Key Points
Question
Can a county-based vision center increase eyeglasses use and improve school performance among primary schoolchildren in rural China?
Findings
This cluster randomized clinical trial of 31 schools and 2613 participants showed that children who received eyeglasses earlier in the school year performed significantly better on an end-of-year mathematics test than children who received eyeglasses later in the year, equivalent to half a semester. Provision of free eyeglasses also improved children's use of spectacles.
Meaning
A county-based vision center is an effective way to address vision care problems and improve school performance in rural China.
Abstract
Importance
Visual impairment is common among children in rural China, but fewer than one-third of children with poor vision own and wear eyeglasses.
Objective
To study the effect of hospital-based vision centers on academic performance, ownership of eyeglasses, and eyeglasses-wearing behavior in rural Chinese children.
Design, Setting, and Participants
Cluster randomized, investigator-masked, clinical trial from September 2014 through June 2015. A vision center capable of providing refractive services was established in the Hospital of Yongshou County, a nationally designated poor county in rural Shaanxi Province, western China. All 31 rural primary schools in Yongshou County participated; participants were all children in grades 4 through 6 (aged approximately 10-12 years) with uncorrected visual acuity of Snellen 6/12 or worse in either eye (2613 children). Data analysis was conducted March through May 2016, and data were analyzed by the intention-to-treat principle.
Interventions
After teacher-led vision screening early in the school year (September-October 2014), schools were randomly assigned to either early referral (December 2014-February 2015) to the vision center for refraction and free eyeglasses if needed or late referral (March-June 2015) for the identical intervention.
Main Outcomes and Measures
The primary outcome was score on a study-administered mathematics test (June 2015) adjusted for baseline score. Secondary outcomes were self-reported eyeglasses ownership and wear at final examination (June 2015).
Results
All 2613 children evaluated were of Han Chinese race/ethnicity, and 1209 (46.3%) were female. Twelve hundred children (45.9%) met the vision criteria. Among these, 543 (45.3%) were randomized to early screening and 657 (54.7%) to late screening; 433 (79.7%) of the early screening group and 516 (78.5%) of the late screening group completed the study. Of eligible children, 120 (27.7%) owned eyeglasses at baseline. The adjusted effect on test scores comparing early and late groups was 0.25 SD (95% CI, 0.01-0.48; 1-sided P = .04), with the point estimate equivalent to half a semester of additional learning. At the end of the study, 347 of the 433 participants in the early group (80%) reported owning eyeglasses and 326 (75%) reported wearing eyeglasses; among the 516 participants in the late group, 371 (61%) reported owning and 286 (55%) reported wearing eyeglasses.
Conclusions and Relevance
In this study, early provision of free eyeglasses was seen to improve children’s academic performance and wearing of spectacles. These findings suggest that a county hospital–based vision center may be an effective way to improve children’s educational opportunities in rural China.
Trial Registration
isrctn.org Identifier: ISRCTN03252665
This cluster randomized clinical trial examines the effect of school-based vision screening and free eyeglasses on eyeglasses ownership, eyeglasses use, and academic performance in rural Chinese schoolchildren.
Introduction
A series of World Health Organization–supported studies suggest that approximately 10% to 20% of school-aged children in low- and middle-income countries have refractive error.1,2,3,4 Nearly half of children worldwide with this type of visual impairment live in China.5 Refractive error can be detected with simple vision screening and safely corrected6 with accurate eyeglasses.1 Despite the existence of this relatively simple intervention, in low-resource settings including rural China, fewer than one-third of children with poor vision own or wear eyeglasses.7,8,9
It is not known what accounts for the low rates of eyeglasses use in these settings. Cost is not the main barrier to access; earlier findings suggest that only the poorest families in rural China cannot afford a pair of eyeglasses.10 In fact, many families are willing to spend money on eyeglasses for their children, even in poor areas.11
A primary reason for the low rate of eyeglasses ownership may be lack of access to vision care services.12 An estimated 625 million people are blind or visually impaired globally for this reason. Underserved areas, including rural China, lack necessary facilities, infrastructure, equipment, and skilled practitioners.13,14,15
Vision centers are one of the most popular strategies used by nongovernmental organizations and governments attempting to overcome barriers to access to high-quality eyeglasses.13,16,17 Vision centers are long-term facilities that provide affordable eye care services for local communities. They tend to be promoted to people with uncorrected refractive error and offer a range of services that may include eye examinations, refraction, and eyeglasses dispensing.13,16,17,18 Despite their popularity, there is little published evidence evaluating the quality and impact of the refractive services they deliver.
