Abstract
Introduction
The aim of this systematic review was to analyze the results of published treatment options in Brucella infection following total joint arthroplasty (TJA).
Methods
We performed a systematic review of the literature regarding outcomes of Brucella infection after TJA (hip and knee). We searched multiple databases for articles in the area published from 1950 to 2016.
Results
A total of 18 patients (12 male and 6 female; mean age 59 years) from 14 published studies were identified. The minimum follow-up time was 6 months (range, 6–120 months). Seven patients were treated with debridement or antibrucella treatment only. Eleven patients (61%) underwent removal of the prosthesis and were treated with one or two-stage exchange arthroplasty. The mean duration of antibiotic therapy was 5.8 months. There was no relapse of infection.
Conclusions
In the absence of loosening of the components of the prosthesis, an attempt to treat Brucella infection medically might be a reasonable choice. One or two-stage exchange arthroplasty could provide successful results without relapse of infection when combined with appropriate antibiotherapy.
Level of evidence
Level III, therapeutic study.
Keywords: Brucella, Periprosthetic infection, Arthroplasty, Treatment
Introduction
Brucellosis is a common zoonosis worldwide but predominantly affects the Persian Gulf, South America, India, Central Asia, and Mediterranean countries.1 Transmission can occur via breaks in the skin in direct contact, through the ingestion of unpasteurized dairy products or raw meat, or through ingestion of aerosolized bacteria.2 Brucella infection following total joint arthroplasty (TJA) is extremely rare and not quickly diagnosed.3 This bacteria tend to be slow growing, so the culture period should be made longer than usual.4 In the majority of cases diagnosis is serological and the low positiveness (15–20%) of the culture increases the period of no diagnosis.5
The generic name of Brucella includes a group of small gram-negative cocci and cocci rods that are aerobic, not mobile, with no spores. Six different species are known: B melitensis, B abortus, B suis, B canis, B ovis, and B neotomae.6 These species are capable of surviving within phagocytic cells, making antibiotic treatment difficult.2 Correct management for Brucellar infection diagnosed through aspiration or over a well fixed TJA is still unclear.7 Traditionally, routine treatment usually includes the surgical removal of all bioprosthetic components.3 Debridement without removal of prosthesis is a controversial issue due to the potential risk of relapse of infection. However, a few cases of Brucella prosthetic infection successfully treated with antibrucella agent alone without surgical treatment had been reported.4, 8 Due to the insufficiency of standardized clinical and evidence-based guidelines, there is no appropriate therapeutic schedule. In addition, the risk of relapse following treatment for Brucella prosthetic joint infection is unknown. Although a few reviews of single institution experience exist on this subject, an absence of systematic literature reviews about the outcomes of Brucella infection following TJA provides the impetus for this systematic review.
The current study was designed to evaluate the epidemiology and treatment outcomes of Brucella infection after TJA with a review of the literature and pooled analysis. We therefore asked: (1) What are the treatment options for Brucella infection following total joint arthroplasty? (2) What are the outcomes of Brucella infection according to treatment modality?
Methods
Literature review
We performed a systematic review of the available literature using multiple separate search strategies. Four computer databases (PubMed, Web of Science, Embase, and Cochrane Library) were searched with the search words “arthroplasty”, “Brucella”, and “infection” in different combinations. Two independent reviewers separately completed the search, and the results were duplicated two times by each reviewer. The initial search was performed on June 10, 2016 with an update in August 10, 2016, to ensure accuracy. No additional study was identified by repeating the search.
Study inclusion
The inclusion criteria included (1) articles published from January 1, 1950 to January 10, 2016, (2) English-written articles in human species, (3) electronic publications that reported cases of Brucella infection, (4) both retrospective and prospective series, (5) only cases of Brucella infection after TJA, and (6) Only those articles that evaluated the final outcomes including reinfection.
