Abstract
To date, all the authors who have recommended external rotation osteotomy (ERO) in the late treatment of obstetrical brachial plexus palsy (OBPP), have neglected upper limb length discrepancy, which is an another sequelae of OBPP. In this paper, a new technique is reported for the late treatment of OBPP patients with upper limb length discrepancy, in which both humeral external rotation osteotomy (ERO) and lengthening are applied with an intramedullary elongation nail. With this technique, upper limb function is improved through re-orientation of the shoulder arc to a more functional range, and further improvements will be seen in the appearance of the upper limb with the elimination of length discrepancy. It is also advocated that there is a potentiating effect of the humeral lengthening on shoulder movements gained by ERO when the osteotomy is applied above the deltoid insertion, as this allows more lateralized placement of the deltoid insertion.
Keywords: Obstetrical brachial plexus palsy, Humeral lengthening, Elongation nail, Lengthening nail
Introduction
The incidence of obstetric brachial plexus palsy has been reported to range from 1 to 4 cases per 1000 live births, with higher rates in underdeveloped countries.1 The classical injury is Erb's palsy (involving C5, C6 ± C7 roots), but all roots can be involved in total paralysis with a worse prognosis.
Spontaneous complete recovery is seen in most children during the first months of life, but a degree of residual dysfunction is present in 5%–19%.2 Fixed adduction and internal rotation deformity of the shoulder is the most common sequela of OBPP, seen at varying severity and usually together with a degree of fixed pronation of the forearm with elbow flexion contracture.3 Shoulder deformities result from a failure in neuromuscular recovery which causes an imbalance between antagonist muscles which dominate the internal rotators and adductors of the shoulder and this may cause progressive glenohumeral dysplasia and/or joint instability in the long-term.4
Older children with long-standing brachial plexus palsy and moderate-to-severe glenohumeral deformity (Waters IV, V, VI) are good candidates for external rotation osteotomy (ERO) to improve upper extremity function with re-orientation of the arc of the shoulder into a more functional range and position.3, 5 Historically, external rotational osteotomies are stabilized with external cast immobilization, interosseous or periosteal sutures, or staples.3 Nowadays, an open approach and rigid internal fixation with a plate is recommended. Recently, Aly et al reported a new technique of percutaneous humeral osteotomy with osteosynthesis using a Hoffmann external fixator.6 To date, no surgical technique has been defined to deal with the upper limb length discrepancy which is also a sequela of OBPP and contributes to the appearance of the affected limb.7, 8 In this paper, a new technique is presented for the late treatment of OBPP, using humeral rotational osteotomy and lengthening with an elongation nail.
Case
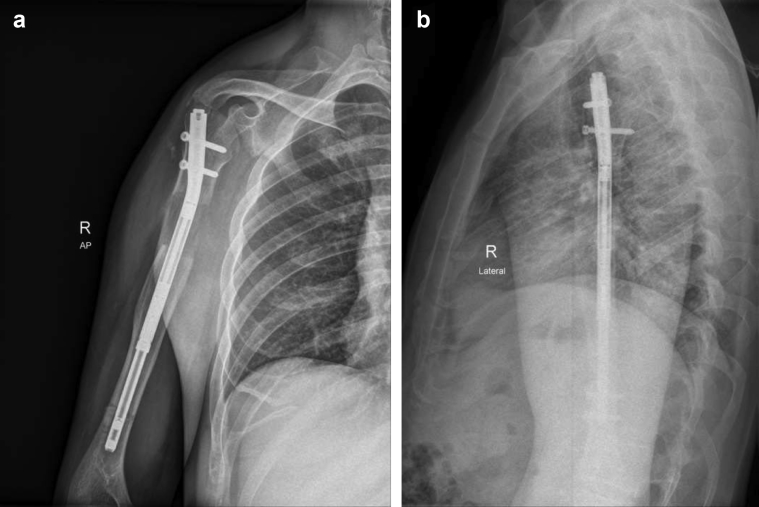
A 33 year-old male was admitted to our clinic suffering from right OBPP sequelae with C5 and C6 injury. The patient presented with internal rotation contracture of the right-side shoulder, pronated forearm and 5 cm limb length discrepancy. Together with the functional limitations, the patient was experiencing low self-esteem because of the appearance of the arm. He had no previous operations. The shoulder range of motion was recorded pre-operatively as external rotation −80° in adduction, internal rotation 100°, abduction 20°, and flexion 20°. Preoperative plain radiographs demonstrated the osseous deformity of the glenohumeral joint (Fig. 1a, b). A score of 1 was obtained in the preoperative shoulder function assessment using the modified Mallet scoring system.
Fig. 1.
a, b: Pre-operative AP and Lat. X-rays.
