Abstract
This study aimed to verify whether salivary total protein (STP) would reflect anaerobic threshold in elderly athletes subjected to an incremental exercise test. Methods: Seven elderly elite athletes (EEA) and six physically active elderly men (PAE) completed a treadmill protocol in which blood and saliva samples were collected. Results: Blood lactate (BL) and STP increased significantly in EEA during the test (0.8 ± 0.2 to 5.1 ± 2.0 mmol/L and 42.5 ± 7.5 to 222.5 ± 63.8 mg/dL, respectively) and remained elevated at five minutes after exercise (5.0 ± 1.9 mmol/L and 147.2 ± 50.0 mg/dL, respectively). Furthermore, correlations between STP and heart rate (r = 0.87, p < 0.001), and between BL and STP (r = 0.96, p < 0.001), were observed in the elderly athletes. Conclusions: STP represents a potential non-invasive biomarker for determining anaerobic threshold during an incremental exercise test, and this parameter may be used as an indicator of physical exercise intensity in elderly athletes.
Keywords: Aging, Exercise, Master athletes, Salivary protein, Anaerobic threshold
INTRODUCTION
Traditionally, respiratory gas exchange ratio, maximal oxygen uptake (VO2max), maximum heart rate (HRmax) and blood lactate (BL) have been used to design training programmes for competitive athletes of all ages [1, 2]. However, evidence suggests that the ageing process can alter these variables, potentially leading to errors in assessing the performance of elderly people [3-5]. Thus, more studies are needed to delineate the mechanisms underlying age-related changes, as well as to find biomarkers that do not change with age, in order to design training programmes for elderly athletes.
Although the ageing process alters the morphology and secretory functions of salivary glands, causing a reduction of salivary flow rate [6] and content of several biomolecules [7], studies have shown that the concentration of salivary total protein does not change with age [8, 9]. Therefore, our hypothesis was that salivary total protein could be an alternative biomarker to evaluate training programmes in elderly athletes, since salivary total protein concentration can be easily quantified, and saliva offers clear advantages over blood analysis, as it is readily available and can be easily collected, handled and stored [10].
Recent studies have highlighted salivary molecules, such as alpha-amylase, nitric oxide and chromogranin A, as biomarkers to assess physiological stress conditions [11-16]. In addition, salivary lactate [17] and salivary total protein [STP) [18] were used to evaluate exercise intensity. It should be noted, however, that young athletes have been the target population of those studies. One of the few studies to have evaluated salivary biomarkers in physically active elderly men showed that alpha-amylase activity changed during a fitness programme comprising a 10 min warm-up, 30 min of exercise and a 10 min cool-down [19].
Due to the lack of literature evaluating salivary biomarkers in elderly athletes, we assessed STP in people over 59 years old during a ramp training protocol with increasing loads. Ramp protocols induce haemodynamic and uniform respiratory responses, which facilitates collecting intensity values at each stage of the test [20-23]. Thus, this study aimed to verify whether STP would reflect the anaerobic threshold in elderly participants subjected to a treadmill protocol with increasing speed and inclination, and to evaluate this salivary parameter as a non-invasive biomarker of physical exercise intensity in older athletes.
MATERIALS AND METHODS
Participants
Seven athletes aged 63.1 ± 3.1 years, who had been running professionally for at least ten years and were part of the Athletics Federation of Minas Gerais, Brazil, were considered for inclusion in the intervention group and were appointed as elderly elite athletes (EEA). The control group consisted of six physically active elderly (PAE) men aged 63.8 ± 1.4 years who had been participating in the Physical and Recreational Activities Program for the Elderly at the Federal University of Uberlândia (AFRID-FAEFI-UFU) for at least five years. The exclusion criteria were as follows: a) blood tests with biochemical results above reference values; b) abnormal values of blood pressure at rest; c) changes in basal electrocardiogram (ECG); d) symptoms of xerostomia; e) use of medications such as antidepressants, antihistamines, diuretics, anti-hypertensives, and β-blockers; all participants were nonsmokers. All the criteria adopted are summarized in Table I. Anthropometric characteristics of both EEA and PAE groups are shown in Table II.
TABLE I.
Exclusion and inclusion criteria to take part in the study.
