Abstract
Background
Utilization of psychotropic medications among the elderly has garnered attention due to concerns about safety and degree of efficacy, but may be used differently across regions.
Methods
We conducted a cross-sectional study of all antipsychotic, benzodiazepine, and trazodone prescriptions dispensed to seniors ( ≥ 65 years) leveraging IQVIA (Durham, NC) GPM data in 2013. We report the units dispensed (per 100 seniors) by province.
Results
Nationally, on average, 26,210 units of antipsychotics, 24,257 of benzodiazepines, and 7,519 of trazodone were dispensed in 2013 for every 100 seniors; reports varied across Canada. The rate of antipsychotic and benzodiazepine prescribing was highest in New Brunswick (AP: 35,375 units per 100, BZD: 43,989 units per 100), and lowest in Newfoundland & Labrador for antipsychotics (20,974 per 100) and Saskatchewan for benzodiazepines (12,692 per 100). Trazodone unit dispensation rates were highest in Nova Scotia (9,164 per 100) and lowest in Newfoundland & Labrador (2,968 per 100).
Conclusions
There is considerable geographic variation in the prescribing patterns of antipsychotics, benzodiazepine, and trazodone. This study serves as the first step in understanding these differences, while future work is needed to develop region-specific strategies to optimize the prescribing of psychotropic medications to older Canadian adults.
Keywords: antipsychotics, benzodiazepines, trazodone, psychotropics, potentially inappropriate prescribing
INTRODUCTION
Antipsychotics are a drug class used to manage psychosis. Antipsychotics are also prescribed to older adults for the management of behavioural and psychological symptoms of dementia (BPSD) and insomnia.(1) Use for these indications is considered off-label in Canada, with the exception of risperidone, which is indicated for severe BPSD in Alzheimer’s dementia.(2) High rates of use amongst older adults is concerning, given the potential for harm associated with antipsychotic use, particularly for frail elderly patients.(3)
Benzodiazepines and trazodone may be prescribed as antipsychotic alternatives among older adults for a variety of indications.(4,5) Benzodiazepine use among older adults, categorized as potentially inappropriate in guidelines,(6,7) is also a concern due to potential harms including falls, daytime sedation, and cognitive impairment.(8–10) Less is known regarding the safety of trazodone, though no benefit over placebo has been shown in clinical trials studying the treatment of BPSD,(11,12) and limited benefit for treating sleep disturbances in older adults was found in one short-term trial.(13) All of these medications have indications for use other than BPSD and insomnia, including schizophrenia and psychotic disorders for antipsychotics, anxiety disorders for benzodiazepines, and depression for trazodone. However, given the relative risks and benefits of these medications, particular consideration is recommended when prescribing these medications for older adults.(14) Use among older adults for indications including BPSD and insomnia continues to grow, as suggested by a number of studies in both community and long-term care settings.(15–17)
Recently, the Choosing Wisely campaign identified both benzodiazepines and antipsychotics as medications to use judiciously for older adults regardless of indication.(18) However, numerous factors drive drug utilization, including reimbursement policies and local clinical practices. There are limited data comparing the national and interprovincial differences in the rates of antipsychotic, benzodiazepine, and trazodone use. The objective of this study was to describe the interprovincial variation in dispensing rates of these drugs in older Canadians.
METHODS
We conducted a population-based, cross-sectional study of all antipsychotic, benzodiazepine, and trazodone prescriptions dispensed by Canadian retail pharmacies to individuals 65 years of age or older from January 1 to December 31, 2013. Trazodone was included as an individual medication due to its frequent use in practice for the treatment of BPSD and insomnia, as observed by the co-authors with clinical practice experience, while additional psychotropic medications were excluded due to their limited use for these indications.
Data Sources
IQVIA GPM dataset was used for all analyses. The source of information supporting this dataset is the IQVIA retail prescription database, which contains prescription transactions from Canadian pharmacies for all dispensed products. At the national level, more than 78% of all prescriptions dispensed are captured by a panel composed of approximately 6,000 pharmacies. Monthly prescription estimates are created using IQVIA patented geospatial projection methodology. The survey design yields a sampling error of approximately 3% for the psychotherapeutics class at the national level. Provincially, the sampling error can reach slightly higher levels, although it usually does not exceed 5% to 10% in the vast majority of cases (IQVIA, personal communication, February 12, 2016). The number of prescriptions and units (i.e., tablets) dispensed for study drugs were reported monthly, and stratified by drug and province. This data source includes aggregate prescription volumes from all payers, both public and private. All antipsychotics and benzodiazepines included in the analyses are listed in Table 1. No restrictions were made regarding medication formulation.
