1. Introduction
Traumatic Brain Injury (TBI) is a prevalent and potentially disabling condition that has impacted military personnel for decades (Ommaya et al., 1996). Recently, epidemiological reports have estimated that between 15% and 23% of soldiers deployed to military conflicts in Afghanistan (Operation Enduring Freedom; OEF) and Iraq (Operation Iraqi Freedom; OIF) sustain at least one Traumatic Brain Injury (TBI) while deployed (Hoge et al., 2008; Terrio et al., 2009). These findings underscore the urgent need to further understand the consequences and sequelae of TBI, particularly among recently deployed military personnel who are at up to 2.5 times greater risk for TBI compared to their civilian counterparts (Ommaya, Ommaya, Dannenberg, & Aalazar, 1996). Of particular concern is the apparent association of TBI with increased risk for post-traumatic stress (PTS; Hoge et al., 2008). PTS, a collection of trauma-related symptoms including re-experiencing the trauma, avoiding reminders, negative cognitions or mood, and hyperarousal (American Psychiatric Association, 2013), is associated with major personal and societal burden (Gadermann, Alonso, Vilagut, Zaslavsky, & Kessler, 2012; Kessler, 2000; Kessler & Greenberg, 2002). Therefore, understanding risk factors for PTS, such as TBI, is crucial to mitigating impairment among our military service members.
There is ample evidence that TBI is associated with elevated risk for PTS, most of which is derived from large surveys of soldiers returning from deployments (Barnes, Walter, & Chard, 2012; Bryan & Clemans, 2013; Bryant et al., 2010; Hoge et al., 2008; Ruff, Riechers, Wang, Piero, & Ruff, 2012; Schneiderman, Braver, & Kang, 2008). For instance, among a sample of 2525 U.S. Army Infantry soldiers returning home following an OIF deployment, trauma-exposed soldiers who sustained a TBI were more likely to meet criteria for PTSD than trauma-exposed individuals without a prior TBI (Hoge et al., 2008). Critically, Hoge et al. found that the greater likelihood of PTSD among those with a TBI (compared to those without a TBI) was robust to combat intensity and other relevant covariates, suggesting that the association of TBI and elevated PTS is not merely an index of the severity of trauma exposure. Extending upon these findings, Bryant et al. (2010) compared psychiatric illness rates among trauma-exposed individuals who experienced a TBI compared to those with other physical injuries that resulted from a trauma. Results demonstrated that individuals with a history of TBI were more likely to meet criteria for PTSD at 3 months and 12 months post-injury compared to individuals who incurred non-brain related physical injuries, demonstrating that the association between prior TBIs and PTSD is not merely the effect of trauma-exposure that yields physical injuries (Bryant et al., 2010). Further, a greater number TBIs appears to be positively associated with PTS symptoms (Bryan & Clemans, 2013; Ruff et al., 2012; Schneiderman et al., 2008), suggesting that individuals with a history of multiple TBIs may be at even greater risk for PTSD. Thus, it is clear that TBI, and in particular multiple TBIs, are associated with elevated PTS even when stringently accounting for demographic and injury-related covariates. Yet, no research that the present authors are aware of has examined the effect of prior TBIs on PTS in the context of well-established cognitive-affective risk factors for PTS.
Perhaps one of the most well-researched cognitive-affective risk factors for PTS is anxiety sensitivity (AS; Reiss & McNally, 1985), which reflects the extent to which an individual fears anxiety-related sensations stemming from their tendency to interpret these sensations as harmful or dangerous. AS was originally conceptualized as being composed of three lower-order factors: AS cognitive concerns (ASCC; i.e., misinterpretation of anxiety-related cognitive dyscontrol as dangerous), AS physical concerns (i.e., fears of physical symptoms of anxiety), and AS social concerns (i.e., fears of the social consequences of anxiety). However, recent research suggests AS may be better conceptualized as a general AS factor and three distinct, orthogonal factors of ASCC, AS physical concerns, and AS social concerns (Allan, Albanese, Short, Raines, & Schmidt, 2015). Though all three subfactors have been associated with PTS, the specificity of ASCC to symptoms of cognitive dyscontrol or dysfunction, which is a primary symptom associated with prior TBIs (Dimoska-Di Marco, McDonald, Kelly, Tate, & Johnstone, 2011), suggests the utility of studying the relationship between TBI and PTS within the context of this subfactor. For instance, individuals with high ASCC may interpret having difficulties concentrating, a common symptom among those with prior TBIs (Ryan & Warden, 2003), to mean that they are going crazy, rather than as a benign and temporary symptom.