We carried out a cluster randomized clinical trial to measure the effect of vision centers on eyeglasses ownership, eyeglasses use, and school performance among children. We hypothesized that access to the optometric services provided by the vision center earlier rather than later in the school year would lead to significant increases in these measures. More specifically, by improving access to eyeglasses, the vision center would engender an increase in ownership of eyeglasses, which we hoped would carry over into an increase in eyeglasses use (wear). We further hypothesized that increases in eyeglasses ownership and wear would lead to improvements in students’ educational outcomes.
In part to help ensure that increased eyeglasses ownership would carry over into eyeglasses wear, we involved children’s primary schoolteachers in the screening process. Our hypothesis was that teachers would provide extra nudges to students that might improve rates of eyeglasses wear. Randomized trials conducted elsewhere have shown that involving teachers in school-based programs can significantly increase rates of eyeglasses use.9 In addition, we hypothesized that greater adherence to regular eyeglasses wear would yield a greater observed effect size on educational outcomes. Previous randomized trials have shown that provision of spectacles to children significantly improves academic performance, even in the face of relatively low adherence to regular eyeglasses wear.8
Methods
Setting
We established a vision center in the local government hospital of Yongshou, a nationally designated poor county in rural Shaanxi Province. Yongshou County has a population of 186 100 and a per capita gross domestic product of $4308, ranking 88th of the 107 counties in Shaanxi Province.19 Before the vision center was established, there was no public provider of refractive services in the county, and the 3 private providers were all located in the county seat. Ethical approval for this study was provided by the Stanford University Institutional Review Board, and the principles of the Declaration of Helsinki20 were followed throughout. Permissions were received from the local boards of education in the study area and the principals of all participating schools. All participating children gave oral assent before baseline data collection, and legal guardians gave written informed consent for their children’s involvement in the study. The study protocol is available in the Supplement.
Vision Center Setup and Staff Training
The vision center was established in collaboration with the Shaanxi Province Ministry of Education and the prefectural bureau of education overseeing Yongshou County. The government’s goal was for Yongshou to act as a model county for all of Shaanxi Province, eventually upscaling the program to provide vision care to all rural children in the province in grades 4 to 6 (aged approximately 10-12 years).
The Yongshou County Hospital selected 3 employees (1 ophthalmologist and 2 ophthalmic nurses) to staff the vision center. These individuals underwent formal refraction training at Zhongshan Ophthalmic Center in Guangzhou, China. The training lasted 1 month, from September to October 2014. At the conclusion of the program, all 3 employees received national certification as qualified refractionists and opticians from China’s Ministry of Labor and Social Security. After this formal training, the Yongshou staff members underwent 1 month of supervised practical training in their home county, during which time each staff member screened and measured refractive error in hundreds of children from local schools and underwent practical instruction in eyeglasses dispensing. A consultant from Brien Holden Vision Institute provided management training, including inventory control and record keeping.
Sampling, Eligibility Criteria
We enrolled all rural primary schools in Yongshou County, and, in each school, examined all children in grades 4 through 6. Children were eligible for participation if they had an uncorrected visual acuity of Snellen 6/12 or worse in either eye.21
Randomization, Interventions, and Masking
The study was conducted as a cluster randomized clinical trial, with randomization occurring at the township level. After students received teacher-led vision screening from September to November 2014 (beginning of the school year), schools were randomly assigned by township (cluster size, 5-6) to 1 of 2 groups: an early referral group, in which all children who met screening criteria were referred to the vision center for refraction and free eyeglasses as needed from December 2014 to February 2015 (middle of the school year), and a late referral group, who received the same intervention between March and June 2015 (end of the school year). Members of the study team conducted randomization at their offices at Shaanxi Normal University, in Xi’an, China, using Stata, version 13.1 (StataCorp).
In total, our study included 11 townships (clusters), with an observed intercluster coefficient of 0.025. Assuming an α of .05 and an R2 of 0.5, our study was powered to observe an effect size of 0.25 at 80% power.
