Abstract
We report the treatment process of a pediatric patient with deformity and shortening in the arm after a recurrent aggressive aneurysmal bone cyst (ABC) in the proximal humerus. The patient was treated with curettage of the lesion and lengthening on an intramedullary nail following an osteotomy just distal to the ABC. The period of lengthening was approximately 50 days. At the end of the treatment the lengthening goal was achieved without any neurovascular complication. There was a minimal loss in shoulder hyperabduction due to the deformity of the humeral head.
Keywords: Humeral lengthening, Humerus, Aneurysmal bone cyst, Lengthening nail
Introduction
Aneurysmal bone cysts (ABCs) are rare benign expansile osteolytic bone tumors which occur throughout pediatric and adult bones. The most frequently affected locations are the metaphysis of the long bones.1 They account for 1% of all biopsied primary bone tumors.2 Histologically, they contain blood-filled spaces separated by the septae containing osteoid tissues and osteoclastic giant cells. ABCs most frequently affect people younger than 20 years old.3 Although benign, can be locally destructive to normal bone and may extend to soft tissue. Their expanding nature can erode cancellous and cortical bones, resulting in growth cessation by disrupting growth plates.4
There have been few clinical reports in literature about analyses of pediatric shoulder girdle ABCs. According to those studies, the clinical behavior of ABC in younger patients can sometimes be more aggressive than in older children.5 In the proximal humerus, it is important to determine whether or not the growth plate is affected. Angular deformity and/or shortening can occur due to growth plate destruction or tumor resection. Therefore, preservation of normal growth and shoulder function should be the aim of the treatment, but it may not always be possible. To achieve this, the curative resection of the tumor should be combined with a lengthening procedure for the restoration of the function of the upper extremity.
Surgical lengthening of the humerus has been performed less frequently than the lengthening of the femur and tibia, and there are fewer reports in literature of humeral lengthening compared with those of lengthening of the femur or tibia. There are noticeable limitations in function or cosmetic appearance if, and only if there is a moderate to large arm length discrepancy. Management options for severe arm length discrepancy vary and include no treatment, surgical lengthening, and epiphysiodesis of the contralateral normal proximal humeral epiphysis. When considering surgical lengthening, distraction osteogenesis arose from Ilizarov's experimental and clinical work in the 1950s. Gradual mechanical distraction can be used for humeral lengthening using either monolateral or circular external fixators.6, 7 As a recent innovation in limb lengthening, magnetic intramedullary nails are becoming a promising option of treatment.8
The case presented here is of a pediatric patient with a deformity and a shortening of the arm due to a recurrent aggressive ABC located in the proximal humerus, with the aim of reporting the healing response of ABC with lengthening intramedullary nail.
Case report
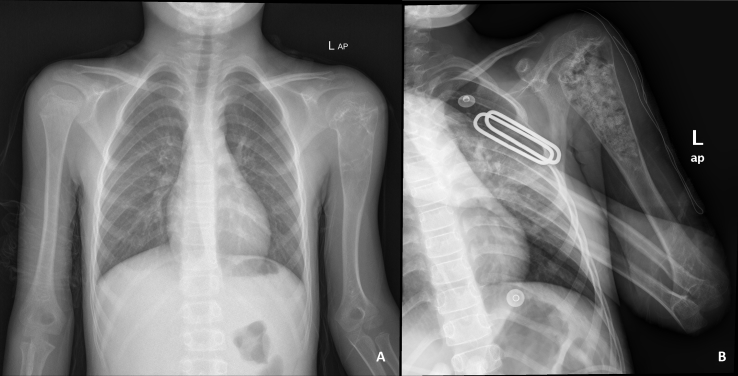
Five years ago a 9-year old boy was admitted to the outpatient clinic with complaints of pain, deformity and shortening of the left arm. Physical examination revealed an expansile tumor at the proximal part of the left arm and minimal (1.5 cm) shortening of the left upper extremity compared to the opposite side. An expansile, lobulated lytic lesion in the proximal metaphysis of the humerus was detected on radiographic evaluation (Fig. 1A). He had been initially treated by curettage and cancellous bone allograft in our center (Fig. 1B). The histopathological results of the tissue samples had been found to be consistent with the ABC. Serial follow-up radiographs showed recurrence of the ABC with concurrent progression of the deformity and limb-length discrepancy of the proximal humerus after 4 years of follow-up.