| Physical caracteristics (n=190) | Exclusion criteria | Biochemical variable (n=79) | Inclusion criteria | Echocardiographic variable (n=23) | Inclusion criteria |
|---|---|---|---|---|---|
| Age (years) | < 60 | Albumin (g/L) | 4.0 – 5.3 | Aorta (mm) | 2.27 – 3.4 |
| Total physical activity (MJkg-1.week-1) | < 1.30 | ALT (U/L) | 41 | Left atrium (mm) | 2.5 – 4.0 |
| VO2 max (ml kg-1.min-1) | < 20.0 | ASP (U/L) | 38 | Right ventricle (mm) | 1.4 – 2.6 |
| Body Mass Index (kg.m-2) | > 25.0 | CK-MB (ng/mL) | < 5 | Intervertricular septum (mm) | 0.5 – 1.0 |
| Systolic Blood Pressure (mmHg) | > 110.0 | Creatinine (umol/L) | 44 – 106 | Left ventricle in diastole (mm) | 4.0 – 5.6 |
| Diastolic Blodd Pressure (mmHg) | > 70.0 | Fasting glucose (mmol/L) | 3.88 – 5.49 | Left ventricle in systole (mm) | 2.3 – 3.6 |
| Globulins (g/L) | 1.0 – 3.0 | Posterior wall (mm) | 0.5 – 1.0 | ||
| Hemoglobin (mmol/L) | 2.09 – 2.55 | Ejection fraction (%) | 57.3 – 75.7 | ||
| Lactate dehydrogenase (U/L) | 240 – 480 | Fractional shortening | 30.0 – 45.0 | ||
| Potassium (mmol/L) | 3.5 – 5.0 | Left ventricle mass (g) | 74.9 – 193.1 | ||
| Serum iron (mmol/L) | 7.16 – 32.22 | Left ventricle mass/BSA (g/m2) | 47.8 – 96.9 | ||
| Sodium (mmol/L) | 135 – 145 | ||||
| Total CK (U/L) | 55 – 177 | ||||
| Total iron binding capacity (mmol/L) | 44.75 – 80.55 | ||||
| Total proteins (g/L) | 6.4 – 8.1 | ||||
| Triglicerídeos (mmol/L) | < 1.7 | ||||
| Urate (umol/L) | 0.18 – 0.42 | ||||
| Urea (mmol/L) | 1.67 – 7.5 |
TABLE II.
Anthropometric characteristics of the elderly elite athletes (EEA) and physically active elderly (PAE) men.
| Demographic characteristics | EEA | PAE |
|---|---|---|
| Age (yrs) | 63.1 ± 6.2 | 63.8 ± 4.0 |
| Weight (kg) | 68.4 ± 8.1 | 70.4 ± 3.1 |
| Height (cm) | 170.1 ± 1.9 | 168.5 ± 2.8 |
| Body Mass Index (kg/m2) | < 20.5 ± 1.0 | < 23.5 ± 1.5 |
| HRrest (bpm) | 67.7 ± 7.0 | 76.4 ± 1.5 |
| HRmáx (bpm) | 154.7 ± 5.2 | 147.0 ± 10.2 |
| VO2 max (ml/kg/min) | 32.8 ± 5.5 | 24.4 ± 7.0 |
All experimental procedures were approved by the Ethics Committee in Research of the Federal University of Mato Grosso n° 1.064.808/15, and followed the ethical standards of the Declaration of Helsinki. The participants signed an informed consent form.
Experimental procedure
Prior to the physical exercise test (R0), age-predicted maximal heart rate (HRmax) was calculated for each individual. Participants’ height and mass were measured to the nearest 0.5 cm and 0.1 kg, respectively, and body mass index (BMI) was calculated. The physical exercise test was performed according to the Bruce protocol [24] with the following modifications. The protocol was composed of six three-minute incremental stages on a motorized treadmill. After the sixth stage, the load remained constant until volitional exhaustion.
A 12-lead electrocardiogram using Ergo PC 13 software was used to measure heart rate. The systolic and diastolic pressures were measured using auscultation with a sphygmomanometer (Tycos, USA) and were recorded during the last minute of each incremental exercise stage until volitional exhaustion, at exhaustion (E), and at 5 and 15 minutes after exercise (R5 and R15, respectively). During the test, the frequency, intensity, time and type (FITT) recommendations by Reed and Pipe [1] were adopted.
The anaerobic threshold (AT) for blood lactate and STP was determined according to the Dmax method [25] in order to facilitate visual analysis of the data.
Blood and saliva collection
Each participant was given 400 mL of water prior to the test to ensure they were adequately hydrated [26-29]. Capillary blood samples were collected at R0, during the last minute of each incremental stage, at E, R5 and R15. Capillary blood obtained from the earlobe of each volunteer was collected using heparinized and calibrated glass capillaries.
Samples of saliva were collected at the same time points of blood lactate collections. Before saliva collection, the individuals were instructed to empty their mouth of the “old” saliva, at which point participants were given distilled water to rinse their mouths. Unstimulated saliva was collected using the spit method [30] with precooled minitubes (4ºC) during one minute at each stage. The saliva samples were centrifuged at 12 000 x g, and the supernatant was stored at -20°C until the analyses.
Blood lactate concentration analysis
Blood lactate was analysed using an electroenzymatic method with the biochemical analyser YSI 2300 STAT plus (Yellow Springs, Ohio, USA). A volume of 25 μL of whole blood was used to determine BL values. The assay precision was ± 2% of the reading or 0.1 mmol/L, with a resolution of 0.1 mmol/L. YSI 2747 Standard (0.45 g/L = 5.00 mmol/L L-lactate) was used as the lactate control for linearity, according to the manufacturer’s recommendations. The samples were analysed in duplicate. The mean, standard deviation and coefficient of variation (CV) for studying the imprecision were obtained. The intra-assay coefficient of variation for duplicate samples was approximately 6.9%.
Salivary total protein concentration
The concentration of salivary total protein was determined using the Bradford method, with bovine serum albumin (Sigma. St. Louis, MO, USA) used for the standard protein [31]. Absorbance was measured at 595 nm using a microplate reader (Molecular Devices, Menlo Park, CA, USA), and all samples were assayed in duplicate. The mean, standard deviation and coefficient of variation (CV) for studying the imprecision were obtained. The limit of detection of the Bradford method is 1 μg of protein. The intra-assay coefficient of variation for the duplicate samples was approximately 4.6%.