Teachers initially received 1 day of instruction on vision screening by vision center staff. Parents of children with uncorrected visual acuity less than or equal to Snellen 6/12 or worse in either eye received a letter describing the program and inviting them to bring their children to the vision center for a free examination that included rescreening, refraction, and a free pair of eyeglasses if needed. Teachers also provided a list of students who met the screening criteria to the vision center staff, who made follow-up phone calls to schools and families to encourage parents to bring their children for services.
Participants (students, parents, and teachers) and vision center staff were not informed of the study design or group assignment. Because teachers did not have the skills to conduct vision screenings before receiving formal training, and the formal trainings were only administered by vision center staff at the assigned time, contamination across treatment arms was nearly impossible. Participants were told only that this was a study of vision care among rural schoolchildren. Teachers were unaware that they were participating in a trial and were masked to group assignment at the time of outcome assessment.
Data Collection
In September 2014, all sampled students were administered a standardized mathematics test as an index of academic achievement. The test was administered by the Bureau of Education and proctored by teachers in each school. Mathematics was chosen for testing to reduce the effect of home learning on performance. Immediately before the start of program interventions in each school, teachers administered a socioeconomic survey to all children, collecting information on sex, eyeglasses ownership, boarding status, and parental migration and educational attainment. Finally, in June 2015, all students in the sample were again administered the standardized mathematics test and socioeconomic survey.
Our primary outcome was the final mathematics score, which was adjusted for the baseline score and expressed in SD. Secondary outcomes were self-reported eyeglasses ownership and wear at the time of final survey. Children were asked to describe their eyeglasses wear as “always,” “only for studying,” or “usually not worn.”
School-Based Visual Acuity Assessment
Visual acuity was tested separately for each eye without refraction at 4 m using Early Treatment Diabetic Retinopathy Study charts (Precision Vision) in a well-lighted indoor area.22 Children owning eyeglasses were requested to bring them to school, and their visual acuity was tested with and without habitual correction. Visual acuity for an eye was defined as the lowest line on which 4 of 5 optotypes were read correctly. If the top line could not be read at 4 m, the participant was tested at 1 m, and the measured visual acuity was divided by 4.
Vision Center–Based Vision Screening
All vision screening at vision centers was carried out by 1 of the 3 trained refractionists in the Yongshou County Hospital vision center and followed China’s strict national guidelines for vision care for prescribing spectacles. Specifically, the refractionists followed 6 steps before prescribing spectacles to sample children. First, they discussed the child’s corrective lens history and readministered the visual acuity screening described above. Based on the results of this screening, children with uncorrected visual acuity of Snellen 6/12 or less in either eye underwent cycloplegia with up to 3 drops of cyclopentolate hydrochloride, 1%, preceded by a drop of proparacaine hydrochloride, 0.5%, to prevent accommodation and inaccurate refraction. All center-based vision testing, including cycloplegia, was conducted in a single visit for each child. Children then underwent automated refraction (Topcon KR 8900; Topcon Medical Systems, Inc.) with subjective refinement by the refractionist. Children were eligible for spectacle prescription if they had an uncorrected visual acuity of Snellen 6/12 or worse in either eye after cycloplegia. Finally, before prescribing spectacles, the refractionist measured each child’s interpupillary distance and measured the lens power of the child’s original eyeglasses, if any. The vision center was stocked with approximately 10 different styles of child-friendly frames. Children were allowed to choose the frames they liked best.
Statistical Analysis
All analyses were performed using Stata, version 13.1 (StataCorp), calculating robust SEs to adjust for clustering by township. Baseline and final mathematics scores were standardized for each grade separately to give a mean of 0 and SD of 1 among late referral group children at baseline. Baseline eyeglasses ownership was defined as having a pair of eyeglasses at school, after being asked to bring them. Refractive power was defined throughout as the spherical equivalent (spherical power plus half the cylindrical power).
For intention-to-treat analyses, with eyeglasses ownership and wear as outcomes, generalized linear models with Poisson regression were used to estimate the relative risk for the intervention arm after adjustment for baseline eyeglasses ownership and other covariates.23 One-way analysis of variance was used to estimate the intraclass correlation coefficient as a measure of clustering of final mathematics scores and eyeglasses ownership and wear within each township. Randomization groups were compared by intention-to-treat analysis using multiple linear regression, with final mathematics scores as the primary outcome for the main hypothesis and treatment assignment and baseline mathematics scores as covariates. For the secondary hypothesis regarding uptake of eyeglasses, the secondary outcomes were self-reported eyeglasses ownership and wear (“only for studying” or “always” compared with “mostly not worn”).
