Abstract
Objectives
The aim of this study was to analyse the variability among Turkish spinal surgeons in the management of thoracolumbar fractures by carrying out a web survey.
Methods
An invitation text and web-link of the survey were sent to the members of the Turkish Spine Society mail group. A fictitious spine trauma vignette, a 23 year-old male with a L1 burst fracture, was presented and 25 questions were asked to participants. Variability of answers in a given question was assessed with the Index of Qualitative Variation (IQV). Questions with high IQV values (>%80) were selected to evaluate the relation between participant factors (speciality, age, degree and experience level of the surgeon, type of the work centre and volume of the trauma patients).
Results
Sixty-four (88%) among the 73 participating surgeons completed the survey. 45 (70%) of them were orthopaedic surgeons and 19 (30%) were neurosurgeons. 11 questions had very high variability (IQV ≥ 0.80), 5 had high variability (0.58–0.75) and 2 had low variability (IQV≤0.20). The question with the highest variability was related to the use of brace after surgery (IQV = 0.93). Following one was about the selection of fixation levels (IQV = 0.91). Neurosurgeons were more likely to use brace postoperatively and professors were less likely to perform decompression.
Conclusion
This survey shows that thoracolumbar spine trauma practice significantly varies among Turkish spine surgeons. Surgeons' characteristics affected some specific answers. Lack of enough knowledge about spine trauma care, fracture classifications and surgical techniques and/or ethical factors may be other reasons for this variability.
Keywords: Spine trauma, Surgical management, Classification, Variability
Introduction
Management of thoracolumbar fractures is one of the main issues in spine surgeons' practice. Although there are well accepted, treatment guiding classification systems, it is possible to observe quite different methods even in the treatment of similar type of fractures. Differences in experience levels, type of the work centre, volume of the trauma patients, perspective differences between disciplines (orthopaedics and neurosurgery) and/or lack of evidence based knowledge may be reasons for this variability.
Lonjon et al studied variability in spine trauma practices among French spine surgeons in 2013 and they defined the influencing factors.1 Little published evidence is available about this topic. Aim of this study is to analyse the variability among Turkish spinal surgeons in the management of thoracolumbar fractures by carrying out a web survey based on a fictitious spine trauma vignette. Measuring the quality of clinical practice by using clinical vignettes is a comprehensive and validated method.2, 3 We hypothesized that significant variability exists between Turkish spinal surgeons' practices in spine trauma care.
Material and methods
Study was designed as a cross sectional study. An invitation text and web-link of the survey were sent to the members of the Turkish Spine Society mail group, which has 350 members. In the first section of the survey, a fictitious spine trauma vignette was presented as, “A 23 year-old male with a L1 burst fracture was presented to the emergency department of your centre, following a traffic accident occurred at 30 min ago, around midnight. Patient was conscious and complaining about back pain. Physical examination revealed paraesthesia in both lower extremities with normal motor and sphincter functions. You can find the sagittal and axial computed tomography images of the patient below” (Fig. 1). Following the presentation of the vignette, 25 questions were asked to participants in 4 sections (treatment choices, infection, classification and personal information); and it was allowed to skip any question, except those in personal information section. Surveys with missing obligatory questions were accepted as incomplete. Clinical vignette and questions were selected mostly similar as in the French study with some additional questions and different images.1 The study team reached a consensus on these questions, which are adequate to discuss about many controversial topics in spine trauma care. These questions were listed in Table 1 and the full survey in Appendix A.
Fig. 1.
Sagittal and axial CT images of the 23 year-old male with a L1 burst fracture.
Table 1.