Statistical analyses
The data were tested for normality using the Shapiro-Wilk test prior to analysis. One-way analysis of variance (ANOVA) with repeated measures, followed by the Tukey test for multiple comparisons, was used to determine differences between BL and STP in samples collected at R0, E, R5 and R15. Pearson’s correlation was used to examine linear relationships between BL and STP. For all of the analyses, significant results were defined at the level of p < 0.05. All results were expressed as means and standard deviations. G*Power: Statistical Power Analyses for Windows (version 3.1.9.2) was used to power calculation based on F-test Power and repeated measures ANOVA. The graphics and all statistical analysis were performed using GraphPad Prism version 6.0.
RESULTS
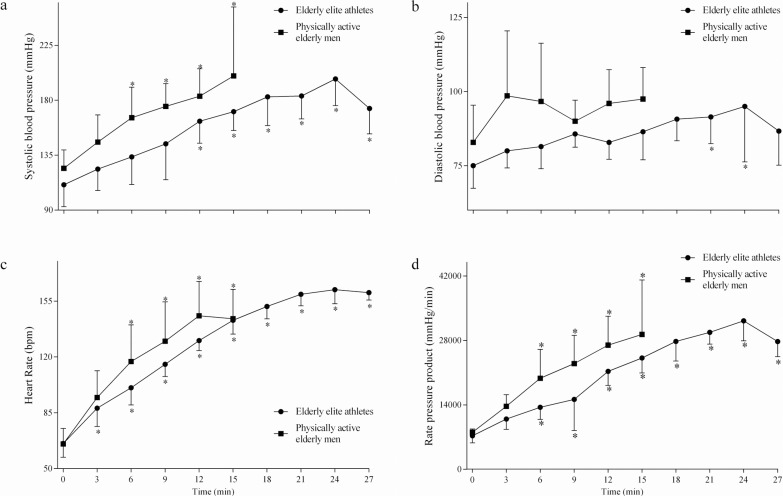
The PAE group performed the exercise test with a duration of 15 ± 3 minutes with > 80% HR (heart rate), while the EEA achieved > 90% HR during the Bruce protocol with a duration of 26 ± 4 min; maximum HR, 145 ± 10 beats/min. No differences were noted in the physiological parameters of the heart between groups during the Bruce protocol (Fig. 1). However, Tukey’s test analysis showed differences within the stages of the incremental test (Fig. 1). Mean systolic blood pressure increased faster in the PAE group than in the EEA group (Fig. 1a). On the other hand, diastolic blood pressure (DBP) oscillated in both groups (Fig. 1b). When compared to the initial stage of the treadmill protocol, DBP did not increase in the PAE group. However, EEA showed oscillatory behaviour of DBP in the first half of the exercise protocol, with significant increases in the seventh and eight stages (Fig. 1b). HR values increased earlier in the EEA group compared to the PAE group (Fig. 1c). The rate pressure product increased at the same stage in both groups (Fig. 1d).
FIG. 1.
Physiological parameters of elite elderly athletes and physically active elderly men measured during the exercise test.
Systolic blood pressure (a), diastolic blood pressure (b), heart rate (c) and rate pressure product (d) were recorded at rest and during the last one minute of each incremental stage until volitional exhaustion. *There is a statistically significant change in relation to basal level (p < 0.05).
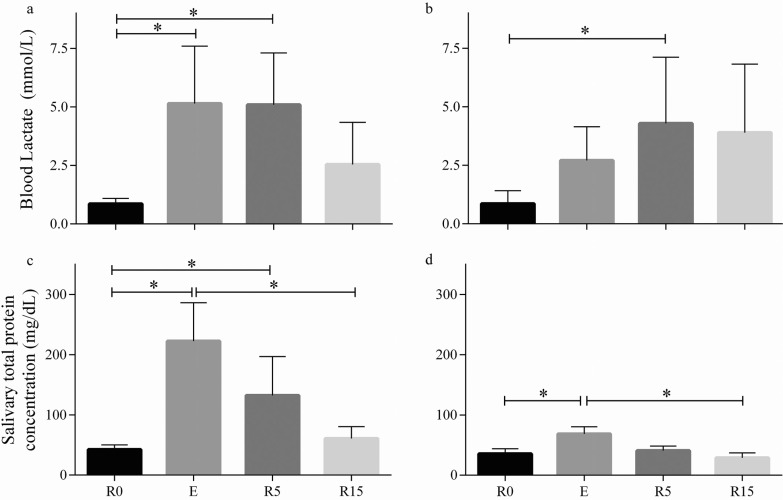
Saliva volumes decreased after exercise in both EEA and PAE groups, increasing 15 minutes after exercise (0.83 ± 0.11 mL at rest, 0.40 ± 0.06 mL at exhaustion, 0.59 ± 0.09 mL at five minutes after exercise and 0.78 ± 0.09 mL at 15 minutes after exercise). BL and STP results are presented in Fig. 2. In the EEA group, both BL and STP increased significantly during the exercise test (0.8 ± 0.2 to 5.1 ± 2.0 mmol/L and 42.5 ± 7.5 mg/dL to 222.5 ± 63.8 mg/dL, respectively) and remained elevated at five minutes after exercise (5.0 ± 1.9 and 147.2 ± 50.0 mg/dL, respectively). In the PAE group, BL had a significant increase only at R5 (1.1 ± 0.3 to 4.5 ± 1.7 mmol/L) while STP doubled at E (35.3 ± 8.7 to 68.3 ± 12.0 mg/dL). STP returned to basal levels at R15 in both groups (54.2 ± 12.2 mg/dL for EEA and 28.7 ± 7.8 mg/dL for PAE).