ASCC is believed to contribute to the genesis and maintenance of PTS by amplifying both peri-traumatic affective reactions as well as post-traumatic emotional responses to reminders of the trauma through the amplification of cognitive-dyscontrol symptoms of anxiety resulting from the misinterpretation that these symptoms are harmful (see Taylor, 2003 for a review). Several studies have demonstrated a positive relationship between ASCC and PTS (Asmundson & Stapleton, 2008; Boffa et al., 2016; Vujanovic, Zvolensky, & Bernstein, 2008). For example, active-duty police officers with PTSD have greater ASCC compared to active-duty police officers without PTSD (Asmundson & Stapleton, 2008). Similarly, Lang, Kennedy, and Stein (2002) assessed risk for PTSD among women exposed to interpersonal violence. Results indicated that trauma-exposed women with PTSD reported greater ASCC than those without PTSD, and ASCC significantly predicted PTS symptom severity. Olatunji and Fan (2015) utilized a trauma-film lab paradigm to elucidate the role of ASCC in PTS symptoms and found that ASCC predicted greater trauma-related intrusive thoughts throughout 1 week following the trauma-film, providing further evidence for the causal role of ASCC in PTS symptomology. This finding was supported in a naturalistic longitudinal study in which ASCC prior to a traumatic event (i.e., a campus shooting) prospectively predicted post-shooting PTS symptoms (Boffa et al., 2016). Taken together, extant literature strongly supports the role of ASCC in the etiology and maintenance of PTS symptoms.
Theoretically, individual differences in levels of ASCC may moderate the effect of TBI on PTS. As described above, ASCC increases PTS through the amplification of cognitive-dyscontrol symptoms of anxiety through the misinterpretation of these sensations as harmful (Asmundson & Stapleton, 2008; Boffa et al., 2016; Taylor, 2003; Vujanovic et al., 2008). Importantly, TBI is associated with similar symptoms of cognitive dyscontrol (Ryan & Warden, 2003) which may be amplified by AS (Albanese, Boffa, Macatee, & Schmidt, 2017) and are theorized to be a mechanism explaining the link between TBI and PTS (Aupperle, Melrose, Stein, & Paulus, 2012). Thus, high ASCC may increase the effect of TBI on PTS through the misinterpretation of cognitive dyscontrol symptoms as harmful, thereby amplifying emotional reactions to a trauma reminder.
The current study is the first to test the unique and interactive effects of ASCC and the number of prior probable TBIs on PTS symptoms among a trauma-exposed sample. Given extant research associating PTS symptoms with higher ASCC (Asmundson & Stapleton, 2008; Boffa et al., 2016; Vujanovic et al., 2008) and a greater number of TBIs (Barnes et al., 2012; Bryan & Clemans, 2013; Bryant et al., 2010; Hoge et al., 2008; Ruff et al., 2012; Schneiderman et al., 2008), we hypothesized that both of these factors would demonstrate unique and positive relationships with PTS symptoms. Moreover, given evidence that ASCC amplifies PTS through the exacerbation of anxiety-related cognitive dyscontrol symptoms, we hypothesized that ASCC would moderate the effects of increasing numbers of probable TBIs on elevated PTS such that the effects of TBI would be stronger among those with greater ASCC. Lastly, research demonstrates that individuals with greater degrees of trauma exposure report greater PTS (Kessler, 2000) and high comorbidity rates of depression and PTS (Gadermann et al., 2012). Therefore, the frequency of traumatic event exposure and depression levels were included as covariates in all analyses.
2. Methods
2.1. Participants
The present sample was composed of 97 active duty U.S. Soldiers who voluntarily presented to an emergency department or behavioral health clinic located at an Army installation in the Western U.S. between January 2013 and February 2016 (78.4% male; M = 26.12 years, SD = 6.35). Participants were selected based on their endorsement of a previous traumatic event from a larger sample of Active duty U.S. Army personnel who were referred for a baseline intake evaluation as a part of a randomized controlled trial testing the efficacy of a brief cognitive-behavioral therapy for the prevention of suicide attempts. Participants completed a structured suicide risk assessment interview and then completed a battery of self-report measures via laptop computer, described below. Data from this initial assessment were used for the present study. All participants gave written consent for their data to be collected and used for research purposes. Regulatory approval for this study was received from the Madigan Army Medical Center Institutional Review Board.
Trauma history data were missing for 5 individuals and 3 individuals reported no history of traumatic events, leaving 89 individuals for analyses. Rank distribution was 75% E1-E4, 16% E5-E6, 4% E7-E9, and 5% officer. Self-reported racial identity was 74% White, 18% Black, 4% Asian, 3% Pacific Island, 8% Native American, and 2% other. Hispanic ethnicity was assessed separately and was endorsed by 7% of participants. Participants had deployed, on average, 1.2 times (SD=1.2).
2.2. Measures
Life Events Checklist (LEC)
The LEC is a self-report measure that assesses the respondent’s exposure to potentially traumatic events (Gray, Litz, Hsu, & Lombardo, 2004). Respondents indicate whether they personally experienced or witnessed any of 16 events potentially relevant to PTSD (e.g., physical assault, combat exposure). The LEC has demonstrated good psychometric properties in student and veteran samples (Gray et al., 2004). The LEC was altered for the parent study to assess the time period during which the traumatic event occurred. Specifically, respondents indicated if the event happened to them or was witnessed before they joined the military, during deployment, or after they joined the military but not during deployment. However, the current study utilized a total score for the LEC that represented lifetime count of traumatic events experienced (i.e., a frequency count of all traumatic events from before they joined the military, during deployment, or after they joined the military but not during deployment), which is consistent with prior use of the LEC (Gray et al., 2004). Lastly, participants were asked to indicate which event was the most stressful or upsetting, which was then referenced when participants were asked to indicate their PTS symptoms (see below).
