Abstract
Objectives
To evaluate national health care use and costs for pediatric acute pancreatitis.
Study design
The Kids’ Inpatient Database for 2006, 2009, and 2012 was queried for patients with a principal diagnosis of acute pancreatitis. Cases were grouped by age: preschool (<5 years of age), school age (5–14 years of age), and adolescents (>14 years of age).
Results
A total of 27 983 discharges for acute pancreatitis were found. The number of admissions increased with age: young n = 1279, middle n = 8012, and older n = 18 692. Duration of stay was highest in preschool children (median, 3.47 days; IQR, 2.01–7.35), compared with school age (median, 3.22 days; IQR, 1.81–5.63) and adolescents (median, 2.87 days; IQR, 1.61–4.81; P < .001). The median cost of hospitalization varied with age: $6726 for preschoolers, $5400 for school-aged children, and $5889 for adolescents (P < .001). Acute pancreatitis–associated diagnoses varied by age. The presence of gallstone pancreatitis, alcohol, and hypertriglyceridemia was more common among older children compared with younger children (P < .001). There was an increasing trend in acute pancreatitis, chronic pancreatitis, and obesity for the 2 older age groups (P < .001).
Conclusion
Admission of children for acute pancreatitis constitutes a significant healthcare burden, with a rising number of admissions with age. However, the cost and duration of stay per admission are highest in young children.
Acute pancreatitis in children is increasingly recognized and growing in incidence.1,2 An estimated incidence of 1 in 10 000 cases occur in children based on single-center studies.2 Factors that have led to the increasing incidence in children are not fully understood. Although the majority of acute pancreatitis attacks are self-limited, with spontaneous resolution, a subset of patients progress to severe acute pancreatitis with morbidity in up to 25% and mortality in about 0.5%.3–6
Signs and symptoms of acute pancreatitis differ in younger children as compared with older children.7 We hypothesized that pediatric acute pancreatitis constitutes a significant healthcare burden, and that age affects acute pancreatitis risk factors as well as healthcare use and outcomes in the pediatric population. We further hypothesized that obesity and chronic pancreatitis have important impacts on these trends. There are limited studies that characterize the hospital course, inpatient procedures, clinical outcomes, mortality, and disease burden in children with acute pancreatitis.8–10 Current published studies lack information about the national health care use for children with acute pancreatitis, because most studies are single center and retrospective in nature.7
We analyzed data from the Kids’ Inpatient Database (KID) on admissions for acute pancreatitis and describe factors that impact trends, healthcare use, and disease outcome in the US. We also evaluated patient characteristics and comorbid conditions of children with acute pancreatitis and their outcomes as they relate to age.
Methods
The KID is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP) (https://www.hcup-us.ahrq.gov/overview.jsp). KID is the largest publicly available, all-payer pediatric inpatient care database in the US covering patient data from 44 states, yielding national estimates of hos pital inpatient stays in children. HCUP inpatient data are based on administrative data and discharge abstracts created by hospitals for billing. The KID is a sample of pediatric discharges from hospitals in states participating in HCUP. Pediatric discharges are defined as all discharges where the patient was ≤20 years of age at admission.
The KID is available every 3 years. For this study we accessed the data for the years 2006, 2009, and 2012, the latest years available in the database. These 3 years were queried for patients with a principal diagnosis of acute pancreatitis. Patient data stratified by age were recorded for sex, race, insurance, hospital type and size, procedures, imaging, duration of stay, cost of admission, and comorbid conditions, among other data, and were analyzed. Duration of stay was defined as the duration of hospital stay in days. Data in the KID were extracted using International Classification of Diseases, 9th edition, Clinical Modification (ICD-9-CM) codes. ICD-9-CM codes used for chronic pancreatitis, endoscopic retrograde cholangiopancreatography, ultrasound imaging, computed tomography of the abdomen, parenteral nutrition, gallstone and biliary pancreatitis, triglyceridemia/lipidemia, trauma, viral, pancreas divisum and other anomalies, obesity, and overweight are listed in Table I (available at www.jpeds.com). Cases were grouped as per the following classification: young age cohort (preschool; <5 years of age), middle age cohort (school age; 5–14 years of age), and adolescents (>14 years of age) on admission. The classification was based on the limited number of previous studies available and the authors’ experience.
Table I.
