Short abstract
Objective
Oxidative stress appears to be a key factor in the pathogenesis of allergic diseases and a potential therapeutic target in allergy treatment. Allergic diseases are reportedly associated with reduced plasma levels of ascorbate, which is a key physiological antioxidant. Ascorbate prevents excessive inflammation without reducing the defensive capacity of the immune system.
Methods
An interim analysis of a multicenter, prospective, observational study was conducted to investigate the change in disease-specific and nonspecific symptoms (fatigue, sleep disorders, depression, and lack of mental concentration) during adjuvant treatment with intravenous vitamin C (Pascorbin®; Pascoe, Giessen, Germany) in 71 patients with allergy-related respiratory or cutaneous indications.
Results
Between the start and end of treatment, the mean sum score of three disease-specific symptoms decreased significantly by 4.71 points and that of four nonspecific symptoms decreased significantly by 4.84 points. More than 50% of patients took no other allergy-related medication besides vitamin C.
Conclusions
Our observations suggest that treatment with intravenous high-dose vitamin C reduces allergy-related symptoms. Our observations form a basis for planning a randomized controlled clinical trial to obtain more definitive evidence of the clinical relevance of our findings. We also obtained evidence of ascorbate deficiency in allergy-related diseases.
Trial registration: Clinical Trials NCT02422901.
Keywords: Ascorbic acid, allergic rhinitis, allergic asthma, dermatitis, eczema, human, pruritus, intravenous administration
Introduction
The management of allergic diseases represents a major health challenge for the 21st century. Complementary and alternative approaches are under investigation.1–4 A recent review of the molecular redox mechanisms in asthma concluded that oxidative stress plays not only a key role in the pathophysiology of asthma but is also a promising therapeutic target.5
During the stages of acute allergic inflammation and in allergy-related respiratory or skin infections, the production of reactive oxygen species (ROS) by membrane-associated NADPH oxidase proteins of neutrophils, macrophages, or eosinophils5–7 plays an important role.7 Although ROS are physiologically produced to eliminate pathogens and invading microorganisms,6 they represent a substantial force in individuals with allergy by promoting pro-inflammatory conditions.8
Interestingly, NADPH oxidase proteins are also of particular relevance in pollens and seem to provide a signal that augments antigen-induced allergic airway inflammation.9 In addition, histamine production and release seems to be triggered by inflammation and ROS,10 causing mast cell degranulation11,12 and/or induction of histidine decarboxylase.13
Identifying ways to suppress the pro-inflammatory activity of ROS and limit potential damage to biological molecules seems to be of significant clinical relevance. A targeted antioxidant intervention to counteract pathophysiological increases in ROS can be achieved by increasing the body’s low-molecular-weight antioxidants by dietary or pharmacological interventions.14 Vitamin C (ascorbate) is one of the most effective aqueous-phase antioxidants in human blood plasma for protection against oxidative stress.15–17 Elevating the plasma concentration of ascorbate, which can only be achieved by intravenous (iv) administration,18 is a popular complementary treatment in the management of inflammatory conditions.19,20
We obtained data from the present multicenter, prospective, observational study to document the clinical effects of high-dose iv vitamin C in the treatment of patients with known respiratory or cutaneous allergies. We obtained findings that are novel to the best of our knowledge.
Materials and methods
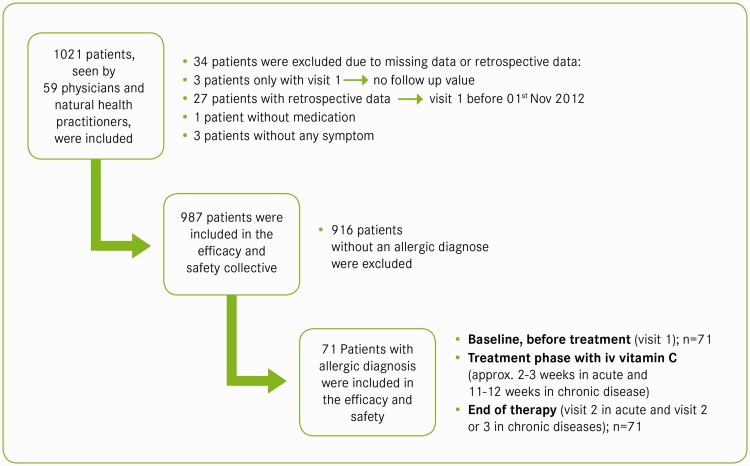
This interim subgroup analysis of a long-term (November 2012 to October 2022) observational study was performed to document the use of Pascorbin® 7.5 g (authorized medicinal product containing 7.5 g ascorbate; Pascoe pharmazeutische Präparate GmbH, Giessen, Germany) in patients with allergic diseases for the reduction of symptoms related to oxidative stress and vitamin C deficiency. Assessment of treatment dosages and treatment tolerance were further aims. To obtain data regarding changes in the application behavior for the investigated product, a 10-year period for submission of case report forms (CRFs) was chosen. All consecutive patients who received elective iv ascorbate treatment for an acute or chronic allergic condition (diagnosis of allergic diseases was previously confirmed and documented by the attending physician) from 1 November 2012 to 15 September 2014 were included in this study. The patients’ characteristics and the criteria for data selection are shown in Figure 1 and Table 1, respectively. Vitamin C deficiency was diagnosed by laboratory tests or symptom investigation. The patients were informed of possible unwanted adverse effects and the anonymity of the data processing, which was assured by a signed statement. All patients signed a statement of agreement to use and publish their data for the observational study.
Figure 1.
Flowchart of study patients.
Table 1.
Eligibility criteria
| Inclusion criteria |
| Age of >12 years |
| Treatment with vitamin C infusion (7.5 g) due to vitamin C deficiency |
| Patient’s statement of agreement to use and publish their data for the observational study |
| Exclusion criteria (anamnestic) |
| Oxalate urolithiasis, nephrolithiasis |
| Renal insufficiency |
| Iron storage disease (thalassemia, hemochromatosis, sideroblastic anemia) |
| Erythrocytic glucose-6-phosphate dehydrogenase deficiency |
| Pregnancy and lactation |
| Hypersensitivity to an ingredient |
The study design and concept are based on the recommendations of the Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM, German Federal Institute for Drugs and Medical Devices) and the Paul-Ehrlich-Institute in accordance with German laws and the principles of the Declaration of Helsinki and Good Clinical Practice. The study was registered at the United States Clinical Trial registry (registration number: NCT02422901).
