirus B exits the host cell in shed microvesicles displaying autophagosomal markers. PLoS Pathog 10:e1004045. doi: 10.1371/journal.ppat.1004045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mansley LM, Donaldson AI, Thrusfield MV, Honhold N. 2011. Destructive tension: mathematics versus experience–the progress and control of the 2001 foot and mouth disease epidemic in Great Britain. Rev Sci Tech 30:483–498. doi: 10.20506/rst.30.2.2054. [DOI] [PubMed] [Google Scholar]
- 51.LaRocco M, Krug PW, Kramer E, Ahmed Z, Pacheco JM, Duque H, Baxt B, Rodriguez LL. 2013. A continuous bovine kidney cell line constitutively expressing bovine alphavbeta6 integrin has increased susceptibility to foot-and-mouth disease virus. J Clin Microbiol 51:1714–1720. doi: 10.1128/JCM.03370-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Callahan JD, Brown F, Osorio FA, Sur JH, Kramer E, Long GW, Lubroth J, Ellis SJ, Shoulars KS, Gaffney KL, Rock DL, Nelson WM. 2002. Use of a portable real-time reverse transcriptase-polymerase chain reaction assay for rapid detection of foot-and-mouth disease virus. J Am Vet Med Assoc 220:1636–1642. doi: 10.2460/javma.2002.220.1636. [DOI] [PubMed] [Google Scholar]
- 53.Vandenbussche F, Lefebvre DJ, De Leeuw I, Van Borm S, De Clercq K. 2017. Laboratory validation of two real-time RT-PCR methods with 5'-tailed primers for an enhanced detection of foot-and-mouth disease virus. J Virol Methods 246:90–94. doi: 10.1016/j.jviromet.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 54.Stenfeldt C, Pacheco JM, Smoliga GR, Bishop E, Pauszek SJ, Hartwig EJ, Rodriguez LL, Arzt J. 2016. Detection of foot-and-mouth disease virus RNA and capsid protein in lymphoid tissues of convalescent pigs does not indicate existence of a carrier state. Transbound Emerg Dis 63:152–164. doi: 10.1111/tbed.12235. [DOI] [PubMed] [Google Scholar]
- 55.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am J Hyg 27:493–497. doi: 10.1093/oxfordjournals.aje.a118408. [DOI] [Google Scholar]
- 56.Balinda SN, Tjornehoj K, Muwanika VB, Sangula AK, Mwiine FN, Ayebazibwe C, Masembe C, Siegismund HR, Alexandersen S. 2009. Prevalence estimates of antibodies towards foot-and-mouth disease virus in small ruminants in Uganda. Transbound Emerg Dis 56:362–371. doi: 10.1111/j.1865-1682.2009.01094.x. [DOI] [PubMed] [Google Scholar]