Abstract
Objective
This study aimed to present a treatment algorithm for the correction of the hallux valgus deformity in Cerebral Palsy (CP) patients and to discuss the outcomes based on our clinical and radiological results.
Methods
29 patients (45 feet) were included in the study. The mean age of the patients at the time of the surgery was 14 (range 6–22) years. The mean follow-up was 33 (range 22–59) months. A reconstructive procedure was performed on 19 patients (27 feet); a soft tissue surgery and exostectomy of the bunion in six patients (11 feet); and MTP joint arthrodesis in four patients (7 feet). The hallux valgus angle (HVA) and the anteroposterior intermetatarsal angle (IMA) were used for radiologic evaluation and the DuPont Bunion Rating Score was used for clinical evaluation.
Results
The follow-up period was 36 (range 22–59) months in reconstructive group, 27 (range 24–29) months in soft tissue group, and 29 (range 23–41) months in MTP arthrodesis group. Significant improvements were detected in hallux valgus angle in three groups postoperatively but in soft tissue group correction loss was observed during follow up. Best results were achieved in arthrodesis group and worse in soft tissue group in terms of clinical evaluation.
Conclusion
According to our results isolated soft tissue procedures are ineffective in CP patients. Soft tissue procedure combined with metatarsal osteotomy has satisfactory results.
Level of evidence
Level IV, therapeutic study.
Keywords: Cerebral palsy, Hallux valgus, Surgical treatment, Toe deformity, Hallux valgus algorithm
Introduction
Hallux valgus is part of a complicated foot malalignment pathology that may affect patients with spastic cerebral palsy (CP) by causing functional disabilities.1, 2 Surgical correction of the deformity is indicated to address disabilities, including pain, difficulty with shoe wear or use of orthotics, poor foot hygiene, skin breakdown, nail infection, and pathologic gait.3, 4
When surgical correction is considered, metatarsophalangeal joint (MTP) arthrodesis is accepted as a primary treatment method. By contrast, reconstructive procedures, such as soft-tissue balancing or corrective osteotomies, are not very beneficial and recurrence rates are high.5, 6, 7, 8, 9, 10 However, primary MTP joint arthrodesis hinders forefoot motion, which is essential for stair walking and for push-off for the heel-to-toe gait, and this leads to joint stiffness.8 In addition, non-union is a common complication of MTP joint arthrodesis.
The available literature lacks any treatment algorithm for hallux valgus deformity in children with CP. We argue that the correction of the hallux valgus deformity, together with the simultaneous correction of a foot malalignment and without hindering forefoot motion, would be effective in most of these cases.
The purpose of this study was to present our treatment algorithm for the correction of the hallux valgus deformity in CP patients and to discuss the outcomes based on our clinical and radiological results.
Patients and methods
Patients with spastic CP who underwent operations between 2013 and 2015 for hallux valgus were evaluated retrospectively. In total, 29 patients (45 feet, bilateral in 16 patients) were included in the study. The mean age of the patients at the time of the surgery was 14 (range 6–22) years. The mean follow-up was 33 (range 22–59) months.
None of the patients had undergone a previous foot surgery. Of the 29 patients, 25 had undergone concomitant surgeries at the same extremity: 19 gastrocnemius recessions, 11 Achilles tendon lengthening, 36 lateral column lengthening in 21 patients, three subtalar arthrodesis surgeries in two patients for pes planovalgus, two talonavicular arthrodesis in one patient in conjunction with lateral column lengthening, one femoral varus-derotation osteotomy, one tibial derotation osteotomy, and six supracondylar femoral extension osteotomies in three patients.
The indication for surgical treatment was a hallux valgus deformity in the CP patient with pain over the forefoot and medial eminence after failed conservative treatment, such as wide shoes or orthosis. A reconstructive procedure was performed on 19 patients (27 feet); a soft tissue surgery and exostectomy of the bunion in six patients (11 feet); and MTP joint arthrodesis in four patients (7 feet).