To reduce the inefficiency of estimation owing to missing values, we used multiple imputation in Stata as described by Royston24 to impute the following data at baseline: boarding at school (n = 34), both parents out-migrated for work (n = 30), and 1 or both parents with 9 years’ education or more (n = 51).24 We used logistic regression for binary variables and ordered logistic regression for ordinal variables. The independent variables used for imputation included all nonmissing variables (Table 1). For each variable, different models were used for selecting the independent variables based on predictive value and data availability. The multiple imputation approach created 20 copies of the data in which missing values were imputed by chained equations. Final results were obtained by averaging these 20 data sets using Rubin rules, which ensured that the SEs for all regression coefficients took into account the uncertainty in the imputations as well as uncertainty in the estimation.24 A 1-sided P value was determined a priori to denote statistical significance.
Table 1. Baseline Characteristics of Children With Correctable Refractive Error, by Group Assignmenta.
| Variables | Analytic Sample (n = 949) | Full Sample (n = 1200) | Difference Between Full and Attrited Samples | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Early Referral Group (n = 433) | Late Referral Group (n = 516) | P Value | Early Referral Group (n = 543) | Late Referral Group (n = 657) | P Value | Analytic Sample (n = 949) | Attrited Sample (n = 251) | P Value | |
| Male sex, No. (%) | 219 (50.6) | 251 (48.6) | .67 | 277 (51.0) | 322 (49.0) | .64 | 470 (49.5) | 129 (51.4) | .68 |
| Mathematics score, mean (SD) | 0.09 (1.1) | −0.05 (1.0) | .59 | 0.04 (1.1) | −0.05 (0.9) | .70 | 0.01 (1.0) | −0.09 (1.0) | .33 |
| Distance between town and county seat, mean (SD), km | 24.2 (15.8) | 27.4 (11.6) | .75 | 23.7 (15.8) | 28.2 (11.1) | .63 | 25.9 (13.7) | 27.1 (13.0) | .73 |
| Visual acuity of better eye, logMAR, mean (SD) [Snellen equivalent] | 0.6 (0.2) [6/24] | 0.7 (0.3) [6/30] | .11 | 0.6 (0.2) [6/24] | 0.7 (0.3) [6/30] | .09 | 0.6 (0.3) [6/24] | 0.6 (0.2) [6/24] | .009 |
| Owned eyeglasses, No. (%)b | 120 (27.7) | 153 (29.7) | .72 | 140 (25.8) | 195 (29.7) | .42 | 273 (28.8) | 62 (24.7) | .32 |
| Boarding at school, No. (%) | 42 (9.7) | 81 (15.7) | .57 | 61 (11.2) | 95 (14.5) | .74 | 123 (13.0) | 33 (13.2) | .98 |
| One or both parents with ≥9 y of education, No. (%) | 82 (18.9) | 96 (18.6) | .93 | 101 (18.6) | 136 (20.7) | .58 | 178 (18.7) | 59 (23.5) | .36 |
| Both parents out-migrated for work, No. (%) | 54 (12.5) | 88 (17.1) | .35 | 73 (13.4) | 110 (16.7) | .41 | 142 (15.0) | 41 (16.3) | .71 |
Analytic sample includes all sample children for whom baseline and end line data were available. Full sample includes all sample children for whom baseline data but no data were available at the end of the study.
Defined as having eyeglasses at school at baseline, and having previously been told to bring them to school.