The participating physicians and natural health practitioners were informed about the scientific basis of this observational study and were requested to complete a detailed form indicating the patients’ clinical characteristics, diagnosis, dosage, and disease symptoms for any elective use of iv vitamin C treatment. Depending on the duration and state of the disease, acute or chronic allergic diseases were differentiated by the physicians, and two separate CRFs were available. The treating physician used the CRF for acute disease if the symptomatology started within the previous 4 weeks and the patient was symptom-free prior to that time (e.g., allergic rhinoconjunctivitis after the start of the pollen season). The characteristics of patients with chronic disease were documented using a different CRF if recurrent symptomatology had been present for longer than the previous 4 weeks (several patients had allergic disease symptoms for several months, such as those with atopic eczema). Patients with psoriasis as the primary diagnosis were included in this interim subgroup analysis because concomitant allergic disease was often present. Furthermore, the symptoms are very similar because of the inflammatory character of the disease.
Data were collected before the start of vitamin C treatment (visit 1, baseline) and after the end of treatment in patients with acute disease (visit 2, approximately 2–3 weeks). In patients with chronic disease, data were collected after an interim observation at 6 to 8 weeks (visit 2) and after the end of treatment (10–14 weeks) (visit 3).
Each patient received iv vitamin C (Pascorbin® 7.5 g/50 mL) diluted in a suitable carrier solution such as 100 mL NaCl 0.9%. Because the vitamin C amount needed to treat a deficiency state depends on different parameters (such as the extent of the deficiency, body weight, age, glomerular filtration rate, and continued metabolic turnover due to oxidative stress), up to 7.5 g can be administered according to the summary of product characteristics. To avoid a shortage, the doctors participating in the study decided to use 7.5 g because vitamin C is consumed continuously due to oxidative stress produced by the allergic response and an excess is given during infusion to saturate tissue. This is a commonly used procedure because vitamin C is a well-tolerated substance that is not accumulated in the body but rapidly eliminated via the kidneys.
The use of other remedies was documented, primarily antiallergic reagents (antihistamines; topical, inhaled, or systemic corticosteroids; beta-2 sympathomimetics; parasympatholytics; and leukotriene receptor antagonists) and antibiotics.
Primary endpoints
The main study parameter was the response of symptoms (change in score) during the period of iv vitamin C treatment. Therefore, at the beginning (visit 1) and end (visit 2 for acute disease, visit 3 for chronic disease) of the observation period, the severity of each symptom was scored on a 4-point Likert scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe) by the treating physician or natural health practitioner.21–23
A one-sample t-test (two-sided, with α = 0.05) was used to assess the changes between baseline and the final visit (calculated as post-treatment minus pretreatment). The statistical analyses were performed by an independent statistician. Subgroup analyses were carried out for the following categories:
- Type of disease
- ○ Acute
- ○ Chronic
- Diagnosis (International Classification of Diseases, 10th revision)
- ○ Diseases of the respiratory system (J00–J99)
- ○ Diseases of the skin and subcutaneous tissue (L00–L99)
The changes in the symptom scores were classified as improvement, no change, and deterioration of symptoms (as designated on the CRFs). In the symptom evaluation, only data of those patients who displayed the symptom and for whom pretreatment and post-treatment assessments were documented were included.
Disease-specific symptoms
The disease-specific symptoms were not predetermined. For each patient, up to three of the most prominent symptoms were assessed as free text and then assigned to appropriate categories (MedDRA coding, version 15.1 and higher) after data collection. For the 4-point Likert scale (0–3 points) of symptom severity, the range of possible sum scores was 0 to 9 points. The three most frequently documented symptoms in the study population were assessed in detail.
Nonspecific symptoms
Four nonspecific symptoms (fatigue, sleep disorders, depression, and lack of mental concentration) as assessed by means of the 4-point Likert scale (0–3 points) had a possible sum score ranging from 0 to 12 points.
Pain
Every type of pain (e.g., headache, abdominal, or cutaneous pain) was evaluated by means of a numeric rating scale for pain ranging from 0 (no pain) to 10 (extreme pain).24
Secondary outcome measures
Assessment of efficacy and tolerability of previous medication and of vitamin C
The efficacy of the previous/current therapies and vitamin C was judged by the physicians on a five-category scale:
Very good efficacy (symptoms eliminated)
Good efficacy (symptoms substantially improved)
Moderate efficacy (symptoms slightly improved)
No effect (symptoms unchanged)
No effect (symptoms worsened)
The tolerability was judged on the basis of a two-category scale:
Very well tolerated (no side effects)
Poorly tolerated (side effects)
Ascorbate concentration
Serum ascorbate concentrations were measured before the start of vitamin C treatment (at visit 1). After collection, the serum samples were cooled, centrifuged, and mixed with a stabilization and precipitating reagent. They were then frozen for storage until analysis. Reversed-phase high-performance liquid chromatography (ProntoSIL C18 AQ, 5 µm; Bischoff Chromatography, Atlanta, GA, USA) was used to analyze the serum ascorbate levels. The intra-assay coefficients of variation were 5.6% (0.44 mg/dL) and 4.1% (1.8 mg/dL), and the inter-assay coefficients of variation were 8.8% and 5.9%.
Safety
Safety of the vitamin C treatment was assessed by the attending physician in terms of adverse events and possible relatedness of such events to vitamin C treatment, underlying disease, or co-medication.
Results
In total, 71 patients with a mean age ± standard deviation of 43.14 ± 17.86 years and an almost even sex distribution were identified using the inclusion criteria for previously confirmed allergic respiratory disease (56.3%) or allergic cutaneous disease (43.7%) (Table 2). The frequency of different types of allergic diseases and the duration of acute and chronic diseases are documented in Table 2. Endocrine, nutritional, and metabolic diseases were the most frequently reported concomitant diseases (E00–E90; n = 8), followed by diseases of the digestive system (K00–K93; n = 7) and diseases of the circulatory system (I00–I99; n = 5) and respiratory system (J00–J99; n = 5).