FIG. 2.
Blood lactate (BL) and total protein of whole saliva (TPWS) concentrations evaluated before exercise (R), at exhaustion (E) and 5 and 15 minutes after exercise (R5 and R15, respectively).
BL results of elderly elite athletes (a) and physically active elderly men (b), and TPWS results of elderly elite athletes (c) and physically active elderly men (d). One-way analysis of variance (ANOVA) with repeated measures, followed by the Tukey test for multiple comparisons, was used to compare the time points R0, E, R5 and R15. Results expressed as mean ± SEM. *There is a statistically significant change (p < 0.05).
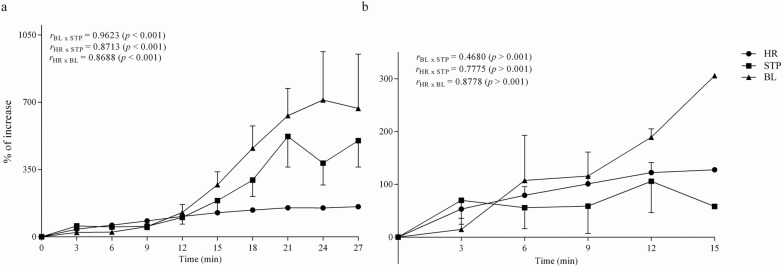
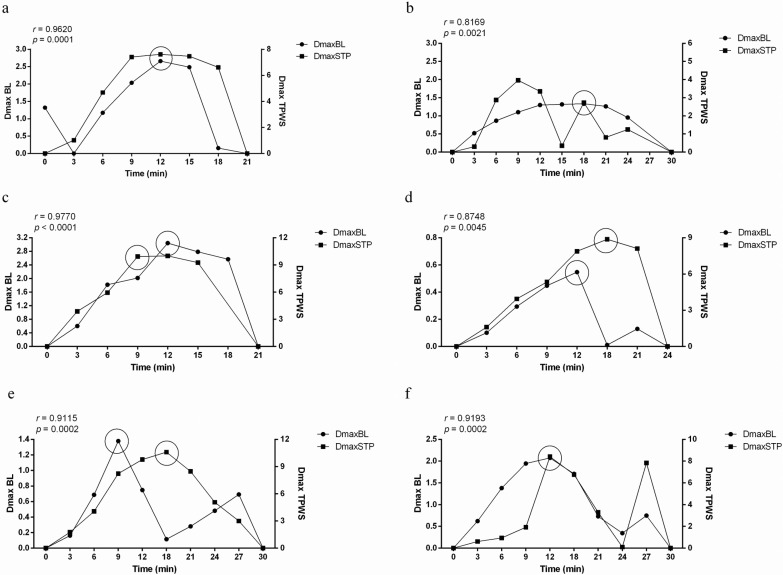
The relationship between HR, BL and STP during the exercise test is illustrated in Fig. 3. The EEA group showed a high correlation between HR and BL (r = 0.8688, p < 0.001), HR and STP (r = 0.8713, p < 0.001), and BL and STP (r = 0.9623, p < 0.001); the power calculation provided for this sample per effect size was approximately 0.8. However, in the PAE group there was no correlation between these parameters. The relationship between STP and BL during the exercise test, with the results from each participant in the EEA group, is shown in Fig. 4. Among the seven EEA, six showed a high correlation between STP and BL (r > 0.8, p < 0.005).
FIG. 3.
Correlation analysis between blood lactate (BL) and total protein of whole saliva (TPWS); heart rate (HR) and TPWS; HR and BL evaluated for elderly elite athletes (a) and physically active elderly men (b) during the exercise test.
FIG. 4.
Analysis of Pearson’s correlation coefficient between blood lactate (BL) and total protein of whole saliva (TPWS), and BL anaerobic threshold (AT) and TPWS anaerobic threshold (PAT) of six elderly elite athletes during the incremental exercise test.
The blood lactate anaerobic threshold (AT) and the salivary total protein anaerobic threshold (PAT) were determined using the Dmax method during the incremental exercise test. AT and PAT are indicated by circles; distances related to TPWS are set on the right y-axis; distances related to BL are set on the left y-axis; time in minutes is set on the x-axis.
DISCUSSION
Our results showed a constant and continuous increase of systolic and diastolic blood pressure, heart rate and rate pressure product, which were independent of the degree of physical performance of the volunteers (Fig. 1). Exercise protocols using ramps induce haemodynamic and uniform respiratory responses, which facilitate collecting information about exercise intensity at each stage of the test [20-23]. The volitional exhaustion was monitored by increases in slope and speed required by Bruce’s protocol, as well as in heart rate (HR), systolic blood pressure (SBP) and diastolic blood pressure (DBP). In addition, increases in BL and STP in both groups were observed (Fig. 2a). Previously, it has been demonstrated that there is a clear association between lactate production and muscle fatigue, [32, 33] and our data corroborate other studies monitoring aging athletes [32, 34, 35].