The exclusion criteria included (1) conference presentations, (2) abstracts only, (3) articles without postoperative follow-up period and outcomes, (4) evaluation of any other lesion than the hip and knee joint, (5) native joint infection before arthroplasty, and (6) non-English articles. Due to the limited evidence available on the topic, case reports and case series were included in our study. Limits for the number of patients in each study or the minimum duration of follow-up were not used. Brucella infection following osteotomy and internal fixation was excluded.9
Study selection
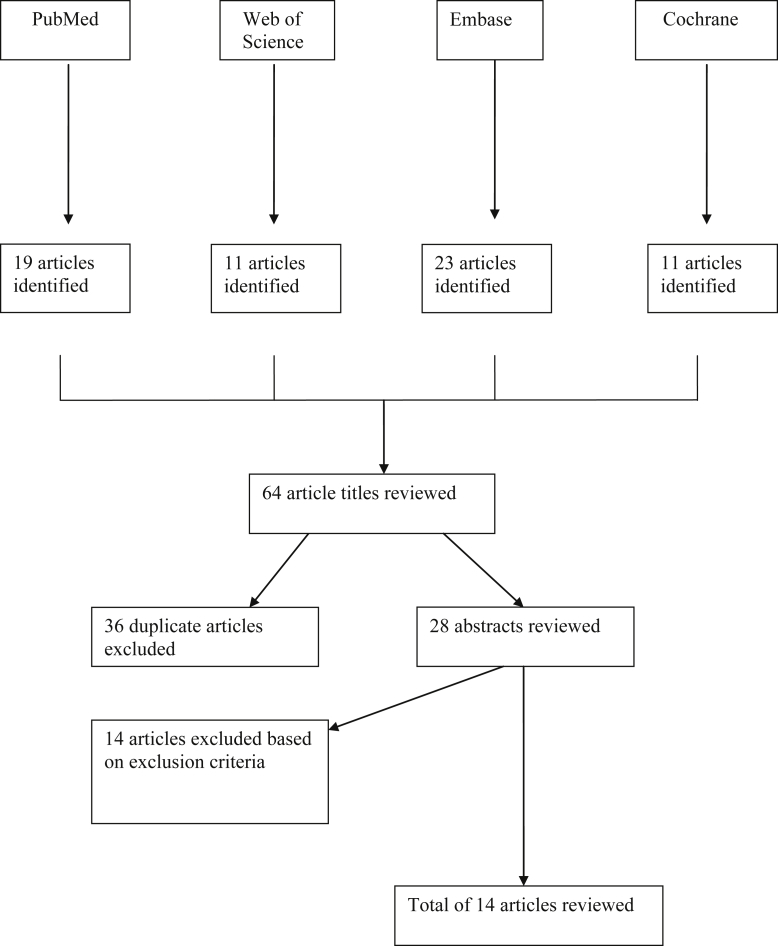
Searching the aforementioned databases yielded a total of 64 articles. A simplified flow-chart depicting this process is seen in Fig. 1. A first search of the PubMed database yielded 19 articles and a second search of the Web of Science database with use of the same search strategy yielded 11 articles. There were 36 articles that appeared in more than one of the four searches yielding a total of 28 unique articles. Abstracts and full texts of the retrieved articles were read by 2 authors independently, and all relevant articles were read in full. In addition, we screened the references of the obtained articles for any additional studies. Disagreements regarding inclusion were resolved by discussion. Stringent exclusion criteria were applied, leaving 14 articles appropriate finally. Owing to a lack of prospective studies, most of the larger cohorts giving an answer or at least an insight to clinical problems were selected for this review. The Preferred reporting items for systematic reviews and meta-analyses (PRISMA) guideline10 was followed. Studies of Brucella infection after TJA predominantly started after the cases of Jones et al in 19833, although there had been several prior reports of osteoarticular infection due to brucella.11
Fig. 1.
The flowchart details the method of retrieval of relevant articles for this study.
Data extraction
Data were extracted from the included studies by two reviewers and checked by another. Where possible, corresponding authors were contacted to obtain missing data. The following data were extracted: demographics including age, gender, underlying disease, history of previous infection, risk factor, time to symptom after TJA, preoperative erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), diagnosis of Brucella infection, management of infection, postoperative antibrucella therapy, outcomes following treatment including clinical resolution, reactivation of infection, and other complications.
Results
Our systematic literature review of PubMed, Web of Science, Embase, and Cochrane literature searches revealed a total of 18 patients from 14 selected articles which have been reported from 1983 to 2015. Although complete data were not available, data such as age, gender, underlying medical/surgical conditions, reactivation of infection and postoperative complications were collected. Age, gender, pathogen organism, and antibiotic treatment were clearly identified in all the reports.