ICD-9-CM codes
| ICD-9 Codes | |
|---|---|
| Acute pancreatitis | 577.0 |
| Chronic pancreatitis | 577.1 |
| Endoscopic retrograde cholangiopancreatography | V45.89, 51.10, 51.11, 52.13, 52.92, 51.14, 52.14, 51.15, 51.86, 52.97, 51.88, 52.94, 51.84, 52.98, 51.87, 52.93, 51.85, 51.64, 52.21, 51.69 |
| Ultrasound | 88.74, 88.76, 88.79 |
| Computed tomography (abdomen) | 793.6, V15.89, 88.38 |
| Parental nutrition | V49.89, 99.15 |
| Gallstone/biliary | 574.40, 574.41, 574.21, 574.50, 574.51 |
| Triglyceridemia/lipidemia | 272.4, 272.1, 272.7 |
| Trauma | 959.9, 959.12, 908.9 |
| Divisum/anomalies | 751.7 |
| Obesity/overweight | 278.00, 278.01 |
The Ohio State University Data and Specimen Policy and Human Subjects Research policy does not require Institutional Review Board approval for population-based public dataset. Per 45 Code of Federal Regulations (CFR 46.101), research using certain publicly available datasets does not involve “human subjects.” The data contained within these specific datasets are neither identifiable nor private and thus do not meet the federal definition of “human subject” as defined in 45 CFR 46.102. Therefore, these research projects do not need to be reviewed and approved by the institutional review board.
Statistical Analyses
Means and 95% CI or medians and IQR were calculated for continuous variables, as appropriate, and frequency counts and percentages were used to summarize categorical variables. Continuous variables were tested for statistical significance using ANOVA and categorical variables were analyzed with χ2 tests. Temporal trends were assessed using the Cochrane–Armitage trend test. To analyze predictors of changes in trends of acute pancreatitis-related admissions, all admissions for any reason were included. A multivariate logistic regression model containing patient and hospital demographics in addition to discharge year was fit for a primary diagnosis of acute pancreatitis. Interactions between discharge year and obesity and chronic pancreatitis were evaluated. All analyses were performed on weighted data using survey procedures to produce national estimates. A P value < .05 was considered statistically significant. Statistical analysis was performed with SAS, version 9.4, (SAS Institute, Cary, North Carolina).
Results
There were 28 288 total discharges in 2006, 2009, and 2012 with a primary diagnosis of acute pancreatitis; of these a total of 27 983 discharges had available patient age data. Demographic data are shown in Table II (available at www.jpeds.com).
Table II.
Patient demographics and hospital characteristics of our sample of pediatric patients with a principal diagnosis of acute pancreatitis (overall n = 27 983)
| Characteristics | Mean (95% CI) or n (%) | |
|---|---|---|
| Age (y) | 15.15 (15.01–15.29) | |
| Sex | ||
| Male | 11 415 | (41.1) |
| Race | ||
| White | 12 680 | (53.5) |
| Black | 2703 | (11.4) |
| Hispanic | 6534 | (27.6) |
| Other | 1773 | (7.5) |
| Insurance | ||
| Medicare | 126 | (0.5) |
| Medicaid | 11 379 | (40.7) |
| Private | 12 439 | (44.5) |
| Other | 3986 | (14.3) |
| Hospital type | ||
| Rural | 2997 | (11.1) |
| Urban nonteaching | 8527 | (31.5) |
| Urban teaching | 15 513 | (57.4) |
The number of admissions increased with age: preschoolers (n = 1279), school age (n = 8012), and adolescents (n = 18 692). There were more female patients in each of the groups at 53.9%, 53.9%, and 61.3%, respectively (Table III). Pre-school children were more likely to be admitted to urban teaching hospitals—84.3%, 74.1%, and 48.7%, respectively, in preschool, school-age, and adolescent groups, respectively (P < .001). Of patients from all age groups, 60%−63% were admitted to large hospitals (Table III).
Table III.