For physical exercise testing, the reference values of SBP and DBP are 200 and 77 mmHg, respectively, at the peak of exercise [36, 37]. Our findings showed a linear increase of SBP during the physical test in both EEA and PAE groups (Fig 1a). These results may be explained by cardiac chronotropic and inotropic effects. According to Rao and Kumar [38], the contribution of the inotropic response is predominantly neurogenic, being a result of decreased vagal outflow and later increased sympathetic activity. In relation to DBP, EEA showed lower values than PAE, with increases in the later stages caused by exercise stress. This may have occurred due to a greater degree of vasodilatation in exercised muscles, corresponding to a decline in peripheral resistance. It is likely that, under states of reduced psychological stress perception, the muscle blood flow, as well as the resistance to exercise, can be improved.
This is the first study to describe increases in the salivary total protein concentration (Fig. 2b) in a population of athletes over 59 years old. Our results showed that in this group, BL and STP changes, as a response to incremental physical exercise to volitional exhaustion, are similar to those observed in young athletes [18]. Increases in the concentrations of these parameters are related to the sympathetic action induced by intense physical exercise, as evidenced by a return to baseline values within 30 minutes [39-41]. An important highlight of the present study was that the BL and STP concentrations returned to base levels after 15 minutes.
Pearson’s correlation analysis showed a relationship between BL and STP concentrations only in the EEA group (Fig. 3a). A correlation between these parameters in the PAE group was not observed due to the few stages reached in the treadmill protocol, which opens up possibilities for further research using different exercise tests to evaluate STP in this population. Previous studies have used salivary compounds as biomarkers for monitoring exercise intensity, such as total protein, alpha-amylase and chromogranin A [13, 15, 16, 42, 43]. A study by Bortolini, De Agostini [18] reinforces the use of saliva to monitor the physical intensity of exercise by finding the STP threshold in young athletes. Thus, the STP may also provide a useful and non-invasive method to determine the anaerobic threshold during an incremental exercise test in aged professional athletes. Furthermore, we were able to detect the salivary total protein anaerobic threshold (PAT) in six of the seven elderly athletes, and three of them showed the PAT and BL threshold (AT) at the same point (Fig. 4). It is note worthy that the individual from Fig. 4b presented possible interference in STP caused by psychological stress in the early stages of the protocol [44], which does not correspond to the anaerobic threshold (observed only in the sixth stage for BL and STP). These results support the findings of Bortolini, De Agostini [18], which showed that AT and PAT appeared together in young athletes.
We were able to relate HR to STP in the EEA group. Our results are similar to those of Capranica, Lupo [45], who demonstrated a correlation between HR and salivary alpha-amylase in young individuals. This phenomenon occurs due to saliva production being modulated by the sympathetic nervous system. Since physical exercise stimulates sympathetic activity, a stimulus occurs in the synthesis and secretion of proteins in saliva, such as alpha-amylase – the most abundant protein in saliva [46], which justifies the use of salivary total protein to evaluate anaerobic threshold. Thus, the salivary threshold exhibited by the aged athletes may reflect the contribution of salivary alpha-amylase.
Another interesting point that should be taken into consideration is the way in which saliva secretion could also be modulated by the circadian cycle [47]. Exercise sessions performed in the morning require the athlete to perform a longer warm-up, which may affect the ventilatory responses, thus interfering with the salivary biomarker concentrations [48]. Therefore, our exercise protocol was performed in the evening (after 4:00 pm) to ensure consistency with the usual training schedule of our volunteers [46]. Furthermore, environmental
conditions were controlled. Walsh, Blannin [40] showed that an exercise protocol designed for 30ºC and 70% relative humidity achieves progressive acute dehydration. This study ensured adequate hydration of the volunteers and was designed to preserve the optimal environmental (well-ventilated room and temperature near 25ºC) and physiological conditions to allow participants to achieve 90% HR during the incremental exercise.
Little is known about salivary biomarkers in elderly athletes. Only one study, by Koibuchi and Suzuki [19], has previously described salivary biomarkers in physically active elderly men and non-elderly elite athletes, which encouraged us to evaluate athletes over 59 years of age. Our data are distinct from other studies that evaluated salivary biomarkers in normal elderly people, in that our population comprised professional athletes. Because of this, the parameters observed in this study are comparable to those of studies performed with young athletes.
One limitation of this study is the sample size (n = 7), and, from a statistical point of view, describing larger samples could provide more power. Nevertheless, we did find significant differences with a smaller sample and the power calculation provided for this sample per effect size was approximately 0.8. It should be noted that previous studies using master athletes of similar age suffered a similar limitation, such as Koibuchi and Suzuki [19] (n = 7), Mattern, Gutilla [5] (n = 9), Masse-Biron, Mercier [34] (n = 7) and Wollein, Bachl [49] (n = 7). Also worth noting here, it is not easy to identify athletes of this age who are still training intensely and who meet the rigorous exclusion and inclusion criteria and who are capable of completing the Bruce protocol.
