Abstract
Objective
The aim of this study was to analyze the risk factors contributing to the misdiagnosis of perilunate injuries.
Methods
The study included patients who had perilunate dislocation or fracture dislocation correctly or incorrectly diagnosed on initial examination between 2008 and 2014. Data related to the length of time until correct diagnosis of the perilunate injury; cause of injury; presence of associated fractures, polytrauma or concomitant trauma in the ipsilateral upper extremity; time between injury and first presentation; first treatment applied; presence of ligamentous perilunar injuries only or fracture and dislocation; inadequate radiographic assessment; and experience of the physicians were recorded and analyzed.
Results
A total of 44 wrists were included in the study. Of those, 10 (22.7%) wrists (mean patient age: 44.4 years [28 ± 58 years]) with perilunate injuries were misdiagnosed in the initial evaluation. All of the risk factors were found to be similar between the group of patients with correct initial diagnosis and missed diagnosis group, except for the experience of the orthopedic surgeon assessing the injury (p = 0.0001). Of the surgeons who missed the diagnosis, 70% reported that it was their first encounter with a perilunate injury.
Conclusion
The results of this study indicated that lack of experience was the most important factor in the misdiagnosis of perilunate fracture dislocation or isolated dislocation. Level of Evidence: Level IV, diagnostic study.
Keywords: Dislocation, Lunate, Perilunate, Wrist injury, Scaphoid fracture, Trans-scaphoid
Perilunate dislocation is an uncommon injury of the carpus most commonly seen in young males. This injury usually results from high-energy trauma, such as a motor vehicle accident, a fall from a height, or a sports-related injury that causes forceful wrist hyperextension, ulnar deviation, and intercarpal supination.1, 2, 3, 4 In addition, a less known and probably less common reverse perilunate instability resulting from hyperextension, ulnar deviation, and midcarpal pronation mechanism has also been described in the literature.5, 6
A patient with perilunate dislocation may be misdiagnosed by a medical professional, which will lead to delay in treatment. Early diagnosis is important due to the progression of carpal instability, and traumatic arthritis may result from delayed treatment. Recognition of perilunate injury patterns may be difficult for the untrained eye.1, 3 In the literature, it has been reported that the diagnosis was missed at the time of initial evaluation in 14.8%–25% of patients.2, 7 Variations in the pattern of perilunate injuries can occur with associated fractures of carpal bones, resulting in perilunate fracture dislocations. Areas of potential fracture include the distal radius, scaphoid, trapezium, capitate, hamate and triquetrum, all aligned along a larger arc encircling the lunate.8 Despite the usual involvement of high-energy trauma and the severity of the carpal injury, initial diagnosis of perilunate injuries may be delayed.2, 9 Inadequate radiographs or improper radiographic technique can also lead to misdiagnosis.10
Studies analyzing misdiagnosed perilunate dislocations are somewhat limited. The main reason for investigating medical errors is to try to prevent them. Therefore, this study was conducted to investigate characteristics of cases with misdiagnosed perilunate injuries and the risk factors for misdiagnosis.
Patients and methods
The current study consisted of a retrospective analysis of wrists with diagnosed and misdiagnosed perilunate dislocation or fracture dislocation (Mayfield stage 3/4) on initial examination at the clinic between 2008 and 2014. Approval for the study was granted by the Local ethics committee.
The study comprised 44 wrists (42 patients) with perilunate dislocation or fracture dislocation. A total of 10 (22.7%) wrists were misdiagnosed on initial examination by an orthopedic surgeon.
All patients who were misdiagnosed were treated with cast or splint immobilization in the orthopedic emergency department before obtaining correct diagnosis. After initial medical assessment and treatment, the patients presented to outpatient clinics for follow-up evaluation, where they were examined either by the same or another physician (Fig. 1, Fig. 2.). All of the patients with misdiagnosis received the correct diagnosis in follow-up clinic examination with new radiographs reviewed by another orthopedic surgeon in the department (Table 2). These patients were correctly diagnosed at mean of 31.7 ± 32.2 days after injury.
Fig. 1.
A 28-year-old male with left transradial volar lunate fracture dislocation. Initial diagnosis was radius styloid fracture and treatment was short arm cast immobilization.