Patient demographics and hospital characteristics by age groups
| Age <5 (n = 1279) | Age 5–14 (n = 8012) | Age >14 (n = 18 692) | P value | ||||
|---|---|---|---|---|---|---|---|
| Age | 2.66 (2.57–2.75) | 10.53 (10.43–10.62) | 17.99 (17.95–18.03) | ||||
| Gender | <.001 | ||||||
| Male | 589 | (46.1) | 3641 | (46.2) | 7185 | (38.7) | |
| Female | 687 | (53.9) | 4249 | (53.9) | 11 398 | (61.3) | |
| Race | <.001 | ||||||
| White | 518 | (48.6) | 3517 | (52.2) | 8645 | (54.4) | |
| Black | 167 | (15.6) | 662 | (9.8) | 1874 | (11.8) | |
| Hispanic | 286 | (26.8) | 2031 | (30.2) | 4217 | (26.5) | |
| Other | 97 | (9.1) | 525 | (7.8) | 1151 | (7.2) | |
| Insurance | <.001 | ||||||
| Medicare | ≤10 | (0.2) | 28 | (0.4) | 96 | (0.5) | |
| Medicaid | 641 | (50.2) | 3522 | (44.0) | 7216 | (38.7) | |
| Private | 554 | (43.4) | 3790 | (47.4) | 8095 | (43.4) | |
| Other | 80 | (6.3) | 664 | (8.3) | 3242 | (17.4) | |
| Income bracket | .19 | ||||||
| Low | 362 | (28.9) | 2349 | (29.9) | 5751 | (31.5) | |
| Moderate | 325 | (25.9) | 1963 | (25.0) | 4792 | (26.3) | |
| High | 297 | (23.7) | 1854 | (23.6) | 4105 | (22.5) | |
| Very high | 270 | (21.6) | 1680 | (21.4) | 3612 | (19.8) | |
| Hospital type | <.001 | ||||||
| Rural | 38 | (3.2) | 532 | (7.0) | 2427 | (13.3) | |
| Urban nonteaching | 146 | (12.5) | 1441 | (18.9) | 6940 | (38.0) | |
| Urban teaching | 982 | (84.3) | 5654 | (74.1) | 8877 | (48.7) | |
| Hospital bed size | .08 | ||||||
| Small | 132 | (11.4) | 790 | (10.4) | 2395 | (13.1) | |
| Medium | 320 | (27.4) | 1995 | (26.2) | 4740 | (26.0) | |
| Large | 713 | (61.2) | 4842 | (63.5) | 11 109 | (60.9) | |
| Hospital region | .83 | ||||||
| Northeast | 201 | (15.7) | 1178 | (14.7) | 2863 | (15.3) | |
| Midwest | 240 | (18.7) | 1691 | (21.1) | 4079 | (21.8) | |
| South | 510 | (39.9) | 2978 | (37.2) | 6913 | (37.0) | |
| West | 328 | (25.7) | 2165 | (27.0) | 4837 | (25.9) | |
Values are n (%) or mean (95% CI).
Older patients were more likely to undergo endoscopic retrograde cholangiopancreatography compared with the younger age groups during admissions; 10.9% in the adolescent group, 6.2% in the school-age group, and 6.3% in the preschool group (P < .001). There were no differences among age groups in associated imaging studies including ultrasound examinations or computed tomography scans of the abdomen. Parenteral nutrition was more frequently used in preschool children(15.5%) compared with 10% in those between 5 and14 years of age and 4.9% in those older than 14 years of age (P < .001) (Table IV).
Table IV.
Elements of management and patient outcomes by age groups
| Age <5 (n = 1279) | Age 5–14 (n = 8012) | Age >14 (n = 18 692) | P value | ||||
|---|---|---|---|---|---|---|---|
| Management | |||||||
| Endoscopic retrograde cholangiopancreatography | 81 | (6.3) | 498 | (6.2) | 2038 | (10.9) | <.001 |
| Ultrasound | 47 | (3.7) | 324 | (4.0) | 619 | (3.3) | .20 |
| Computed tomography (abdomen) | ≤10 | (0.1) | 28 | (0.4) | 52 | (0.3) | .54 |
| Parental nutrition | 199 | (15.5) | 800 | (10.0) | 922 | (4.9) | <.001 |
| Outcomes | |||||||
| Mortality | ≤10 | (0.2) | 17 | (0.2) | 23 | (0.1) | .30 |
| Duration of stay | 3.47 (2.01–7.35) | 3.22 (1.81–5.63) | 2.87 (1.61–4.81) | <.001 | |||
| Costs | 6726 (3485–14 080) | 5400 (3156–10 629) | 5889 (3609–9775) | <.001 | |||
| Disposition | <.001 | ||||||
| Routine | 1132 | (88.5) | 7384 | (92.2) | 17 163 | (91.9) | |
| Short-term hospital | 56 | (4.4) | 318 | (4.0) | 595 | (3.2) | |
| Other transfers | 13 | (1.1) | 66 | (0.8) | 158 | (0.9) | |
| Home health care | 72 | (5.6) | 219 | (2.7) | 341 | (1.8) | |
| Against medical advice | ≤10 | (0.1) | ≤10 | (<0.1) | 399 | (2.1) | |
Values are n (%) or median (IQR).