In this study, correlations between salivary total protein and heart rate, as well as between salivary total protein and blood lactate, were observed in the elderly athletes subjected to a treadmill protocol. Salivary total protein analysis shows some advantage in convenience, cost and safety. Therefore, these results suggest that salivary total protein could be a useful, non-invasive and attractive biomarker for determining the anaerobic threshold during incremental exercise tests in elderly athletes, with practical applications in the health and sports areas. Thus, to relate salivary biomarkers with stress conditions in elderly athletes may help to monitor training intensity and indicate a better training programme for older people, as well as to strengthen the use of saliva as a diagnostic fluid.
CONCLUSIONS
The elderly athletes showed a high correlation between heart rate, blood lactate and salivary total protein, which was not observed in the elderly control group. The results of this study suggest that changes in salivary total protein could potentially be used as an alternative non-invasive method for determining anaerobic threshold in elderly athletes. Furthermore, saliva offers clear advantages over blood for monitoring exercise, since it is readily available and can be easily collected, handled and stored. The possibility of determining the anaerobic threshold through analysis of salivary composition is interesting and justifies further research using different physical exercises to substantiate the value and utility of salivary total protein as a biomarker of physical exercise intensity in elderly athletes.
Acknowledgments
The authors would like to thank the volunteers of the present study for their hard work and willingness to participle in this investigation. Also, we would like to thank the Physical and Recreational Activities Program for Elderly of the Federal University of Uberlandia (AFRID-FAEFI-UFU) and the Athletics Federation of Minas Gerais, Brazil for their support and assistance. FSE are grant recipients of National Council for Scientific and Technological Development (CNPq – 308965/2015-9).
Disclosure of potential conflicts of interest
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
REFERENCES
- 1.Reed JL, Pipe AL. Practical Approaches to Prescribing Physical Activity and Monitoring Exercise Intensity. Can J Cardiol. 2016;32(4):514–522. doi: 10.1016/j.cjca.2015.12.024. [DOI] [PubMed] [Google Scholar]
- 2.Wasserman K, McIlroy MB. Detecting the threshold of anaerobic metabolism in cardiac patients during exercise. Am J Cardiol. 1964;14(6):844–852. doi: 10.1016/0002-9149(64)90012-8. [DOI] [PubMed] [Google Scholar]
- 3.Ballak SB, Degens H, de Haan A, Jaspers RT. Aging related changes in determinants of muscle force generating capacity: a comparison of muscle aging in men and male rodents. Ageing Res Rev. 2014;14:43–55. doi: 10.1016/j.arr.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 4.Brooks SV, Faulkner JA. Skeletal muscle weakness in old age: underlying mechanisms. Med Sci Sports Exerc. 1994;26(4):432–439. [PubMed] [Google Scholar]
- 5.Mattern CO, Gutilla MJ, Bright DL, Kirby TE, Hinchcliff KW, Devor ST. Maximal lactate steady state declines during the aging process. J Appl Physiol. 2003;95(6):2576–2582. doi: 10.1152/japplphysiol.00298.2003. [DOI] [PubMed] [Google Scholar]
- 6.Affoo RH, Foley N, Garrick R, Siqueira WL, Martin RE. Meta-Analysis of Salivary Flow Rates in Young and Older Adults. J Am Geriatr Soc. 2015;63(10):2142–2151. doi: 10.1111/jgs.13652. [DOI] [PubMed] [Google Scholar]
- 7.Vissink A, Spijkervet FK, Van Nieuw Amerongen A. Aging and saliva: a review of the literature. Spec Care Dentist. 1996;16(3):95–103. doi: 10.1111/j.1754-4505.1996.tb00842.x. [DOI] [PubMed] [Google Scholar]
- 8.Ben-Aryeh H, Shalev A, Szargel R, Laor A, Laufer D, Gutman D. The salivary flow rate and composition of whole and parotid resting and stimulated saliva in young and old healthy subjects. Biochem Med Metab Biol. 1986;36(2):260–265. doi: 10.1016/0885-4505(86)90134-9. [DOI] [PubMed] [Google Scholar]
- 9.Shaila M, Pai GP, Shetty P. Salivary protein concentration, flow rate, buffer capacity and pH estimation: A comparative study among young and elderly subjects, both normal and with gingivitis and periodontitis. J Indian Soc Periodontol. 2013;17(1):42–46. doi: 10.4103/0972-124X.107473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malamud D. Saliva as a diagnostic fluid. Dent Clin North Am. 2011;55(1):159–178. doi: 10.1016/j.cden.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nater UM, La Marca R, Florin L, Moses A, Langhans W, Koller MM, et al. Stress-induced changes in human salivary alpha-amylase activity - associations with adrenergic activity. Psychoneuroendocrinology. 2006;31(1):49–58. doi: 10.1016/j.psyneuen.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Chicharro JL, Lucia A, Perez M, Vaquero AF, Urena R. Saliva composition and exercise. Sports Med. 1998;26(1):17–27. doi: 10.2165/00007256-199826010-00002. [DOI] [PubMed] [Google Scholar]