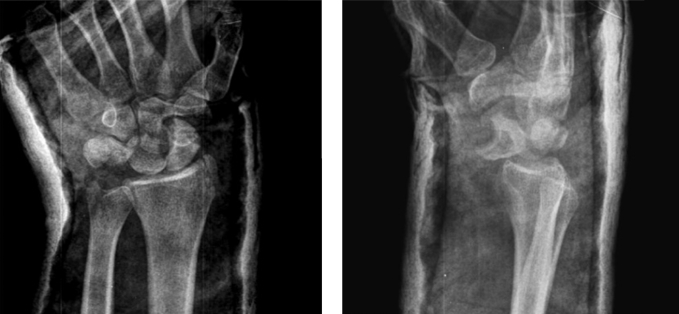
Fig. 2.
A 35-year-old male with right transscaphoid dorsal perilunate fracture dislocation. Initial diagnosis was scaphoid fracture and treatment was thumb spica cast immobilization.
Table 2.
Experience of the physicians who missed diagnosis of perilunate injury.
| Wrists | Orthopedic surgeons who evaluated the patients |
|||
|---|---|---|---|---|
| 1st physician | 2nd physician | 3rd physician | 4th physician | |
| Wrist 1 | Senior | Senior | In the 4th year of practice, CD | |
| Wrist 2 | In the 1st year of practice | In the 3rd year of practice | In the 3rd year of practice | Senior, CD |
| Wrist 3 | In the 2nd year of practice | In the 4th year of practice | In the 4th year of practice | Senior, CD |
| Wrist 4 | In the 1st year of practice | In the 3rd year of practice | In the 4th year of practice | Senior, CD |
| Wrist 5 | In the 2nd year of practice | In the 4th year of practice | Senior, CD | |
| Wrist 6 | In the 1st year of practice | Senior | In the 4th year of practice, CD | |
| Wrist 7 | Senior | Senior, CD | ||
| Wrist 8 | In the 1st year of practice | In the 3rd year of practice | Senior, CD | |
| Wrist 9 | Senior | In the 2nd year of practice | In the 4th year of practice, CD | |
| Wrist 10 | In the 1st year of practice | In the 4th year of practice, CD | ||
*There are 27 orthopedic surgeons represented in the table.
CD: Correct diagnosis.
Patient data were collected retrospectively from the electronic medical record system at Kartal Dr. Lütfi Kırdar Research and Education Hospital. Specific International Classification of Diseases 10th Revision codes were used for data collection: S63.03, subluxation and dislocation of midcarpal joint; S63.09, other subluxation and dislocation of the wrist and hand; S62.001A, unspecified fracture of navicular (scaphoid) bone of the right wrist, initial encounter for closed fracture; and S62.002A, unspecified fracture of navicular (scaphoid) bone of the left wrist, initial encounter for closed fracture.
An assessment form was prepared by the authors. The items documented were the length of time until diagnosis of the perilunate dislocation, cause of injury, associated fracture(s), presence of polytrauma or concomitant trauma in the ipsilateral upper extremity, time of first presentation, first treatment applied, presence of ligamentous perilunar injuries only or fracture dislocation, inadequate radiographic assessment, the experience of the physicians, and time between injury and hospital presentation.
The initial radiographs were reviewed by the authors for the purpose of this study. Associated fractures and injuries were noted. In cases where radiographs were inadequate or missing, the case was classified by the researchers as inadequate radiographic evaluation.
If the orthopedic surgeons had no previous encounter with a lunate injury in clinical practice, they were classified as inexperienced, whereas previous observation and diagnosis was classified as experienced.
The injuries were classified as stage I (the relationship of the lunate to the radius is normal), stage IIa (lunate is displaced to the palmar side with rotation of lunate of less than 90°) and stage IIb (rotation of the lunate of more than 90°) according to the Herzberg radiological classification.2
As a result of other medical conditions or contraindication for early surgical treatment, closed reduction and cast immobilization were applied to 4 wrists as definitive treatment. A total of 40 wrists (38 patients) were operated on under general or regional anesthesia with a tourniquet. Fractures and dislocations were reduced using open reduction. Volar or dorsal or combined volar and dorsal approaches were used as required. The dorsal approach was performed routinely unless there was an irreducible volar lunate dislocation. The treatment costs of the patients were covered by their health insurance.