Surgical technique
The procedure was performed under general anesthesia in the beach chair position. The flouroscopy machine was placed on the opposite side of the table to ensure a good AP and axillary view. The entire affected upper extremity was then prepared and draped for the surgical field. A standard deltopectoral approach was applied. Under fluoroscopy guidance, the entry point for the nail was determined through the sulcus between the greater tuberosity and the articular surface. The medullary canal was reamed to 12.5 mm with elastic reamers in 0.5 mm increments under flouroscopy guidance control to obtain 1.5–2 mm overreaming. A transverse osteotomy between the insertion of the deltoid and pectoralis major muscles was performed with a small oscillating blade under continuous irrigation to avoid thermal necrosis. Then, a 10.7 mm × 255 mm antegrade tibial lengthening nail (ISKD, Orthofix Inc, Lewisville, TX, USA) with a 5 cm lengthening capacity was implanted (Fig. 2a, b). Proximal locking was performed with a drill guide. Prior to the distal locking of the nail, adequate rotation of the humerus was decided intraoperatively by ascertaining that the ipsilateral hand could be placed to the mouth while putting the flexed elbow to the side of trunk. Once the desired amount of rotation was achieved, the distal locking screws were placed using a free hand technique with a radiolucent gear drive using a mini open approach to protect the radial nerve. Finally, fixation was checked under fluoroscopy.
Fig. 2.
a, b: Post-operative plain AP and Lat. X-rays.
Postoperative care
The shoulder activity was limited by immobilization with a shoulder abduction orthosis and bed rest in the first 5 days after surgery. Using a magnetic control device, it was confirmed that there was no lengthening in the first 5 days. Distraction was initiated on postoperative day 5 with a 0.25-mm distraction rate every 6 h and prior to the patient being discharged, radiographs were taken. The patient was instructed in the need to perform the lengthening process 4 times a day and it was explained how to use the magnetic monitor after every lengthening. Follow-up radiographs were taken weekly during the distraction period of the lengthening to be able to check the lengthening process. During the distraction period, the upper limb was kept in a shoulder abduction orthosis to avoid excessive rotational movements and only passive shoulder and elbow movements were permitted in a controlled way. After completion of the planned 5 cm lengthening in 6 weeks, active-assisted movements were permitted and the distracted osteotomy site consolidation was monitored with radiographic follow-up every 4 weeks (Fig. 3a, b). Three months after the operation, the weight limitation was removed as all four cortices at the osteotomy site were visualised on the radiographs (Fig. 4a, b). At 9 months, bone healing was completed (Fig. 5a, b). At 15 months post-operatively, the nail was extracted in a second operation. At the 3-year follow-up examination, shoulder range of motion was recorded as active external rotation 0° and passive external rotation 40° in adduction, internal rotation 70°, abduction 100°, and flexion 120°. A modified Mallet score of 4 was obtained. The patient's hand was able to reach to the occiput with the absence of the trumpet sign, and the palm rather than the dorsum was facing the mouth, which he could not do before the operation (Fig. 6).
Fig. 3.
a, b: At the end of 5 cm distraction, AP and Lat. X-rays.
Fig. 4.
a, b: After 3 months, AP and Lat. X-rays.
Fig. 5.
a, b: At 9 months. AP and Lat. X-rays.
Fig. 6.
Range of motions at 36 months.
Discussion
To date, all the authors who have recommended ERO in the late treatment of OBPP, have neglected upper limb length discrepancy which is an another sequela of OBPP. In this paper, a new technique is presented for late treatment of OBPP in patients with upper limb length discrepancy, using humeral ERO and lengthening with an elongation nail. With this technique, in addition to the improvement of upper limb function by re-orientation of the shoulder arc into a more functional range, further improvement will be seen in the appearance of the upper limb with the elimination of length discrepancy, visible antecubital fossa and diminished forearm pronation. Moreover, it is also advocated that lengthening the humerus with the osteotomy above the deltoid insertion, will allow a more lateralized placement of deltoid insertion, thus improving shoulder abduction more than expected. In this case, the lengthening of the humerus increases the effect of the ERO by providing better functional recovery in addition to the improvement in the appearance of the upper limb. In literature, 5–6 cm upper limb length discrepancy is the accepted value for lengthening.9 However, lower values should be accepted in the late treatment of OBPP with this technique to take advantage of the more lateralized deltoid insertion. Nevertheless, it must be kept in mind that lengthening the humerus from the osteotomy side that is proximal to the deltoid insertion is not a good place due to its incremental pressure on the shoulder joint that can also cause dislocation, especially in OBBP cases. In the current case, upper migration of the humeral dysplastic head was observed at the end of 5 cm distraction. On the follow-up radiographs, upper migration of the humeral head can be determined from the visualised contact of the humeral head with the acromion (Fig. 2). The development of such a complication was predicted to lead to restriction in the range of movement gained in the shoulder, particularly in abduction, and a painful shoulder. However, at the end of the 3-year follow-up period, the modified Mallet score was 4 and the patient was able to reach the occiput without any trumpet sign, and the palm rather than the dorsum was facing the mouth, which he could not do before the operation (Fig. 6).