Epidemiology
There were 12 male patients and 6 female patients. The mean age of the patients was 59 years. The minimum follow-up was 6 months (range, 6–120 months). Demographic information is detailed in Table 1. The median duration from prosthesis implantation to the onset of symptoms was 3.9 years. It was difficult to analyze blood levels of CRP and ESR at presentation due to reporting inconsistencies (Table 2). Preoperative arthrocentesis and joint fluid cultures were performed in 13 patients and yielded negative culture results for 5 patients (38%). Eight patients (62%) were diagnosed with Brucella infection by Preoperative joint aspirates. B. melitensis was found to be the most common pathogen organism, with a pooled percentage of 78% (14/18). B. abortus was the second most common pathogen organism (22%). Additional history taken from the patients after the culture results revealed that almost all patients (94%) had a history of contact with livestock, or ingestion of unpasteurized dairy products (Table 3). Patient's history was not clearly reported in one study.5
Table 1.
Demographic information in the studies.
| Author | Journal | Year | Country | Gender | Age | Location | UD or risk factor |
|---|---|---|---|---|---|---|---|
| Carothers | Am J Orthop | 2015 | USA | F | 67 | Hip | NA |
| Erdogan | Knee Surg Sports Traumatol Arthrosc | 2010 | Turkey | F | 63 | Knee | DM, previous infection |
| Dauty | Joint Bone Spine | 2009 | France | F | 65 | Knee | NA |
| Tassinari | Chir Organi Mov | 2008 | Italy | M | 68 | Knee | NA |
| Tena | Diagnostic Microbiology and Infectious Disease | 2007 | Spain | M | 51 | Hip | NA |
| Ruiz-Iban | Journal of Orthopaedic Surgery | 2006 | Spain | F | 66 | Hip | None |
| M | 71 | Hip | None | ||||
| Cairo | J Bone Joint Surg Am | 2006 | Spain | M | 50 | Hip | ON |
| M | 71 | Hip | OA | ||||
| Kasim | Scand J Infect Dis | 2004 | Lebanon | F | 47 | Hip | OA |
| Weil | Clinical Infectious Diseases | 2003 | Israel | M | 38 | Hip | Psoriatic arthritis |
| M | 64 | Knee | Hip fusion | ||||
| M | 67 | Knee | OA | ||||
| Ortega-Andreu | The Journal of Arthroplasty | 2002 | Spain | M | 63 | Hip | OA, heavy smoker |
| Orti | Eur. J. Clin. Microbiol. Infect. Dis | 1997 | Spain | M | 60 | Knee | hyperglycemia, nephrolithiasis, ON |
| malizos | Am J Orthop | 1997 | Greece | M | 74 | Knee | NA |
| Agarwal | Clin Orthop Relat Res | 1991 | Saudi Arabia | F | 24 | Knee | RA |
| Jones | Orthopedics | 1983 | USA | M | 54 | Hip | ON, OA |
UD, underlying disease; NA, not available; DM, diabetes mellitus; ON, osteonecrosis; OA, osteoarthritis; RA, rheumatoid arthritis.
Table 2.
Data on the studies.
| Author | Symptom | Time to symptom after arthroplasty (years) | Admission radiographic finding | ESR/CRP | Aspiration | Joint fluid culture |
|---|---|---|---|---|---|---|
| Carothers | Thigh pain | 2 | Bone loss around cement | 54/0.24 | Yes (yellow synovial fluid) | Negative |
| Erdogan | Knee pain, chills, fever | 2 | No sign of implant loosening | 43/18 | Yes | Positive |
| Dauty | Discharge, fever | NA | Loosening of tibial plateau | 60/80 | Yes | Negative |
| Tassinari | Knee pain | 2 | Small area of resorption on tibial component | 81/4.61 | Yes (turbid yellowish corpuscolated fluid) | Positive |
| Tena | Hip pain, fever | 5 | Implant loosening | ESR 40 | Yes (purulent fluid) | Positive |
| Ruiz-Iban | Thigh pain, groin pain | 3 | Radiolucent lines | increased | Yes | Positive |
| Painless suppuration | 2 | Well-integrated | NA | No | No | |
| Cairo | Intraoperative culture | Intraoperative culture | No loosening | ESR 123 | No | No |
| Hip pain, limping | 3 | Loosening | NA | No | No | |
| Kasim | Hip pain | 14 | Loosening | ESR 88 | No | No |
| Weil | Hip pain, fever | 4 | Loosening of femoral component | ESR 20 | Yes | Negative |
| Swollen, painful, warm knee | 3 | Loosening of both femoral and tibial components | NA | Yes | Negative (Acinetobacter baumanii) | |
| Fever, pelvic pain | 14 | Loosening of the femoral component. | ESR 76 | Yes | Positive | |
| Ortega-Andreu | Hip pain | 5 | Loosening of femoral component | NA | No | No |
| Orti | Knee pain | 1 | No loosening | 57/64 | Yes (serosanguineous synovial material) | Positive |
| Malizos | Synovitis, knee pain | 0.3 | No loosening | NA | Yes (serosanguineous synovial material) | Positive |
| Agarwal | Superficial infection, abscess | 0.2 | No loosening | NA | Yes (serosanguineous synovial material) | Positive |
| Jones | Fever | 3 | No loosening | ESR 36 | Yes | Negative |
NA, not available; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein.