Statistical analysis was performed using SPSS for Windows, Version 16.0 (SPSS Inc., Chicago, IL, USA) statistical software. The data obtained were analyzed using descriptive statistical methods at a 95% confidence interval and at 0.05 significance level to determine mean, percentage distribution, and standard deviation. The Fisher's exact test, Chi-square test, and Mann–Whitney U test were used to compare groups.
Results
Among the evaluations of 27 orthopedic surgeons, 10 wrists were initially misdiagnosed. The mean age of the patients was 35.5 ± 11.3 years (range: 20–60 years) in the correctly diagnosed group and 44.4 ± 10.4 years (range: 28–58 years) in the undiagnosed group. No statistically significant difference was determined with respect to age (p = 0.056). With the exception of patients with polytrauma, all other patients were treated immediately following the correct diagnosis. The time from trauma to surgery was 9.07 ± 9.4 days (range: 0–47 days) in the diagnosed group and 34.2 ± 36.2 days (range: 3–120 days) in the initially misdiagnosed group. The difference between the 2 groups was statistically significant (p = 0.023). The mean length of hospital stay was 14.9 ± 22.9 days (range: 2–86 days) in the diagnosed group and 5.9 ± 5.1 days (range: 3–20 days) in the undiagnosed group. Among the patients with correct immediate diagnosis, 18 right wrists and 16 left wrists were injured, and in the group correctly diagnosed with perilunate injury later, 1 right wrist and 9 left wrists were injured. None of the patients in the late diagnosis group had bilateral injury or concomitant trauma in the ipsilateral extremity. Two patients with bilateral injury were correctly diagnosed on admission by an experienced surgeon.
In a comparison of the cause of injury, associated fractures, polytrauma, injury type, radiographical assessment and Herzberg classification, there were no significant differences between groups. There was also no statistically significant difference in the time until hospital presentation (Table 1).
Table 1.
Clinical characteristics of the patients.
| Factors | Diagnosed wrists (n = 34) | Missed diagnosis wrists (n = 10) | p value | |
|---|---|---|---|---|
| Time until correct diagnosis (days) | Perilunate injury | 5.7 ± 2.3 | 31.7 ± 32.2 | 0.029** |
| Cause of injury | Fall from a height (wr*) | 9 (26.5) | 4 (40) | |
| Fall from a height | 12 (35.2) | 1 (10) | ||
| Fall | 4 (11.7) | 3 (30) | 0.760 | |
| Motor vehicle accident | 6 (17.6) | 2 (20) | ||
| Crushed or trapped between objects | 3 (8.8) | |||
| Associated fracture(s) | Scaphoid | 16 (47.1) | 2 (20) | 0.147 |
| Radius styloid | 14 (41.1) | 5 (50) | 0.720 | |
| Lunate | 1 (2.9) | – | 0.572 | |
| Triquetrum | 7 (20.5) | 2 (20) | 0.930 | |
| Ulna styloid | 6 (17.6) | 3 (30) | 0.449 | |
| Polytrauma | Head trauma, internal organ injury, or other fracture (pelvis, vertebra, etc.) | 7 (21.9) | 1 (10) | 0.445 |
| Concomitant trauma in ipsilateral extremity | Elbow dislocation | 1 (2.9) | ||
| Radial head dislocation | 1 (2.9) | – | No statistics computed | |
| Ulna and humerus shaft fracture | 1 (2.9) | |||
| 2nd metacarpal base fracture | 1 (2.9) | |||
| Initial treatment | Cast immobilization | 3 (8.8) | 7 (70) | No statistics computed |
| Brace | 1 (2.9) | 3 (30) | ||
| Surgical treatment | 30 (88.2) | – | ||
| Injury type | Pure ligamentous injury | 4 (11.7) | 3 (30) | 0.423 |
| Fracture dislocation | 30 (88.2) | 7 (70) | ||
| Radiographic assessment | Correct | 32 (94.1) | 8 (80) | 0.236 |
| Inadequate | 2 (5.8) | 2 (20) | ||
| Experience of the orthopedic surgeon | Experienced | 34 (100) | 4 (40) | 0.000*** |
| Inexperienced | – | 6 (60) | ||
| Time of presentation | Day shift (8:00 am–8:00 pm) | 24 (70) | 3 (30) | 0.062 |
| Night shift (8:00 pm–8:00 am) | 10 (29) | 7 (70) | ||
| Herzberg classification | I | 10 (29.4) | 3 (30) | |
| IIa | 14 (41.1) | 4 (40) | 0.993 | |
| IIb | 10 (29.4) | 3 (30) | ||
wr*: work-related. **p < 0.05, Mann–Whitney U test, ***p < 0.05, Fisher’s Exact test.