TABLE 1.
Antipsychotic and benzodiazepine medications included in analysis
| Class | Medications Included in Analysis |
|---|---|
| Antipsychotics | Aripiprazole, Asenapine, Chlorpromazine, Droperidol, Clozapine, Fluphenazine, Haloperidol, Loxapine, Lurasidone, Methotrimeprazine Olanzapine, Paliperidone, Periciazine, Perphenazine, Pimozide, Quetiapine, Risperidone, Thioridazine, Trifluoperazine, Zuclopenthixol |
| Benzodiazepines | Alprazolam, Bromazepam, Chlordiazepoxide, Clorazepate, Diazepam, Lorazepam, Midazolam, Oxazepam |
Statistical Analyses
We calculated the rate of units dispensed per 100 seniors for each drug in 2013 by province and nationally. As a sensitivity analysis, the prescription dispensing rate per 1,000 seniors was calculated to determine whether trends observed remained consistent. The rate of units dispensed was selected for primary analyses over prescription dispensing rate as provincial differences in regulations on the allowable amount of drug dispensed per prescription was more likely to bias results than the availability of medication doses on the unit dispensing rate (e.g., clonazepam in New Brunswick is available beginning at 0.25 mg, while coverage in Saskatchewan begins at 0.5 mg). Despite the differing availability of doses of specific medications, this availability may vary from drug to drug, which is why we approached this analysis on a drug class level. All rates were age-standardized using population estimates stratified by province for the year 2013 obtained from the Statistics Canada CANSIM database.(19) We used the Extreme Studentized Deviate (ESD) methods to determine if any value varied from the national average. A z-score greater than 1 was flagged as variation from the national average. We used SAS software version 9.4(20) to conduct data cleaning and Microsoft Excel (2010) for analyses.
RESULTS
Antipsychotics
Nationally, a total of 1.4 billion units of antipsychotics were dispensed in 2013, at a rate of 26,210 units per 100 persons. We observed a greater than 1.5-fold difference in antipsychotics dispensing between the provinces with the highest rate occurring in New Brunswick (35,375 units per 100 persons) and lowest in Newfoundland & Labrador (20,974 units per 100 persons) (see Table 2). Provinces with dispensing rates above the national rate included Alberta, Saskatchewan, Quebec, New Brunswick, and Prince Edward Island.
TABLE 2.
Antipsychotic, benzodiazepine, and trazodone unit dispensing rates in 2013, by province per 100 seniors
| Province | Antipsychotics | Benzodiazepines | Trazodone |
|---|---|---|---|
| National* | 26,210 | 24,257 | 7,519 |
| British Columbia | 23,178 | 16,575* | 7,615 |
| Alberta | 28,608 | 21,724 | 7,808 |
| Saskatchewan | 27,594 | 12,692* | 4,347 |
| Manitoba | 25,085 | 30,510 | 5,414 |
| Ontario | 22,164 | 21,513 | 8,040 |
| Quebec | 31,333* | 27,967 | 7,205 |
| New Brunswick | 35,375* | 43,989* | 4,853 |
| Prince Edward Island | 26,791 | 32,133 | 4,316 |
| Nova Scotia | 24,213 | 34,976 | 9,164* |
| Newfoundland & Labrador | 20,974* | 39,394* | 2,968* |
Indicates provincial rates vary from the national rate.
Benzodiazepines
In 2013, 1.3 billion units of benzodiazepines were dispensed across Canada, at a rate of 24,257 units per 100 persons. In general, provinces in eastern Canada (New Brunswick, Prince Edward Island, Nova Scotia, and Newfoundland & Labrador), as well as Manitoba, had benzodiazepine dispensing rates above the national average. Specifically, in New Brunswick the dispensing rate was nearly 3.5 times higher (43,989 per 100 persons) than in Saskatchewan, the province with the lowest rate of benzodiazepine dispensing (12,692 per 100 persons) (Table 2).
Trazodone
Nationally, 404.6 million trazodone units were dispensed in 2013, at a rate of 7,519 units per 100. Nova Scotia had the highest trazodone unit dispensing rate (9,164 per 100) which was over three times higher than the rate in Newfoundland & Labrador, the province with the lowest rate (2,968 per 100 persons). There was no consistent geographic pattern in trazodone prescribing, with British Columbia, Alberta, Ontario, and Nova Scotia having dispensing rates above the national average (Table 1).
Sensitivity Analysis
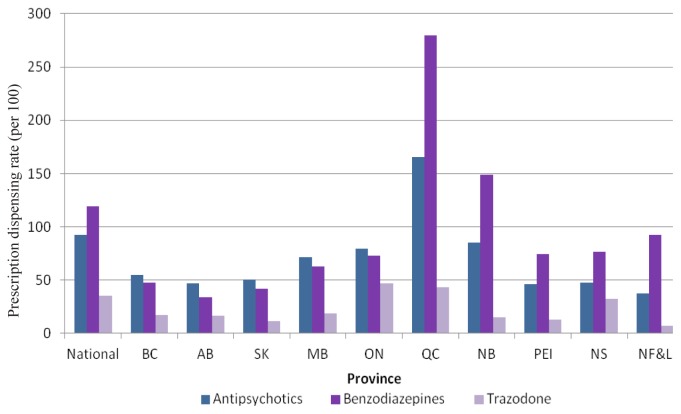
When the rate of total prescriptions dispensed was assessed, the results mostly remained consistent, though there was more variability between the provinces (Figure 1). For some provinces, the total number of prescriptions dispensed was much higher relative to the rates of other provinces and the trend observed from unit dispensing, indicating the prescription dispensing rate may overestimate psychotropic utilization in some provinces, as fewer units were dispensed per prescription.
Figure 1.
Prescription dispensing rate in 2013, by province (per 100)
DISCUSSION
In this descriptive cross-sectional study, we observed variation in the patterns of psychotropic medication dispensing among older Canadian adults. Prescription dispensing rates for each of the psychotropics studied varied across provinces, and a geographic trend emerged for antipsychotics and benzodiazepines. Specifically, western provinces, save for Manitoba, dispensed more antipsychotics than benzodiazepines, while eastern provinces dispensed more benzodiazepines than antipsychotics. Additionally, New Brunswick had the highest unit dispensing rate for both antipsychotics and benzodiazepines, and all provinces included in the analysis dispensed at least one of the classes at a higher rate than the national unit dispensing rate.
Geographic clustering of prescription utilization trends presents a novel finding of potentially differing regional prescribing. Access to these drug classes through public drug programs is generally similar across most provinces, based on a search of relevant formularies, and utilization differences are likely driven by factors unrelated to formulary listing. There are a number of potential hypotheses that can explain this trend of differing utilization rates observed across the provinces, such as access to specialized care, prescribing habits, and prescriber training.(21) Strategic initiatives targeting reductions in the use of antipsychotics and benzodiazepines in certain provinces have begun, but their impact is unknown. For example, in western provinces, the provincial governments have specifically targeted antipsychotics as a problem area since early in the study period, though in residential care most specifically.(22,23) Some western provinces, such as Alberta, now have much stricter policies around the prescribing of antipsychotics, mandating monthly clinical reviews for their continued use in some instances.(24) Other provinces had existing initiatives focused on optimizing prescribing practices, such as academic detailing in Saskatchewan, from before the study period. Notably, since 2013, many initiatives at the international (e.g., Choosing Wisely Campaign, deprescribing guidelines for both antipsychotics and benzodiazepines), national (e.g., widespread national media attention, continued reporting of CIHI indicators for antipsychotics), and provincial levels (e.g., Appropriate Use of Antipsychotics Collaborative,(25) academic detailing programs in Nova Scotia and Ontario(26)) have been undertaken to understand and address potentially inappropriate prescribing of both antipsychotics and benzodiazepines.(27) It is hoped that the impact of these will be detectable through future studies of psychotropic utilization. There are other possibilities for differences in prescribing rates of specific classes that may not be attributable to availability of other agents. For example, in the case of benzodiazepines, it is possible that differing availability of Z-drugs explains the trends in use of traditional benzodiazepines.
Importantly, the data used in this study contain prescriptions dispensed to patients living both in the community and in long-term care settings. Patterns and indications of use vary between the two settings.(14) Previous work has shown that the prevalence of these medications is substantially higher in those living in long-term care settings, but the number of users is higher in those living in the community. Much of the literature on use of medications in this population has been conducted on the long-term care population;(28,29) further work is needed to better understand indications of use and the optimal use of these medications among community-dwelling older Canadians
Our study is subject to limitations that warrant discussion. First, the IQVIA data source only includes aggregate prescription volumes without clinical information such as associated indications (i.e., for BPDS or insomnia, vs. mental health), patient information (i.e., age, sex), or location of dispensation (i.e., long-term care or community), precluding analysis of prescribing appropriateness or the effectiveness of interventions targeted at specific settings. Additionally, the sampling error of this data source can reach slightly higher levels, although it usually does not exceed 5% to 10% in the vast majority of cases (IQVIA, personal communication, February 12, 2016). Arguably, other antidepressant medications with sedating profiles, including mirtazapine or doxepin, may also be used as alternatives for management of insomnia, but were not included in this study. Lastly, this data source does not contain information from the Canadian territories. Despite these limitations, our study possesses strengths. The data represent drug dispensing volumes from most Canadian jurisdictions, with data extrapolated to represent the entire Canadian population. Furthermore, we are able to capture prescriptions paid for by any means (i.e., public payer, private insurance or cash payment). The data source also provides prescription dispensing data from pharmacies, which ensures that it does not inappropriately include in the estimates those prescriptions recommended by physicians, but not filled. Prescription and unit counts have been shown to be a good estimator of utilization,(14) though we cannot confirm that all prescriptions and units dispensed have been consumed by patients.
CONCLUSION
Regional variation in antipsychotic, benzodiazepine, and trazodone use among older adults in Canada was observed. This study serves as the first step in characterizing these differences, and future work is needed to determine the reasoning for the geographic preference for antipsychotics or benzodiazepines in the east versus west of Canada. These insights will help inform development of region-specific strategies to optimize prescribing of psychotropic medications in the elderly.
ACKNOWLEDGEMENTS
This study was funded by a grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC) Health System Research Fund.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
Dr. Mamdani has received honoraria from Boehringer Ingelheim, Pfizer, Bristol-Myers Squibb, and Bayer. All other authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
REFERENCES
- 1.Maglione M, Maher A, Hu J, et al. Off-label use of atypical antipsychotics: an update. Rockville, MD: Agency for Healthcare Research & Quality; 2011. [PubMed] [Google Scholar]
- 2.Marketed Health Products Directorate. Risperidone—restriction of the dementia indication [Internet] Ottawa, ON: Health Canada; 2015. Available from: http://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2015/43797a-eng.php. [Google Scholar]
- 3.Ballard C, Creese B, Corbett A, et al. Atypical antipsychotics for the treatment of behavioral and psychological symptoms in dementia, with a particular focus on longer term outcomes and mortality. Expert Opin Drug Saf. 2011;10(1):35–43. doi: 10.1517/14740338.2010.506711. [DOI] [PubMed] [Google Scholar]
- 4.Madhusoodanan S, Bogunovic O. Safety of benzodiazepines in the geriatric population. Expert Opin Drug Saf. 2004;3(5):485–93. doi: 10.1517/14740338.3.5.485. [DOI] [PubMed] [Google Scholar]
- 5.Mendelson W. A review of the evidence for the efficacy and safety of trazodone in insomnia. J Clin Psychiatry. 2005;66(4):469–76. doi: 10.4088/JCP.v66n0409. [DOI] [PubMed] [Google Scholar]
- 6.O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–18. doi: 10.1093/ageing/afu145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46. doi: 10.1111/jgs.13702. [DOI] [PubMed] [Google Scholar]
- 8.Glass J, Lanctot K, Hermann N, et al. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. 2005;331(7526):1169. doi: 10.1136/bmj.38623.768588.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buffett-Jerrott S, Steward S. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45–58. doi: 10.2174/1381612023396654. [DOI] [PubMed] [Google Scholar]