Table 3.
History taken from the patient.
| Author | History taken from the patient |
|---|---|
| Carothers | Febrile illness consistent with brucellosis |
| Erdogan | Nonpasteurized milk products, previous Brucella infection |
| Dauty | Unpasteurized goat cheese |
| Tassinari | Systemic infection from Brucella |
| Tena | Farmer with sheep, no history of raw milk ingestion |
| Ruiz-Iban | Contact with cattle |
| Worked in an agricultural field | |
| Cairo | Working with cattle |
| Farmer contact with cattle | |
| Kasim | Eating home-made cheese, prepared from unpasteurized fresh milk, |
| Weil | Ingestion of unpasteurized milk or goat cheese |
| Ingestion of unpasteurized milk or goat cheese | |
| Ingestion of unpasteurized milk or goat cheese | |
| Ortega-Andreu | Cattle owner |
| Orti | Worked with goats |
| Malizos | Shepherd |
| Agarwal | NA |
| Jones | Dairy farmer exposed to the infected cattle |
NA, not available.
Treatment
Eleven patients (61%) underwent removal of the prosthesis for initial treatment and were treated with one or two-stage exchange arthroplasty (Table 4). Two-stage exchange arthroplasty was performed in 8 patients (44%) with variable time frame between removal of the prosthesis and reimplantation (median 3.1 months, range 1.5–6 months). No patient underwent resection arthroplasty. Surgical debridement, retention of implant, and antibrucella therapy were performed in one patient.7 Six patients were treated with antibrucella treatment only. The mean duration of antibiotic therapy for all patients was 5.8 months. Antibiotic therapy duration ranged from 6 weeks to 26 months, and the antibiotic treatment involved combination therapy with multiple agents (most commonly doxycycline, rifampin, and streptomycin). It was difficult to analyze the dose of antibrucella drugs due to a wide variation.
Table 4.
Treatments and outcomes of the studies.
| Author | Agglutination titer | Operation | Pathogen | Antibiotic treatment | Duration (months) | Follow up (years) | Outcome |
|---|---|---|---|---|---|---|---|
| Carothers | NA | Yes (2 stage) | B. abortus | Rifampin 600 mg, doxycycline 200 mg | 5 | 2 | No reinfection |
| Erdogan | 640 | No | B. melitensis | Rifampin 600 mg, doxycycline 200 mg | 4 | 3 | No reinfection |
| Dauty | NA | Yes (2 stage) | B. melitensis | Rifampin 900 mg, vibramycin 200 mg | 1.5 | 10 | No reinfection |
| Tassinari | 800 | No | B. melitensis | Rifampin 250 mg, doxycycline 200 mg | 2 | 1 | No reinfection |
| Tena | 80 | Yes (2 stage) | B. melitensis | Rifampin 900 mg, doxycycline 200 mg | 2 | 4 | No reinfection |
| Ruiz-Iban | NA | Yes (2 stage) | B. abortus | Rifampin 900 mg, doxycycline 200 mg | 1.5 | 5.5 | No reinfection |
| 640 | Yes (drainage) | B. melitensis | Rifampin 900 mg, SM 1 g, doxycycline 200 mg | 6 | 5 | No reinfection | |
| Cairo | 320 | No | B. melitensis | Doxycycline 200 mg, SM 1 g | 26 | 5 | No reinfection |
| NA | Yes (1 stage) | B. melitensis | Rifampin 600 mg doxycycline 200 mg, SM 750 mg | 6 | 3 | No reinfection, radiolucent line at the femoral interface | |
| Kasim | 80 | Yes (1 stage) | B. abortus | Vibramycin 200 mg, rifampin 600 mg | 5 | 4 | No reinfection, |
| Weil | 1600 | Yes (2 stage) | B. melitensis | Rifampin 600 mg doxycycline 200 mg | 1.5 | 1 | No reinfection |
| 1600 | Yes (2 stage) | B. melitensis | Rifampin 600 mg doxycycline 200 mg | 1.5 | 1 | No reinfection | |
| 1600 | Yes (2 stage) | B. melitensis | Rifampin 600 mg doxycycline 200 mg | 1.5 | 1 | No reinfection | |
| Ortega-Andreu | NA | Yes (2 stage) | B. melitensis | Rifampin 900 mg, SM 1 g, doxycycline 200 mg | 3 | 0.5 | No reinfection |