Results
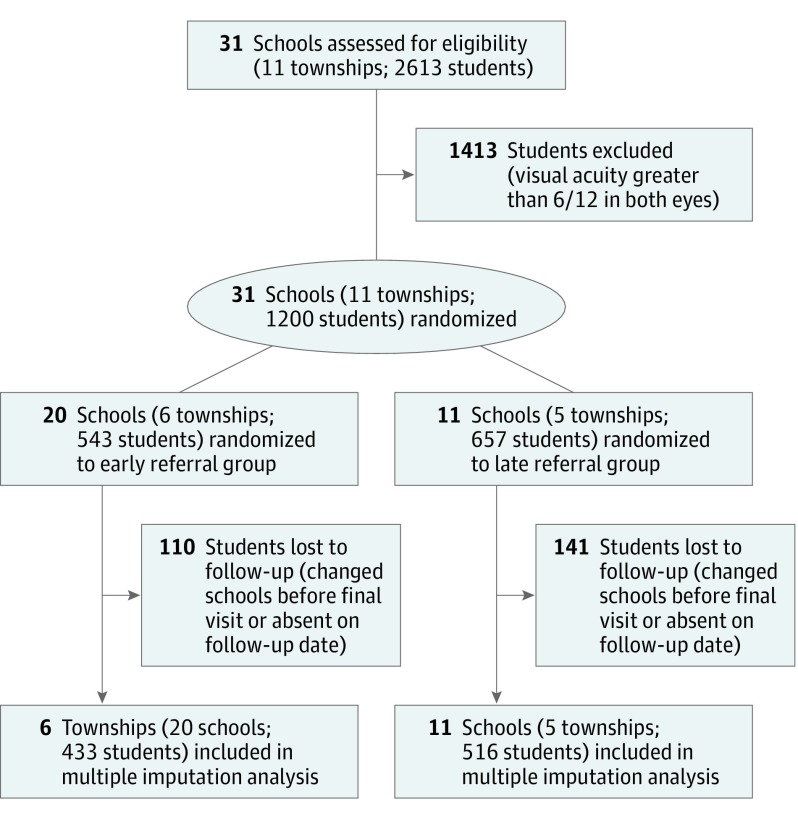
All children included in the study were of Han Chinese race/ethnicity, and 1209 (46.3%) were female. Twenty schools (6 townships, 543 children) were randomized to the early referral group and 11 schools (5 townships, 657 children) to the late referral group (Figure). Of the 2613 children who underwent vision screening at 31 selected schools in 11 townships, 1200 (45.9%) had an uncorrected visual acuity of Snellen 6/12 or worse in either eye. The mean visual acuity at baseline for sample students who met the study criteria for poor vision was Snellen 6/24 (logMAR 95% CI, 0.61-0.64; Snellen equivalent, 6/24-6/30) or worse in the better eye.
Figure. Flow Diagram of Enrollment and Progress of Children Through the Trial.
Of the 1200 students with poor vision identified during the school-based screening, 251 children (20.9%) were lost to follow-up owing to a failure to complete the final mathematics test. This left a final analytic sample of 949 students: 433 children in the early referral group and 516 children in the late referral group (Figure). Children in the 2 groups did not differ on any individual or cluster-level variables at baseline (Table 1).
At the end of the study, unadjusted mathematics scores were higher in the early referral group (0.30 SD; 95% CI, 0.002-0.614; P = .05) (Table 2). This is consistent with results from the full multivariate model (0.25 SD; 95% CI, 0.01-0.48); P = .04) (Table 3). We found that the baseline mathematics score and parental educational level were associated with a higher final mathematics score (Table 3).
Table 2. Mathematics Score, Eyeglasses Ownership, and Wear by Study Group at the Final Visit Among 949 Children.
| Outcome Variables at Final Visit | Early Referral Group (n = 433) | Late Referral Group (n = 516) | P Valuea |
|---|---|---|---|
| Mathematics score, mean (SD) | 0.14 (1.01) | −0.16 (0.97) | .05 |
| Self-reported eyeglasses ownership, No. (%) | 347 (80.1) | 317 (61.4) | .008 |
| Self-reported eyeglasses wear, No. (%) | 326 (75.3) | 286 (55.4) | .03 |
Calculated using the paired 2-sample t test.
Table 3. Linear Regression Model of Potential Factors Associated With the Final Mathematics Score.