The reconstructive procedures consist of a distal first metatarsal osteotomy according to Lindgren-Turan technique,11 soft tissue surgery, and exostectomy of the bunion.12 In the first stage, a three-cm dorsal longitudinal incision was centered in the first intermetatarsal web space. The adductor hallucis tendon was released from the base of the proximal phalanx. The transverse metatarsal ligament was then transected. At this point, the first MTP joint congruency was evaluated and the flexor hallucis brevis and lateral joint capsule were resected, if necessary. In the second step, a medial incision was made in the midline between the midportion of the proximal phalanx and two cm beyond the medial eminence. A vertical capsular incision was made proximal to the base of proximal phalanx, and a second capsular incision was made 5 mm proximally and parallel to the first one. The medial eminence was then removed, with the bursa overlying the MTP joint, in a line parallel with the medial diaphyseal cortex of the first metatarsal. The medial joint capsule was repaired during the hallux and then placed in correct alignment. In the third stage, the periosteum was elevated around the first metatarsal as far distally as possible through the second incision. An osteotomy was done 1,5 cm proximal to the metatarsal head, with a lateral inclination of 30° with the metatarsal joint surface.11 After the osteotomy, the distal fragment was displaced as far laterally as possible, and the tip of the proximal fragment was resected. The osteotomy was fixed with a cancellous cannulated bone screw or two Kirschner wires (Fig. 1).
Fig. 1.
Preoperative and postoperative radiographs of a patient.
The first MTP joint fusion involved a dorsal longitudinal incision along the great toe and the adjacent first metatarsal, along the medial edge of the extensor hallucis longus tendon. Cartilage was removed while preserving the contour of the metatarsal head and the base of the proximal phalanx. Internal fixation was performed with a transphalangeal intramedullary screw.
An ankle foot orthosis (AFO) with a toe plate was used for three weeks to protect the soft-tissue repair. The Kirschner wires (if used) were removed three weeks after surgery. At the sixth week after a bone procedure, full weight bearing was allowed if complete bone union was confirmed with radiographs. Patients were allowed full weight bearing immediately after an isolated soft tissue surgery.
Anteroposterior and lateral radiographs of the feet were obtained. The hallux valgus angle (HVA) and the anteroposterior intermetatarsal angle (IMA) were used. The radiographs were examined periodically for union at the site of the osteotomy. Bone union was defined by signs of a bridging callus and the ability to bear weight without pain.
The DuPont Bunion Rating Score, as modified by Jenter et al,8 was used to assess the clinical outcome of the surgical procedures (Table 1). Complications, such as wound infections, non-unions, loss of correction, overcorrection, and recurrence of the deformity, were recorded.
Table 1.
The DuPont Bunion Rating Score: excellent, 23–25 points; good, 20–22 points; fair, 17–19 points; poor, <16 points. Modified in cases of MTP arthrodesis by subtracting 5 points because of expected loss of motion: excellent, 17–20; good, 14–16; fair, 11–13; poor, <10. Jenter M, Lipton GE, Miller F. Operative treatment for hallux valgus in children with cerebral palsy. Foot Ankle Int. 1998 Dec; 19(12):830–5. (DF, dorsiflexion; PF, plantar flexion; RSD, reflex sympathetic dystrophy).
| Evaluation score | 5 point | 4 point | 3 point | 2 point | 1 point |
|---|---|---|---|---|---|
| Hallux valgus angle | 0–15 | 16–25 | 26–35 | 36–45 | >45 or varus |
| IMA | <9 | 10–15 | 16–20 | 21–25 | >25 |
| Dorsiflexion Plantar flexion |
>25 >15 |
15 < DF < 25 or 10 < PF < 15 |
15 < DF < 25 and 10 < PF < 15 |
DF < 15 or PF < 10 |
No motion |
| Pain | None | Occasional, not limiting |
Constant, not limiting |
Constant, limiting | RSD |
| Cosmesis | Excellent | Good | Fair | Poor | Worse than preoperative |
The correlations were evaluated statistically using SPSS 15 (SPSS Inc., Chicago, IL; USA). For descriptive statistical methods and to compare the differences between means of groups Chi-square test was used. Kruskal Wallis test was used to compare the difference between means of three groups and then Dunn's test was used for comparing the differences between means of two subgroups. A p value of less than 0.05 was accepted as statistically significant.
Results
The mean age was 14 (range 6–22) years in reconstructive group, 14 (range 13–15) years in soft tissue group, and 13 (range 11–15) years in MTP arthrodesis group. The follow-up period was 36 (range 22–59) months in reconstructive group, 27 (range 24–29) months in soft tissue group, and 29 (range 23–41) months in MTP arthrodesis group.