Table 2.
Baseline demographic and clinical characteristics of patients (n = 71)
| Age, years | 43.14 ± 17.86, (12–79) |
| Sex | |
| Male | 38 (53.5%) |
| Female | 33 (46.5%) |
| Body mass index, kg/m2 | 24.95 ± 3.61, (18.4–33.6) |
| Inclusion diagnosis (ICD-10 category) | |
| J00–J99: Diseases of the respiratory system | 40 (56.3%) |
| J30: Vasomotor and allergic rhinitis | 30 (75.0%) |
| J45: Bronchial asthma | 10 (25.0%) |
| L00–L99: Diseases of the skin and subcutis | 31 (43.7%) |
| L20–L30: Dermatitis and eczema | 19 (61.3%) |
| L40–L41 Psoriasis and parapsoriasis | 7 (22.6%) |
| L50: Urticaria | 5 (16.1%) |
| Proportion of acute and chronic diseases | |
| Respiratory allergic disease (acute) | 26 (65.0%) |
| Respiratory allergic disease (chronic) | 14 (35.0%) |
| Cutaneous allergic disease (acute) | 11 (35.5%) |
| Cutaneous allergic disease (chronic) | 20 (64.5%) |
| Concomitant disease | |
| Yes | 24 (33.8%) |
| No | 47 (66.2%) |
| Duration of inclusion diagnosis, years | |
| Acute | 0.07 ± 0.13 |
| Chronic | 19.23 ± 18.92 |
| Intake of antiallergic reagents | |
| Yes | 25 (35.2%) |
| No | 46 (64.8%) |
| Intake of antibiotics | |
| Yes | 11 (15.5%) |
| No | 60 (84.5%) |
| Number of antiallergic reagents or antibiotics | |
| 1 | 21 (61.8%) |
| 2 | 7 (20.6%) |
| 3 | 4 (11.8%) |
| ≥4 | 2 (5.9%) |
Data are presented as mean ± standard deviation, range, or n (%).
ICD-10: International Classification of Diseases, 10th revision.
Of patients included in the interim subgroup analysis, 45.1% (32/71) received additional treatment with antiallergic reagents or antibiotics (Table 2).
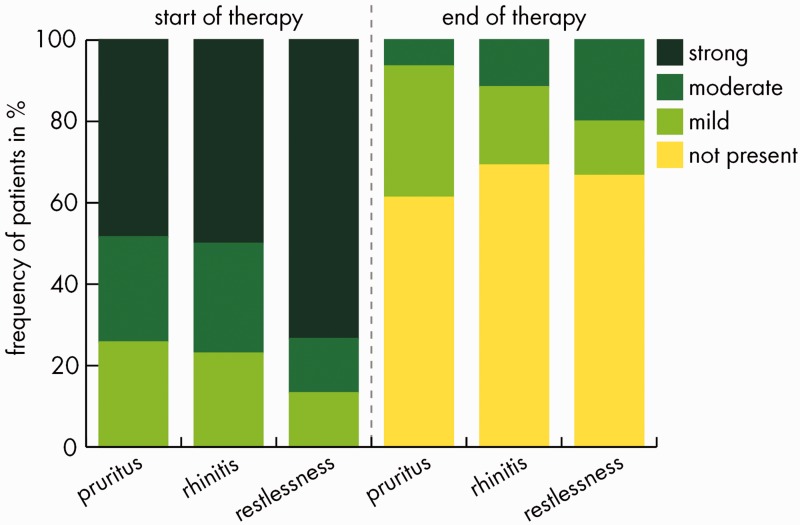
Disease-specific symptoms
Two patients (both with psoriasis) had no disease-specific symptoms throughout the observation period; they were therefore excluded from the analysis. Thus, 69 patients were included in the analysis and had a total of 182 symptoms (average of 2.6 symptoms/patient), corresponding to 52 preferred terms (MedDRA coding, version 15.1 and higher). The three most frequently preferred terms were pruritus (n = 31), rhinitis (n = 26), and restlessness (n = 15). During the observation period, symptoms improved in 67 (97.1%) of the 69 analyzed patients, and 173 (95.1%) of the 182 recorded disease-specific symptoms improved. The mean sum score of the disease-specific clinical symptoms decreased significantly from 5.91 at baseline to 1.20 at the final visit (mean change, −4.71, p < 0.0001). Subgroup analyses revealed significant changes for each diagnosis (respiratory or cutaneous) and for acute and chronic disease (p < 0.0001) (Table 3).
Table 3.
Sum scores (0–9 points) for specific symptoms (n = 69)
| Total population and subgroups | Start of treatment | End of treatment | Change (beginning – end) | Probability estimate* |
|---|---|---|---|---|
| Total population | 5.91 | 1.20 | 4.71 | p < 0.0001 |
| Respiratory allergic diseases | 5.58 | 1.08 | 4.50 | p < 0.0001 |
| Cutaneous allergic diseases | 6.38 | 1.38 | 5.00 | p < 0.0001 |
| Acute diseases | 5.78 | 1.46 | 4.32 | p < 0.0001 |
| Chronic diseases | 6.06 | 0.91 | 5.16 | p < 0.0001 |
*Student’s t-test.
Analysis of the most frequently recorded symptoms revealed symptom improvement rates (in terms of the number of patients) during the observation period of 29/31 (93.5%), 25/26 (96.2%), and 15/15 (100%) for pruritus, rhinitis, and restlessness, respectively (Table 4).
Table 4.
Changes in the three most frequently recorded disease-specific symptoms, baseline/visit 1 vs. end of observation period
|
Pruritus |
Rhinitis |
Restlessness |
||||
|---|---|---|---|---|---|---|
| n | %* | n | %* | n | %* | |
| Improvement | 29 | 93.5 | 25 | 96.2 | 15 | 100.0 |
| No change | 2 | 6.5 | 1 | 3.8 | 0 | 0.0 |
| Deterioration | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Valid data | 31 | 100.0 | 26 | 100.0 | 15 | 100.0 |
| Missing data | 38 | – | 43 | – | 54 | – |
*Valid data analysis; missing data refer to patients without the symptom because the treating physician selected for each patient the three most prominent symptoms among all allergic symptoms.