Fig. 1.
A. Radiography on admission B. After curettage and grafting.
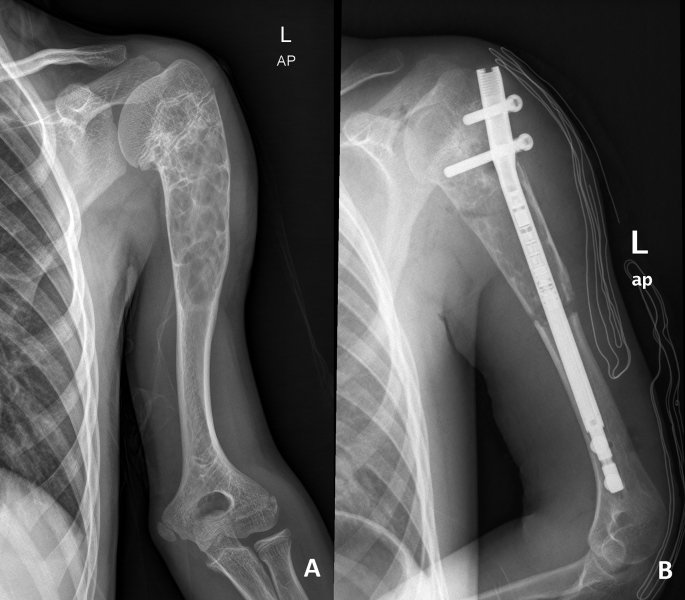
During examination at the age of 13, a short left arm secondary to an ABC recurrence on the proximal metaphysodiaphyseal of the humerus was noted (Fig. 2). He reported no pain but preferred to wear only long-sleeved shirts. Physical examination showed minimal limitation of movement, although clinically and radiologically, the left humerus was 5 cm shorter than the contralateral side. On radiographic evaluation, the growth plate was closed. The management option was surgical lengthening of the humerus by distraction osteogenesis via magnetic intramedullary nail.
Fig. 2.
A. Preop ABC recurrence B. Postoperative radiography.
A percutaneous osteotomy was applied in the diaphysial region of the humerus just distal to the ABC and curettage of the ABC zone (without grafting) just proximal to the osteotomy site. According to the preoperative planning, the insertion of the nail was prepared by conditioning the medullary canal with long, straight millers in 0.5 mm steps under careful radiological control in two planes. Then, an 8.5 mm × 195 mm magnetic antegrade tibial lengthening nail (PRECICE® Intramedullary Limb Lengthening System, Ellipse Technologies, USA) with a 5 cm lengthening capacity was implanted. Proximal locking was performed with a drill guide, and the distal locking with the free hand technique with a radiolucent gear drive using a mini open approach to protect the radial nerve. The nail function was tested radiologically with the c-arm, by lengthening 0.5 mm under sterile conditions immediately after implantation.
Distraction was initiated on post-operative day 5 with a 0.25-mm distraction rate every 6 h and was checked radiologically at least twice prior to the patient's discharge. After discharge, clinical examination and radiological control were performed weekly in an outpatient clinic. The planned weekly lengthening goal and the radiological lengthening were compared in order to control the lengthening process (Fig. 3). The distraction rate was adapted according to the radiological signs of consolidation of the bone regeneration, and the conditions of the joints and neuro-vascular structures.
Fig. 3.