Posttraumatic Stress Disorder Checklist – Specific Stressor Version (PCL-S)
The PCL-S is a 17-item self-report measure that assesses PTSD symptoms as defined by the DSM-IV (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). The PCL-S was administered immediately following the LEC, and participants were instructed to endorse each item on the PCL-S with regard to the event on the LEC that they endorsed as the most stressful or upsetting. Respondents indicate the extent to which each PTS symptom bothered them over the last month on a 1 (not at all) to 5 (extremely) Likert-type scale. The PCL-S has demonstrated good psychometric properties in prior work (Blanchard et al., 1996; Ruggiero, Del Ben, Scotti, & Rabalais, 2003). The PCL-S demonstrated good internal consistency in the current study (α = 0.95).
Anxiety Sensitivity Index – 3 Cognitive Concerns Subscale (ASI-3)
The ASI-3, adapted from the ASI (Reiss, Peterson, Gursky, & McNally, 1986), is an 18-item self-report measure that assesses fear of the physical, social, and cognitive consequences of anxiety symptoms (Taylor et al., 2007). Respondents indicate the extent to which they agree with each item on a five-point Likert-type scale from one (very little) to five (very much). The ASI-3 has demonstrated good psychometric properties in prior work (Chavarria et al., 2015; Taylor et al., 2007) and recent evidence suggests that each of the AS subfactors are best understood as distinct, orthogonal constructs (Allan, Albanese, et al., 2015). Only the cognitive concerns subscale was available in the current study.1 The cognitive concerns subscale is composed of six items that assess fears of the cognitive consequences of anxious arousal (e.g., “When I cannot keep my mind on a task, I worry that I might be going crazy”), though only five of the six items were available in the current study due to the omission of one item (“It scares me when I am unable to keep my mind on a task”) in the parent study. Critically, the internal consistency of the five-item subscale score was excellent (α = 0.92) and comparable to prior studies using the full six-item subscale (Norr, Albanese, Allan, & Schmidt, 2015), providing justification for the use of the 5-item subscale for the proposed analyses. The ASI-3 cognitive concerns subscale demonstrated excellent internal consistency in the current study (α = 0.92), which is consistent with prior research (e.g., α = 0.94 – 0.95; Norr et al., 2015; Norr, Albanese, Boffa, Short, & Schmidt, 2016)
Traumatic Brain Injury – 4 (TBI-4)
The TBI-4 (Olson-Madden et al., 2010) is a 4-item screening questionnaire used to assess for history of probable TBI. This measure has shown good sensitivity and high specificity for verified past TBIs (Olson-Madden et al., 2010). In the current study, an additional item was added in which participants indicated the number of different times that any of these items applied to them during their lifetime (“How many times during your life has this occurred?”). Therefore, the present study used the TBI-4 to identify the history of any probable TBIs that an individual may have experienced, and the additional item (i.e., the number of probable TBIs) was utilized to assess for the number of times that each individual has experienced a probable TBI, as defined by the TBI-4.
Beck Depression Inventory – II (BDI-II)
The BDI-II is a 21-item self-report measure of depressive symptoms (Beck, Steer, & Brown, 1996). Respondents are asked to choose the statement that best reflects how they have felt over the past two weeks, with higher scores indicating greater depressive symptoms. The BDI-II has demonstrated good psychometric properties in prior work (Wang & Gorenstein, 2013). The BDI-II demonstrated excellent internal consistency in the current study (α = 0.90).
3. Results
3.1. Sample descriptives
Please see Table 1 for means, standard deviations, and bivariate correlations of all study variables. Among those who indicated a probable history of TBI (n = 59), 48 reported either losing consciousness or being hospitalized/treated in an emergency room following a probable TBI at least once, and the mean number of probable TBIs was 2.61 (SD = 3.92). With regard to trauma exposure, the most commonly reported deployment-related traumatic events were exposure to a fire/explosion (n = 41) followed by exposure to combat/war zone (i.e., directing fire at others; n = 41). The most commonly reported non-deployment traumatic events were traffic accidents (n = 62) followed by physical assault (n = 60).
Table 1.
Descriptives and Bivariate Correlations
| Measures | M (SD) | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 1. PCL-C | 50.73 (17.25) | – | ||||
| 2. ASI-3 CC | 15.32 (6.23) | 0.64*** | – | |||
| 3. Number of TBIs | 2.61 (3.92) | 0.22* | 0.21 | – | ||
| 4. BDI-2 | 33.27 (11.43) | 0.43*** | 0.43*** | 0.22* | – | |
| 5. Number of traumas | 8.93 (4.81) | 0.35** | 0.37*** | 0.25* | 0.13 | – |
Note. PCL-C = Posttraumatic Stress Disorder Checklist – Civilian Version. ASI-3 CC = Anxiety Sensitivity Index – 3 Cognitive Concerns Subscale (5-item version). Number of TBIs = Total past TBIs reported. BDI-2 = Beck Depression Inventory – 2. Number of traumas = Life Events Checklist.
p < .05.
p < .01.
p < .001.