| Characteristic | Univariate Model Adjusted for Baseline Mathematics Score (n = 949) | Full Model (n = 949) | ||
|---|---|---|---|---|
| Regression Coefficient (95% CI)a | P Value | Regression Coefficient (95% CI) | P Value | |
| Early referral group | 0.22 (−0.05 to 0.50) | .10 | 0.25 (0.01 to 0.48)b | .04 |
| Male sex | 0.04 (−0.14 to 0.22) | .60 | 0.02 (−0.16 to 0.21) | .77 |
| Baseline standardized mathematics score | 0.53 (0.42 to 0.65)b | <.001 | 0.53 (0.42 to 0.63)b | <.001 |
| Distance between town and county seat | 0.00 (−0.01 to 0.02) | .34 | 0.01 (0.00 to 0.02) | .21 |
| Visual acuity of better eye | 0.32 (−0.36 to 0.42) | .86 | 0.10 (−0.37 to 0.57) | .64 |
| Owned eyeglasses at baseline | −0.04 (−0.22 to 0.14) | .60 | −0.09 (−0.30 to 0.12) | .36 |
| Boarding at school at baseline | 0.04 (−0.18 to 0.25) | .70 | 0.06 (−0.26 to 0.38) | .67 |
| One or both parents with ≥9 y of education | 0.12 (0.01 to 0.23)b | .04 | 0.13 (0.01 to 0.26)b | .03 |
| Both parents out-migrated for work | 0.0001 (−0.21 to 0.21) | .99 | 0.01 (−0.16 to 0.19) | .87 |
Except for the regression coefficient for baseline mathematics score (simple regression), coefficients for the different variables are for multiple models with the final mathematics score as dependent variable after adjustment for the baseline mathematics score.
Indicates comparisons for which the 95% CI for effect size does not cross zero.
Unadjusted results (Table 2) further show that rates of both eyeglasses ownership and eyeglasses wear were higher in the early referral group (ownership: 347 [80.1%] vs 317 [61.4%]; difference, 30 [18.7%] [95% CI, 6.19% to 31.22%]; P = .008; wear: 326 [75.3%] vs 286 [55.4%]; difference, 40 [19.9%] [95% CI, 2.62% to 37.10%]; P = .03). Again, these results were consistent with the results of the multivariate analysis, which showed higher rates of eyeglasses ownership and wear among children in the early referral group. Factors associated with eyeglasses ownership at the end of the study in multivariate models included baseline ownership (relative risk, 1.32; 95% CI, 1.08-1.60; P = .005) and uncorrected visual acuity (children with worse visual acuity were more likely to own eyeglasses: relative risk, 1.76; 95% CI, 1.49-2.08; P < .001). Results were similar for eyeglasses wear at the end of the study, with baseline eyeglasses ownership and worse uncorrected visual acuity the only associated variables (Table 4).
Table 4. Linear Regression Model of Potential Factors Associated With Self-reported Eyeglasses Ownership and Wear.
| Variable | Self-reported Eyeglasses Ownership at End of Study | Self-reported Eyeglasses Wear at End of Study | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate Adjusted for Baseline Ownership, RR (95% CI) (n = 949) | P Value | Full Model, RR (95% CI) (n = 949)a | P Value | Univariate Adjusted for Baseline Ownership, RR (95% CI) (n = 949) | P Value | Full Model, RR (95% CI) (n = 949) | P Value | |
| Early referral group | 1.32 (1.13-1.55)b | .001 | 1.36 (1.15-1.60)b | <.001 | 1.38 (1.07-1.78)b | .01 | 1.43 (1.10-1.86)b | .008 |
| Male sex, No. (%) | 0.96 (0.90-1.03) | .31 | 0.96 (0.89-1.05) | .34 | 0.98 (0.87-1.09) | .70 | 0.97 (0.85-1.12) | .70 |
| Baseline standardized mathematics score | 1.02 (0.96-1.09) | .47 | 1.00 (0.96-1.05) | .99 | 1.02 (0.94-1.11) | .60 | 0.99 (0.94-1.05) | .82 |
| Distance between town and county seat | 1.00 (0.99-1.00) | .22 | 1.00 (0.99-1.00) | .27 | 1.00 (0.99-1.00) | .26 | 1.00 (0.99-1.00) | .37 |
| Visual acuity of better eye | 1.61 (1.29-2.01)b | <.001 | 1.76 (1.49-2.08)b | <.001 | 1.51 (1.22-1.87)b | <.001 | 1.87 (1.59-2.22)b | <.001 |
| Owned eyeglasses at baseline | 1.56 (1.29-1.88)b | <.001 | 1.32 (1.08-1.60)b | .005 | 1.72 (1.35-2.20)b | <.001 | 1.43 (1.11-1.85)b | .005 |
| Boarding at school at baseline | 0.95 (0.81-1.11) | .48 | 0.98 (0.86-1.11) | .76 | 0.99 (0.84-1.17) | .94 | 1.03 (0.89-1.20) | .64 |
| One or both parents with ≥9 y of education | 1.03 (0.99-1.08) | .15 | 1.03 (0.97-1.11) | .29 | 0.99 (0.91-1.09) | .90 | 1.00 (0.91-1.10) | .96 |
| Both parents out-migrated for work | 0.91 (0.81-1.04) | .16 | 0.94 (0.84-1.06) | .29 | 0.89 (0.78-1.01) | .09 | 0.93 (0.82-1.05) | .23 |
Abbreviation: RR, relative risk
Except for the regression coefficient for baseline mathematics score (simple regression), coefficients for the different variables are for multiple models with the final mathematics score as the dependent variable after adjustment for the baseline mathematics score.