The fraction of symptom-free patients and patients with only mild symptoms at the end of the observation period was 29/31 (93.6%) for pruritus, 23/26 (88.5%) for rhinitis, and 12/15 (80.0%) for restlessness at the end of the observation (Figure 2).
Figure 2.
Frequencies of the three most frequently recorded disease-specific symptoms. The severity of each symptom was documented on a 4-point Likert scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe) by the treating physician or natural health practitioner at start and end of treatment. Valid data for pruritus, n = 31; for rhinitis, n = 26; and for restlessness, n = 15.
Regarding the percentage of patients with an improvement in the symptom sum score, there was a tendency for greater improvement in the patients receiving no antiallergic and/or antibiotic medication additionally to vitamin C (93.8% vs. 100%).
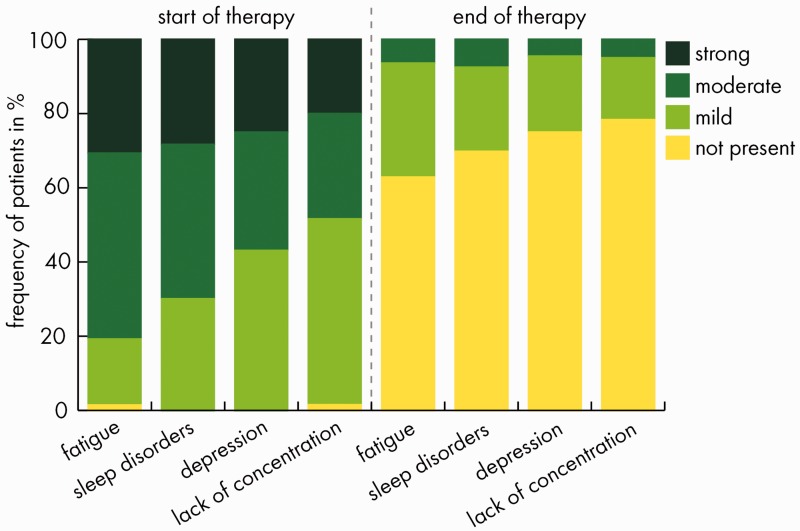
Nonspecific symptoms
In total, nonspecific symptoms (fatigue, sleep disorders, depression, and lack of mental concentration) were analyzed in 70 patients because 1 patient had no nonspecific symptoms. The mean sum score of nonspecific clinical symptoms decreased from 5.93 at baseline to 1.09 at the final visit (mean change, −4.84; p < 0.0001). Subgroup analyses revealed significant changes for each diagnosis (respiratory or cutaneous) and for acute and chronic disease (p < 0.0001) (Table 5).
Table 5.
Sum scores (0–12 points) for nonspecific symptoms (fatigue, sleep disorders, depression, and lack of concentration) (n = 70)
| Total population and subgroups | Start of treatment | End of treatment | Change (beginning – end) | Probability estimate* |
|---|---|---|---|---|
| Total population | 5.93 | 1.09 | 4.84 | p < 0.0001 |
| Respiratory allergic diseases | 5.10 | 1.10 | 4.00 | p < 0.0001 |
| Cutaneous allergic diseases | 6.97 | 1.06 | 5.90 | p < 0.0001 |
| Acute diseases | 4.97 | 1.35 | 3.62 | p < 0.0001 |
| Chronic diseases | 7.00 | 0.79 | 6.21 | p < 0.0001 |
*Student’s t-test.
Nonspecific symptoms were found to decrease in 65 (92.9%) of 70 of patients during the observation period. The fraction of symptom-free patients and patients with only mild symptoms at the end of the observation was >90% for all nonspecific symptoms. The degrees of improvement of individual symptoms are presented in Table 6.
Table 6.
Changes in nonspecific symptoms, baseline/visit 1 vs. end of observation period
|
Tiredness/ fatigue |
Sleep disorders |
Depression |
Lack of concentration |
|||||
|---|---|---|---|---|---|---|---|---|
| n | %* | n | %* | n | %* | n | %* | |
| Improvement | 58 | 93.5 | 49 | 92.5 | 42 | 95.5 | 55 | 91.7 |
| No change | 3 | 4.8 | 4 | 7.5 | 2 | 4.5 | 4 | 6.7 |
| Deterioration | 1 | 1.6 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 |
| Valid data | 62 | 100.0 | 53 | 100.0 | 44 | 100.0 | 60 | 100.0 |
| Missing data | 8 | – | 17 | – | 26 | – | 10 | – |
*Valid data analysis; missing data refer to patients without the symptom at the beginning of treatment.
The frequencies of the nonspecific symptoms, according to the degree of manifestation, are shown in Figure 3.
Figure 3.
Frequency of nonspecific symptoms (tiredness/fatigue, sleep disorders, depression, and lack of mental concentration). The severity of each symptom was documented on a 4-point Likert scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe) by the treating physician or natural health practitioner at start and end of treatment. Valid data for tiredness/fatigue, n = 62; for sleep disorders, n = 53; for depression, n = 44; and for lack of mental concentration, n = 60.
Regarding the percentage of patients with an improved sum score, there was a tendency for greater improvement in the patients receiving no antiallergic and/or antibiotic medication additionally to vitamin C (90.3% vs. 94.9%).
Any type of associated pain
Of the 70 analyzed patients, 48 (68.6%) experienced pain of some type. The initial mean value of 3.8 ± 2.8 on the numeric rating scale decreased to 0.7 ± 1.3 after treatment.
Duration and dosage of vitamin C
Treatment was performed during a mean of 3.2 weeks for acute disease and 11.9 weeks for chronic disease. The mean number of vitamin C infusions was 7 in the acute disease group and 26 in the chronic disease group. Because the vitamin C infusion was administered mainly over the complete treatment period, the frequency of infusions was two to three per week for both acute and chronic states.
Subgroup analysis of serum ascorbate concentrations
Serum ascorbate concentrations were measured in 21 of 71 patients (30%) prior to high-dose vitamin C treatment. The reason for this elective measurement lies in the fact that ascorbate measurements are not part of standard clinical laboratory assessments, and the costs of analysis are not reimbursable in Germany. Clinical vitamin C deficiency (scurvy) is defined as a plasma concentration of <0.2 mg/dL, and subclinical deficiency is defined as a plasma concentration of <0.5 mg/dL.25,26 The latter vitamin C depletion applied to 15 of 21 (71.4%) of the analyzed patients. The mean serum ascorbate level was 0.34 mg/dL with a median of 0.2 mg/dL (Table 7).