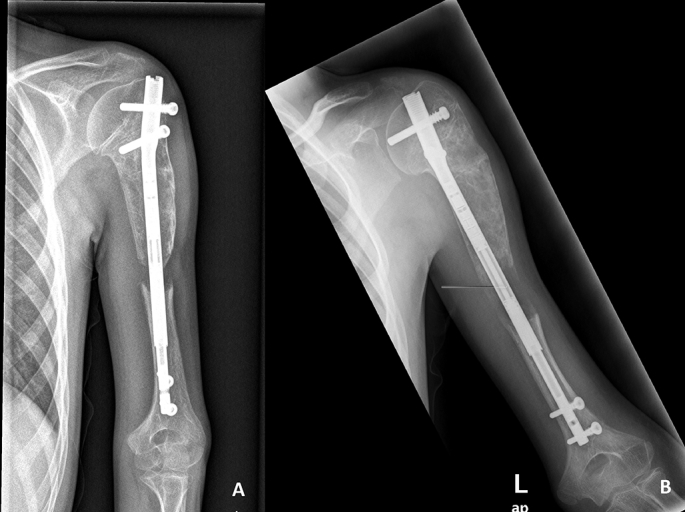
A. 4th week of distraction B. 7th week of distraction.
The period of lengthening was approximately 50 days. In the first 3 weeks of distraction, the patient used an arm sling and during this period of time, passive and active assisted exercises were allowed. After removing the sling, the patient was not allowed to lift heavy weights but was advised to undertake daily activities with a protective attitude. After the completion of the planned 5 cm lengthening, consolidation was monitored by radiographic follow-up every 4 weeks (Fig. 4). Four months after the operation, the weight limitation was abolished after all 4 cortices were seen on the radiographs. At the end of the total process, the targeted lengthening and the treatment of the aneurysmal bone cyst was accomplished.
Fig. 4.
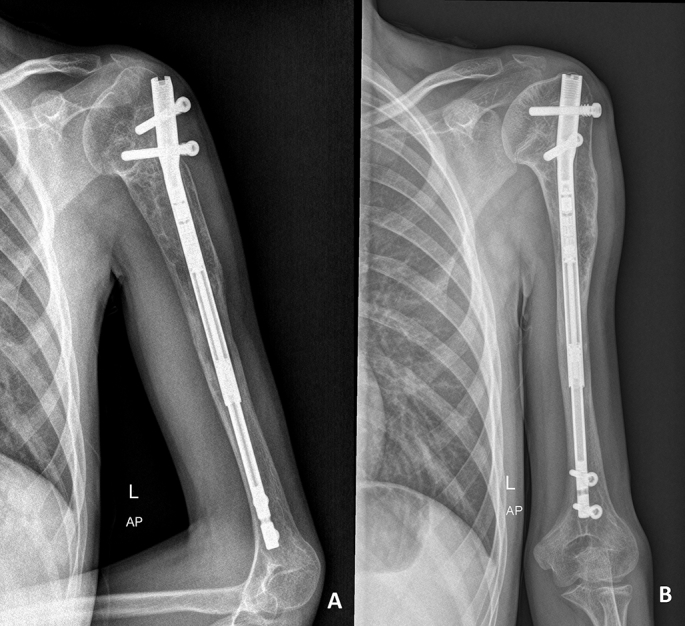
A. Postoperative 4th month; B. Postoperative 1st year.
After the lengthening, there were no neurovascular sequelae or loss in elbow range of motion, although there was a minimal loss in the shoulder hyperabduction due to the deformations on the humeral head (Fig. 5).
Fig. 5.
Range of motion.
Discussion
The treatment of ABC should be individualized depending on the location, aggressiveness and extent of the lesion. Although curettage and/or en bloc resection are the treatments of choice for accessible lesions, other treatment modalities including percutaneous intralesional injection, cryotherapy, radiation and embolization have been used for less accessible or recurrent lesions. Chemical cauterization with phenol is recommended for relatively large primary lesions to kill any surface tumor cells of the curetted cavity.3 Cryotherapy has also been proposed as an adjuvant therapy with surgical treatment to achieve local control.9 Radiation is used in inaccessible sites where no surgical options are available.3 Selective arterial embolization is recommended as a procedure for lesions where the location or size make other treatment modalities difficult or dangerous.4
If the proximal humerus is involved, it is important to determine whether or not the growth plate is affected, because 80% of the total humeral length is provided by the proximal humeral growth plate.10, 11 Proximal humerus physis closure takes place at the age of 14–16 years in boys and the humerus lengthens by about 1.2–1.3 cm a year after the age of 7 years.11 Preservation of normal growth and enabling maximum shoulder and arm function should be the aim of treatment, although this process can be problematic. The general approach to primary proximal humeral ABC is curettage alone. For lesions involving the growth plate, curettage rather than resection, can still be complicated by humeral shortening owing to epiphysiodesis.4, 12 Primary and recurrent surgery using curettage alone and curettage with bone grafting have been reported to avoid recurrence, but reports in literature have frequently omitted the documentation of full treatment details and outcomes. Similar small frequencies of recurrence at the proximal humerus have been identified after curettage alone and curettage with bone grafting.