Indicates comparisons for which the 95% CI for effect size does not cross zero.
Discussion
Principal Findings
Intention-to-treat analysis in this trial found a statistically significant improvement in mathematics test scores among children randomized to receive early vs late referral to a vision center after vision screening, where they received free eyeglasses if needed. The observed effect size of 0.25 SD is the equivalent of approximately half a semester of additional learning.25
Previous studies of programs providing free eyeglasses8,12,26 have generally shown low resulting ownership and wear, even when educational interventions to promote eyeglasses use were included.8,27 The positive results of this trial have important implications for future eyeglasses distribution programs: our results suggest that placement of a vision center in a local hospital may significantly increase service uptake and educational outcomes.
Comparison With Other Studies
We searched PubMed on April 11, 2014, using the terms refractive error and myopia, cross-indexed with glasses and spectacle, and vision center, vision care, distribution, impact, educational, academic, and school performance for articles published in any language since 1970. We found no previous randomized trials designed to examine the effect of local spectacle service and delivery models on children’s school performance, ownership of eyeglasses, and eyeglasses-wearing behavior.
A recent review25,28 of randomized trials with educational outcomes in primary schools in the developing world listed 60 health-related trials, including 22 deworming studies, with a mean effect size of 0.013 SD, and 38 nutritional studies, with a mean effect size of 0.035 SD. The improved educational outcomes achieved through the provision of eyeglasses in this study (0.25 SD) thus compares favorably with that of other health-related interventions.25,28
Strengths and Limitations
Strengths of this study include its randomized design, population-based sampling, successful collaboration with the local bureau of education and the local county hospital in the conduct of the study, and a policy-relevant choice of county hospital as the distribution point for eyeglasses, all of which increase confidence in the findings and their relevance to actual programs. Weaknesses must also be acknowledged: the unadjusted effect size of our main study outcome was not statistically significant, although the adjusted effect size was significant and the point estimate of 0.25 to 0.3 SD was larger than that recorded in a previous similar trial. Furthermore, all schools were drawn from a single county in rural northwest China, which limits external validity. Other weaknesses include the modest follow-up (79.1%); although children with and without follow-up differed only with regard to visual acuity (Table 1), and follow-up rates did not differ between groups. Also, one of our secondary outcome variables (spectacle wear) relied on self-reported data, which may overestimate actual behavior.8,9 For ethical reasons, our study design delivered an identical service to both groups. This may be viewed as a weakness, but because the late group received refraction and eyeglasses late in the school year, the expected association with our principal outcome, performance on the mathematics test, would logically be reduced by the shorter period of learning without visual impairment. Finally, we did not attempt in the current article to calculate program costs or attempt any economic modeling, which may be valuable in the future.
Conclusions
Despite the limitations, this test of a county hospital–based model of refractive service delivery shows that provision of free eyeglasses both improved children's academic performance and increased their use of eyeglasses. These findings suggest that vision centers may be an important model for China and other counties with a high prevalence of refractive error.
Trial Protocol.