Table 7.
Vitamin C serum levels at baseline before treatment with Pascorbin®
| Subgroups | Vitamin C (mg/dL) |
|---|---|
| Total (n = 21) | 0.34 ± 0.28 |
| Acute diseases (n = 13) | 0.40 ± 0.31 |
| Chronic diseases (n = 8) | 0.24 ± 0.19 |
| Respiratory diseases (n = 10) | 0.45 ± 0.34 |
| Cutaneous diseases (n = 11) | 0.24 ± 0.17 |
Data are presented as mean ± standard deviation. Clinical vitamin-C-deficiency (ascorbate), <0.2 mg/dL; subclinical deficiency, <0.5 mg/dL.
Efficacy and tolerability of prior medication and vitamin C treatment
Of the 71 investigated patients, 51 (71.8%) reported the use of antiallergic medication before the start of vitamin C treatment. Assessment of the efficacy and tolerability of prior medication versus vitamin C is documented in Table 8. Notably, at the end of the observation period, 69% of the patients (n = 49) (data not shown) treated with vitamin C were assessed as having very good treatment efficacy (completely eliminated symptoms). In all cases, the physician recommended vitamin C treatment.
Table 8.
Comparison of subjectively reported efficacy and tolerability of vitamin C vs. previous medication
| Rating |
Previous therapy |
Vitamin C |
||
|---|---|---|---|---|
| n | %* | n | %* | |
| Efficacy | ||||
| Very good and good efficacy | 12 | 23.5 | 67 | 94.4 |
| Moderate or no effect or deterioration | 39 | 76.5 | 4 | 5.6 |
| Tolerability | ||||
| Good tolerability | 24 | 47.1 | 70 | 98.6 |
| Poor tolerability | 27 | 52.9 | 1 | 1.4 |
| Total | 51 | 100.0 | 71 | 100.0 |
*Valid data analysis.
Safety of vitamin C infusion
Very good tolerability was reported in 70 of 71 patients (98.6%). In 1 of the 71 patients (1.4%), 2 adverse reactions to vitamin C infusion were recorded, but treatment was continued. These adverse reactions were “repeated unpleasant sensation of cold a few hours after infusion” and “tiredness the next morning.”
Discussion
The results of this interim subgroup analysis of a large observational study indicate that high-dosage vitamin C reduces disease-specific and nonspecific symptoms in patients with respiratory and cutaneous allergic conditions as evidenced by improvements in a standardized symptom score and the physicians’ rating. The reduction in the sum scores of disease-specific and nonspecific symptoms was significant for the whole population and in the subgroup analyses of the type of diagnosis (respiratory or cutaneous) and disease (acute or chronic) (p < 0.0001).
This was an observational study without a control group; notably, however, 54% of our vitamin C-treated patients took no other allergy-related medication (antiallergic reagents or antibiotics). Comparison of the percentage of patients with an improvement in the symptom sum score showed no meaningful difference between patients with and without allergy-related medication besides vitamin C.
Interestingly, in this context, a randomized study showed corticosteroid-sparing effects of daily oral vitamin C substitution (1 g) in asthmatic patients.27
Despite symptomatic medication, diseases such as allergic rhinitis, asthma, and dermatitis are associated with impairments of functioning in day-to-day life and so reduce patients’ health-related quality of life.28 Therefore, in the treatment of allergic diseases, nonspecific symptoms such as fatigue, sleep disturbances, cognitive impairment, and mood changes are considered to warrant more attention than they have been given to date.29,30 Our cohort data revealed fatigue in 88.6%, lack of concentration in 85.7%, sleep disorders in 75.7%, and depression in 62.9% of the study group at the start of treatment.
Notably, we observed that iv vitamin C had a greater effect on chronic nonspecific symptoms than on acute nonspecific symptoms, with a nearly 100% greater sum score reduction (6.21 vs. 3.62) (see Table 5). These symptoms may be either related to inflammation and oxidative stress or associated with the undesired effects of antihistaminic drugs.
Sleep impairment, which improved in 92.5% of affected patients in our study group, had a demonstrably significant impact on health-related quality of life in patients with allergic rhinitis and atopic dermatitis.31,32
The observed reduction of specific symptoms, such as rhinitis and pruritus, in our study group may have been associated with the histamine-reducing effect of vitamin C, which was examined in other studies. The effect of vitamin C on histamine blood levels has been investigated in both preclinical33–36 and clinical studies,37–42 but the detailed mode of action has not been fully elucidated. In a recent study investigating the acute effect of 7.5 g of iv vitamin C on the histamine levels in 89 patients with allergies or upper respiratory infections, a significant reduction in the histamine levels was observed. A higher initial serum histamine level was associated with a more pronounced observed reduction after vitamin C treatment.41 Regulation and modulation of histamine levels by vitamin C appear to be biological phenomena because a similar relationship was reported in guinea pigs, who, like humans, cannot synthesize ascorbate.43 In animals that synthesize vitamin C on demand, histaminosis is accompanied by a rise in circulating ascorbate.44 Several investigations have shown a correlation between ascorbate depletion and histaminaemia.40 Histamine levels increased exponentially as plasma ascorbate decreased to <1 mg/dL, and a further reduction to <0.7 mg/dL resulted in a highly significant increase in the blood histamine level.40 Although serum ascorbate levels were only available in an elective subgroup of 21 patients (29.6%) in the present interim analysis, a severe deficiency (median, 2.0 mg/dL) was very apparent, and 18 of the 21 investigated patients (85.7%) had plasma ascorbate levels below the critical value of 0.7 mg/dL. This corresponds well to the observed improvements in this patient cohort, in which the sum score for specific symptoms improved in all 18 patients and the score for nonspecific symptoms improved in 17 of 18 patients.
Therefore, an important therapeutic goal may be to prevent ascorbate levels declining to <0.7 mg/dL in patients with allergic diseases. However, the optimal plasma ascorbate levels for allergic individuals remain undefined.