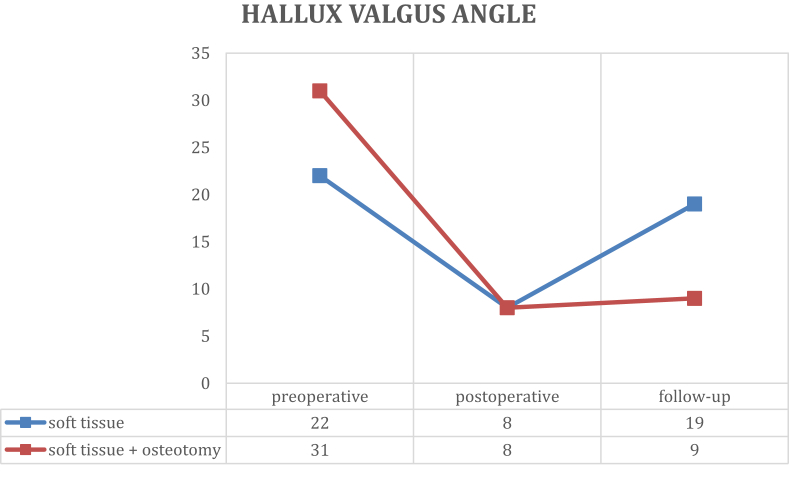
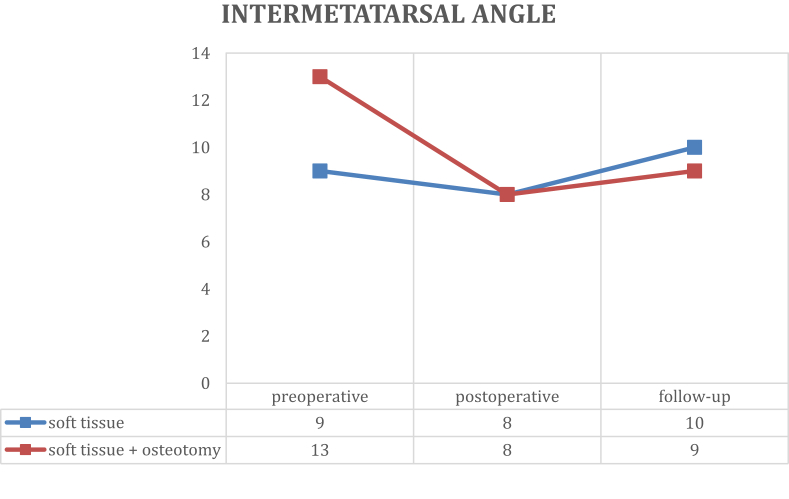
The mean HVA in the reconstructive group improved from 31°±8° preoperatively to 8°±5° postoperatively and to 9°±5° at follow-up (Table 2). The difference between the mean preoperative and postoperative HVA values was statistically significant(p = 0.0001). The mean HVAs in the soft tissue group were 22°±2° preoperatively, 10°±2° postoperatively, and 19°±4° at the final follow-up (Table 2). The mean HVA in the MTP arthrodesis group was 35°±5° preoperatively, 3°±3° postoperatively, and 3°±5° at the final follow-up.
Table 2.
The hallux valgus angles of patients who underwent only a soft tissue procedure and patients who underwent an osteotomy in addition to soft tissue surgery. Deterioration of the HVA during follow-up after soft tissue reconstruction is readily observed.
In reconstruction group the mean IMA values were measured as 13°±3° and 7°±3° before and after procedures, respectively(p = 0.0001). At the last follow-up, the mean IMA was 9°±3 (Table 3). The mean preoperative, postoperative, and follow-up IMA values in the soft tissue group were almost the same (Table 3). In the MTP arthrodesis group, the mean IMA was 16°±3° preoperatively and 11°±5° at both postoperative and final follow-up measurements.
Table 3.
The intermetatarsal angles of patients who underwent only soft tissue procedure and of patients who underwent osteotomy in addition to soft tissue surgery. No significant change was noted in the IMA after soft tissue reconstruction, as expected.
The modified DuPont Bunion Rating Score gave 17 excellent outcomes, eight good outcomes, and two fair outcomes in the reconstruction group. The soft tissue group had one good and ten fair outcomes at the end of follow up period. The MTP arthrodesis group had five excellent and two good outcomes.