Preschool patients were discharged to home health care in 5.6% of the cases vs 2.7% in those 5–14 years of age, and 1.8% in those >14 years of age. Death was a rare event in pediatric acute pancreatitis and occurred in 0.12%−0.24% in all age groups (Table IV).
Duration of stay was greatest in the younger group, the preschool children (median, 3.47 days; IQR, 2.01–7.35), compared with those in the middle age group (median, 3.22 days; IQR, 1.81–5.63), and older children (median, 2.87 days; IQR-1.61, 4.81; P < .001). Cost of hospitalization varied with age: $6726 in the preschool group, $5400 in the school-age group, and $5889 in adolescents (P < .001) (Table IV).
Comorbid conditions varied in distribution between the age groups. In general, diabetes, hypertension, depression, drug abuse, and psychosis increased with age (P < .05) (Table V; available at www.jpeds.com).
Table V.
Comorbidities by age groups
| Age <5 (n = 1279) | Age 5–14 (n = 8012) | Age >14 (n = 18 692) | P value | ||||
|---|---|---|---|---|---|---|---|
| AIDS | 0 | (0.0) | ≤10 | (<0.1) | 15 | (0.1) | .12* |
| Anemia | 100 | (7.8) | 345 | (4.3) | 1544 | (8.3) | <.001 |
| Rheumatoid arthritis/collagen vascular disease | 0 | (0.0) | 51 | (0.6) | 167 | (0.9) | .13* |
| Chronic blood loss | ≤10 | (0.3) | 17 | (0.2) | 57 | (0.3) | .63 |
| Congestive heart failure | ≤10 | (0.2) | ≤10 | (0.1) | 26 | (0.1) | .80 |
| Chronic lung disease | 97 | (7.6) | 793 | (9.9) | 1561 | (8.4) | .005 |
| Coagulopathy | 29 | (2.2) | 179 | (2.2) | 325 | (1.7) | .10 |
| Depression | 0 | (0.0) | 133 | (1.7) | 1028 | (5.5) | <.001* |
| Diabetes mellitus | 11 | (0.8) | 239 | (3.0) | 1454 | (7.8) | <.001 |
| Diabetes with chronic complications | 0 | (0.0) | 25 | (0.3) | 142 | (0.8) | .001* |
| Drug abuse | ≤10 | (0.1) | 29 | (0.4) | 861 | (4.6) | <.001 |
| Hypertension | 32 | (2.5) | 255 | (3.2) | 903 | (4.8) | <.001 |
| Hypothyroidism | 12 | (1.0) | 79 | (1.0) | 269 | (1.4) | .08 |
| Liver disease | 25 | (1.9) | 265 | (3.3) | 670 | (3.6) | .06 |
| Lymphoma | 0 | (0.0) | 20 | (0.2) | 35 | (0.2) | .44* |
| Fluid and electrolyte disorders | 378 | (29.6) | 1576 | (19.7) | 3815 | (20.4) | <.001 |
| Metastatic cancer | ≤10 | (0.4) | ≤10 | (0.1) | 15 | (0.1) | .035 |
| Neurologic disease | 111 | (8.7) | 531 | (6.6) | 575 | (3.1) | <.001 |
| Paralysis | 48 | (3.8) | 333 | (4.2) | 282 | (1.5) | <.001 |
| Peripheral vascular disorders | ≤10 | (0.1) | 13 | (0.2) | 40 | (0.2) | .80 |
| Psychoses | ≤10 | (0.1) | 150 | (1.9) | 588 | (3.2) | <.001 |
| Pulmonary circulation disorders | ≤10 | (0.8) | 13 | (0.2) | 40 | (0.2) | .002 |
| Renal failure | 12 | (0.9) | 78 | (1.0) | 185 | (1.0) | .99 |
| Solid tumor without metastasis | ≤10 | (0.1) | 11 | (0.1) | 16 | (0.1) | .64 |
| Peptic ulcer disease | 0 | (0.0) | 0 | (0.0) | ≤10 | (<0.1) | — |
| Valvular disease | ≤10 | (0.7) | 24 | (0.3) | 47 | (0.3) | .06 |
| Weight loss | 23 | (1.8) | 169 | (2.1) | 517 | (2.8) | .016 |
Values are n (%).
P value excludes youngest age group.
Known etiologies and risk factors for acute pancreatitis were analyzed by age groups. The presence of alcohol, gallstones/biliary etiologies, and hypertriglyceridemia were more common among older children compared with younger children (P < .001). Pancreas divisum and other pancreatic anomalies were not significantly different between the groups (Table VI).
Table VI.
Risk factors for acute pancreatitis by age groups
| Age <5 (n = 1279) | Age 5–14 (n = 8012) | Age >14 (n = 18692) | P value | ||||
|---|---|---|---|---|---|---|---|
| Gallstone/biliary | 29 | (2.3) | 162 | (2.0) | 901 | (4.8) | <.001 |
| Triglyceridemia/lipidemia | ≤10 | (0.6) | 216 | (2.7) | 961 | (5.1) | <.001 |
| Trauma | 0 | (0.0) | ≤10 | (0.1) | 16 | (0.1) | .93* |
| Divisum/anomalies | 11 | (0.8) | 74 | (0.9) | 108 | (0.6) | .07 |
| Alcohol abuse | 0 | (0.0) | 17 | (0.2) | 1269 | (6.8) | <.001* |
| Obesity/overweight | ≤10 | (0.6) | 673 | (8.4) | 2144 | (11.5) | <.001 |
| Chronic pancreatitis | 96 | (7.5) | 920 | (11.5) | 1438 | (7.7) | <.001 |
Values are n (%).
P value excludes youngest age group.
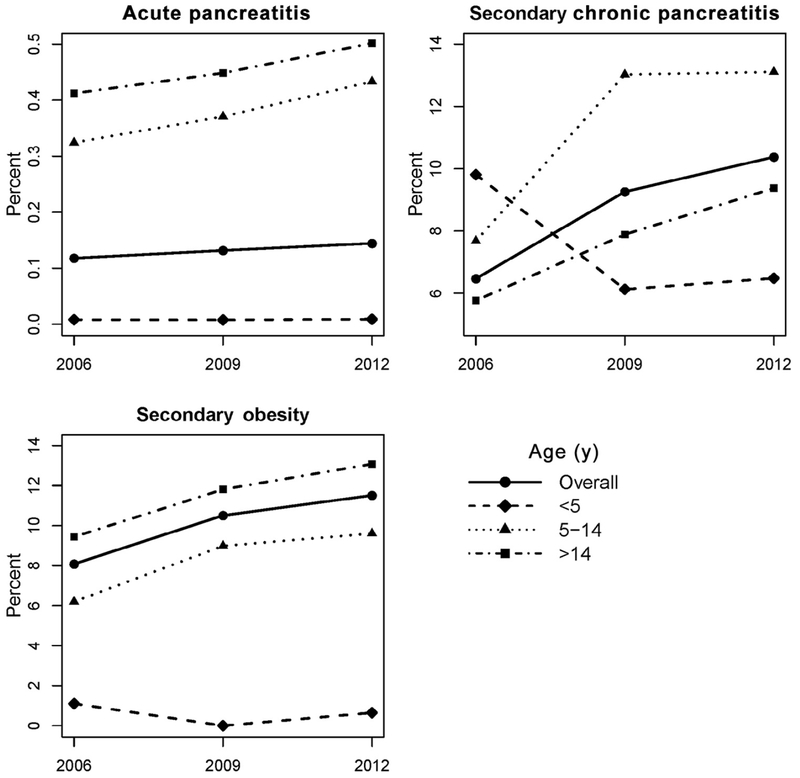
There was a significant increasing trend in acute pancreatitis from 2006 to 2012 (P < .001). Secondary diagnoses (as coded in the KID database) of obesity and chronic pancreatitis showed significant increasing trends as well (P < .001). Stratified by age groups, trends of the secondary diagnoses of obesity and chronic pancreatitis were significant only in the school age and older age groups, but not in the young age groups (Figure). Our analysis showed that there is a significant association between chronic pancreatitis and age (P < .001) and a signifi-cant association between obesity and age (P < .001).
Figure.