- 13.Chicharro JL, Perez M, Carvajal A, Bandres F, Lucia A. The salivary amylase, lactate and electromyographic response to exercise. Jpn J Physiol. 1999;49(6):551–554. doi: 10.2170/jjphysiol.49.551. [DOI] [PubMed] [Google Scholar]
- 14.Calvo F, Chicharro JL, Bandres F, Lucia A, Perez M, Alvarez J, et al. Anaerobic threshold determination with analysis of salivary amylase. Can J Appl Physiol. 1997;22(6):553–561. doi: 10.1139/h97-035. [DOI] [PubMed] [Google Scholar]
- 15.Bocanegra OL, Diaz MM, Teixeira RR, Soares SS, Espindola FS. Determination of the lactate threshold by means of salivary biomarkers: chromogranin A as novel marker of exercise intensity. Eur J Appl Physiol. 2012;112(9):3195–3203. doi: 10.1007/s00421-011-2294-4. [DOI] [PubMed] [Google Scholar]
- 16.Diaz MM, Bocanegra OL, Teixeira RR, Soares SS, Espindola FS. Salivary nitric oxide and alpha-amylase as indexes of training intensity and load. Int J Sports Med. 2013;34(1):8–13. doi: 10.1055/s-0032-1316318. [DOI] [PubMed] [Google Scholar]
- 17.Segura R, Javierre C, Ventura JL, Lizarraga MA, Campos B, Garrido E. A new approach to the assessment of anaerobic metabolism: measurement of lactate in saliva. Br J Sports Med. 1996;30(4):305–309. doi: 10.1136/bjsm.30.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bortolini MJ, De Agostini GG, Reis IT, Lamounier RP, Blumberg JB, Espindola FS. Total protein of whole saliva as a biomarker of anaerobic threshold. Res Q Exerc Sport. 2009;80(3):604–610. doi: 10.1080/02701367.2009.10599599. [DOI] [PubMed] [Google Scholar]
- 19.Koibuchi ERI, Suzuki Y. Exercise upregulates salivary amylase in humans (Review) Exp Ther Med. 2014;7(4):773–777. doi: 10.3892/etm.2014.1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bires AM, Lawson D, Wasser TE, Raber-Baer D. Comparison of Bruce treadmill exercise test protocols: is ramped Bruce equal or superior to standard bruce in producing clinically valid studies for patients presenting for evaluation of cardiac ischemia or arrhythmia with body mass index equal to or greater than 30? J Nucl Med Technol. 2013;41(4):274–278. doi: 10.2967/jnmt.113.124727. [DOI] [PubMed] [Google Scholar]
- 21.Will PM, Walter JD. Exercise testing: improving performance with a ramped Bruce protocol. Am Heart J. 1999;138(6 Pt 1):1033–1037. doi: 10.1016/s0002-8703(99)70067-0. [DOI] [PubMed] [Google Scholar]
- 22.Mead WF. Maximal exercise testing-- Bruce protocol. J Fam Pract. 1979;9(3):479–490. [PubMed] [Google Scholar]
- 23.Maeder M, Wolber T, Atefy R, Gadza M, Ammann P, Myers J, et al. A nomogram to select the optimal treadmill ramp protocol in subjects with high exercise capacity: validation and comparison with the Bruce protocol. J Cardiopulm Rehabil Prev. 2006;26(1):16–23. doi: 10.1097/00008483-200601000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Bruce RA. Exercise testing of patients with coronary heart disease. Principles and normal standards for evaluation. Ann Clin Res. 1971;3(6):323–332. [PubMed] [Google Scholar]
- 25.Cheng B, Kuipers H, Snyder AC, Keizer HA, Jeukendrup A, Hesselink M. A new approach for the determination of ventilatory and lactate thresholds. Int J Sports Med. 1992;13(7):518–522. doi: 10.1055/s-2007-1021309. [DOI] [PubMed] [Google Scholar]
- 26.Von Duvillard SP, Braun WA, Markofski M, Beneke R, Leithauser R. Fluids and hydration in prolonged endurance performance. Nutrition. 2004;20(7- 8):651–656. doi: 10.1016/j.nut.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Popkin BM, D’Anci KE, Rosenberg IH. Water, Hydration and Health. Nutr Rev. 2010;68(8):439–458. doi: 10.1111/j.1753-4887.2010.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noakes TD. Drinking guidelines for exercise: what evidence is there that athletes should drink „as much as tolerable”, „to replace the weight lost during exercise” or „ad libitum”? J Sports Sci. 2007;25(7):781–796. doi: 10.1080/02640410600875036. [DOI] [PubMed] [Google Scholar]
- 29.Convertino VA, Armstrong LE, Coyle EF, Mack GW, Sawka MN, Senay LC, Jr, et al. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc. 1996;28(1):i–vii. doi: 10.1097/00005768-199610000-00045. [DOI] [PubMed] [Google Scholar]
- 30.Navazesh M. Methods for collecting saliva. Ann N Y Acad Sci. 1993;694:72–77. doi: 10.1111/j.1749-6632.1993.tb18343.x. [DOI] [PubMed] [Google Scholar]