| Orti | 160 | No | B. melitensis | Rifampin 900 mg, SM 1 g, doxycycline 200 mg | 1.5 | 0.7 | No reinfection |
| Malizos | 160 | No | B. melitensis | SM 1 g, doxycycline 200 mg, Septrin Forte twice | 7 | 2.6 | No reinfection |
| Agarwal | 2560 | No | B. melitensis | Rifampin 300 mg, two septra tablets | 19 | 1.6 | No reinfection |
| Jones | 640 | Yes (1 stage) | B. abortus | Tetracycline 2 g, SM 1 g | 12 | 3 | No reinfection |
NA, not available; SM, streptomycin.
Outcomes
Mean duration of follow up after the surgical procedure was 3 years (range, 0.5–10 years). There was no relapse of infection. In one patient, at the time of the latest follow-up at three years, radiographs showed a radiolucent line at the femoral interface. There was no death related to the brucella infection following TJA and deteriorating systemic brucellosis. No postoperative neurological or vascular complications were observed in any of the patients.
Discussion
Brucellosis is a zoonosis that generally causes systemic infection and affects osteoarticular tissue in 10%–85% of patients.12 To date, prosthetic joint infection has been discussed extensively in the literature whereby staphylococci, streptococci and Gram-negative bacilli have been reported to be the most common causative organisms.8, 13, 14 However, the treatment and outcome of Brucella infection involving prosthetic joints is not well known. The aim of this report was to evaluate the epidemiology and to give treatment recommendations of Brucella infection after TJA with a pooled analysis of the reported cases.
There are generally three ways for the infection to spread: by contaminated food or drinks, inhalation, or through small wounds in the skin.15 Of these, however, the first one is surely the most common way.5, 16 Dairy products, especially soft cheeses, unpasteurized milk, and ice cream, are the most frequently implicated sources.9 It is thought that the implant is infected by hematogenous spread of the microorganism at the time of systemic infection. Since the disease is still present, in varying trends, both in European countries and in the USA17, screening for brucellosis is recommended for countries where brucellosis is still endemic5 and the possibility of exposure exists (e.g., travel to or previous residence in endemic areas)2.
Several reports comment on the ability to treat periprosthetic joint infection in the setting of well-fixed components with antibiotic therapy alone.2, 15 There is no general consensus regarding the type and dose of antibrucella agents that can be administered systemically to treat this challenging condition. Most authors suggested a minimum duration of antibrucella therapy of 6 weeks.7, 8, 18, 19 There is no evidence that a shorter period of antibrucella treatment will give the same results. In our pooled analysis, the mean duration of antifungal therapy was 5.8 months (range 6 weeks–26 months). Rifampin, doxycycline, and streptomycin have been considered the drugs of choice for administration in most report.2, 4, 16, 20 Selecting the appropriate antibrucella treatment requires a multiteam approach involving the treating orthopaedic surgeon, infectious disease specialists, and clinical pharmacologists. If removal of the arthroplasty is not an option (for instance due to the wishes of the patient or poor general condition), chronic suppression with antibrucella treatment could be recommended in the absence of loosening of the components of the prosthesis.5 Further multicenter studies are needed to establish objective treatment guidelines for Brucella infection following TJA before this method attains widespread use.