The observed extent of pain reduction (81.6%) was similar to that of symptom reduction. Because inflammation and oxidative stress play a significant pathophysiological role in the development of pain, vitamin C was recently considered an important component of pain treatment.45,46 In patients with herpes zoster, cancer and postoperative states, iv vitamin C was shown to reduce or prevent pain.21,47–49
Although serum ascorbate levels were only available in an elective subgroup of less than one-third of the cohort, the observed severe baseline deficiency is consistent with findings in patients with other inflammatory diseases.50–54 Ascorbate is an important low-molecular-weight antioxidant that maintains antioxidative defenses at the air–lung interface.55 Any loss of ascorbate across the large surface area of the lung induces a major drain on the systemic ascorbate reserves; this has already been documented in patients with asthma,50,56–58 but not in patients with all other allergic diseases. However, patients with atopic dermatitis and psoriasis reportedly have reduced cutaneous ascorbate levels.59,60 In our subgroup of patients who underwent elective ascorbate measurements, respiratory diseases (n = 10) and cutaneous diseases (n = 11) were evenly distributed. Both groups were found to have deficient serum ascorbate levels at baseline, but the levels in patients with cutaneous diseases (mean, 0.24 mg/dL) were much lower than those in patients with respiratory diseases (mean, 0.45 mg/dL). To the best of our knowledge, this finding provides novel preliminary evidence of the risk of ascorbate deficiency in patients with allergic diseases. The mean serum ascorbate levels appeared to differ between patients with acute and chronic (0.40 vs. 0.24 mg/dL) symptoms at baseline, with possibly lower levels associated with chronic disease.
The iv vitamin C treatment in this study was judged by the attending physician to be very safe and to have a higher tolerability than the prior medications, which were mainly antihistamines and local or systemic steroids. In our cohort, 52.9% of patients exhibited poor tolerability to standard allergy medication (Table 8) compared with only 1 of 71 patients who had an adverse event after iv vitamin C. This single patient developed adverse events during iv vitamin C but decided to continue receiving treatment. These observations are consistent with the findings of clinical studies and of a comprehensive survey that indicated the tolerability of iv vitamin C in doses up to 0.5 g/kg body weight (also up to 1.5 g/kg in phase-I trials) in patients without the documented contraindications of oxalate calculi, renal failure, hemochromatosis, and glucose-6-phosphate dehydrogenase deficiency.19,61–63
The observations from this noninterventional study form a basis for planning a randomized controlled clinical trial to obtain more definitive evidence of the clinical relevance of our findings. Based on the information received, an investigation of the effects of a 3-week intervention involving two to three infusions per week appears to be appropriate for patients with acute allergic diseases. In any case, nonspecific symptoms such as fatigue and lack of concentration should be inquired in addition to the allergy-specific symptoms.
Strengths and weakness of the study
We consider that our study provides important novel evidence suggesting that elective high-dose parenteral (iv) vitamin C treatment has positive effects on the progression of both disease-specific and nonspecific symptoms in patients with allergic diseases while exhibiting high tolerability in this patient group. Our observed effects on nonspecific symptoms, such as tiredness/fatigue, sleep disorders, lack of concentration, and depression, are important because these symptoms of quality of life are rarely monitored in detail in studies of patients with allergic diseases. Interpretation of our observations is significantly limited by the absence of a control group and the small sample of our interim subgroup analysis.
Conclusion
Preclinical and clinical data indicate that the reduction of oxidative stress and inflammation by vitamin C can be beneficial in patients with allergic diseases. This study provides observational evidence of the use of high-dose iv vitamin C in daily practice in the treatment of respiratory and cutaneous allergic diseases. We also observed evidence of serum ascorbate deficiency in our patients with allergic disease. Based on our observations and the plausible therapeutic effect of vitamin C, clinical trials with high-dose iv vitamin C are warranted in patients with allergic diseases.
Authors’ contributions
CV conceived and initiated the study and participated in its design, contributed to the data evaluation, and drafted the manuscript. MR participated in the data evaluation and manuscript writing. BK participated in the data evaluation. KK participated in the study design and manuscript writing. AH participated in the study design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript. The explorative statistical analyses were performed by an independent statistician (Gesellschaft für Therapieforschung mbH, www.gkm-therapieforschung.de, Munich, Germany).
Acknowledgements
The authors thank the physicians and natural health practitioners for agreeing to collate their observations and provide them for analysis and interpretation.
Declaration of conflicting interest
AH, MR, and KK declare that they have no competing interests. CV and BK are employed by Pascoe pharmazeutische Präparate GmbH (Giessen, Germany).
Funding
Study fees for the medical practices and data collection, the charges for the independent statistician and the language editing service, and the article-processing charge for the open-access journal were provided by Pascoe pharmazeutische Präparate GmbH, Germany.