Questions of the survey.
| 1 | Would you obtain an emergent MRI scan? |
| 2 | Would you perform surgery on this patient? |
| 3 | If you decide that surgery is required, would you perform the procedure at night? |
| 4 | If you decide that surgery is required, would you initially use a posterior approach? |
| 5 | If you were to choose an initial posterior approach, would you perform surgical decompression? |
| 6 | If you were to choose an initial posterior approach, would you perform percutaneous fixation? |
| 7 | If you were to choose an initial posterior approach, would you seek to obtain fusion via bone grafting (with any type of bone material)? |
| 8 | If you were to choose an initial posterior approach, into which vertebrae would you implant the fixation material? |
| 9 | If you were to choose an initial posterior approach, would you perform a complementary anterior step? |
| 10 | If you were to perform surgery, would you prescribe post-operative bracing? |
| 11 | The patient is doing well 3 months after surgery. For how long after surgery would you provide follow-up? |
| 12 | After 12 months, the patient is doing very well (with no pain). Would you routinely remove the material? |
| 13 | In the event of an acute, deep (below the fascia) surgical-site infection, if you decide to perform revision surgery, would you change the material? |
| 14 | How many days of antibiotic therapy would you prescribe? (In case of the situation in Q13) |
| 15 | Do you use defined classification systems in the management of thoracolumbar fractures? |
| 16 | If you use classification systems, which of following would you prefer? |
| 17 | If you use classification systems, how it affects your treatment choice? |
| 18 | How do you classify the fracture of the clinical vignette according to AOSpine Thoracolumbar Fracture Classification system? |
| 19 | Speciality |
| 20 | Age |
| 21 | Sex |
| 22 | Type of the work centre |
| 23 | Degree |
| 24 | Experience in spinal surgery |
| 25 | How many patients with vertebral fractures do you manage each year? |
The survey was prepared on SurveyMonkey Inc (San Mateo, California, USA, www.surveymonkey.com) platform. Data collection protocol was selected, as Weblink and multiple responses were not allowed from the same device.
An invitation for participation to survey was sent with a brief explanation and with survey word in the subject line of email. The invitation process was repeated 2 more times in 7 days interval. This process was conducted in accordance with published guideline to improve the response rate.4
Statistical analysis
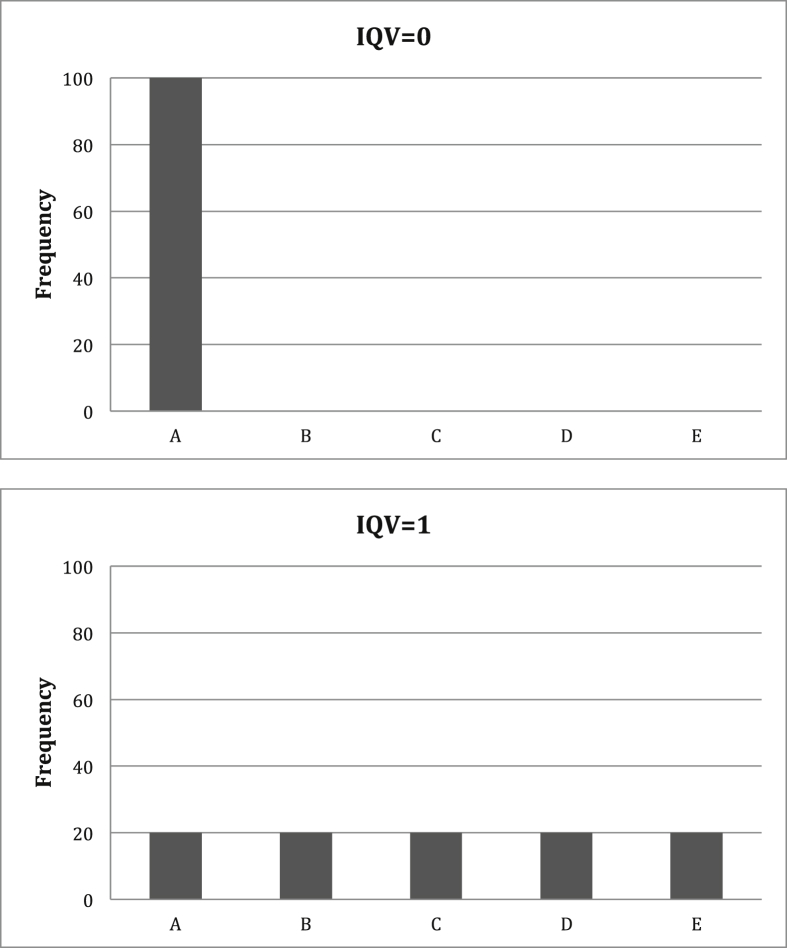
All valid data for each question were used for statistical analysis, even if the questionnaire was not answered fully. Variability of answers in a given question was assessed with the Index of Qualitative Variation (IQV). The IQV is based on the ratio of the total number of differences in the distribution to the maximum number of possible differences. The IQV can vary from 0.0 to 1.0. If all cases of the distribution fall within one category, without any diversity or variation, the IQV is 0.0. Conversely, the maximum value 1 occurs if, an identical number of cases fall within each category5 (Fig. 2).
Fig. 2.
The Index of Qualitative Variation (IQV) examples.
Questions with high IQV values (>%80) were selected to evaluate the relation between participant factors (speciality, age, degree and experience level of the surgeon, type of the work centre and volume of the trauma patients). Chi square test with Yates correction and Fisher's exact test were used to analyse nominal variables. The statistical significance was set as p <0.05. Statistical analyses were carried out using the NCSS 10 Statistical Software programme (2015. Kaysville, Utah, USA, ncss.com/software/ncss).
Results
64 (88%) among the 73 participating surgeons completed the survey. The rest answered some questions but not all of the obligatory personal information questions. All of the respondents were male (n = 64), with a mean age of 45 ± 7 years (range, 30–60). 45 (70%) of them were orthopaedic surgeons and 19 (30%) were neurosurgeons. Type of the work centres were distributed as, 44% university hospital, %28 training and research hospital, 28% private hospital, 9% private practice and 3% public hospital (7 respondents selected more than one centre). Respondents were 30% professor, 30% associate professor, 23% specialist, 14% assistant professor and 3% chief assistant. Experience in spinal surgery was more than 15 years for 41% of the respondents; respectively 23% between 5 and 10 years, 22% between 10 and 15 years and 14% less than 5 years. Lastly, number of vertebral fractures have been treated in a year was distributed as, between 10 and 15 for 39% of the respondents and respectively <10 for 33%, 25–50 for 22%, 50–100 for 3% and >100 for 3% (Table 2).
Table 2.
Characteristics of the respondents.
| n = 64 | Mean ± SD, range |
|---|---|
| Age, years | 45 ± 7 (30–60) |
| n(%) | |
| Sex | |
| Female | – |
| Male | 64 (100) |
| Speciality | |
| Orthopaedic surgeons | 45 (70) |
| Neurosurgeons | 19 (30) |
| Type of work centrea | |
| University hospital | 28 (44) |
| Training and Research hospital | 18 (28) |
| Public hospital | 2 (3) |
| Private hospital | 18 (28) |
| Private practice | 6 (9) |
| Degree | |
| Resident | – |
| Specialist | 15 (23) |
| Chief assistant | 2 (3) |
| Assistant professor | 9 (14) |
| Associated professor | 19 (30) |
| Professor | 19 (30) |
| Experience in spinal surgery | |
| <5 years | 9 (14) |
| 5–10 years | 15 (23) |
| 10–15 years | 14 (22) |
| >15 years | 26 (41) |
| Number of vertebral fractures/year | |
| <10 | 21 (33) |
| 10–25 | 25 (39) |
| 25–50 | 11 (22) |
| 50–100 | 2 (3) |
| >100 | 2 (3) |
7 respondents selected more than one centre.
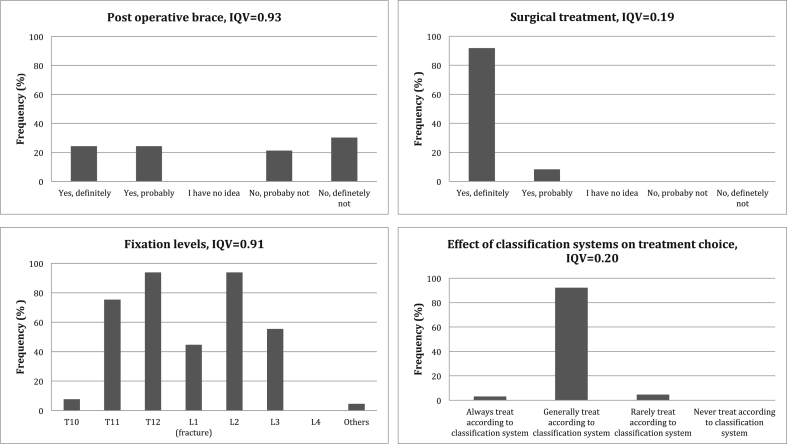
11 questions had very high variability (IQV ≥ 0.80), 5 had high variability (0.58–0.75) and 2 had low variability (IQV ≤ 0.20) (Table 3). The question with the highest variability was related to the use of brace after surgery (IQV = 0.93). Following one was about the selection of fixation levels (IQV = 0.91) Two questions with the lowest IQV values were about preference for a surgical treatment (IQV = 0.19) and effect of classification systems on treatment choice (IQV = 0.20) (Fig. 3).
Table 3.
IQV values of questions.
| Q | IQV | Q | IQV |
|---|---|---|---|
| 1 | 0.82 | 10 | 0.93 |
| 2 | 0.19 | 11 | 0.88 |
| 3 | 0.88 | 12 | 0.72 |
| 4 | 0.58 | 13 | 0.80 |
| 5 | 0.84 | 14 | 0.81 |
| 6 | 0.71 | 15 | 0.75 |
| 7 | 0.71 | 16 | 0.86 |
| 8 | 0.91 | 17 | 0.20 |
| 9 | 0.80 | 18 | 0.86 |
Fig. 3.
Questions with the highest and lowest IQV values.
64% of the respondents answered as they would definitely or probably obtain an emergent MRI examination while 36% would not. 67% preferred to perform an emergent surgery at night and 73% preferred to perform posterior decompression, while 27% not. 59% preferred long segment posterior fixation, 23% fixation between two levels above and one level below the fractured vertebra. 46% preferred pedicle screw fixation to the fractured level. 48% answered, as they would use brace following the surgery. 63% preferred ≥2 years follow up duration. Most frequently preferred classification system was TLICS (67%) and the others were AOSpine classification system (38%), Denis classification (31%), McCormack Load sharing system (9%) and others (4%) respectively. Most of the respondents (38%) answered, as hey have no idea about AOSpine classification of our case, 20% classified as B2, 16% A3, 13% A4, 8% C, 3% B3, 2% B1. Distributions of answers for each corresponding question were given in Appendix B.
Relation between surgeons' characteristics and answers was significant in two questions. 1) 72% of the neurosurgeons (n = 13) preferred to use post-operative brace while 64% of the orthopaedic surgeons (n = 28) did not (p = 0.02). 2) 64% of the professors (full and associate) (n = 23) preferred to perform posterior decompression which was significantly lower than the others' (specialists, assistant professors and chief assistants) preference, 91% of them (n = 20) answered as, they would perform posterior decompression (p = 0.26). There was not any statistically significant relation between participants' studied characteristics and answers in other questions.
Discussion
Our survey showed significant variability exists between Turkish spinal surgeons' practices in spine trauma care. 11 questions among 18 had very high variability, 5 had high variability and only two questions had low variability. Few answers influenced by surgeons' speciality and degree. Some of the questions with very high IQV values and related literature will be discussed briefly in 6 topics to be able to interpret our findings.
Need for MRI examination and fracture classification
MRI is a useful tool for visualizing the neural elements, integrity of posterior ligamentous complex (PLC) and status of the intervertebral discs. It is also valuable to evaluate the entire spinal column to identify distant fractures or space occupying lesions.6 Although CT is currently the standard imaging modality for the initial evaluation of spinal fractures, need for MRI examination is increasing due to recognition of soft tissues' function in stability especially the PLC. It has an important role in recent classifications and in decision-making.
Avulsion fracture of the interspinous process, interspinous spacing, diastasis of the facet joints, local kyphosis > 20°, loss of vertebral body height >50% are some parameters have been studied on to estimate the integrity of PLC. But there were no universally accepted radiological criteria to demonstrate PLC injury on X-rays and CT.7 Petersilge et al reported that, there were no radiological parameters correlating with supraspinous ligament injury in burst fractures.8 Radcliff et al reported that, loss of vertebral body height >50% and local kyphosis >20° are not predictive of PLC injury in thoracolumbar burst fractures. Translation greater than 3.5 mm was associated with PLC injury.9
In a prospective study including 30 patients, Pizones et al showed that addition of MRI to X-rays and CT had modified their diagnosis in %40 of patients, classification fracture pattern (AO type) in 24% of fractures and therapeutic management in 16% of patients.10 In a retrospective study, including 100 patients, it was shown that with addition of MRI to CT, 21% new fractures were detected and AO classification changed in 31%, TLICS classification changed 33% of the patients.11 Salgado et al reported that, MRI improves reliability in evaluation of fractures with AO classification according to CT alone. On the other hand, Rajasekaran et al stated that for accurate classification of fractures CT is mandatory; MRI only provided moderate gain in sensitivity for B2 type fractures according to AOSpine classification.12
Our clinical vignette had L1 burst fracture, with superior and inferior end plate involvement and moderate to severe canal compromise. CT scans did not exhibit any facet joint dislocation. Patient had incomplete sensory deficit in both limbs. According to TLICS system, patient's score is greater than 4, which is suggesting a surgical treatment.13 It is not easy to exactly define the AOSpine type of the fracture, depending just on the CT images, without knowledge of the PLC status. It may be A4 or B2.14 All our respondents preferred surgical management for this case and 64% of them needed an emergent MRI scan. 67% of the respondents were using TLICS classification and 37% AOSpine classification solely or in combination with other classifications. According to both classifications surgery is the recommended treatment for our case.13, 15 MRI seems not to be necessary in deciding need for surgical management. But assessment of the status of PCL and neural tissue may be helpful in determining prognosis and may affect the type of the surgical procedure.13
The IQV was high for the question asking AOSpine type of the fracture. The most frequent answer was I have no idea (38%). One of the reasons may be because most of the respondents were using TLICS classification and another one may be the absence of an MR image. AOSpine classification was the most recent introduced classification accounts simply for the various patterns of spinal fracture and soft-tissue injury, the extent of neurological deficit and the presence or absence of key medical comorbidities. Mostly based on features identifiable using CT scans. One of the important criticisms about TLICS system that it does not accurately represent treatment algorithms commonly used in many parts of the world; and this was one of the motivation behind development of AOSpine classification.14, 15 The AOSpine classification system has been shown to have a good intra-observer reliability and the level of surgeons' experience did not influence the classification and reliability.16 In our case, second frequent answer was type B2 (20%) and respectively A3 (16%) and A4 (13%).
Urgent surgery
The knowledge about optimal surgical timing in spinal fractures mostly comes from retrospective studies and databases. Briefly, early surgical stabilization of spinal fractures (within 72 h of injury) has been shown to decrease the length of hospital stay, respiratory complications and mortality.17 In case of an accompanying spinal cord injury, surgical decompression within 24 h improves the neurological outcomes for incomplete injuries.18, 19 Our clinical vignette had presented with pure sensory deficit in both lower extremities with normal motor functions. Surgeons may have different opinions about the severity of this neurologic condition. According to TLICS classification, incomplete sensory or motor spinal cord injuries were assigned 3 points and classified as the most urgent conditions.13 Best strategy seems to perform an urgent surgery within 24 h. Rapid organization of the surgical team and earlier access to operating theatre, even surgery at night may be preferable.20
Decompression
Degree of canal compromise may be quite variable with burst fractures. There is not a specific rule for surgical intervention without neurological involvement. It has been demonstrated that retropulsed bony fragments were resorbed and canal modelled up to %50 over time in patients without any neurological involvement.6, 21 In presence of a neurological deficit, as previously mentioned, urgent surgical decompression improves the neurological outcomes. Vaccaro et al recommended an anterior approach if an incomplete neurology was present due to compression from anterior spinal elements and combined approach with additional PLC disruption.13 Posterior decompression techniques have also been shown to be effective in many studies. Indirect decompression by ligamentotaxis or direct decompression by laminectomy or transpedicular way may be the choices for decompression with or without corpectomies and reconstructions.22, 23 In our case, 73% of the respondents preferred to perform posterior decompression, while 27% not.
Selection of fixation levels
Various surgical techniques have been described for surgical stabilization of thoracolumbar fractures. Vertebral column reconstruction and instrumentation through an anterior approach, posterior short or long segment pedicle screw fixations or combined methods may be the choices. Posterior techniques are frequently preferred to avoid potential complications of anterior surgery in majority of the cases. Also it is possible to obtain a better sagittal alignment with posterior techniques. Short segment posterior instrumentation, fixation between one level above and below the fractured vertebra, has motion segment sparing advantage. Clinical outcomes were mostly satisfying and comparable with long segment fixations for burst fractures.24, 25 McCormack et al recommended short segment fixation in mild burst fractures with load sharing score ≤6, long segment fixation in fractures with severe comminution and score >7.26 Additional screws to fractured vertebra have been shown to increase the stability of short segment fixations in cadaveric models and improved the results in clinical studies.27, 28, 29 59% of respondents preferred long segment posterior fixation in the treatment of our clinical vignette. 23% preferred fixation between two levels above and one level below the fractured vertebra. 46% preferred pedicle screw fixation to the fractured level. Authors' believes that short segment fixation with intermediate screws to the fractured level provides sufficient stability for this case.
Post-operative bracing
There is not enough evidence behind post-operative bracing. In a systematic review evaluating brace usage after surgical stabilization of thoracolumbar fractures, it was reported that there were no significant differences between pain, screw breakage, infection, or return to work with post-operative bracing. Overall complication rates and loss of kyphotic correction were significantly higher with brace group while pseudoarthrosis rate was higher in non-brace group.30 Given the fact that post-operative bracing is costly and has potential complications, better evidence is needed defining the indications of post-operative bracing in thoracolumbar fractures.
Follow-up duration
We could not find any studies about the optimum follow-up duration after thoracolumbar fracture surgery. Most of the clinical studies in the literature evaluate ≥2 years follow-up data. While 37% of the respondents preferred ≤1 year follow-up for our clinical vignette, 63% preferred ≥2 years follow up. We also prefer at least 2 years follow-up duration after thoracolumbar trauma surgery.
Two answers were influenced by surgeons' speciality and degree. Neurosurgeons were more likely to use brace postoperatively and professors (full and associate) were less likely to perform decompression according to others. Other studied surgeon factors seemed did not have significant effect on the answers. Lack of enough knowledge about spine trauma care, fracture classifications and surgical techniques and/or ethical factors were considered as possible reasons for observed significant variability in this study.
Our findings were comparable with the similar French study. In a similar survey, they also found great variability between French spinal surgeons practice in the management of a trauma case. They found very high variability in questions about need for emergent MRI (IQV = 0.93), emergency surgery (IQV = 0.93), need for fusion (IQV = 0.92), post-operative brace (IQV = 0.91) and routine instrument removal in asymptomatic patient (IQV = 0.94). They also reported that neurosurgeons were more likely to request an MRI, younger surgeons operate at night and orthopaedic surgeons to consider post-operative bracing unnecessary.1
Limitation of this study may be the number of the respondents. Our target population was the members of the Turkish Spine Society mail group (n = 350). Actually, with %5 Type 1 error and 5% confidence interval the sample size was calculated to be 183, 76 with 10% confidence interval, 65 with 11% confidence interval. It was 73 in our study.
Conclusion
This survey shows that thoracolumbar spine trauma practice significantly varies among Turkish spine surgeons. Surgeons' characteristics affected some specific answers. Lack of enough knowledge about spine trauma care, fracture classifications and surgical techniques and/or ethical factors may be other reasons for this variability.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.aott.2017.11.013.
Contributor Information
Engin Çetin, Email: enginctn@yahoo.com.tr.
Alpaslan Şenköylü, Email: drsenkoylu@gmail.com.