- 31.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1006/abio.1976.9999. [DOI] [PubMed] [Google Scholar]
- 32.Garcia-Pinillos F, Soto-Hermoso VM, Latorre-Roman PA. Acute Physiological and Thermoregulatory Responses to Extended Interval Training in Endurance Runners: Influence of Athletic Performance and Age. J Hum Kinet. 2015;49:209–217. doi: 10.1515/hukin-2015-0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Facey A, Irving R, Dilworth L. Overview of Lactate Metabolism and the Implications for Athletes. Am J Sports Sci Med. 2013;1(3):42–46. [Google Scholar]
- 34.Masse-Biron J, Mercier J, Collomp K, Hardy JM, Prefaut C. Age and training effects on the lactate kinetics of master athletes during maximal exercise. Eur J Appl Physiol Occup Physiol. 1992;65(4):311–315. doi: 10.1007/BF00868133. [DOI] [PubMed] [Google Scholar]
- 35.Wiswell RA, Hawkins SA, Jaque SV, Hyslop D, Constantino N, Tarpenning K, et al. Relationship between physiological loss, performance decrement, and age in master athletes. J Gerontol A Biol Sci Med Sci. 2001;56(10):M618–626. doi: 10.1093/gerona/56.10.m618. [DOI] [PubMed] [Google Scholar]
- 36.Robinson TE, Sue DY, Huszczuk A, Weiler-Ravell D, Hansen JE. Intra-arterial and cuff blood pressure responses during incremental cycle ergometry. Med Sci Sports Exerc. 1988;20(2):142–149. doi: 10.1249/00005768-198820020-00007. [DOI] [PubMed] [Google Scholar]
- 37.Wasserman K, Hansen JE, Sue DY, Stringer WW, Whipp BJ. Can J Cardiol. 4. Lippincott Willians and Wilkins; 2004. Principles of exercise testing and interpretation: including pathophysiology and clinical applications. [Google Scholar]
- 38.Rao NS, Kumar JV. Role of Perceptual Factors on Endurance Profiles on Treadmill Exercise. J Clin Diagn Res. 2015;9(6):Cc13–15. doi: 10.7860/JCDR/2015/12359.6063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gallina S, Di Mauro M, D’Amico MA, D’Angelo E, Sablone A, Di Fonso A, et al. Salivary chromogranin A, but not alpha-amylase, correlates with cardiovascular parameters during high-intensity exercise. Clin Endocrinol. 2011;75(6):747–752. doi: 10.1111/j.1365-2265.2011.04143.x. [DOI] [PubMed] [Google Scholar]
- 40.Walsh NP, Blannin AK, Clark AM, Cook L, Robson PJ, Gleeson M. The effects of high-intensity intermittent exercise on saliva IgA, total protein and alpha-amylase. J Sports Sci. 1999;17(2):129–134. doi: 10.1080/026404199366226. [DOI] [PubMed] [Google Scholar]
- 41.Walsh NP, Laing SJ, Oliver SJ, Montague JC, Walters R, Bilzon JL. Saliva parameters as potential indices of hydration status during acute dehydration. Med Sci Sports Exerc. 2004;36(9):1535–1542. doi: 10.1249/01.mss.0000139797.26760.06. [DOI] [PubMed] [Google Scholar]
- 42.Chicharro JL, Legido JC, Alvarez J, Serratosa L, Bandres F, Gamella C. Saliva electrolytes as a useful tool for anaerobic threshold determination. Eur J Appl Physiol Occup Physiol. 1994;68(3):214–218. doi: 10.1007/BF00376769. [DOI] [PubMed] [Google Scholar]
- 43.de Oliveira VN, Bessa A, Lamounier RP, de Santana MG, de Mello MT, Espindola FS. Changes in the salivary biomarkers induced by an effort test. Int J Sports Med. 2010;31(6):377–381. doi: 10.1055/s-0030-1248332. [DOI] [PubMed] [Google Scholar]
- 44.Takai N, Yamaguchi M, Aragaki T, Eto K, Uchihashi K, Nishikawa Y. Effect of psychological stress on the salivary cortisol and amylase levels in healthy young adults. Arch Oral Biol. 2004;49(12):963–968. doi: 10.1016/j.archoralbio.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 45.Capranica L, Lupo C, Cortis C, Chiodo S, Cibelli G, Tessitore A. Salivary cortisol and alpha-amylase reactivity to taekwondo competition in children. Eur J Appl Physiol. 2012;112(2):647–652. doi: 10.1007/s00421-011-2023-z. [DOI] [PubMed] [Google Scholar]
- 46.Rantonen PJ, Meurman JH. Correlations between total protein, lysozyme, immunoglobulins, amylase, and albumin in stimulated whole saliva during daytime. Acta Odontol Scand. 2000;58(4):160–165. doi: 10.1080/000163500429154. [DOI] [PubMed] [Google Scholar]
- 47.Nunes LA, Brenzikofer R, Macedo DV. Reference intervals for saliva analytes collected by a standardized method in a physically active population. Clin Biochem. 2011;44(17-18):1440–1444.. doi: 10.1016/j.clinbiochem.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 48.Martin L, Doggart AL, Whyte GP. Comparison of physiological responses to morning and evening submaximal running. J Sports Sci. 2001;19(12):969–976. doi: 10.1080/026404101317108471. [DOI] [PubMed] [Google Scholar]
- 49.Wollein W, Bachl N, Prokop L. Endurance capacity of trained older aged athletes. Eur Heart J. 1984;5(Suppl E):21–25. doi: 10.1093/eurheartj/5.suppl_e.21. [DOI] [PubMed] [Google Scholar]