The number of missed diagnoses was significantly different when assessed according to the experience of the orthopedic surgeon (Table 1).
Missing an abnormality on the radiograph was the primary reason for 90% of incorrect diagnoses; in 70% of wrists, fracture was diagnosed but perilunate injury was missed (Table 2). In the group that was initially misdiagnosed, 70% of the orthopedic surgeons who performed the examination were inexperienced (Table 3).
Table 3.
Primary reason for missed diagnosis.
| Primary reason | Number of wrists | % |
|---|---|---|
| Abnormality missed on radiograph | 9 | 90 |
| Failure to radiograph | 2 | 20 |
| Associated fractures – fracture diagnosed and perilunate injury missed | 7 | 70 |
| Abnormality seen and commented on but misinterpreted | 3 | 30 |
Discussion
Perilunate dislocation and fracture dislocation are relatively uncommon injuries of the carpus, and early diagnosis of these injuries is important for successful surgical treatment and functional outcomes.11, 12, 13, 14, 15
The results of the current study demonstrated that 10 (22.7%) of 44 wrists in 42 patients were not correctly diagnosed in the initial assessment. This result was similar to Herzberg's.2 The length of time from trauma to surgery was longer, and 70% of the orthopedic surgeons were inexperienced in misdiagnosed group. Missing an abnormality on the radiograph was the primary reason for most cases of incorrect diagnosis.
Various factors, such as severe disruption of the carpal bones, lack of appreciation of the complex carpal anatomy, severity of the injury, priority of associated life-threatening injuries resulting from high-energy trauma, associated fractures of the wrist, concomitant upper-extremity injuries, lack of experience of the physician, and inadequate or improper radiographs can contribute to a misdiagnosis or late diagnosis of perilunate dislocation or fracture dislocation.2, 4, 10, 11, 16
In 1997, the National Patient Safety Foundation conducted a telephone survey and reported that 42% of the individuals surveyed had experienced a medical error, and of that group, 40% had been misdiagnosed or treated erroneously.17 Misdiagnosis is known to be a risk in clinical practice that may occur through a human error of medical staff. As a result of the intense working conditions of many hospitals, physicians may be over-stretched and young doctors with limited experience and knowledge may not be sufficiently supervised.18
Guly reported 953 diagnostic errors in 934 patients in an accident and emergency department over a period of 4 years. He noted that 79.7% were missed fractures, and that the most common reasons for error were misleading radiographs (77.8%) and failure to perform radiograph (13.4%), and that the majority of errors were made by junior doctors.19 Apergis suggested that the first viewing of the radiographic image of the injury is the most important factor in the delayed or missed diagnosis of perilunate injuries.7 In the current study, it was determined that 70% of the surgeons who missed the diagnosis were encountering perilunate dislocation for the first time; they were in the first 2 years of professional practice. Of the orthopedic surgeons who made the correct diagnosis in the misdiagnosed group, 4 reported that they had previously misdiagnosed a perilunate case and therefore examined wrist radiographs much more carefully, and particularly the Gilula arcs.