Overall trend of acute pancreatitis as a primary diagnosis, chronic pancreatitis, and obesity as secondary diagnoses increased over 2006, and 2009–2012. Secondary diagnosis of obesity and chronic pancreatitis trends were significant only in the middle and older age groups, but not in the young age groups.
Our multivariate logistic regression model for a primary diagnosis of acute pancreatitis revealed significant interactions between chronic pancreatitis and obesity with discharge year. Among patients with chronic pancreatitis, the odds of having a discharge diagnosis of acute pancreatitis increased over time (OR, 1.37 for 2009; OR, 1.51 for 2012 as compared with 2006). This trend is not seen in patients without chronic pancreatitis. Among patients with obesity, the odds of a primary discharge diagnosis of acute pancreatitis are not significantly different among the 3 years; however, there is an increased odds of having acute pancreatitis in 2009 and 2012 as compared with 2006 for patients without obesity (Table VII; available at www.jpeds.com).
Table VII.
Multivariate logistic regression analysis for a primary diagnosis of acute pancreatitis*
| a0R | (95% CI) | |
|---|---|---|
| Patients with chronic pancreatitis | ||
| 2006 | Reference | |
| 2009 | 1.37 | (1.04–1.80) |
| 2012 | 1.51 | (1.16–1.96) |
| Patients without chronic pancreatitis | ||
| 2006 | Reference | |
| 2009 | 1.10 | (0.92–1.11) |
| 2012 | 1.08 | (0.98–1.18) |
| Patients with obesity | ||
| 2006 | Reference | |
| 2009 | 1.14 | (0.93–1.40) |
| 2012 | 1.15 | (0.94–1.40) |
| Patients without obesity | ||
| 2006 | Reference | |
| 2009 | 1.21 | (1.05–1.38) |
| 2012 | 1.41 | (1.24–1.61) |
The model was adjusted for age, gender, race, insurance, income, hospital type, size, and region.
Discussion
We found that admissions for acute pancreatitis are increasing among children, with variability in healthcare resource use by age group. Duration of stay and cost of admission were highest in the youngest age group and decreased with age. Obesity and chronic pancreatitis trends, similar to acute pancreatitis, are increasing over time in the pediatric population. Chronic pancreatitis seems to correlate with the increased acute pancreatitis trends over the years. Alcohol and biliary causes are more commonly found in the older pediatric age groups. It is known from previous studies that biliary etiologies and alcohol play significant roles in adult acute pancreatitis,11,12 whereas pediatric cases are associated with different etiologies, including biliary, metabolic, hereditary, and anatomic anomalies.1,6,7,13
We were interested in studying the relation of chronic pancreatitis and obesity as comorbid conditions. Chronic pancreatitis is one of the manifestations of recurrent pancreatitis, and is a debilitating disease with the hallmarks being pain, organ damage, and atrophy resulting in exocrine and endocrine insufficiencies.14,15 In children, these disorders have implications not only on the overall functioning and quality of life, but also on their growth potential, bone disease, and nutrition.16 Our results show that chronic pancreatitis and obesity are more prevalent in the older age groups.
A study by Pant et al included a large cohort of children with acute pancreatitis from the KID database as well; however, their cohort consisted of primary and secondary acute pancreatitis cases, likely overestimating the acute pancreatitis admissions.17 Their results were similar to ours in that acute pancreatitis increased with age, although the previous study did not estimate the age factor on the admissions that resulted directly from acute pancreatitis. We aimed to focus our analysis on admissions with acute pancreatitis as the primary (the principle) diagnosis based on KID database coding, to study admissions that result from acute pancreatitis. The number of admissions with acute pancreatitis as a primary or secondary diagnosis over the 3 time periods studied in our analysis totaled 48 132 as expected, a higher number (1.7 times) the total admissions owing to acute pancreatitis as a primary diagnosis alone.
This study does have its limitations. KID is a billing database collected with an administrative purpose. Moreover, diagnosis, procedure, comorbidities, and complications data are reported in the form of ICD-9, Major Diagnostic Code, and Diagnosis-Related Group codes, and these methods have their limitations when applied. Recurring admissions from patients are not captured, but instead are counted as individual occurrences. We aimed to study acute pancreatitis admissions and burden on the healthcare system, so the fact that recurring admissions from the same patient are counted serves our study purpose. Certain codes may be underreported in the database, such as the use of endoscopic retrograde cholangiopancreatography or obesity. In contrast, strengths of the database are that it provides national estimates, including all types of community, academic, teaching, children’s, or nonchildren’s hospitals by using a complex survey sampling design.