In recent years, fully implantable, mechanical or motorized elongation nails have been developed to avoid the problems caused by external fixators in limb lengthening. However, these devices have their own unique complications, especially related to the lengthening mechanisms. The main problem with ISKD nail is the difficulty in controlling the lengthening.10 In the technique used in the current case, ISKD was used with close monitoring during the distraction period to avoid uncontrolled lengthening. The ISKD nail used was 10.7 mm in diameter, which is the minimum diameter option for ISKD. This may present problems in the treatment of younger patients with a narrower meduller cavity, but there is also the option of the 8.5 mm diameter Precice nail. To be able to use this technique with an elongation nail, the medulla should be reamed at least up to 10 mm, taking 1.5–2 mm over-reaming into account. The minimum length option of the Precice nail is 195 mm, which also has to be considered.
Some authors have recommended ERO with added flexion to the distal part of the humerus to create increased flexion of the arm.11 Others have recommended adding a varus component to repair the abduction contracture.12, 13 With this new technique, it is impossible to add varus or flexion to the distal part of the humerus, due to use of the intramedullary elongation nail.
In conclusion, this is a report of a new surgical technique which takes account of upper limb length discrepancy in the late treatment of OBPP. With this technique, both ERO and lengthening can be applied with an elongation nail from the transverse osteotomy proximal to the deltoid insertion. It can also be said that the effect of humeral lengthening on functional improvements, especially in shoulder abduction, is potentiated by ERO. However, it must not be forgotten that the potential complication of upper migration of the humeral head may endanger the gain in range of shoulder motion in the long-term. Although there is the limitation of this report being of a single case rather than a series, benefits of the technique are apparent. There is a need for long-term, comprehensive, comparative studies to evaluate the advantages, limitations and complications of this technique.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Kay S.P. Obstetrical brachial palsy. Br J Plast Surg. 1998 Jan;51(1):43–50. doi: 10.1054/bjps.1997.0166. [DOI] [PubMed] [Google Scholar]
- 2.Pondaag W., Malessy M.J., van Dijk J.G., Thomeer R.T. Natural history of obstetric brachial plexus palsy: a systematic review. Dev Med Child Neurol. 2004 Feb;46(2):138–144. doi: 10.1111/j.1469-8749.2004.tb00463.x. [DOI] [PubMed] [Google Scholar]
- 3.Kirkos J.M., Papadopoulos I.A. Late treatment of brachial plexus palsy secondary to birth injuries: rotational osteotomy of the proximal part of the humerus. J Bone Jt Surg Am. 1998 Oct;80(10):1477–1483. doi: 10.2106/00004623-199810000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Waters P.M., Smith G.R., Jaramillo D. Glenohumeral deformity secondary to brachial plexus birth palsy. J Bone Jt Surg Am. 1998 May;80(5):668–677. doi: 10.2106/00004623-199805000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Al-Qattan M.M. Rotation osteotomy of the humerus for Erb's palsy in children with humeral head deformity. J Hand Surg Am. 2002 May;27(3):479–483. doi: 10.1053/jhsu.2002.33198. [DOI] [PubMed] [Google Scholar]
- 6.Aly A., Bahm J., Schuind F. Percutaneous humeral derotational osteotomy in obstetrical brachial plexus palsy: a new technique. J Hand Surg Eur Vol. 2014 Jun;39(5):549–552. doi: 10.1177/1753193413492058. Epub 2013 Jun 7. [DOI] [PubMed] [Google Scholar]
- 7.McDaid P.J., Kozin S.H., Thoder J.J., Porter S.T. Upper extremity limb-length discrepancy in brachial plexus palsy. J Pediatr Orthop. 2002 May-Jun;22(3):364–366. doi: 10.1097/01241398-200205000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Bae D.S., Ferretti M., Waters P.M. Upper extremity size differences in brachial plexus birth palsy. Hand (N Y) 2008 Dec;3(4):297–303. doi: 10.1007/s11552-008-9103-5. Epub 2008 Apr 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dahl T.M. Upper-extremity lengthening. In: Gupta A., Kay S.P.J., Scheker L.R., editors. The Growing Hand: Diagnosis and Management of the Upper Extremity in Children. Mosby; London: 2000. pp. 1049–1056. [Google Scholar]
- 10.Mahboubian S., Seah M., Fragomen A.T., Rozbruch S.R. Femoral lengthening with lengthening over a nail has fewer complications than intramedullary skeletal kinetic distraction. Clin Orthop Relat Res. 2012 Apr;470(4):1221–1231. doi: 10.1007/s11999-011-2204-4. Epub 2011 Dec 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Zahrani S. Combined Sever's release of the shoulder and osteotomy of the humerus for Erb's palsy. J Hand Surg Br. 1997 Oct;22(5):591–593. doi: 10.1016/S0266-7681(97)80352-X. [DOI] [PubMed] [Google Scholar]
- 12.Bae D.S., Waters P.M. External rotation humeral osteotomy for brachial plexus birth palsy. Tech Hand Up Extrem Surg. 2007 Mar;11(1):8–14. doi: 10.1097/01.bth.0000248359.14448.e6. [DOI] [PubMed] [Google Scholar]
- 13.Waters P.M., Bae D.S. The effect of derotational humeral osteotomy on global shoulder function in brachial plexus birth palsy. J Bone Jt Surg Am. 2006 May;88(5):1035–1042. doi: 10.2106/00004623-200605000-00014. [DOI] [PubMed] [Google Scholar]