According to a recent study, in cases of Brucella infection and loose components, surgical treatment (one- or two-stage revision) with appropriate antibiotic therapy was recommended.2 In the present study, more than half of the patients (61%) underwent removal of the prosthesis for initial treatment and were treated with one or two-stage exchange arthroplasty. There was no relapse of infection after surgery. The ideal interval between implant removal and reimplantation is unknown. We found a mean of 3.1 months, with a range from 1.6 to 6 months. We recommend that that reimplantation should be performed only in the absence of clinical signs of infectious symptoms, with CRP and ESR serum levels within the normal range.21 Additional 4–6 weeks of combined antibiotic therapy after reimplantation is also recommended.18, 19 To the best of our knowledge, there exist currently no guidelines according to which Brucella periprosthetic infections should be locally managed. Nevertheless, we believe that impregnating the bone cement with antibiotics could be recommended, because Brucella joint infections have a high risk of subsequent other bacterial infections.19 Even though antibiotic-loaded bone cement may not prevent relapse of Brucella infection, it could reduce the risk of other bacterial infection.22 The incorporation of antibrucella drugs (streptomycin) into the methylmethacrylate powder used in cementing the replacement prosthesis has been reported previously.3
Of note, in cases of Brucella infection, the appropriate preventative measures to avoid transmission are necessary. Because of the nature of the surgical procedure (irrigation and debridement using pulse lavage), surgeons should be worried about aerosolization of Brucella bacteria and possible transmission to all staff present during the procedure.2
Limitations of this systematic review
Our study has some limitations. First, our study is limited by the quality of the studies we included. Due to the limited available evidence on antibrucella treatment for infection after TJA, we relied considerably on case reports and case series in this study. Second, because this is a pooled analysis of several retrospective case series with a heterogeneous cohort of patients, not all the data that we sought to include in our analysis was presented in sufficient detail to allow meaningful statistical inferences and comparisons.
Conclusion
In conclusion, in the consideration of Brucella periprosthetic joint infections treatment, one or two-stage exchange arthroplasty combined with adequate systemic antibiotic therapy is highly recommended. Local antibacterial drugs could be added to the cement especially when there is suspicious co-infection with other bacteria. In the setting of well-fixed components, Brucella infections can be managed conservatively with the combination antibiotic therapy. Additional prospective studies with involvement of larger number of patients with Brucella infection to include a wide range of ethnic backgrounds will help improve our ability to avoid the devastating outcomes.
Conflicts of interest
No conflicts declared.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Seung-Ju Kim, Email: sju627@hotmail.com.
Hyun-Soo Park, Email: swkoo9@gmail.com.
Dong-Woo Lee, Email: kgsldw@naver.com.
Jong Hun Kim, Email: sju627@naver.com.
References
- 1.Ariza J. Brucellosis in the 21st Century. Med Clin (Barc) 2002;119(9):339–344. doi: 10.1016/s0025-7753(02)73409-x. [DOI] [PubMed] [Google Scholar]
- 2.Carothers J.T., Nichols M.C., Thompson D.L. Failure of total hip arthroplasty secondary to infection caused by Brucella abortus and the risk of transmission to operative staff. Am J Orthop (Belle Mead NJ) 2015;44(2):E42–E45. [PubMed] [Google Scholar]
- 3.Jones R.E., Berryhill W.H., Smith J., Hofmann A., Rogers D. Secondary infection of a total hip replacement with Brucella abortus. Orthopedics. 1983;6(2):184–186. doi: 10.3928/0147-7447-19830201-09. [DOI] [PubMed] [Google Scholar]