References
- 1.World Health Organization Sight test and glasses could dramatically improve the lives of 150 million people with poor vision. http://www.who.int/mediacentre/news/releases/2006/pr55/en/. Published October 11, 2006. Accessed November 4, 2017. [PubMed]
- 2.Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol. 2000;129(4):445-454. [DOI] [PubMed] [Google Scholar]
- 3.Murthy GV, Gupta SK, Ellwein LB, et al. . Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43(3):623-631. [PubMed] [Google Scholar]
- 4.He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. 2007;114(2):374-382. [DOI] [PubMed] [Google Scholar]
- 5.Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86(1):63-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma X, Congdon N, Yi H, et al. . Safety of spectacles for children’s vision: a cluster-randomized controlled trial. Am J Ophthalmol. 2015;160(5):897-904. [DOI] [PubMed] [Google Scholar]
- 7.Li T. Remedial education with incentivized peer-tutoring: evidence from migrant children schools in China. Dev Econ. 2012;50(4):334-350. [Google Scholar]
- 8.Ma X, Zhou Z, Yi H, et al. . Effect of providing free glasses on children’s educational outcomes in China: cluster randomized controlled trial. BMJ. 2014;349:g5740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yi H, Zhang H, Ma X, et al. . Impact of free glasses and a teacher incentive on children’s use of eyeglasses: a cluster-randomized controlled trial. Am J Ophthalmol. 2015;160(5):889-896.e1. [DOI] [PubMed] [Google Scholar]
- 10.Li L, Lam J, Lu Y, et al. . Attitudes of students, parents, and teachers toward glasses use in rural China. Arch Ophthalmol. 2010;128(6):759-765. [DOI] [PubMed] [Google Scholar]
- 11.Congdon NG, Wang X, Ma Y, et al. . Cluster-randomized controlled trial of the effects on purchase of children's glasses in China: the PRICE (Potentiating Rural Investment in Children's Eyecare) study. PLoS ONE. 2017;12(11):e0187808. doi: 10.1371/journal.pone.0187808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castanon Holguin AM, Congdon N, Patel N, et al. . Factors associated with spectacle-wear compliance in school-aged Mexican children. Invest Ophthalmol Vis Sci. 2006;47(3):925-928. [DOI] [PubMed] [Google Scholar]
- 13.Brien Holden Vision Institute (BHVI) Service Development, http://www.brienholdenvision.org/global-eye-care/service-development.html. Accessed November 4, 2017.
- 14.International Agency for the Prevention of Blindness Vision Center Model. https://www.iapb.org/resource/vision-centre-model. Accessed November 4, 2017.
- 15.Bai Y, Yi H, Zhang L, et al. . An investigation of vision problems and the vision care system in rural China. Southeast Asian J Trop Med Public Health. 2014;45(6):1464-1473. [PubMed] [Google Scholar]
- 16.Fred Hollows Foundation Training. http://www.hollows.org/au/what-we-do/ending-avoidable-blindness/training. Accessed November 4, 2017.
- 17.Helen Keller International (HKI) ChildSight. http://www.hki.org/our-work/helping-people-see/childsight#.V7IwjJOAOko. Accessed November 4, 2017.
- 18.Sightsavers: Sight. http://www.sightsaversusa.org/what-we-do/sight/. Accessed November 4, 2017.
- 19.Wikipedia list of Chinese administrative divisions by GDP per capita in 2015. http://bit.ly/1Y9zlPP. Accessed November 4, 2017.
- 20.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 21.Congdon NG, Patel N, Esteso P, et al. . The association between refractive cutoffs for spectacle provision and visual improvement among school-aged children in South Africa. Br J Ophthalmol. 2008;92(1):13-18. [DOI] [PubMed] [Google Scholar]
- 22.Ferris FL III, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94(1):91-96. [PubMed] [Google Scholar]
- 23.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702-706. [DOI] [PubMed] [Google Scholar]
- 24.Royston P. Multiple imputation of missing values. Stata J. 2004;4(3):227-241. [Google Scholar]
- 25.Hill CJ, Bloom HS, Black R, Lipsey MW. Empirical benchmarks for interpreting effect sizes in research. Child Dev Perspect. 2008;2(3):172-177. [Google Scholar]
- 26.Wedner S, Masanja H, Bowman R, Todd J, Bowman R, Gilbert C. Two strategies for correcting refractive errors in school students in Tanzania: randomised comparison, with implications for screening programmes. Br J Ophthalmol. 2008;92(1):19-24. [DOI] [PubMed] [Google Scholar]
- 27.Congdon N, Li L, Zhang M, et al. . Randomized, controlled trial of an educational intervention to promote spectacle use in rural China: the See Well to Learn Well Study. Ophthalmology. 2011;118(12):2343-2350. [DOI] [PubMed] [Google Scholar]
- 28.McEwan P. Improving learning in primary schools of developing countries: a meta-analysis of randomized experiments. Rev Educ Res. 2015;85(3):353-394. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol.