Key Points
Question
Can binocular optical coherence tomography (OCT) be used to measure the size of strabismus?
Findings
This study included 15 participants with strabismus and 15 healthy volunteers. In participants with strabismus, binocular OCT imaging correctly revealed the type and direction of the deviation and had fair agreement in misalignment size with the alternating prism cover test.
Meaning
These data suggest binocular anterior segment OCT imaging can provide measurements of strabismus with fair agreement to alternating prism cover test, and thus could be useful for diagnosis and monitoring.
Abstract
Importance
Current clinical methods for assessing strabismus can be prone to error. Binocular optical coherence tomography (OCT) has the potential to assess and quantify strabismus objectively and in an automated manner.
Objective
To evaluate the use of a binocular OCT prototype to assess the presence and size of strabismus.
Design, Setting, and Participants
Fifteen participants with strabismus were recruited in 2016 as part of the EASE study from Moorfields Eye Hospital National Health Service Foundation Trust, London, England, and 15 healthy volunteers underwent automated anterior segment imaging using the binocular OCT prototype. All participants had an orthoptic assessment, including alternating prism cover test (APCT), before undergoing imaging. Simultaneously acquired pairs of OCT images, captured with 1 eye fixating, were analyzed using ImageJ (National Institutes of Health) to assess the presence and angle of strabismus.
Main Outcomes and Measures
The direction and size of strabismus measured using binocular OCT was compared with that found using APCT.
Results
The median age for participants with strabismus was 55 years (interquartile range [IQR], 33-66.5 years) and for the healthy group, 50 years (IQR, 41-59 years); 15 participants (50%) were women, and 25 participants (83.3%) were white. The median magnitude of horizontal deviation was 20∆ (IQR, 13-35∆) and for vertical deviation, 3∆ (IQR, 0-5∆). Binocular OCT imaging correctly revealed the type and direction of the deviation in all 15 participants with strabismus, including horizontal and vertical deviations. The APCT and OCT measurements were strongly correlated for the horizontal (Pearson r = 0.85; 95% CI, 0.60-0.95; P < .001) and vertical (r = 0.89; 95% CI, 0.69-0.96; P < .001) deviations. In the healthy cohort, 9 of 15 participants (60%) had a latent horizontal deviation on APCT results (median magnitude 2∆, range 2-4∆). Six (40%) had orthophoria. Horizontal deviations were observed on OCT imaging results in 12 of the 15 participants (80%), and a vertical deviation was visible in 1 participant (6.7%).
Conclusions and Relevance
These findings suggest that binocular anterior segment OCT imaging can provide clinicians with a precise measurement of strabismus. The prototype can potentially incorporate several binocular vision tests that will provide quantitative data for the assessment, diagnosis, and monitoring of ocular misalignments.
This study explores optical coherence tomography–derived quantification and assessment of strabismus angles using a novel prototype binocular optical coherence tomography system.
Introduction
Strabismus is a common condition that can affect both children and adults.1,2 Clinical assessments designed to measure ocular misalignment often require specialist orthoptic expertise and good patient cooperation. An alternating prism cover test (APCT) is most commonly used; however, the end point of such testing can be subtle or variable and is prone to interobserver and intraobserver error, particularly in less cooperative children.3,4 Electronic instruments that use infrared light to track the eye position of both eyes simultaneously, such as video goggles5 and gaze trackers,6 have been developed to increase the precision of measurements but are mainly used for research purposes.
Optical coherence tomography (OCT) devices are becoming ubiquitous in eye clinics as they provide objective and quantitative data about ocular structures to aid in diagnosing and monitoring eye disease. In this article we demonstrate an application of a prototype binocular optical coherence tomography system (Envision Diagnostics) that acquires anterior segment images of both eyes simultaneously, even with 1 eye fixating, and in an automated manner. By analyzing simultaneously acquired pairs of anterior segment images, the presence of strabismus can be identified. We evaluate the use of anterior segment OCT as a method of assessing strabismus and measuring the angle of deviation.
Methods
Participants with strabismus were prospectively recruited from clinics at Moorfields Eye Hospital National Health Service Foundation Trust, London, England, as part of the Human Factor and Usability Testing of a Binocular OCT System (EASE) study (ClinicalTrials.gov Identifier: NCT02822612). Healthy volunteers were recruited from staff members at the hospital. Written informed consent was obtained from all participants in the study. All participants were required to have no significant hearing impairment that would affect their ability to respond to instructions delivered by the device. A conversational level of English was required for users to understand the instructions and to be able to communicate with the device via an English language voice recognition system. No participants were excluded based on disease status to ensure that our cohort consisted of everyday users of eye care services. All participants underwent an orthoptic assessment before receiving a binocular OCT examination, including visual acuity measurement and APCT at distance in primary position, with habitual refractive error correction if appropriate. Approval for data collection and analysis was obtained from a UK National Health Service Research ethics committee (London-Central). The study adhered to the tenets of the Declaration of Helsinki.