3.2. Main effects analyses
First, multiple linear regression was used to evaluate the unique effects of ASCC and number of probable TBIs on PTS symptoms. After controlling for number of past traumatic events [β = 0.14, t(82) = 1.51, p = 0.13, r2 = 0.02] and depressive symptoms [β = 0.17, t(82) = 1.87, p = 0.07, r2 = 0.02], a significant main effect of ASCC [β = 0.51, t(82) = 5.21, p < 0.001, r2 = 0.18] but not number of probable TBIs [β = 0.04, t(82) = 0.42, p = 0.68, r2 = 0.001] emerged. The overall model predicted a significant amount of variance in PTS symptoms, R2 = 0.45, F(4, 82) = 16.77, p < 0.001.
3.3 Moderating effects of ASCC on the relationship between number of probable TBIs and PTS
Next, we used multiple regression to test the hypothesis that the relationship between number of probable TBIs and PTS symptoms is moderated by ASCC. Number of probable TBIs and ASCC were mean-centered prior to creating the interaction term. BDI-2 scores and the number of traumatic events experienced were included as covariates. The overall model predicted a significant amount of variance in PTS symptoms, R2 = 0.48, F(5, 81) = 15.06, p < 0.001. After controlling for history of trauma exposure [β = 0.17, t(81) = 1.90, p = 0.06, r2 = 0.02 ] and depressive symptoms [β = 0.18, t(81) = 1.95, p = 0.06, r2 = .02], a significant main effect of ASCC [β = 0.50, t(81) = 5.28, p < 0.001, r2 = 0.18] but not number of probable TBIs [β = −0.15, t(81) = −1.24, p = 0.22, r2 = 0.01] emerged. Further, the interaction effect was also significant [β = 0.25, t(81) = 2.23, p = 0.03, r2 = 0.03].
We then probed the interaction at high (+1.5 SD and +2 SD) and low (−1.5 SD and −2 SD) levels of ASCC to test the moderating effects of ASCC on the relationship between number of probable TBIs and PTS. Results indicated that number of probable TBIs was marginally and negatively related to PTS for individuals 1.5 SDs below the mean of ASCC [β = −0.44 t(81) = −1.92, p = 0.059, r2 = 0.04] and non-significantly related to PTS at 1.5 SDs above the mean of ASCC [β = 0.15, t(81) = 1.50, p = 0.14, r2 = 0.01]. This pattern of effects of number of probable TBIs on PTS was further highlighted when probing the interaction at 2 SDs below [β = −0.54, t(81) = −1.99, p = 0.05, r2 = 0.03] and above [β = 0.24, t(81) = 1.95, p = 0.055, r2 = 0.02] the mean of ASCC (see Figure 1).
Figure 1.
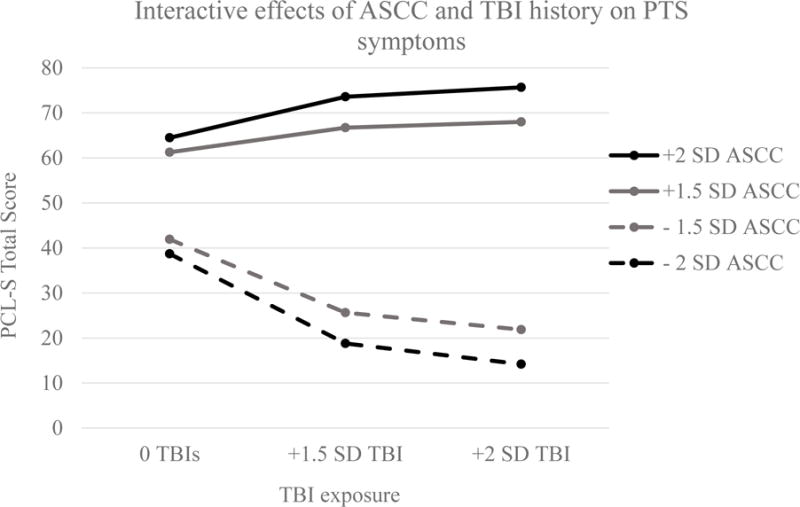
TBI = Traumatic Brain Injury. ASCC = Anxiety sensitivity cognitive concerns. PTS = Post-traumatic stress. PCL-5 = Post-traumatic stress checklist for DSM-5. SD = Standard Deviation. Effects of TBI exposure on PTS symptoms at low (1.5 SD and 2 SD below the mean) and high (1.5 SD and 2 SD above the mean) ASCC. Results indicated that a greater number of probable TBIs has a stronger relationship with PTS at high ASCC, such that the number of probable TBIs is negatively associated with PTS at low ASCC and positively related to PTS at high ASCC.