Even if the anamnesis and physical examination suggest perilunate injury, the cornerstone of diagnosis of perilunate dislocation and fracture dislocation is the radiographic evaluation.11 Standard wrist posteroanterior (PA) and lateral radiographs are typically sufficient for diagnosis in most injuries. The PA radiograph should be scrutinized for uneven gapping in the carpal bones, and the 3 smooth carpal arcs of Gilula should be free of discontinuity.13, 20 It must be remembered that dislocation of the midcarpal joint can be best evaluated with the lateral view, as there is a good visualization of lunocapitate dissociation.13, 21 Analysis of the current study radiographs indicated that most were taken in full PA and lateral view in both groups and that these were adequate for the correct diagnosis to be made at the initial examination.
Herzberg reported that the rates of missed diagnosis of perilunate dislocation and fracture-dislocation are similar.2 However, Garcia-Elias stated that dislocations are more likely to be missed than fracture-dislocations due to the absence of a clear pathology in ligamentous perilunar injuries.22 In the current study, the rate of injury type was similar in the correctly diagnosed and misdiagnosed groups.
Previous studies have pointed out that radial styloid fractures and carpal dislocations commonly occur together.16, 23 A more serious injury may be indicated when there are disruptions of Gilula's lines or a radial styloid fracture, particularly if the fracture line extends to the crest between the scaphoid and lunate fossa. In these cases, the treating surgeon should have a high index of suspicion.23 Apergis reported that in the absence of a scaphoid or radius styloid fracture, it is more probable that misalignment in the injured carpus will be overlooked.7 In the current study, the estimated rate of associated fractures of the wrist was similar in both groups. The small sample size of the misdiagnosed group may have led to this result, as orthopedic surgeons who missed the diagnosis of perilunate injury diagnosed an associated fracture. In another study, it was reported that the highest risk factor for a delayed foot fracture diagnosis was a fracture already diagnosed on the same foot.24 Based on our clinical observations, the authors suggest that diagnosis of a fracture in the wrist, especially the scaphoid and radius styloid, should make the physician more aware of possible further fractures.
All of the patients in the current series with perilunate dislocation or fracture-dislocation had sustained a high-energy trauma, and most were young, as in previous studies.12, 25 It has been reported in the literature that 26% of these patients had polytrauma,2 65% had internal organ injury,26 and 11% had an ipsilateral upper extremity injury.27 No significant differences were found between the rates of polytrauma and concomitant trauma in the ipsilateral extremity in the correctly diagnosed and misdiagnosed groups. In the current study, there were 7 patients with polytrauma in the group diagnosed with perilunate injury and 1 patient with polytrauma in misdiagnosed group. Patients with polytrauma had a long stay in the hospital, and mean length of hospital stay in correctly diagnosed group was longer than the misdiagnosed group.
In a comparison of the diagnostic results of junior doctors and senior doctors, it was reported that only 32% of junior doctors made the correct diagnosis of significant X-ray abnormalities occurring after trauma.28 Similarly, we found that all of the patients correctly diagnosed on initial evaluation were examined by senior doctors, and that 70% of the misdiagnosed patients were examined by inexperienced residents.
The time of presentation at the hospital can be considered another important issue in misdiagnosis. Working for long hours and job overload may negatively impact the performance of a physician. It has been reported that the greatest diagnosis error rate occurred between 12:00 pm and 3:59 pm.29
In our clinic, we change shift at 8:00 am and 6:00 pm in the emergency department. When we compared the hospital presentation time of the patients in this study, we determined that most of the patients (70%) in the misdiagnosed group were admitted to the hospital during the night shift, between 8:00 pm and 8:00 am. In the literature, it has been determined that if physicians slept for less than 8 h, it resulted in a drop in the performance of tasks that required concentration and the evidence also indicated that sleep deprivation causes doctors to treat patients with less care and sensitivity.30
Diagnostic errors are important in all branches of medicine. Guly pointed out that emergency departments need to provide for more patients to be seen by more experienced doctors and for better supervision of the more junior doctors. In addition, junior doctors in emergency or the department of orthopedic surgery should receive specific training on radiology and subspecialty areas to avoid misdiagnosis.19
It may be necessary to double-check uncertain X-ray identifications and ask for a second opinion or consultation with a physician who has specialized in this area to minimize diagnostic errors in complex cases. Comparison of X-rays of the injured wrist with those of the uninjured side may also help inexperienced specialists and residents avoid misdiagnosis.