Binocular OCT Examination
All participants underwent a binocular OCT examination as described elsewhere.7 Briefly, this is an automated prototype device that acquires OCT images of the anterior and posterior segments of both eyes simultaneously using a tunable swept-source laser without requiring an operator. The device uses a Maxwellian view system to simulate distance fixation. The fixation target was presented to the nondeviating eye in the strabismus group, selected manually before examination. Therefore, the primary deviation was measured on OCT. For healthy participants, the target was presented to the dominant eye (the right eye in all of the participants). The spherical equivalent of the user’s habitual refractive error was corrected within the device.
Measurement of the Angle
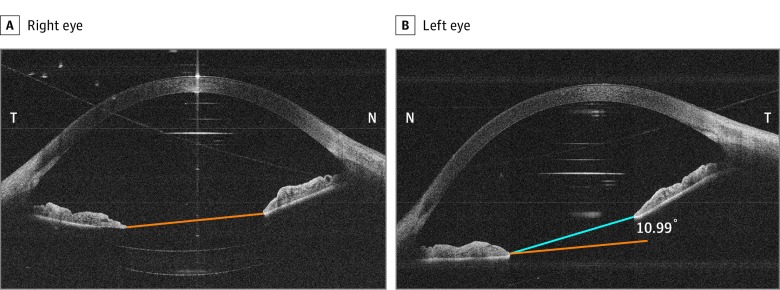
A volume comprising 128 B-scans of the anterior segment was acquired by the device in the horizontal and vertical planes. Only 1 central anterior segment image was used for each plane for analyses. The central image can be deduced by visualizing the corneal vertex reflection in the fixing eye.8 This hyper-reflective line was used as a surrogate for the visual axis. The image captured at the same time was used for the fellow nonfixing eye. The images were adjusted to a 16.5 × 14.9 aspect ratio as they were acquired at a 16.5-mm width and 14.9-mm depth. ImageJ (National Institutes of Health), a widely used open-source Java image analysis program, was used to measure the difference in angles in degrees between the fixing and nonfixing eye. A line was drawn between the pupil margins at the posterior epithelium of the iris for both eyes. These landmarks were chosen because they were visible in the horizontal and vertical scans. The angle between the lines was calculated as the angle of deviation (Figure 1).
Figure 1. Simultaneously Acquired Pair of Anterior Segment Optical Coherence Tomography Images Obtained for Participant 15.
The right eye is the fixating eye (A), and the left eye is the strabismic eye (B). The angle of the deviation is calculated by measuring the tilt of the eye with respect to the fixating eye. The pupil margins are used as landmarks to measure tilt. This pair of images indicates a left esotropia. N indicates nasal; T, temporal.
Outcome Measures
The direction of the deviation was determined by the direction of the fellow eye with respect to the fixating eye in both the horizontal and vertical scans. This was compared with the direction of the misalignment found using APCT for distance fixation. The size of the misalignment was compared with that found using distance APCT. Values in prism diopters (∆) were converted to degrees using the following formula9: degrees = tan-1(Δ/100) × 180/π. Statistical significance was set at P < .05.
Results
Twelve participants (80%) in the group with strabismus had concomitant strabismus, 1 of whom had glaucoma and strabismus. One participant (6.7%) had a decompensated strabismus as a consequence of loss of vision after a retinal detachment. Two participants (13.3%) had an acquired restrictive incomitant strabismus that was related to sphenoid wing meningioma and thyroid eye disease. These participants are described further in the Table. The median age was 55 years (interquartile range [IQR], 33-66.5 years). Thirteen participants (86.7%) were white and 2 participants (13.3%) were Asian. Seven of the 15 participants (46.7%) were women. The median magnitude of horizontal deviation was 20∆ (IQR, 13-35∆), and the vertical deviation was 3∆ (IQR, 0∆-5∆). The mean (SD) spherical equivalent was 0.53 D (2.19) (range for the sphere, −2.50 D to 5.50 D; range for the cylinder, 0 to −3.50 D). The cohort of healthy participants had no manifest deviation. Nine healthy participants (60%) had a latent deviation for distance, and 6 (40%) had orthophoria. The median age of this group was 50 years (IQR, 41-59 years). Twelve healthy participants (80%) were white, 2 (13.3%) were Asian, and one (6.7%) was black. Eight of the healthy participants (53.3%) were women. The mean (SD) spherical equivalent for this cohort was −0.51 D (1.45) (range for the sphere, −3.50 D to 2.75 D; range for the cylinder, 0 D to −2.50 D). All participants understood the examination and were cooperative, as discussed further in a usability study of the device.7
Table. Orthoptic Assessment and Binocular Optical Coherence Tomography Measurements for 15 Participants With Strabismusa.
| Participant | Clinical Diagnosis | Binocular Status in Primary Position | Age, y | Visual Acuity (logMAR) | Mean Spherical Equivalent (Both Eyes) (DS) | Distance Prism Cover Test (6 m) | Prism Cover Test − Equivalent Angle, Degrees | Angle Measured on OCT (Degrees) | OCT Angle Converted to Prism (Rounded to Nearest D) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RE | LE | Horizontal | Vertical | Horizontal | Vertical | |||||||
| 1 | RE consecutive exotropia (prior strabismus surgery for childhood esotropia) | No diplopia, RE suppression | Mid-30s | 0.60 | 0.00 | 0 (Unaided) | 12∆ BI, 5∆ BD, R/L |
6.84 | 2.86 | 6.14 (exo) | 11.13 (RE hyper) | 11∆ BI, 20∆ BD, R/Lb |
| 2 | LE/alternating esotropia (Duane syndrome) | No diplopia, LE suppression | Mid-20s | −0.10 | −0.10 | −0.63 | 45∆ BO | 24.23 | 18.67 (eso) | 2.23 (LE hyper) | 34∆ BO, 4∆ BD, L/R | |
| 3 | RE fully accommodative esotropia | No diplopia, binocular single vision | Early 20s | 0.62 | 0.02 | +2.88 | 6∆ BO, 4∆ BD, R/L |
3.43 | 2.29 | 6.17(eso) | 4.87 (RE hyper) | 11∆ BO, 9∆ BD, R/L |
| 4 | RE consecutive exotropia (prior strabismus surgery for childhood esotropia) | No diplopia, RE suppression | Early 60s | 0.00 | 0.16 | +5.38 | 45∆ BI, 3∆ BD, R/L | 24.23 | 1.72 | 29.34 (exo) | 2.93 (RE hyper) | 56∆ BI, 5∆, R/L |
| 5 | RE consecutive exotropia (prior strabismus surgery for childhood esotropia) | No diplopia, RE suppression | Early 50s | 0.18 | −0.02 | −0.06 | 25∆ BI | 14.04 | 19.83 (exo) | 2.28 (RE hypo) | 36∆ BI, 4∆ BD, L/R |
|
| 6 | LE childhood esotropia | No diplopia, LE suppression | Late 40s | 0.16 | 0.76 | −2.44 | 25∆ BO | 14.04 | 11.08 (eso) | 0.00 | 20∆ BO | |
| 7 | LE longstanding distance esotropia | Diplopia | Mid-70s | 0.00 | 0.00 | −1.25 | 14∆ BO, 4∆ BD, L/R |
7.97 | 2.29 | 12.96 (eso) | 2.18 (LE hyper) | 23∆ BO, 4∆ BD, L/R |
| 8 | LE myopic esotropia | Diplopia | Mid-70s | −0.10 | 0.00 | −0.5 | 25∆ BO, 2∆ BD, R/L |
14.0 | 1.15 | 23.74 (eso) | 3.48 (LE hypo) | 44∆ BO, 6∆ BD, R/L |
| 9 | LE hypertropia (secondary to thyroid eye disease) | Diplopia | Early 60s | −0.10 | 0.00 | +1.25 | 20∆ BD, L/R | 11.31 | 0.00 (ortho) | 18.15 (LE hyper) | 33∆ BD, L/R | |
| 10 | RE residual esotropia with hypertropia (prior strabismus surgery for childhood esotropia) | No diplopia, RE suppression | Early 30s | −0.08 | −0.12 | +3.13 | 14∆BO, 5∆ BD, R/L |
7.97 | 2.86 | 2.07 (eso) | 5.89 (RE hyper) | 4∆ BO, 10∆ BD, R/L |
| 11 | RE exotropia with hypertropia (decompensated after loss of vision from a right retinal detachment) | Diplopia | Early 30s | 0.78 | −0.20 | 0 (Unaided) | 45∆ BI, 3∆ BD, R/L |
24.23 | 2.29 | 16.97 (exo) | 2.02 (RE hyper) | 31∆ BI, 4∆ BD, R/L |
| 12 | LE exotropia with hypotropia (secondary to left sphenoid wing meningioma) | Diplopia | Mid-70s | −0.04 | 0.30 | +1.25 | 20∆ BI, 25∆ BD, R/L | 11.31 | 14.04 | 14.75 (exo) | 14.26 (LE hypo) | 26∆ BI, 25∆ BD, R/L |
| 13 | LE residual exotropia (prior strabismus surgery for childhood exotropia) | No diplopia, LE suppression | Mid-50s | 0.00 | 0.48 | 0 (Unaided) | 60∆ BI, 6∆ BD, R/L |
30.96 | 3.43 | 26.33 (exo) | 6.30 (LE hypo) | 49∆ BI, 11∆ BD, R/L |