3.4 Moderating effects of number of probable TBIs on the relationship between ASCC and PTS
To further understand the interactive effects of number of probable TBIs and ASCC, we conducted an exploratory analysis evaluating the moderating effects of ASCC on the relationship between number probable TBIs and PTS. To accomplish this, we probed the previously presented significant interaction between ASCC and number of probable TBIs to test the effects of ASCC at different levels of TBI exposure [β = 0.25, t(81) = 2.23, p = 0.03, r2 = 0.03]. To remain consistent with the primary analyses, we elected to probe the effects of ASCC on PTS among individuals with 1.5 SDs above the mean number of probable TBIs and 2 SDs above the mean number of probable TBIs. Further, because an individual cannot have fewer than zero probable TBIs, we elected to not probe the interaction at values below the mean and instead probed the interaction among individuals with zero TBIs. Results indicated that ASCC was significantly and positively related to PTS regardless of the number of probable TBIs, though this effect was stronger for those a greater number of probable TBIs [i.e., 2 SDs above the mean number of probable TBIs, β = 0.89, t(81) = 4.54, p < .001, r2 = 0.13; 1.5 SDs above the mean number of probable TBIs, β = 0.79, t(81) = 4.97, p < .001, r2 = 0.16], compared to those with zero prior TBIs [β = 0.40, t(81) = 3.76, p < .001, r2 = 0.09].
4. Discussion
The present study was the first to investigate the effects of the number of probable TBIs on PTS in the context of cognitive-affective factors among trauma-exposed, active duty soldiers, specifically the moderating effects of ASCC on the relationship between number of probable TBIs and PTS. The hypothesis that a greater number of probable TBIs would have a stronger and positive relationship with PTS among those with high (compared to low) ASCC garnered partial support; number of probable TBIs was positively associated with PTS for those with high (2 SDs above the mean) ASCC. Unexpectedly, our results also indicated that a greater number of probable TBIs was negatively related to PTS for individuals with progressively lower ASCC, despite the positive bivariate relationship between number of probable TBIs and PTS. This pattern of results suggests that high ASCC may exacerbate the effects of a greater number of probable TBIs on PTS while low ASCC may suppress this risk. Results further indicated that ASCC was more strongly related to PTS among those with a greater number of probable TBIs, indicating that a TBIs may potentiate the effects of variability in ASCC on PTS symptomology. These results are consistent with prior findings demonstrating that ASCC (Asmundson & Stapleton, 2008; Boffa et al., 2016; Vujanovic et al., 2008) and probable TBIs (Bryan & Clemans, 2013; Ruff et al., 2012; Schneiderman et al., 2008) contribute to PTS symptoms, and extend our knowledge of these relationships by demonstrating a two-way interaction of ASCC and the number of probable TBIs an individual has incurred.
It is plausible that the moderating effects of ASCC on the relationship between the number of probable TBIs and PTS arises from the amplification (high ASCC) or suppression (low ASCC) of cognitive dyscontrol symptoms, which are believed to be a mechanism by which the number of probable TBIs influences PTS (Aupperle et al., 2012; Bryant, 2008; Dimoska-Di Marco et al., 2011; Schneiderman et al., 2008). Elevated ASCC is characterized by the catastrophic misinterpretation of cognitive dyscontrol as harmful or dangerous, which subsequently generates greater cognitive dyscontrol symptoms via heightened anxious arousal (Olatunji & Wolitzky-Taylor, 2009). Thus, high ASCC may amplify the symptoms of cognitive dyscontrol that contribute to PTS (Aupperle et al., 2012) and are likely to be experienced by those with a greater number of probable TBIs (Dimoska-Di Marco et al., 2011; Dockree & Robertson, 2011; Ryan & Warden, 2003). Conversely, for individuals with a more probable TBIs and low ASCC, the interpretation of cognitive dyscontrol symptoms as benign may enable them to better tolerate these sensations, as opposed to responding anxiously and thereby enhancing their cognitive dyscontrol symptoms and, subsequently, PTS. Thus, having low ASCC may help individuals better tolerate TBI sequelae (e.g., cognitive dyscontrol) with regard to PTS. This interpretation is consistent with literature demonstrating the roles of cognitive dyscontrol (Aupperle et al., 2012) and ASCC (Aupperle et al., 2012; Bryant, 2008) in PTS, as well as the influence of ASCC on the expression of cognitive dyscontrol symptoms (Olatunji & Wolitzky-Taylor, 2009).
Interestingly, we also conducted an exploratory analysis that found a moderating effect of the number of probable TBIs on the relationship between ASCC and PTS, such that ASCC has a stronger influence on PTS among those with a greater number of probable TBIs. One interpretation of this finding is that trauma-exposed soldiers with probable TBIs are more likely to experience cognitive dyscontrol (Dimoska-Di Marco et al., 2011; Dockree & Robertson, 2011; Ryan & Warden, 2003), making beliefs about the relative harm/safety of cognitive dyscontrol symptoms (i.e., ASCC) a stronger predictor of PTS. Alternatively, it is plausible that experiencing multiple probable TBIs may intensify the influence of ASCC on PTS via reductions in cognitive control. This viewpoint is consistent with a larger body of work that suggests that intact cognitive control may protect those vulnerable to psychopathology (e.g., those with high ASCC; Asmundson & Stapleton, 2008; Vujanovic et al., 2008) from experiencing negative mental health outcomes (B. Albanese et al., in press; Bardeen & Fergus, 2015; Fergus, Bardeen, & Orcutt, 2012; Jones, Fazio, & Vasey, 2012; Richey, Keough, & Schmidt, 2012). For instance, Bardeen and Fergus (2015) found that intact attentional control, a facet of cognitive control, moderated the effects of the broad anxiety sensitivity factor on PTS. Thus, exposure to multiple TBIs may diminish the protective effects of good cognitive control, leaving the vulnerability for PTS conferred by high ASCC essentially uncensored.
The results of the current study suggest that mitigating cognitive-affective risk factors for PTS, such as ASCC, may be particularly important among trauma exposed soldiers with an extensive history of probable TBIs. Notably, ASCC has demonstrated malleability to brief interventions. For instance, Schmidt, Capron, Raines, and Allan (2014) demonstrated that a single-session, 45-minute computerized ASCC intervention significantly reduced ASCC, and that changes were maintained at a 1-month follow-up. Another investigation of brief AS interventions revealed that reductions in ASCC mediated PTS symptom amelioration (Allan, Short, Albanese, Keough, & Schmidt, 2015). Though no current studies have investigated the use of brief ASCC interventions to prevent PTS prior to or immediately following a traumatic event, evidence from investigations of anxiety and depression prevention suggest that this may be a promising avenue of investigation to ameliorate rates of PTSD among those with a history of multiple probable TBIs. Thus, active-duty soldiers who are likely to experience traumatic events, such as those deployed to combat zones, may benefit from an ASCC intervention, particularly if they have incurred multiple probable TBIs in the past.
There are several limitations to the present study that must be noted. First, the measure of TBI used in the present study provides only an index of the number of probable TBIs incurred in an individual’s lifetime. This method of assessing TBIs relies on participant self-reported memory of potential TBIs, which may be vulnerable to self-report and memory biases. This method also relies on self-diagnosis, as opposed to clinician-verification, of past TBIs which may introduce diagnostic error. However, the measure of TBI used in the current study is one of the most widely used self-report assessments of probable TBIs, and it has been favorably compared with clinical interviews (Brenner et al., 2013; Olson-Madden et al., 2010), lending confidence that these data represent accurate histories of TBI. In addition, the present study used a 5-item version of the ASCC, as opposed to the traditional 6-item ASCC subscale of the ASI-3 (Taylor et al., 2007). The reliability of the 5-item ASCC measure was supported by the demonstration of good internal reliability, though the validity of a 5-item measure of ASCC has yet to be supported. Therefore, the present findings should be replicated using the full ASCC subscale. Lastly, the present data are cross-sectional, limiting the interpretation of results. Future research should seek to utilize longitudinal designs to capture the prospective effects of ASCC and number of probable TBIs on PTS development and maintenance.
The present study was also limited by the inability to test the relative influences of the other AS subscales (i.e., AS physical concerns, AS social concerns) on traumatic stress in the context of probable TBIs, as these data were not collected by the parent study (as discussed in the methods section). Future research should attempt to address this limitation by testing the interactive effects of the number of probable TBIs and all AS total and subfactor scores. Lastly, the present study relied on self-reported PTS symptomology, which presents potentially biased reporting. This limitation should be mitigated in future research by utilizing a clinical interview of PTS symptomology such as the Structured Clinical Interview for DSM-5, Research Version (SCID-5-RV; First, Williams, Karg, & Spitzer, 2015) or Clinician Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013).
Despite these limitations, the main finding that ASCC moderates the effect of more probable TBIs on PTS addresses a noticeable gap in TBI and PTS literature by evaluating the effects of TBI on PTS in the context of a well-established cognitive-affective risk factor for PTS (i.e., ASCC). Given research demonstrating that those with a more probable TBIs are more likely to have symptoms of cognitive dyscontrol (Ryan & Warden, 2003), which can contribute to greater PTS if misinterpreted as harmful or dangerous (Asmundson & Stapleton, 2008; Boffa et al., 2016; Vujanovic et al., 2008), it is reasonable that non-distorted interpretations of cognitive dyscontrol (i.e., low ASCC) are helpful in tolerating TBI sequelae with regard to PTS symptomology. However, further research is needed to establish the prospective predictive utility of the reported cross-sectional effects as well as to evaluate the relative contributions of the other AS subscales. Moreover, future research may benefit from further investigating the moderating effects of other malleable cognitive-affective risk factors (e.g., Distress Tolerance; Leyro, Zvolensky, & Bernstein, 2010; Macatee & Cougle, 2015) on the relationship between the number of probable TBIs and PTS.
Acknowledgments
Role of funding source
This work was in part supported by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award No. W81XWH-10-2-0181. Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the MSRC or the Department of Defense.
This work was also in part supported by the National Institute of Health Integrated Clinical Neuroscience Training for Translational Research (4T32MH093311-05). Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the National Institute of Health.
Footnotes
Conflicts of interest: Brian J. Albanese declares that he has no conflicts of interest. Richard J. Macatee declares that he has no conflicts of interest. Norman B. Schmidt declares that he has no conflicts of interest. Bruce Leeson declares that he has no conflicts of interest. Tracy A. Clemans declares that she has no conflicts of interest. Jim Mintz declares that he has no conflicts of interest. M. David Rudd declares that he has no conflicts of interest. Craig J. Bryan declares that he has no conflicts of interest.
The parent study, which focused on risk factors for suicidality, collected only the ASCC subscale due to research demonstrating that ASCC is uniquely related to suicidality (Capron, Norr, Macatee, & Schmidt, 2013).
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- Albanese B, Macatee RJ, Allan NP, Short NA, Norr AM, Schmidt NB. Interactive effects of anxiety sensitivity and attentional control on post-traumatic stress in community and clinical populations. Psychiatry: Interpersonal and Biological Processes. doi: 10.1080/00332747.2017.1309867. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albanese BJ, Boffa JW, Macatee RJ, Schmidt NB. Anxiety sensitivity mediates gender differences in post-concussive symptoms in a clinical sample. Psychiatry Research. 2017;252:242–246. doi: 10.1016/j.psychres.2017.01.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan NP, Albanese BJ, Short NA, Raines AM, Schmidt NB. Support for the general and specific bifactor model factors of anxiety sensitivity. Personality and Individual Differences. 2015;74:78–83. [Google Scholar]
- Allan NP, Short NA, Albanese BJ, Keough ME, Schmidt NB. Direct and mediating effects of an anxiety sensitivity intervention on posttraumatic stress disorder symptoms in trauma-exposed individuals. Cognitive Behaviour Therapy. 2015;44(6):512–524. doi: 10.1080/16506073.2015.1075227. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Dsm 5. American Psychiatric Association; 2013. [Google Scholar]
- Asmundson GJ, Stapleton JA. Associations between dimensions of anxiety sensitivity and ptsd symptom clusters in active-duty police officers. Cognitive Behaviour Therapy. 2008;37(2):66–75. doi: 10.1080/16506070801969005. [DOI] [PubMed] [Google Scholar]
- Aupperle RL, Melrose AJ, Stein MB, Paulus MP. Executive function and ptsd: Disengaging from trauma. Neuropharmacology. 2012;62(2):686–694. doi: 10.1016/j.neuropharm.2011.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardeen JR, Fergus TA. Emotional distress intolerance, experiential avoidance, and anxiety sensitivity: The buffering effect of attentional control on associations with posttraumatic stress symptoms. Journal of Psychopathology and Behavioral Assessment. 2015:1–10. [Google Scholar]
- Barnes SM, Walter KH, Chard KM. Does a history of mild traumatic brain injury increase suicide risk in veterans with ptsd? Rehabilitation psychology. 2012;57(1):18. doi: 10.1037/a0027007. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck depression inventory-ii. San Antonio, TX. 1996:78204–72498. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the ptsd checklist (pcl) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Boffa JW, Norr AM, Raines AM, Albanese BJ, Short NA, Schmidt NB. Anxiety sensitivity prospectively predicts posttraumatic stress symptoms following a campus shooting. Behavior Therapy. 2016;47(3):367–376. doi: 10.1016/j.beth.2016.02.006. [DOI] [PubMed] [Google Scholar]
- Brenner LA, Homaifar BY, Olson-Madden JH, Nagamoto HT, Huggins J, Schneider AL, Corrigan JD. Prevalence and screening of traumatic brain injury among veterans seeking mental health services. The Journal of head trauma rehabilitation. 2013;28(1):21–30. doi: 10.1097/HTR.0b013e31827df0b5. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Clemans TA. Repetitive traumatic brain injury, psychological symptoms, and suicide risk in a clinical sample of deployed military personnel. JAMA psychiatry. 2013;70(7):686–691. doi: 10.1001/jamapsychiatry.2013.1093. [DOI] [PubMed] [Google Scholar]
- Bryant RA. Disentangling mild traumatic brain injury and stress reactions. New England Journal of Medicine. 2008;358(5):525–527. doi: 10.1056/NEJMe078235. [DOI] [PubMed] [Google Scholar]
- Bryant RA, O’donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. The American Journal of Psychiatry. 2010;167:312–320. doi: 10.1176/appi.ajp.2009.09050617. [DOI] [PubMed] [Google Scholar]
- Chavarria J, Allan NP, Boffa JW, Albanese BJ, Schmidt NB, Zvolensky MJ. Decomposing the relationship between anxiety sensitivity and alcohol use. Journal of studies on alcohol and drugs. 2015;76(6):957–961. doi: 10.15288/jsad.2015.76.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimoska-Di Marco A, McDonald S, Kelly M, Tate R, Johnstone S. A meta-analysis of response inhibition and stroop interference control deficits in adults with traumatic brain injury (tbi) Journal of clinical and experimental neuropsychology. 2011;33(4):471–485. doi: 10.1080/13803395.2010.533158. [DOI] [PubMed] [Google Scholar]
- Dockree PM, Robertson IH. Electrophysiological markers of cognitive deficits in traumatic brain injury: A review. International Journal of Psychophysiology. 2011;82(1):53–60. doi: 10.1016/j.ijpsycho.2011.01.004. [DOI] [PubMed] [Google Scholar]
- Fergus TA, Bardeen JR, Orcutt HK. Attentional control moderates the relationship between activation of the cognitive attentional syndrome and symptoms of psychopathology. Personality and Individual Differences. 2012;53(3):213–217. [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL. Structured clinical interview for dsm-5 – research version (scid-5 for dsm-5, research version; scid-5-rv) Arlington, VA: American Psychiatric Association; 2015. [Google Scholar]
- Gadermann AM, Alonso J, Vilagut G, Zaslavsky AM, Kessler RC. Comorbidity and disease burden in the national comorbidity survey replication (ncs-r) Depression and Anxiety. 2012;29(9):797. doi: 10.1002/da.21924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in us soldiers returning from iraq. New England Journal of Medicine. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- Jones CR, Fazio RH, Vasey MW. Attentional control buffers the effect of public-speaking anxiety on performance. Social psychological and personality science. 2012;3(5):556–561. doi: 10.1177/1948550611430166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61:4–14. [PubMed] [Google Scholar]
- Kessler RC, Greenberg PE. The economic burden of anxiety and stress disorders. Neuropsychopharmacology: The fifth generation of progress. 2002;67:982–992. [Google Scholar]
- Lang AJ, Kennedy CM, Stein MB. Anxiety sensitivity and ptsd among female victims of intimate partner violence. Depression and Anxiety. 2002;16(2):77–83. doi: 10.1002/da.10062. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological bulletin. 2010;136(4):576. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macatee RJ, Cougle JR. Development and evaluation of a computerized intervention for low distress tolerance and its effect on performance on a neutralization task. Journal of Behavior Therapy and Experimental Psychiatry. 2015;48:33–39. doi: 10.1016/j.jbtep.2015.01.007. [DOI] [PubMed] [Google Scholar]
- Norr AM, Albanese BJ, Allan NP, Schmidt NB. Anxiety sensitivity as a mechanism for gender discrepancies in anxiety and mood symptoms. Journal of Psychiatric Research. 2015;62:101–107. doi: 10.1016/j.jpsychires.2015.01.014. [DOI] [PubMed] [Google Scholar]
- Norr AM, Albanese BJ, Boffa JW, Short NA, Schmidt NB. The relationship between gender and ptsd symptoms: Anxiety sensitivity as a mechanism. Personality and Individual Differences. 2016;90:210–213. [Google Scholar]
- Olatunji B, Fan Q. Anxiety sensitivity and post-traumatic stress reactions: Evidence for intrusions and physiological arousal as mediating and moderating mechanisms. Journal of Anxiety Disorders. 2015;34:76–85. doi: 10.1016/j.janxdis.2015.06.002. [DOI] [PubMed] [Google Scholar]
- Olatunji B, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: A meta-analytic review and synthesis. Psychological bulletin. 2009;135(6):974–999. doi: 10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Olson-Madden JH, Brenner L, Harwood JE, Emrick CD, Corrigan JD, Thompson C. Traumatic brain injury and psychiatric diagnoses in veterans seeking outpatient substance abuse treatment. The Journal of head trauma rehabilitation. 2010;25(6):470–479. doi: 10.1097/HTR.0b013e3181d717a7. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. Theoretical Issues in Behavior Therapy. 1985:107–121. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Richey JA, Keough ME, Schmidt NB. Attentional control moderates fearful responding to a 35% co 2 challenge. Behavior Therapy. 2012;43(2):285–299. doi: 10.1016/j.beth.2011.06.004. [DOI] [PubMed] [Google Scholar]
- Ruff RL, Riechers RG, Wang XF, Piero T, Ruff SS. A case–control study examining whether neurological deficits and ptsd in combat veterans are related to episodes of mild tbi. BMJ open. 2012;2(2):e000312. doi: 10.1136/bmjopen-2011-000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the ptsd checklist—civilian version. Journal of traumatic stress. 2003;16(5):495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Ryan LM, Warden DL. Post concussion syndrome. International Review of Psychiatry. 2003;15(4):310–316. doi: 10.1080/09540260310001606692. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, Allan NP. Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. Journal of Counseling and Clinical Psychology. 2014;82(6):1023–1033. doi: 10.1037/a0036651. [DOI] [PubMed] [Google Scholar]
- Schneiderman AI, Braver ER, Kang HK. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in iraq and afghanistan: Persistent postconcussive symptoms and posttraumatic stress disorder. American journal of epidemiology. 2008;167(12):1446–1452. doi: 10.1093/aje/kwn068. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety sensitivity and its implications for understanding and treating ptsd. Journal of Cognitive Psychotherapy. 2003;17(2):179–186. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the anxiety sensitivity index-3. Psychological Assessment. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Zvolensky MJ, Bernstein A. Incremental associations between facets of anxiety sensitivity and posttraumatic stress and panic symptoms among trauma-exposed adults. Cognitive Behaviour Therapy. 2008;37(2):76–89. doi: 10.1080/16506070801969039. [DOI] [PubMed] [Google Scholar]
- Wang YP, Gorenstein C. Psychometric properties of the beck depression inventory-ii: A comprehensive review. Revista Brasileira de Psiquiatria. 2013;35(4):416–431. doi: 10.1590/1516-4446-2012-1048. [DOI] [PubMed] [Google Scholar]
- Weathers F, Blake D, Schnurr P, Kaloupek D, Marx B, Keane T. The clinician-administered ptsd scale for dsm-5 (caps-5) Interview available from the National Center for PTSD. 2013 at www.ptsd.va.gov.