It should not be forgotten that there are disease-specific factors in misdiagnosis of perilunate injuries in addition to physician-specific factors, including fatigue, lack of sleep, intense work conditions, and radiograph misinterpretation or inadequate radiographs.
The authors acknowledge that a limitation of the study was that there was no measurement of functional outcomes of late treatment, and therefore no comparison could be made with previous studies. A second limitation was the smaller sample size of the misdiagnosed group compared with the correctly diagnosed group.
Conclusion
The results of this study demonstrated that the most important factor in the misdiagnosis of perilunate fracture dislocation or isolated dislocation is the lack of experience. Therefore, it is strongly recommended that if there is a scaphoid and radial styloid fracture, the radiograph should be examined very carefully. There should be a routine assessment of the Gilula arcs on AP views and a lunate assessment on lateral views.
Conflicts of interest
No conflicts declared.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Siegert J.J., Frassica F.J., Amadio P.C. Treatment of chronic perilunate dislocations. J Hand Surg. 1988;13(2):206–212. doi: 10.1016/s0363-5023(88)80049-2. [DOI] [PubMed] [Google Scholar]
- 2.Herzberg G., Comtet J.J., Linscheid R.L., Amadio P.C., Cooney W.P., Stalder J. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am. 1993;18(5):768–779. doi: 10.1016/0363-5023(93)90041-Z. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Elias M. Carpal instability. In: Wolfe S.W., Hotchkiss R.N., Pederson W.C., Kozin S.H., editors. Green's Operative Hand Surgery. 6th ed. Churchill Livingstone; Philadelphia: 2010. pp. 465–522. [Google Scholar]
- 4.Mayfield J.K., Johnson R.P., Kilcoyne R.K. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5(3):226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 5.Reagan D.S., Linscheid R.L., Dobyns J.H. Lunotriquetral sprains. J Hand Surg Am. 1984;9(4):502–514. doi: 10.1016/s0363-5023(84)80101-x. [DOI] [PubMed] [Google Scholar]
- 6.Viegas S.F., Patterson R.M., Peterson P.D. Ulnar sided perilunate instability: an anatomic and biomechanic study. J Hand Surg Am. 1990;15(2):268–278. doi: 10.1016/0363-5023(90)90107-3. [DOI] [PubMed] [Google Scholar]
- 7.Apergis E. Acute perilunate dislocations and fracture dislocations. In: Apergis E., editor. Fracture Dislocations of the Wrist. Springer-Verlag; Italia: 2013. pp. 61–137. [Google Scholar]
- 8.Gaeber C., McQueen M.M. Carpus fractures and dislocations. In: Bucholz R.W., Heckman J.D., Court-Brown C.M., Tornetta P., editors. Rockwood and Green's Fractures in Adults. 7th ed. Lippincott, Williams and Wilkins; Philadelphia: 2010. pp. 781–828. [Google Scholar]
- 9.Johnson R.P. The acutely injured wrist and its residuals. Clin Orthop. 1980;149:33–44. [PubMed] [Google Scholar]
- 10.Kozin S.H., Berlet A.C. Injuries to the perilunar carpus. Orthop Rev. 1992;21(4):435–448. [PubMed] [Google Scholar]
- 11.Kozin S., Murphy M., Cooney W. Perilunate dislocations. In: Cooney W.P., Linscheid R.L., Dobyns J.H., editors. vol. 1. Mosby; St. Louis: 1998. pp. 632–650. (The Wrist: Diagnosis and Operative Treatment). [Google Scholar]
- 12.Bain G.I., Pallapati S., Eng K. Translunate perilunate injuries-a spectrum of this uncommon injury. J Wrist Surg. 2013;2(1):63–68. doi: 10.1055/s-0032-1333064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Redjal H.R., Rafijah G.H. Perilunate injuries of the wrist. In: Slutsky D.J., Osterman A.L., editors. Saunders Elsevier; Philadelphia: 2009. pp. 425–436. (Fractures and Injuries of the Distal Radius and Carpus: The Cutting Edge). [Google Scholar]