| 14 | RE age-related distance esotropia | Diplopia | Late 60s | 0.16 | 0.00 | −1.50 | 6∆ BO | 3.43 | 1.33 (eso) | 0.00 | 2∆ BO | |
| 15 | LE myopic esotropia (and glaucoma) | Diplopia | Early 60s | −0.10 | 0.10 | −0.25 | 16∆ BO | 9.09 | 10.99 (eso) | 1.54 (LE hyper) | 19∆ BO, 3∆ BD, L/R | |
Abbreviations: APCT, alternating prism cover test; BD, base down; BI, base in; BO, base out; L, left; LE, left eye; LoA, limits of agreement; OCT, optical coherence tomography; R, right; RE, right eye.
Vertical deviation measurements obtained using OCT are indicated as hyper or hypo with respect to the strabismic eye (ie, the eye with a horizontal deviation if present).
When denoted R/L, this relates to prism measured on the right eye over the left eye.
Direction and Size of Misalignment
Orthoptic assessments revealed that 5 participants (33.3%) in the strabismus group had a horizontal deviation only, 1 participant (6.7%) had a vertical deviation only, and 9 participants (60%) had both horizontal and vertical deviations. A torsional element was not detected in any participants. Binocular OCT imaging correctly identified the direction of misalignment in all 15 participants with strabismus, including both horizontal and vertical deviations. Three of the 5 participants who were assessed as having a horizontal deviation only using APCT were also found to have an additional vertical deviation on binocular OCT imaging (Table).
There was a strong correlation between measuring strabismus using APCT and the measurement calculated from the OCT images for the horizontal (Pearson r = 0.85; 95% CI, 0.60-0.95; P < .001) and vertical (r = 0.89; 95% CI, 0.69-0.96; P < .001) deviations. The confidence intervals indicate a strong relationship between the 2 methods. Bland-Altman10 plots show heteroscedasticity in which the agreement between the methods decreases as the size of the deviation increases (Figure 2). There was a mean (SD) difference of −0.30° ( ~ −0.52∆) for horizontal misalignment and -2.20° ( ~ −3.84∆) for vertical misalignment. The 95% limits of agreement (LoA) for horizontal misalignment were between 9.55° ( ~ 16.82∆) and −10.16° (−17.55∆). For vertical misalignment the LoA were narrower, between 2.66° ( ~ 4.65∆) and −7.06° (−12.38∆). Regression on the Bland-Altman plots show no significant proportional bias for horizontal misalignments (R2 = 0.44; P = .96); however, the regressions show a significant relationship for vertical misalignments (R2 = 2.32e−4; P = .007).
Figure 2. Equality and Bland-Altman Plots Comparing Agreement of Measurements Obtained Using the Alternating Prism Cover Test (APCT) and Binocular Optical Coherence Tomography (OCT).
Measurements for horizontal misalignments (A and B) and vertical misalignment (C and D). For vertical deviations, the orange dots represent a hypodeviation with respect to the strabismic eye. The blue squares indicate no measured deviation with either method. Regression lines are represented in orange. For the equality plots, the dashed line represents perfect agreement. The reference lines on the Bland-Altman plots show the mean and 95% limits of agreement (LoA). The LoA were ±9.85° from the mean for horizontal misalignments and ±4.86° for vertical misalignments.
In the healthy cohort, 8 (53.3%) had an exophoria (median magnitude, 2∆; range 2-4∆ [1.15°-2.29°]), 1 participant (6.7%) had an esophoria measuring 2∆, and 6 participants (40%) had orthophoria, which were measured using distance APCT. One participant (6.7%) had a vertical deviation on near APCT. No other participants in this group had a vertical or torsional component at distance or nearby. Among the 8 participants with exophoria, 6 had a misalignment corresponding to an exodeviation on OCT results (median [SD] magnitude, 5.25° [ ~ 9.19∆]; IQR, 2.63-6.49° [ ~ 4.59∆-11.38∆]), 1 had an esodeviation on OCT results measuring 8.61° ( ~ 15∆), and 1 participant had no deviation on OCT results. From the 6 participants with orthophoria, 3 had an exodeviation on OCT results (range, 2.93°-6.38°) and 1 had an esodeviation (4.09°). The single participant with an esophoria did not have any measured deviation on the binocular OCT results. Two participants measured as orthophoric on APCT also had orthophoria on binocular OCT results. A vertical component corresponding to a left hyperdeviation was identified in 1 healthy participant on OCT measuring 2.26° ( ~ 3.95∆). This participant did not have a vertical latent deviation on distance APCT but did have a left hyperphoria measuring 5∆ on near APCT. A weak correlation was observed between APCT and OCT measurements for horizontal deviation in this group (r = 0.06, 95% CI, 0.14-0.85; P = .83).
Discussion
In this study we explored OCT-derived quantification and assessment of strabismus angles using a novel prototype binocular OCT system. The device was able to correctly identify the direction of the deviation in the strabismus group, including horizontal and vertical elements. The device also indicated a vertical deviation (<4∆) in 3 participants, who were recorded as having vertical orthophoria. Small deviations (<2∆), particularly vertical deviations, may not be reliably perceived by the unaided eye on cover testing11,12 but may be visible on the OCT. The binocular OCT identified a horizontal deviation in 12 participants (80%) of the healthy cohort. In 9 of these participants, the direction of the deviation on OCT was the same as the latent deviation found on APCT. This suggests that the binocular OCT is measuring both manifest and latent components.
In horizontal misalignment, the agreement between the methods tended to decrease as the size of the deviation increased. A similar heteroscedastic pattern was found for vertical misalignments; however, our sample was skewed toward smaller deviations. The LoA were larger than the interexaminer variability found by de Jongh et al13 for horizontal deviations (10∆). This would suggest that our method is not in strong agreement with APCT. However, a larger sample is required to confirm inferences from Bland-Altman plots. Differences between the methods may be partly attributable to the limited scale of prism diopters; as the deviation becomes larger, the difference in degrees between each prism diopter also increases. In addition, increments between diopters in prism bars increase as the power increases. For example, between 1∆ to 10∆, prism power increases in increments of 1 diopter, whereas between 20∆ to 50∆, power increases by 5∆ increments, forcing the orthoptist to choose the closest prism that neutralizes the misalignment. However, the binocular OCT is able to measure strabismus angles more precisely using a scale of degrees instead of diopters. A longitudinal and repeatability study is required to validate this method and to investigate whether OCT-derived measurements are valuable for monitoring the change in misalignment size over time.
Limitations
The device currently has several limitations, however, it is likely that these can be overcome in future iterations. A significant limitation of the device includes the inability to ascertain whether a heterophoria or heterotropia is present. We observed deviations in both the healthy and strabismus cohorts. It is likely that the device is reliably identifying manifest vertical and horizontal components in the strabismus group. However, if the device was used as a screening device for manifest strabismus, it may have a high false-positive rate, particularly for horizontal deviations, as observed in the healthy cohort. The unique features of the binocular OCT could potentially be extended to perform a cover test by switching the fixation between the eyes to differentiate between these entities. In this study, all participants with strabismus had a constant deviation. Those with intermittent deviations may not be identified using the current prototype setup. Real-time video OCT with 3-dimensional rendering would also aid the measurement of torsional deviations. By bringing the fixation target closer to the eyes, the device has the capacity to simulate near fixation to measure deviations at various distances. In addition, the current prototype setup performs ocular motility testing by displaying the fixation target at different locations of the screen.7 Strabismus with varying gaze or motion, in addition to alternating fixation, may help discern between primary and secondary deviations in incomitant strabismus.
The prototype currently corrects a mean spherical equivalent of the user’s habitual correction to aid visualization of the fixation target. Refractive error can affect the size of the deviation, and the inability to correct cylindrical error may contribute to the differences that were observed between the methods. Additionally, although the device simulates distance fixation, proximal convergence may attribute to differences between APCT and OCT measurements. In 1 participant with exophoria, a significant esodeviation was found on OCT. Monocular viewing conditions have been shown to cause accommodative convergence, which may affect these results.14 In subsequent devices with binocular viewing conditions this may be reduced. Some users of the device may naturally fixate closer than distance fixation, and this could explain the larger exodeviations found on OCT compared with APCT in the healthy cohort. This may also explain the vertical component found in the 1 healthy participant who had a vertical deviation at near.
Our method of using the pupil margin as a reference plane for tilt may have contributed to this error. An anatomical landmark, such as the Schwalbe line, may be less variable, as this cannot change dynamically like the iris, but may be less discernible, particularly in vertical scans because of occlusion of this landmark by the eyelids. Visual axis data could potentially provide more accurate measurements of strabismus. This could be determined by using retinal OCT images of the fovea that are also acquired using the device. The device currently does not measure axial length, which prevents mapping the retinal and anterior segment images to each other to determine the visual axis. However, if axial length data could be obtained, the visual axis could potentially provide a reliable method of measuring strabismus using OCT, particularly in strabismus with normal retinal correspondence.
Conclusions
We present a novel application of OCT imaging to detect and measure ocular misalignment. The advantage of this method is the ability to detect subtle differences in the size of strabismus that may not be visible to the naked eye. This is encompassed within a device that can perform several functional tests in addition to whole-eye imaging. The automated manner of the device means that a highly skilled specialist is not required to take measurements of the deviation, therefore making it ideal for screening purposes. As discussed, measuring strabismus using prism bars has limitations, particularly at larger angles. The binocular OCT can provide a more precise measurement of this angle using degrees (without converting back to prism diopters). This may be useful for measuring strabismus over time, before and after surgery, or for patients who are undergoing botulinum toxin injections. Although the current setup has many caveats, future iterations of the binocular OCT may allow quicker and more accurate assessments of strabismus, particularly when orthoptists are limited with huge patient volumes. In addition, the device can output objective quantitative data for ocular misalignments, as well as for other diagnostic tests,7 aiding the diagnosis and monitoring of eye disease.
References.
- 1.Graham PA. Epidemiology of strabismus. Br J Ophthalmol. 1974;58(3):224-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stidwill D. Epidemiology of strabismus. Ophthalmic Physiol Opt. 1997;17(6):536-539. [PubMed] [Google Scholar]
- 3.Pediatric Eye Disease Investigator Group Interobserver reliability of the prism and alternate cover test in children with esotropia. Arch Ophthalmol. 2009;127(1):59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johns HA, Manny RE, Fern K, Hu YS. The intraexaminer and interexaminer repeatability of the alternate cover test using different prism neutralization endpoints. Optom Vis Sci. 2004;81(12):939-946. [PubMed] [Google Scholar]
- 5.Weber KP, Rappoport D, Dysli M, et al. . Strabismus measurements with novel video goggles. Ophthalmology. 2017;124(12):1849-1856. [DOI] [PubMed] [Google Scholar]
- 6.BCN Innova Gazelab. http://www.bcninnova.com/gazelab. Accessed October 18, 2017.
- 7.Chopra R, Mulholland PJ, Dubis AM, Anderson RS, Keane PA. Human factor and usability testing of a binocular optical coherence tomography system. Transl Vis Sci Technol. 2017;6(4):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Shekhar R, Huang D. Corneal pachymetry mapping with high-speed optical coherence tomography. Ophthalmology. 2006;113(5):792-799.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irsch K. Optical issues in measuring strabismus. Middle East Afr J Ophthalmol. 2015;22(3):265-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307-310. [PubMed] [Google Scholar]
- 11.Ludvigh E. Amount of eye movement objectively perceptible to the unaided eye. Am J Ophthalmol. 1949;32(5):649-650. [DOI] [PubMed] [Google Scholar]
- 12.Romano PE, von Noorden GK. Limitations of cover test in detecting strabismus. Am J Ophthalmol. 1971;72(1):10-12. [DOI] [PubMed] [Google Scholar]
- 13.de Jongh E, Leach C, Tjon-Fo-Sang MJ, Bjerre A. Inter-examiner variability and agreement of the alternate prism cover test (APCT) measurements of strabismus performed by 4 examiners. Strabismus. 2014;22(4):158-166. [DOI] [PubMed] [Google Scholar]
- 14.Chirre E, Prieto P, Artal P. Dynamics of the near response under natural viewing conditions with an open-view sensor. Biomed Opt Express. 2015;6(10):4200-4211. [DOI] [PMC free article] [PubMed] [Google Scholar]