In this case, at the age of 9 years and when the length discrepancy was 1.5 cm, the first choice of treatment was curettage and grafting. After 4 years of follow-up, there was ABC recurrence and 5 cm-length discrepancy. In the literature, 5–6 cm discrepancy is the limit value for lengthening.6, 13 The amount of limb discrepancy affected the self-esteem of the current patient in addition to the functional limitations, so this made the lengthening procedure necessary. To overcome the social problems and complications such as pin tract infection, pain, and movement restrictions, the intramedullary lengthening system was preferred instead of an external fixator.14, 15, 16, 17
Moreover, because the osteotomy made from distal margin of the ABC may not be sufficient for proximal curettage of the ABC, the reaming process might help the proximal curettage and the medullary bone fragments originating from the reaming process, serve as autologous graft.
In 1978 Dick and Tietjen reported the first humerus lengthening case followed by many monolateral and circular fixator-aided humerus lengthening cases.18 Occasional complications occur with the lengthening procedures, but most are temporary. Compared to the lower limb, fewer complications and faster functional recovery have been reported in lengthening of the humerus.19, 20 Flexion contracture of the elbow is one of the more common complications.21, 6 As the hardware is intramedullary, there is no soft tissue transfixation which could cause pin tract infection, joint stiffness and pain during lengthening.14, 15, 16, 22
A more serious complication is an injury to the radial nerve. The injury can be associated with an osteotomy, an insertion of the device, or an actual distraction process. When associated with the distraction, it is usually temporary and resolves between one week and six months. Permanent paralysis of the radial nerve has also been described in literature, produced by the manipulation of the osteotomy to correct varus angulation.23 It prevents the radial nerve from becoming stretched across the osteotomy site. If paresis occurs during the lengthening process, the rate of the lengthening should be decreased for several days until the paresis disappears, so that the normal lengthening point can be resumed. However, Kiss et al reported that they did not stop distraction even though the radial nerve palsy occurred and that the nerve also healed spontaneously.19 As there is no humeral lengthening with an intramedullary nail system previously reported in literature, it is hard to say that this system is superior to external fixator devices regarding the nerve injury. In the current case, a mini-open approach was preferred to protect the radial nerve while placing the distal locking screws of the nail.
In conclusion, in such cases of ABC with an accompanying deformity and limb length discrepancy, intramedullary lengthening might be a treatment option. The case reported above is the first in literature, which proposes an ABC treatment with lengthening and it is also the first to report lengthening of the humerus by distraction osteogenesis via magnetic intramedullary nail.
Conflicts of interest
The authors whose names are listed above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Ahmet Emrah Acan, Email: dremrahacan@hotmail.com.
Onur Basci, Email: dronurbasci@gmail.com.
Hasan Havitcioglu, Email: hasan.havitcioglu@deu.edu.tr.
References
- 1.Farsetti P., Tudisco C., Rosa M., Pentimalli G., Ippolito E. Aneurysmal bone cyst. Long-term follow-up of 20 cases. Arch Orthop Trauma Surg. 1990 June;109(4):221–223. doi: 10.1007/BF00453145. [DOI] [PubMed] [Google Scholar]
- 2.Mirra J.M. Aneurysmal bone cyst. In: Mirra J.M., Picci P., Gold R.H., editors. Bone Tumors. Clinical, Radiologic, and Pathologic Correlations. 2nd ed. Lea and Febiger; Philadelphia: 1989 June. pp. 1267–1311. [Google Scholar]
- 3.Campanacci M., Capanna R., Picci P. Unicameral and aneurysmal bone cysts. Clin Orthop Relat Res. 1986 March;204:25–36. [PubMed] [Google Scholar]