No wound infection, non-union, or overcorrection was observed at follow-up. One loss of correction occurred in the reconstruction group and was treated with a revision surgery of the MTP arthrodesis at the sixth week following the first surgery. Recurrence of the deformity was detected in 10 cases (all in only the soft tissue surgery group).
Discussion
The hallux valgus deformity, part of a complex foot malalignment pathology, is one of the major causes of disability in children with CP.3, 4, 13 The preferred treatment is first MTP arthrodesis; however, we observed that appropriate alignment of the MTP joint and satisfying functional results can be achieved with a combined method consisting of soft tissue release, exostectomy of the bunion, and a corrective metatarsal osteotomy when surgical treatment was required.1, 9, 14, 15 We also determined that isolated soft tissue surgery was ineffective in the treatment of hallux valgus in CP patients. Additionally, simultaneous correction of the associated midfoot or hindfoot deformity might be an important factor for maintaining the clinical and radiological correction after a hallux valgus surgery. However, it is the fact that literature lacks any consensus related to treatment of hallux valgus in CP patients. In accordance with our clinical experience and with results of this study, also supported by limited literature, we established an algorithm of hallux valgus treatment in CP patients.
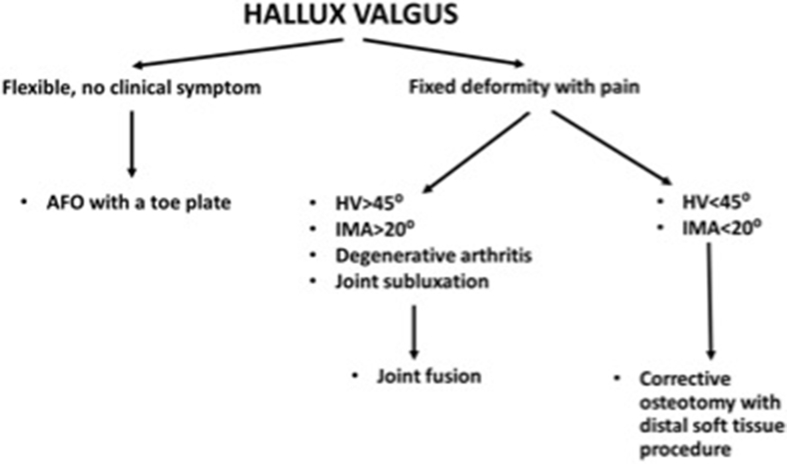
Age is one of decisive factors in pediatric treatment algorithms and it is reported that half of the final length of the foot is reached by 12–18 months of age. Then, the growth rate of the foot drops rapidly until 5 years of age.16, 17, 18 Therefore, we believe that our treatment algorithm can be used from age 5 in CP patients with hallux valgus deformity. Our treatment algorithm consists of three steps (Fig. 2). First, we prefer to treat deformities using an AFO with a toe plate when the deformities are supple and cause no pain in non-weight bearing children as Miler suggested.19 He reported that mild bunions are very supple, occur often in early and middle childhood, and are not fixed deformities when the children are non-weight bearing. Additionally, he preferred surgical correction for symptomatic bunions with less than 30° of HVA, or less than 20° of IMA. We similarly treat the symptomatic deformities surgically when resistant to non-operative treatment; e.g., pain over the forefoot and medial eminence and difficulty in using shoes or orthosis. Our experience indicates that if the IMA is less than 20° and the HVA is less than 45°, a distal corrective osteotomy, in addition to a soft tissue surgery, successfully corrects hallux valgus. We used to treat mild deformities only with soft tissue surgery, consisting of lateral release, plication of the medial capsule, and bunionectomy. However, we detected that the 12° correction obtained by the soft tissue surgery was deteriorated almost completely in follow-up. Because of this high recurrence rate, we no longer prefer soft tissue surgery alone for correction of hallux valgus deformities in CP patients, contrary to many other authors.8 Jenter et al8 reported that MTP joint fusion can be considered if the HVA is greater than 40° and the IMA is greater than 20°. Likewise, HVA greater than 45°, a MTP joint dislocation, or severe arthritis may lead us to perform an MTP joint fusion, combined with a distal soft tissue surgery (a proximal metatarsal osteotomy can be added to this procedure when the IMA is greater than 20°).
Fig. 2.
Treatment algorithm for hallux valgus in patients with cerebral palsy.