- 14.Massoud A.H., Naam N.H. Functional outcome of open reduction of chronic perilunate injuries. J Hand Surg Am. 2012;37(9):1852–1860. doi: 10.1016/j.jhsa.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 15.Herzberg G., Cooney W.P. Perilunate fracture dislocations. In: Cooney W.P., Linscheid R.L., Dobyns J.H., editors. vol. 1. Mayo Clinic; Mosby, St. Louis: 1998. pp. 651–683. (The Wrist: Diagnosis and Operative Treatment). [Google Scholar]
- 16.Mudgal C., Hastings H. Scapho-lunate diastasis in fractures of the distal radius. Pathomechanics and treatment options. J Hand Surg Br. 1993;18(6):725–729. doi: 10.1016/0266-7681(93)90231-4. [DOI] [PubMed] [Google Scholar]
- 17.National Patient Safety Foundation Public Opinion of Patient Safety Issues: Research Findings. 1997. https://c.ymcdn.com/sites/www.npsf.org/resource/collection/ABAB3CA8-4E0A-41C5-A480-6DE8B793536C/Public_Opinion_of_Patient_Safety_Issues.pdf [Google Scholar]
- 18.ASONS Solicitors. Misdiagnosis Claims. http://www.asons.co.uk/medical.negligence/misdiagnosis-claims Accessed 23 March 2016.
- 19.Guly H. Diagnostic errors in an accident and emergency department. Emerg Med J. 2001;18(4):263–269. doi: 10.1136/emj.18.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stanbury S.J., Elfar J.C. Perilunate dislocation and perilunate fracture-dislocation. J Am Acad Orthop Surg. 2011;19(9):554–562. doi: 10.5435/00124635-201109000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy P., Cohn B. Lunate and perilunate dislocations. In: Lewiss R., Saul T., Shah K., editors. Essential Emergency Imaging. Lippincott Williams & Wilkins; Philadelphia: 2012. pp. 750–779. [Google Scholar]
- 22.Garcia-Elias M. Perilunar injuries including fracture dislocations. In: Berger R., Weiss A.P., editors. vol. 1. Lippincott Williams Wilkins; Philadelphia: 2004. pp. 511–523. (Hand Surgery). [Google Scholar]
- 23.Reichel L.M., Bell B.R., Michnick S.M., Reitman C.A. Radial styloid fractures. J Hand Surg Am. 2012;37(8):1726–1741. doi: 10.1016/j.jhsa.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Ahrberg A.B., Leimcke B., Tiemann A.H., Josten C., Fakler J.K. Missed foot fractures in polytrauma patients: a retrospective cohort study. Patient Saf Surg. 2014;8(1):10. doi: 10.1186/1754-9493-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kucuk L., Ozalp T., Gunay H., Coskunol E., Ozdemir O. Treatment of acute and subacute dorsal perilunate fracture dislocations. Hand Microsurg. 2014;3(1):1–7. [Google Scholar]
- 26.Cooney W.P., Bussey R., Dobyns J.H., Linscheid R.L. Difficult wrist fractures: perilunate fracture-dislocations of the wrist. Clin Orthop Rel Res. 1987;214:136–147. [PubMed] [Google Scholar]
- 27.Herzberg G. Acute dorsal trans-scaphoid perilunate dislocations: open reduction and internal fixation. Tech Hand Up Extrem Surg. 2000;4(1):2–13. doi: 10.1097/00130911-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 28.McLauchlan C.A., Jones K., Guly H.R. Interpretation of trauma radiographs by junior doctors in accident and emergency department: a cause for concern? J Accid Emerg Med. 1997;14(1):295–298. doi: 10.1136/emj.14.5.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lesar T.S., Briceland L.L., Delcoure K., Parmalee J.C., Masta-Gornic V., Pohl H. Medication prescribing errors in a teaching hospital. JAMA. 1990;263(17):2329–2334. [PubMed] [Google Scholar]
- 30.McKee M., Black N. Does the current use of junior doctors in the United Kingdom affect the quality of medical care? Soc Sci Med. 1992;34(5):549–558. doi: 10.1016/0277-9536(92)90210-h. [DOI] [PubMed] [Google Scholar]