- 4.Erdogan H., Cakmak G., Erdogan A., Arslan H. Brucella melitensis infection in total knee arthroplasty: a case report. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):908–910. doi: 10.1007/s00167-010-1048-x. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal S., Kadhi S.K., Rooney R.J. Brucellosis complicating bilateral total knee arthroplasty. Clin Orthop Relat Res. 1991;(267):179–181. [PubMed] [Google Scholar]
- 6.Ortega-Andreu M., Rodriguez-Merchan E.C., Aguera-Gavalda M. Brucellosis as a cause of septic loosening of total hip arthroplasty. J Arthroplasty. 2002;17(3):384–387. doi: 10.1054/arth.2002.30284. [DOI] [PubMed] [Google Scholar]
- 7.Ruiz-Iban M.A., Crespo P., Diaz-Peletier R., Rozado A.M., Lopez-Pardo A. Total hip arthroplasty infected by Brucella: a report of two cases. J Orthop Surg (Hong Kong) 2006;14(1):99–103. doi: 10.1177/230949900601400122. [DOI] [PubMed] [Google Scholar]
- 8.Orti A., Roig P., Alcala R. Brucellar prosthetic arthritis in a total knee replacement. Eur J Clin Microbiol Infect Dis. 1997;16(11):843–845. doi: 10.1007/BF01700416. [DOI] [PubMed] [Google Scholar]
- 9.Cairo M., Calbo E., Gomez L. Foreign-body osteoarticular infection by Brucella melitensis: a report of three cases. J Bone Jt Surg Am. 2006;88(1):202–204. doi: 10.2106/JBJS.D.02656. [DOI] [PubMed] [Google Scholar]
- 10.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(1):b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keenan M.A., Guttmann G.G. Brucella osteomyelitis of the distal part of the femur. A case report. J Bone Jt Surg Am. 1982;64(1):142–144. [PubMed] [Google Scholar]
- 12.Mousa A.R., Muhtaseb S.A., Almudallal D.S., Khodeir S.M., Marafie A.A. Osteoarticular complications of brucellosis: a study of 169 cases. Rev Infect Dis. 1987;9(3):531–543. doi: 10.1093/clinids/9.3.531. [DOI] [PubMed] [Google Scholar]
- 13.Tattevin P., Cremieux A.C., Pottier P., Huten D., Carbon C. Prosthetic joint infection: when can prosthesis salvage be considered? Clin Infect Dis. 1999;29(2):292–295. doi: 10.1086/520202. [DOI] [PubMed] [Google Scholar]
- 14.Garvin K.L., Hanssen A.D. Infection after total hip arthroplasty. Past, present, and future. J Bone Jt Surg Am. 1995;77(10):1576–1588. doi: 10.2106/00004623-199510000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Malizos K.N., Makris C.A., Soucacos P.N. Total knee arthroplasties infected by Brucella melitensis: a case report. Am J Orthop (Belle Mead NJ) 1997;26(4):283–285. [PubMed] [Google Scholar]
- 16.Tassinari E., Di Motta D., Giardina F., Traina F., De Fine M., Toni A. Brucella infection in total knee arthroplasty. Case report and revision of the literature. Chir Organi Mov. 2008;92(1):55–59. doi: 10.1007/s12306-008-0031-x. [DOI] [PubMed] [Google Scholar]
- 17.Pappas G., Papadimitriou P., Akritidis N., Christou L., Tsianos E.V. The new global map of human brucellosis. Lancet Infect Dis. 2006;6(2):91–99. doi: 10.1016/S1473-3099(06)70382-6. [DOI] [PubMed] [Google Scholar]
- 18.Dauty M., Dubois C., Coisy M. Bilateral knee arthroplasty infection due to Brucella melitensis: a rare pathology? Jt Bone Spine. 2009;76(2):215–216. doi: 10.1016/j.jbspin.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Weil Y., Mattan Y., Liebergall M., Rahav G. Brucella prosthetic joint infection: a report of 3 cases and a review of the literature. Clin Infect Dis. 2003;36(37):e81–e86. doi: 10.1086/368084. [DOI] [PubMed] [Google Scholar]
- 20.Tena D., Romanillos O., Rodriguez-Zapata M. Prosthetic hip infection due to Brucella melitensis: case report and literature review. Diagn Microbiol Infect Dis. 2007;58(4):481–485. doi: 10.1016/j.diagmicrobio.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Ueng S.W., Lee C.Y., Hu C.C., Hsieh P.H., Chang Y. What is the success of treatment of hip and knee candidal periprosthetic joint infection? Clin Orthop Relat Res. 2013;471(479):3002–3009. doi: 10.1007/s11999-013-3007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cui Q., Mihalko W.M., Shields J.S., Ries M., Saleh K.J. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J Bone Jt Surg Am. 2007;89(4):871–882. doi: 10.2106/JBJS.E.01070. [DOI] [PubMed] [Google Scholar]