Sherif et al1 concluded that MTP arthrodesis is the appropriate treatment method for hallux valgus in children with CP because of high recurrence rates and the low correction capacity of soft-tissue releases and corrective osteotomies, which have a higher percentage of corrections needed at follow-up. However, Jenter's review concluded that the use of soft tissue release and a proximal osteotomy of the metatarsal or an osteotomy of the proximal phalanx of the great toe yielded results like those of an arthrodesis of the MTP joint.8 We also obtained satisfactory results with distal soft tissue surgery, exostectomy of the bunion, and metatarsal osteotomy. Our results are comparable to those reported by the series of authors who used first MTP arthrodesis in the treatment of a hallux valgus deformity in CP patients, where the average HVA was 31° preoperatively and 8° after the last follow-up.1, 8, 9 Likewise, the mean IMA was 9° at the last follow-up.
DuPont Bunion Rating Score, as modified by Jenter et al,8 assessed results of hallux valgus surgery with hallux valgus angle, intermetatarsal angle, range of motion, cosmetic and pain. Our study, using the DuPont Bunion Rating Score, found a significant improvement in functional outcomes for all subscores and the total score by distal soft tissue surgery, exostectomy of the bunion, and a metatarsal osteotomy. These outcomes are comparable with the outcome after the treatment of hallux valgus deformity by different surgical procedures in neurologically normal patient population.20, 21 Johnson reported successful results with first metatarsal double osteotomy in 90% of patients suffering from adolescent hallux valgus.22 Our combined method yielded excellent or good outcomes in 93% of the patients, based on their DuPont Bunion Rating scores.
Davids et al9 reported that spasticity and imbalance between the intrinsic muscles (e.g., abductor and adductor hallucis muscles, and extensor hallucis longus muscle) may contribute metatarsal varus malalignment. Additionally, midfoot and hindfoot pathologies, such as medial longitudinal arch collapse or planus foot, contribute to hallux valgus in CP.2, 5, 8, 10, 23 For instance, the hindfoot valgus applies pressure to the medial side of the hallux during weight bearing and pronation of the first ray, especially in the terminal stance of the gait cycle. Likewise, the increased peroneal muscle spasticity acts on the oblique head of the adductor hallucis muscle through the insertion of the peroneus longus tendon sheath, resulting in a lateral pull of the first proximal phalanx and hallux valgus. After correction of the 29 planovalgus foot deformities, all patients in our series showed excellent or good results, without recurrence of the hallux valgus deformity. We also believe that a treatment strategy consisting of reconstruction of the midfoot and hindfoot biomechanics, combined with soft tissue release and a corrective metatarsal osteotomy to treat a hallux valgus deformity in patients with CP, might help to maintain the corrected position after the hallux valgus surgery. Because it is reported that isolated soft tissue botulinum toxin injection, lengthening, or release to improve foot intrinsic muscle tightness and soft tissue balance leads to poor results when accompanying foot deformity is not corrected.9
Our findings conclude that when performed according to the algorithm we proposed, soft tissue release, exostectomy of the bunion, and a corrective metatarsal osteotomy achieved good clinical and radiological results for a hallux valgus deformity in most patients with CP. Also, the treatment of hallux valgus should be performed in conjunction with treatment of other segmental malalignments of the foot.
Acknowledgements
Conflict of Interest: The authors declare that they have no conflict of interest.