Emre Acaroğlu, Email: acaroglue@gmail.com.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Lonjon G., Grelat M., Dhenin A. Survey of French spine surgeons reveals significant variability in spine trauma practices in 2013. Orthop Traumatol Surg Res. 2015 Feb;101(1):5–10. doi: 10.1016/j.otsr.2014.10.018. Epub 2015 Jan 9. [DOI] [PubMed] [Google Scholar]
- 2.Peabody J.W., Luck J., Glassman P., Dresselhaus T.R., Lee M. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000 Apr 5;283(13):1715–1722. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- 3.Peabody J.W., Luck J., Glassman P. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med. 2004 Nov 16;141(10):771–780. doi: 10.7326/0003-4819-141-10-200411160-00008. [DOI] [PubMed] [Google Scholar]
- 4.Edwards P.J., Roberts I., Clarke M.J. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009 Jul 8;3 doi: 10.1002/14651858.MR000008.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilcox A.R. OakRidgeNationalLab; Tenn: 1967. Indices of qualitative variation. [Google Scholar]
- 6.Wood K.B., Li W., Lebl D.S., Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014 Jan;14(1):145–164. doi: 10.1016/j.spinee.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 7.Pizones J., Sánchez-Mariscal F., Zúñiga L., Álvarez P., Izquierdo E. Prospective analysis of magnetic resonance imaging accuracy in diagnosing traumatic injuries of the posterior ligamentous complex of the thoracolumbar spine. Spine (Phila Pa 1976) 2013 Apr 20;38(9):745–751. doi: 10.1097/BRS.0b013e31827934e4. [DOI] [PubMed] [Google Scholar]
- 8.Petersilge C.A., Pathria M.N., Emery S.E., Masaryk T.J. Thoracolumbar burst fractures: evaluation with MR imaging. Radiology. 1995 Jan;194(1):49–54. doi: 10.1148/radiology.194.1.7997581. [DOI] [PubMed] [Google Scholar]
- 9.Radcliff K., Su B.W., Kepler C.K. Correlation of posterior ligamentous complex injury and neurological injury to loss of vertebral body height, kyphosis, and canal compromise. Spine (Phila Pa 1976) 2012 Jun 1;37(13):1142–1150. doi: 10.1097/BRS.0b013e318240fcd3. [DOI] [PubMed] [Google Scholar]
- 10.Pizones J., Izquierdo E., Álvarez P. Impact of magnetic resonance imaging on decision making for thoracolumbar traumatic fracture diagnosis and treatment. Eur Spine J. 2011 Aug;20(Suppl. 3):390–396. doi: 10.1007/s00586-011-1913-4. Epub 2011 Jul 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winklhofer S., Thekkumthala-Sommer M., Schmidt D. Magnetic resonance imaging frequently changes classification of acute traumatic thoracolumbar spine injuries. Skeletal Radiol. 2013 Jun;42(6):779–786. doi: 10.1007/s00256-012-1551-x. Epub 2012 Dec 27. [DOI] [PubMed] [Google Scholar]
- 12.Rajasekaran S., Vaccaro A.R., Kanna R.M. The value of CT and MRI in the classification and surgical decision-making among spine surgeons in thoracolumbar spinal injuries. Eur Spine J. 2017 May;26(5):1463–1469. doi: 10.1007/s00586-016-4623-0. Epub 2016 Jun 1. [DOI] [PubMed] [Google Scholar]
- 13.Vaccaro A.R., Lehman R.A., Hurlbert R.J. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 2005 Oct 15;30(20):2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 14.Vaccaro A.R., Oner C., Kepler C.K. AOSpine thoracolumbar spine injury classification system. Spine (Phila Pa 1976) 2013 Nov 1;38(23):2028–2037. doi: 10.1097/BRS.0b013e3182a8a381. [DOI] [PubMed] [Google Scholar]
- 15.Kepler C.K., Vaccaro A.R., Schroeder G.D. The thoracolumbar AOSpine injury score. Global Spine J. 2016 Jun;6(4):329–334. doi: 10.1055/s-0035-1563610. Epub 2015 Sep 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sadiqi S., Oner F.C., Dvorak M.F., Aarabi B., Schroeder G.D., Vaccaro A.R. The influence of spine surgeons' experience on the classification and intraobserver reliability of the novel AOSpine thoracolumbar spine injury classification system-an international study. Spine (Phila Pa 1976) 2015 Dec;40(23):E1250–E1256. doi: 10.1097/BRS.0000000000001042. [DOI] [PubMed] [Google Scholar]