References
- 1.Kiewiet MB, Gros M, van Neerven RJ, et al. Immunomodulating properties of protein hydrolysates for application in cow's milk allergy. Pediatr Allergy Immunol 2015; 26: 206–217. [DOI] [PubMed] [Google Scholar]
- 2.Marlow G, Han DY, Wickens K, et al. Differential effects of two probiotics on the risks of eczema and atopy associated with single nucleotide polymorphisms to Toll-like receptors. Pediatr Allergy Immunol 2015; 26: 262–271. [DOI] [PubMed] [Google Scholar]
- 3.Asher BF, Seidman MD, Reddy WD, et al. Integrative medical approaches to allergic rhinitis. Curr Opin Otolaryngol Head Neck Surg 2015; 23: 221–225. [DOI] [PubMed] [Google Scholar]
- 4.Resnick ES, Bielory BP, Bielory L. Complementary therapy in allergic rhinitis. Curr Allergy Asthma Rep 2008; 8: 118–125. [DOI] [PubMed] [Google Scholar]
- 5.Jiang L, Diaz PT, Best TM, et al. Molecular characterization of redox mechanisms in allergic asthma. Ann Allergy Asthma Immunol 2014; 113: 137–142. [DOI] [PubMed] [Google Scholar]
- 6.Campbell EL, Colgan SP. Neutrophils and inflammatory metabolism in antimicrobial functions of the mucosa. J Leukoc Biol 2015; 98: 517–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown DI, Griendling KK. Nox proteins in signal transduction. Free Radic Biol Med 2009; 47: 1239–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ortiz GG, Pacheco-Moises FP, Bitzer-Quintero OK, et al. Immunology and oxidative stress in multiple sclerosis: clinical and basic approach. Clin Dev Immunol 2013; 2013: 708659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boldogh I, Bacsi A, Choudhury BK, et al. ROS generated by pollen NADPH oxidase provide a signal that augments antigen-induced allergic airway inflammation. J Clin Invest 2005; 115: 2169–2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciz M, Lojek A. Modulation of neutrophil oxidative burst via histamine receptors. Br J Pharmacol 2013; 170: 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohmori H, Komoriya K, Azuma A, et al. Xanthine oxidase-induced histamine release from isolated rat peritoneal mast cells: involvement of hydrogen peroxide. Biochem Pharmacol 1979; 28: 333–334. [DOI] [PubMed] [Google Scholar]
- 12.Ohmori H, Yamamoto I, Akagi M, et al. Properties of hydrogen peroxide-induced histamine release from rat mast cells. Biochem Pharmacol 1980; 29: 741–745. [DOI] [PubMed] [Google Scholar]
- 13.Hocker M, Rosenberg I, Xavier R, et al. Oxidative stress activates the human histidine decarboxylase promoter in AGS gastric cancer cells. J Biol Chem 1998; 273: 23046–23054. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt HH, Stocker R, Vollbracht C, et al. Antioxidants in translational medicine. Antioxid Redox Signal 2015; 23: 1130–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frei B, Stocker R, Ames BN. Antioxidant defenses and lipid peroxidation in human blood plasma. Proc Natl Acad Sci U S A 1988; 85: 9748–9752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frei B, England L, Ames BN. Ascorbate is an outstanding antioxidant in human blood plasma. Proc Natl Acad Sci U S A 1989; 86: 6377–6381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frei B. Ascorbic acid protects lipids in human plasma and low-density lipoprotein against oxidative damage. Am J Clin Nutr 1991; 54: 1113S–1118S. [DOI] [PubMed] [Google Scholar]
- 18.Levine M, Rumsey SC, Daruwala R, et al. Criteria and recommendations for vitamin C intake. JAMA 1999; 281: 1415–1423. [DOI] [PubMed] [Google Scholar]
- 19.Padayatty SJ, Sun AY, Chen Q, et al. Vitamin C: intravenous use by complementary and alternative medicine practitioners and adverse effects. PLoS One 2010; 5: e11414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levine M, Padayatty SJ, Espey MG. Vitamin C: Concentration- function approach yields pharmacology and therapeutic discoveries. Adv Nutr 2011; 2: 78–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schencking M, Vollbracht C, Weiss G, et al. Intravenous Vitamin C in the treatment of shingles: Results of a multicenter prospective cohort study. Med Sci Monit 2012; 18: CR215–CR224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Srivastava VK, Agrawal S, Kadiyala VN, et al. The efficacy of pregabalin for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled double-blind study. J Anesth 2015; 29: 212–216. [DOI] [PubMed] [Google Scholar]
- 23.Li Z, Mu G, Chen W, et al. Comparative evaluation of topical pranoprofen and fluorometholone in cases with chronic allergic conjunctivitis. Cornea 2013; 32: 579–582. [DOI] [PubMed] [Google Scholar]
- 24.Koenig J, Sevinc S, Frohme C, et al. Does visualisation during urethrocystoscopy provide pain relief? Results of an observational study. BMC Urol 2015; 15: 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnston CS, Thompson LL. Vitamin C status of an outpatient population. J Am Coll Nutr 1998; 17: 366–370. [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine (US) panel on dietary antioxidants and related compounds. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington (DC: ): National Academies Press (US), 2000. [PubMed] [Google Scholar]
- 27.Fogarty A, Lewis SA, Scrivener SL, et al. Corticosteroid sparing effects of vitamin C and magnesium in asthma: a randomised trial. Respir Med 2006; 100: 174–179. [DOI] [PubMed] [Google Scholar]
- 28.Bateman ED, Esser D, Chirila C, et al. Magnitude of effect of asthma treatments on Asthma Quality of Life Questionnaire and Asthma Control Questionnaire scores: Systematic review and network meta-analysis. J Allergy Clin Immunol 2015; 136: 914–922. [DOI] [PubMed] [Google Scholar]
- 29.Soler ZM, Eckert MA, Storck K, et al. Cognitive function in chronic rhinosinusitis: a controlled clinical study. Int Forum Allergy Rhinol 2015; 5: 1010–1017. [DOI] [PubMed] [Google Scholar]
- 30.Silverberg JI, Garg NK, Paller AS, et al. Sleep disturbances in adults with eczema are associated with impaired overall health: a US population-based study. J Invest Dermatol 2015; 135: 56–66. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez-Nunez V, Valero AL, Mullol J. Impact of sleep as a specific marker of quality of life in allergic rhinitis. Curr Allergy Asthma Rep 2013; 13: 131–141. [DOI] [PubMed] [Google Scholar]