Acute pancreatitis in children constitutes a significant health-care burden, with an increasing number of admissions with age. Cost and duration of stay per admission are greatest in preschool children. Future studies are needed to measure the impact of acute pancreatitis on inpatient pediatric hospitalizations.
Glossary
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, 9th edition, Clinical Modification
- KID
Kids’ Inpatient Database
Footnotes
The authors declare no conflicts of interest.
References
- 1.Lopez MJ. The changing incidence of acute pancreatitis in children: a single-institution perspective. J Pediatr 2002;140:622–4. [DOI] [PubMed] [Google Scholar]
- 2.Morinville VD, Barmada MM, Lowe ME. Increasing incidence of acute pancreatitis at an American pediatric tertiary care center: is greater awareness among physicians responsible? Pancreas 2010;39:5–8. [DOI] [PubMed] [Google Scholar]
- 3.Coffey MJ, Nightingale S, Ooi CY. Serum lipase as an early predictor of severity in pediatric acute pancreatitis. J Pediatr Gastroenterol Nutr 2013;56:602–8. [DOI] [PubMed] [Google Scholar]
- 4.DeBanto JR, Goday PS, Pedroso MR, Iftikhar R, Fazel A, Nayyar S, et al. Acute pancreatitis in children. Am J Gastroenterol 2002;97:1726–31. [DOI] [PubMed] [Google Scholar]
- 5.Lautz TB, Chin AC, Radhakrishnan J. Acute pancreatitis in children: spectrum of disease and predictors of severity. J Pediatr Surg 2011;46:1144–9. [DOI] [PubMed] [Google Scholar]
- 6.Abu-El-Haija M, Lin TK, Palermo J. Update to the management of pediatric acute pancreatitis: highlighting areas in need of research. J Pediatr Gastroenterol Nutr 2014;58:689–93. [DOI] [PubMed] [Google Scholar]
- 7.Bai HX, Lowe ME, Husain SZ. What have we learned about acute pancreatitis in children? J Pediatr Gastroenterol Nutr 2011;52:262–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Szabo FK, Fei L, Cruz LA, Abu-El-Haija M. Early enteral nutrition and aggressive fluid resuscitation are associated with improved clinical outcomes in acute pancreatitis. J Pediatr 2015;167:397–402 e1. [DOI] [PubMed] [Google Scholar]
- 9.Uc A Predicting the severity of pediatric acute pancreatitis: are we there yet? J Pediatr Gastroenterol Nutr 2013;56:584–5. [DOI] [PubMed] [Google Scholar]
- 10.Uc A Death in pediatric intensive care unit: not for children with acute pancreatitis. J Pediatr Gastroenterol Nutr 2015;61:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yadav D, Whitcomb DC. The role of alcohol and smoking in pancreatitis. Nat Rev Gastroenterol Hepatol 2010;7:131–45. [DOI] [PubMed] [Google Scholar]
- 12.Wang GJ, Gao CF, Wei D, Wang C, Ding SQ. Acute pancreatitis: etiology and common pathogenesis. World J Gastroenterol 2009;15:1427–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park AJ, Latif SU, Ahmad MU, Bultron G, Orabi AI, Bhandari V, et al. A comparison of presentation and management trends in acute pancreatitis between infants/toddlers and older children. J Pediatr Gastroenterol Nutr 2010;51:167–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morinville VD, Husain SZ, Bai H, Barth B, Alhosh R, Durie PR, et al. Definitions of pediatric pancreatitis and survey of present clinical practices. J Pediatr Gastroenterol Nutr 2012;55:261–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palermo JJ, Lin TK, Hornung L, Valencia CA, Mathur A, Jackson K, et al. Genophenotypic analysis of pediatric patients with acute recurrent and chronic pancreatitis. Pancreas 2016;45:1347–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schwarzenberg SJ, Bellin M, Husain SZ, Ahuja M, Barth B, Davis H, et al. Pediatric chronic pancreatitis is associated with genetic risk factors and substantial disease burden. J Pediatr 2015;166:890–6, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pant C, Deshpande A, Olyaee M, Anderson MP, Bitar A, Steele MI, et al. Epidemiology of acute pancreatitis in hospitalized children in the United States from 2000–2009. PLoS ONE 2014;9:e95552. [DOI] [PMC free article] [PubMed] [Google Scholar]