- 17.O'Boynick C.P., Kurd M.F., Darden B.V., Vaccaro A.R., Fehlings M.G. Timing of surgery in thoracolumbar trauma: is early intervention safe? Neurosurg Focus. 2014;37(1):E7. doi: 10.3171/2014.5.FOCUS1473. [DOI] [PubMed] [Google Scholar]
- 18.Fehlings M.G., Rabin D., Sears W., Cadotte D.W., Aarabi B. Current practice in the timing of surgical intervention in spinal cord injury. Spine (Phila Pa 1976) 2010 Oct 1;35(21 Suppl):S166–S173. doi: 10.1097/BRS.0b013e3181f386f6. [DOI] [PubMed] [Google Scholar]
- 19.Dvorak M.F., Noonan V.K., Fallah N. The influence of time from injury to surgery on motor recovery and length of hospital stay in acute traumatic spinal cord injury: an observational Canadian cohort study. J Neurotrauma. 2015 May 1;32(9):645–654. doi: 10.1089/neu.2014.3632. Epub 2014 Nov 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agostinello J., Battistuzzo C.R., Skeers P., Bernard S., Batchelor P.E. Early spinal surgery following thoracolumbar spinal cord injury: process of care from trauma to theater. Spine (Phila Pa 1976) 2017 May 15;42(10):E617–E623. doi: 10.1097/BRS.0000000000001903. [DOI] [PubMed] [Google Scholar]
- 21.Wood K., Buttermann G., Mehbod A., Garvey T., Jhanjee R., Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003 May;85(A(5)):773–781. doi: 10.2106/00004623-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Lin B., Chen Z., Guo Z., Liu H., Yi Z. Anterior approach versus posterior approach with subtotal corpectomy, decompression, and reconstruction of spine in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech. 2011 Jun 1 doi: 10.1097/BSD.0b013e3182204c53. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Ge C.-M., Wang Y.-R., Jiang S.-D., Jiang L.-S. Thoracolumbar burst fractures with a neurological deficit treated with posterior decompression and interlaminar fusion. Eur Spine J. 2011 Dec;20(12):2195–2201. doi: 10.1007/s00586-011-1875-6. Epub 2011 Jun 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tezeren G., Kuru I. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005 Dec;18(6):485–488. doi: 10.1097/01.bsd.0000149874.61397.38. [DOI] [PubMed] [Google Scholar]
- 25.Aly T.A. Short segment versus long segment pedicle screws fixation in management of thoracolumbar burst fractures: meta-analysis. Asian Spine J. 2017 Feb;11(1):150–160. doi: 10.4184/asj.2017.11.1.150. Epub 2017 Feb 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCormack T., Karaikovic E., Gaines R.W. The load sharing classification of spine fractures. Spine (Phila Pa 1976) 1994 Aug 1;19(15):1741–1744. doi: 10.1097/00007632-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Kanna R.M., Shetty A.P., Rajasekaran S. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J. 2015 Feb 1;15(2):256–264. doi: 10.1016/j.spinee.2014.09.004. Epub 2014 Sep 22. [DOI] [PubMed] [Google Scholar]
- 28.Pellisé F., Barastegui D., Hernandez-Fernandez A. Viability and long-term survival of short-segment posterior fixation in thoracolumbar burst fractures. Spine J. 2015 Aug 1;15(8):1796–1803. doi: 10.1016/j.spinee.2014.03.012. Epub 2014 Mar 15. [DOI] [PubMed] [Google Scholar]
- 29.Norton R.P., Milne E.L., Kaimrajh D.N., Eismont F.J., Latta L.L., Williams S.K. Biomechanical analysis of four- versus six-screw constructs for short-segment pedicle screw and rod instrumentation of unstable thoracolumbar fractures. Spine J. 2014 Aug 1;14(8):1734–1739. doi: 10.1016/j.spinee.2014.01.035. Epub 2014 Jan 23. [DOI] [PubMed] [Google Scholar]
- 30.Skoch J., Zoccali C., Zaninovich O. Bracing after surgical stabilization of thoracolumbar fractures: a systematic review of evidence, indications, and practices. World Neurosurg. 2016 Sep;93:221–228. doi: 10.1016/j.wneu.2016.05.067. Epub 2016 Jun 1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.