Funding: There is no funding source.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Bishay S.N., El-Sherbini M.H., Lotfy A.A., Abdel-Rahman H.M., Iskandar H.N., El-Sayed M.M. Great toe metatarsophalangeal arthrodesis for hallux valgus deformity in ambulatory adolescents with spastic cerebral palsy. J Child Orthop. 2009;3:47–52. doi: 10.1007/s11832-008-0147-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bleck E.E. Forefoot problems in cerebral palsy—diagnosis and management. Foot Ankle. 1984;4:188–194. doi: 10.1177/107110078400400405. [DOI] [PubMed] [Google Scholar]
- 3.Goldner J.L. Hallux valgus and hallux flexus associated with cerebral palsy: analysis and treatment. Clin Orthop Relat Res. 1981;157:98–104. [PubMed] [Google Scholar]
- 4.Davids J.R. The foot and ankle in cerebral palsy. Orthop Clin North Am. 2010;41:579–593. doi: 10.1016/j.ocl.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Green N.E. The orthopaedic management of the ankle, foot, and knee in patients with cerebral palsy. Instr Course Lect. 1987;36:253–265. [PubMed] [Google Scholar]
- 6.Renshaw T.S., Sirkin R.B., Drennan J.C. The management of hallux valgus in cerebral palsy. Dev Med Child Neural. 1979;21:202–208. [Google Scholar]
- 7.Richardson E.G. Disorders of the hallux. In: Crenshaw A.H., editor. Campbell's Operative Orthopaedics. Mosby Year Book; St. Louis: 1992. pp. 2615–2692. [Google Scholar]
- 8.Jenter M., Lipton G.E., Miller F. Operative treatment for hallux valgus in children with cerebral palsy. Foot Ankle Int. 1998;19:830–835. doi: 10.1177/107110079801901207. [DOI] [PubMed] [Google Scholar]
- 9.Davids J.R., Mason T.A., Danko A., Banks D., Blackhurst D. Surgical management of hallux valgus deformity in children with cerebral palsy. J Pediatr Orthop. 2001;21:89–94. doi: 10.1097/00004694-200101000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Fulford G.E. Surgical management of ankle and foot deformities in cerebral palsy. Clin Orthop Relat Res. 1990;253:55–61. [PubMed] [Google Scholar]
- 11.Lindgren U., Turan I. A new operation for hallux valgus. Clin Orthop Relat Res. 1983;175:179–183. [PubMed] [Google Scholar]
- 12.Silver D. Operative treatment of hallux valgus. J Bone Joint Surg. 1923;5:225–232. [Google Scholar]
- 13.Holstein A. Hallux valgus: an acquired deformity of the foot in cerebral palsy. Foot Ankle. 1980;1:33–38. doi: 10.1177/107110078000100112. [DOI] [PubMed] [Google Scholar]
- 14.Merkel K.D., Katoh Y., Johnson E.W., Jr., Chao E.Y. Mitchell osteotomy for hallux valgus: long-term follow-up and gait analysis. Foot Ankle. 1983;3:189–196. doi: 10.1177/107110078300300402. [DOI] [PubMed] [Google Scholar]
- 15.Vittas D., Jansen E.C., Larsen T.K. Gait analysis before and after osteotomy for hallux valgus. Foot Ankle. 1987;8:134–136. doi: 10.1177/107110078700800303. [DOI] [PubMed] [Google Scholar]
- 16.Morrison S.C., Durward B.R., Watt G.F., Donaldson M.D. Prediction of anthropometric foot characteristics in children. J Am Podiatr Med Assoc. 2009;99:497–502. doi: 10.7547/0990497. [DOI] [PubMed] [Google Scholar]
- 17.Bertsch C., Unger H., Winkelmann W., Rosenbaum D. Evaluation of early walking patterns from plantar pressure distribution measurements. First year results of 42 children. Gait Posture. 2004;19:235–242. doi: 10.1016/S0966-6362(03)00064-X. [DOI] [PubMed] [Google Scholar]
- 18.Ricco A.I., Richards B.S., Herring J.A. Disorders of the foot. In: Herring J.A., editor. Tachdjian's Pediatric Orthopedics. Vol. 761. WB Saunders; Philadelphia: 2014. [Google Scholar]
- 19.Miller F. Hallux valgus. In: Miller F., editor. Cerebral Palsy. Springer; New York, NY: 2005. pp. 779–784. [Google Scholar]
- 20.Petratos D.V., Anastasopoulos J.N., Plakogiannis C.V., Matsinos G.S. Correction of adolescent hallux valgus by proximal crescentic osteotomy of the first metatarsal. Acta Orthop Belg. 2008;74:496–502. [PubMed] [Google Scholar]
- 21.Andreacchio A., Origo C., Rocca G. Early results of the modified Simmonds–Menelaus procedure for adolescent hallux valgus. J Pediatr Orthop. 2002;22:375–379. [PubMed] [Google Scholar]
- 22.Johnson A.E., Georgopoulos G., Erickson M.A., Eilert R. Treatment of adolescent hallux valgus with the first metatarsal double osteotomy: the Denver experience. J Pediatr Orthop. 2004;24:358–362. doi: 10.1097/00004694-200407000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Weiner B.K., Weiner D.S., Mirkopulos N. Mitchell osteotomy for adolescent hallux valgus. J Pediatr Orthop. 1997;17:781–784. [PubMed] [Google Scholar]