- 32.LeBovidge JS, Elverson W, Timmons KG, et al. Multidisciplinary interventions in the management of atopic dermatitis. J Allergy Clin Immunol 2016; 138: 325–334. [DOI] [PubMed] [Google Scholar]
- 33.Nandi BK, Subramanian N, Majumder AK, et al. Effect of ascorbic acid on detoxification of histamine under stress conditions. Biochem Pharmacol 1974; 23: 643–647. [DOI] [PubMed] [Google Scholar]
- 34.Subramanian N, Nandi BK, Majumder AK, et al. Effect of ascorbic acid on detoxification of histamine in rats and guinea pigs under drug treated conditions. Biochem Pharmacol 1974; 23: 637–641. [DOI] [PubMed] [Google Scholar]
- 35.Ridzwan BH, Jais AM, Waton NG. The depletion effects of chlorpromazine, reserpine and ascorbic acid on tissue histamine of guinea-pigs. Gen Pharmacol 1988; 19: 631–636. [DOI] [PubMed] [Google Scholar]
- 36.Johnston CS, Huang SN. Effect of ascorbic acid nutriture on blood histamine and neutrophil chemotaxis in guinea pigs. J Nutr 1991; 121: 126–130. [DOI] [PubMed] [Google Scholar]
- 37.Johnston CS, Martin LJ, Cai X. Antihistamine effect of supplemental ascorbic acid and neutrophil chemotaxis. J Am Coll Nutr 1992; 11: 172–176. [PubMed] [Google Scholar]
- 38.Johnston CS, Solomon RE, Corte C. Vitamin C depletion is associated with alterations in blood histamine and plasma free carnitine in adults. J Am Coll Nutr 1996; 15: 586–591. [DOI] [PubMed] [Google Scholar]
- 39.Johnston CS, Retrum KR, Srilakshmi JC. Antihistamine effects and complications of supplemental vitamin C. J Am Diet Assoc 1992; 92: 988–989. [PubMed] [Google Scholar]
- 40.Clemetson CAB. Histamine and Ascorbic Acid in Human Blood. J Nutr 1980; 110: 662–668. [DOI] [PubMed] [Google Scholar]
- 41.Hagel AF, Layritz CM, Hagel WH, et al. Intravenous infusion of ascorbic acid decreases serum histamine concentrations in patients with allergic and non-allergic diseases. Naunyn Schmiedebergs Arch Pharmacol 2013; 386: 789–793. [DOI] [PubMed] [Google Scholar]
- 42.Romero SA, Ely MR, Sieck DC, et al. Effect of antioxidants on histamine receptor activation and sustained postexercise vasodilatation in humans. Exp Physiol 2015; 100: 435–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vashisht A, Chhabra SK, Banerjee BD, et al. Rapidly adapting receptor activity during oxidative stress induced airway hyperresponsiveness. Respir Physiol Neurobiol 2013; 186: 273–284. [DOI] [PubMed] [Google Scholar]
- 44.Johnston CS. The antihistamine action of ascorbic acid. Subcell Biochem 1996; 25: 189–213. [DOI] [PubMed] [Google Scholar]
- 45.Hasanzadeh Kiabi F, Soleimani A, Habibi MR, et al. Can Vitamin C be used as an adjuvant for managing postoperative pain? a short literature review. Korean J Pain 2013; 26: 209–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li R, Shen L, Yu X, et al. Vitamin C enhances the analgesic effect of gabapentin on rats with neuropathic pain. Life Sci 2016; 157: 25–31. [DOI] [PubMed] [Google Scholar]
- 47.Chen S, Roffey DM, Dion CA, et al. Effect of perioperative Vitamin C supplementation on postoperative pain and the incidence of chronic regional pain syndrome: a systematic review and meta-analysis. Clin J Pain 2016; 32: 179–185. [DOI] [PubMed] [Google Scholar]
- 48.Kapoor S. Vitamin C and its emerging role in pain management: beneficial effects in pain conditions besides post herpetic neuralgia. Korean J Pain 2012; 25: 200–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carr AC, Vissers MC, Cook JS. The effect of intravenous vitamin C on cancer- and chemotherapy-related fatigue and quality of life. Front Oncol 2014; 4: 283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shanmugasundaram K, Kumar S, Rajajee S. Excessive free radical generation in the blood of children suffering from asthma. Clinica Chimica Acta 2001; 305: 107–114. [DOI] [PubMed] [Google Scholar]
- 51.Lunec J, Blake DR. The determination of dehydroascorbic acid and ascorbic acid in the serum and synovial fluid of patients with rheumatoid arthritis (RA). Free Radic Res Commun 1985; 1: 31–39. [DOI] [PubMed] [Google Scholar]
- 52.Mayland CR, Bennett MI, Allan K. Vitamin C deficiency in cancer patients. Palliat Med 2005; 19: 17–20. [DOI] [PubMed] [Google Scholar]
- 53.Fowler AA, 3rd, Syed AA, Knowlson S, et al. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J Transl Med 2014; 12: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rodemeister S, Duquesne M, Adolph M, et al. Massive and long-lasting decrease in vitamin C plasma levels as a consequence of extracorporeal circulation. Nutrition 2014; 30: 673–678. [DOI] [PubMed] [Google Scholar]
- 55.Larsson N, Rankin GD, Bicer EM, et al. Identification of vitamin C transporters in the human airways: a cross-sectional in vivo study. BMJ open 2015; 5: e006979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aderele WI, Ette SI, Oduwole O, et al. Plasma vitamin C (ascorbic acid) levels in asthmatic children. Afr J Med Med Sci 1985; 14: 115–120. [PubMed] [Google Scholar]
- 57.Kalayci O, Besler T, Kilinc K, et al. Serum levels of antioxidant vitamins (alpha tocopherol, beta carotene, and ascorbic acid) in children with bronchial asthma. Turk J Pediatr 2000; 42: 17–21. [PubMed] [Google Scholar]
- 58.Vural H, Uzun K. Serum and red blood cell antioxidant status in patients with bronchial asthma. Can Respir J 2000; 7: 476–80. [DOI] [PubMed] [Google Scholar]
- 59.Leveque N, Robin S, Muret P, et al. In vivo assessment of iron and ascorbic acid in psoriatic dermis. Acta Derm Venereol 2004; 84: 2–5. [DOI] [PubMed] [Google Scholar]
- 60.Leveque N, Robin S, Muret P, et al. High iron and low ascorbic acid concentrations in the dermis of atopic dermatitis patients. Dermatology 2003; 207: 261–264. [DOI] [PubMed] [Google Scholar]
- 61.Hoffer LJ, Levine M, Assouline S, et al. Phase I clinical trial of i.v. ascorbic acid in advanced malignancy. Ann Oncol 2008; 19: 1969–1974. [DOI] [PubMed] [Google Scholar]
- 62.Nielsen TK, Hojgaard M, Andersen JT, et al. Elimination of ascorbic acid after high-dose infusion in prostate cancer patients: a pharmacokinetic evaluation. Basic Clin Pharmacol Toxicol 2015; 116: 343–348. [DOI] [PubMed] [Google Scholar]
- 63.Monti DA, Mitchell E, Bazzan AJ, et al. Phase I evaluation of intravenous ascorbic acid in combination with gemcitabine and erlotinib in patients with metastatic pancreatic cancer. PLoS One 2012; 7: e29794. [DOI] [PMC free article] [PubMed] [Google Scholar]