- 4.Cottalorda J., Kohler R., Sales de Gauzy J. Epidemiology of aneurysmal bone cyst in children: a multicenter study and literature review. J Pediatr Orthop B. 2004 Nov;13(6):389–394. doi: 10.1097/01202412-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Kaila R., Ropars M., Briggs T.W., Cannon S.R. Aneurysmal bone cyst of the pediatric shoulder girdle: a case series and literature review. J Pediatr Orthop Br. 2007 Nov;16(6):429–436. doi: 10.1097/BPB.0b013e3282f05a6e. [DOI] [PubMed] [Google Scholar]
- 6.Cattaneo R., Villa A., Catagni M.A. Lengthening of the humerus using the Ilizarov technique: description of the method and report of 43 cases. Clin Orthop. 1990 Jan;250:117–124. [PubMed] [Google Scholar]
- 7.Poul J., Svebis M. Results of lengthening 20 humeri. Acta Chir Orthop Traumatol Cech. 2001 Jan;68:289–293. [PubMed] [Google Scholar]
- 8.Thaller P.H., Fürmetz J., Wolf F., Eilers T., Mutschler W. Limb lengthening with fully implantable magnetically actuated mechanical nails (PHENIX(®)) preliminary results. Injury. 2014 Jan;45(Suppl. 1):S60–S65. doi: 10.1016/j.injury.2013.10.029. [DOI] [PubMed] [Google Scholar]
- 9.Schreuder H.W., Veth R.P., Pruszczynski M. Aneurysmal bone cysts treated by curettage, cryotherapy and bone grafting. J Bone Jt Surg Br. 1997 Jan;79(1):20–25. doi: 10.1302/0301-620x.79b1.7097. [DOI] [PubMed] [Google Scholar]
- 10.Dameron T.B., Jr., Reibel D.B. Fractures involving the proximal humeral epiphyseal plate. J Bone Jt Surg Am. 1969 Mar;51(2):289–297. [PubMed] [Google Scholar]
- 11.Pritchett J.W. Growth and predictions of growth in the upper extremity. J Bone Jt Surg Am. 1988 Apr;70(4):520–525. [PubMed] [Google Scholar]
- 12.Bollini G., Jouve J.L., Cottalorda J., Petit P., Panuel M., Jacquemier M. Aneurysmal bone cyst in children: analysis of twenty-seven patients. J Pediatr Orthop B. 1998 Oct;7(4):274–285. doi: 10.1097/01202412-199810000-00005. [DOI] [PubMed] [Google Scholar]
- 13.De Bastiani G., Aldegheri R., Renzi-Brivio L., Trivella G. Limb lengthening by callus distraction (callotasis) J Pediatr Orthop. 1987 Mar–Apr;7(2):129–134. doi: 10.1097/01241398-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Dahl M.T., Gulli B., Berg T. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res. 1994 Apr;301:10–18. [PubMed] [Google Scholar]
- 15.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990 Jan;250:81–104. Review. [PubMed] [Google Scholar]
- 16.Krieg A.H., Speth B.M., Foster B.K. Leg lengthening with a motorized nail in adolescents: an alternative to external fixators? Clin Orthop Relat Res. 2008 Jan;466(1):189–197. doi: 10.1007/s11999-007-0040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramaker R.R., Lagro S.W., van Roermund P.M., Sinnema G. The psychological and social functioning of 14 children and 12 adolescents after Ilizarov leg lengthening. Acta Orthop Scand. 2000 Feb;71(1):55–59. doi: 10.1080/00016470052943900. [DOI] [PubMed] [Google Scholar]
- 18.Dick H.M., Tietjen R. Humeral lengthening for septic neonatal growth arrest. Case report. J Bone Jt Surg Am. 1978 Dec;60(8):1138–1139. [PubMed] [Google Scholar]
- 19.Kiss S., Pap K., Vízkelety T., Terebessy T., Balla M., Szoke G. The humerus is the best place for bone lengthening. Int Orthop. 2008 Jun;32(3):385–388. doi: 10.1007/s00264-007-0327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanaka K., Nakamura K., Matsushita T., Horinaka S., Kusaba I., Kurokawa T. Callus formation in the humerus compared with the femur and tibia during limb lengthening. Arch Orthop Trauma Surg. 1998 Apr;117(4–5):262–264. doi: 10.1007/s004020050242. [DOI] [PubMed] [Google Scholar]
- 21.Schopler S.A., Lawrence J.F., Johnson M.K. Lengthening of the humerus for upper extremity limb length discrepancy. J Pediatr Orthop. 1986 Aug;6(4):477–480. doi: 10.1097/01241398-198607000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Herzenberg J.E., Scheufele L.L., Paley D., Bechtel R., Tepper S. Knee range of motion in isolated femoral lengthening. Clin Orthop Relat Res. 1994 Apr;301:49–54. [PubMed] [Google Scholar]
- 23.Dal Monte A., Andrisans A., Manfrini M. Humeral lengthening in hypoplasia of the upper limb. J Pediatr Orthop. 1985 March;5(2):202–207. [PubMed] [Google Scholar]