- 10.Cumming R, Le Couteur D. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs. 2003;17(11):825–37. doi: 10.2165/00023210-200317110-00004. [DOI] [PubMed] [Google Scholar]
- 11.Teri L, Logsdon R, Peskind E, et al. Treatment of agitation in AD: a randomized, placebo-controlled clinical trial. Neurology. 2000;55(9):1271–78. doi: 10.1212/WNL.55.9.1271. [DOI] [PubMed] [Google Scholar]
- 12.Sultzer D, Gray K, Gunay I, et al. Does behavioral improvement with haloperidol or trazodone treatment depend on psychosis or mood symptoms in patients with dementia? J Am Geriatr Soc. 2001;49(10):1294–300. doi: 10.1046/j.1532-5415.2001.49256.x. [DOI] [PubMed] [Google Scholar]
- 13.Camargos E, Louzada L, Quintas J, et al. Trazodone improves sleep parameters in Alzheimer disease patients: a randomized, double-blind, and placebo-controlled study. Am J Geriatr Psychiatry. 2014;22(12):1565–74. doi: 10.1016/j.jagp.2013.12.174. [DOI] [PubMed] [Google Scholar]
- 14.Ontario Drug Policy Research Network. Antipsychotic use in the elderly—final consolidated report. Toronto, ON: The Network; 2015. [Google Scholar]
- 15.Mast G, Fernandes K, Tadrous M, et al. Persistence of antipsychotic treatment in elderly dementia patients: a retrospective, population-based cohort study. Drugs—Real World Outcomes. 2016;3(2):175–82. doi: 10.1007/s40801-016-0073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.BlueCross BlueShield of Illinois. National initiative examines antipsychotic drug use in the elderly [Internet] Chicago, IL: BCBSIL; 2014. Available from: https://www.bcbsil.com/pdf/pharmacy/medicare_part_d/pharmacy_updates_august_2014.pdf. [Google Scholar]
- 17.Power C, McCarthy B, Lawlor BA, Carton L, et al. Antipsychotic prescribing practices amongst the elderly of St. James’s hospital (SJH), Dublin. Eur Psychiatry. 2017;41( Suppl):S663. doi: 10.1016/j.eurpsy.2017.01.1123. [DOI] [Google Scholar]
- 18.Choosing Wisely Canada Consortium. Five things physicians and patients should question [Internet] Toronto, ON: Choosing Wisely Canada; 2017. Available from: https://choosingwiselycanada.org/geriatrics/ [Google Scholar]
- 19.Statistics Canada. Table 051-0001: estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual (persons unless otherwise noted) Ottawa, ON: Stats Canada; 2017. Retrieved from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501. [Google Scholar]
- 20.SAS Institute Inc. SAS University Edition. Cary, NC: SAS Institute Inc; 2016. [Google Scholar]
- 21.Sketris I, Langille Ingram E, Lummis H. Optimal prescribing and medication use in Canada: challenges and opportunities [Internet] Ottawa, ON: Health Council of Canada; 2007. Available from: http://publications.gc.ca/collections/collection_2007/hcc-ccs/H174-6-2007E.pdf. [Google Scholar]
- 22.British Columbia Ministry of Health. A review of the use of antispychotic drugs in British Columbia residential care facilities. Vancouver, BC: Ministry of Health; 2011. [Google Scholar]
- 23.Alberta Health Services. Strategic Clinical Networks appropriate use of antipsychotic medication in long term care [Internet] Edmonton, AB: Alberta Health Services; 2013. Available from: https://www.albertahealthservices.ca/assets/about/scn/ahs-scn-srs-project-aua.pdf. [Google Scholar]
- 24.Alberta Health Services. Medication review of antipsychotic medications [Internet] Edmonton, AB: Alberta Health Services; 2016. Available from: http://www.albertahealthservices.ca/assets/about/scn/ahs-scn-srs-aua-medication-review.pdf. [Google Scholar]
- 25.Canadian Foundation for Healthcare Improvement. Antipsychotic Reduction Collaborative. Reducing antipsychotic medication use in long term care [Internet] 2017. [Accessed 2017 Apr 23]. Available from: http://www.cfhi-fcass.ca/WhatWeDo/reducing-antipsychotic-medication-use-collaborative.
- 26.Desveaux L, Gomes T, Tadrous M, et al. Appropriate prescribing in nursing homes demonstration project (APDP) study protocol: pragmatic, cluster-randomized trial and mixed methods process evaluation of an Ontario policy-maker initiative to improve appropriate prescribing of antipsychotics. Implement Sci. 2016;11:45. doi: 10.1186/s13012-016-0410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Canadian Agency for Drugs and Technology in Health. Narcotics, benzodiazepines, stimulants, and gabapentin: policies, initiatives, and practices across Canada, 2014 [Internet] Ottawa, ON: The Agency; 2014. Available from: https://www.cadth.ca/narcotics-benzodiazepines-stimulants-and-gabapentin-policies-initiatives-and-practices-across-Canada. [Google Scholar]
- 28.Vogel L. Two-thirds of seniors in long-term care take 10 or more drugs: CIHI. CMAJ. 2014;186(9):E309. doi: 10.1503/cmaj.109-4797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Canadian Institute for Health Information (CIHI) Use of antipsychotics among seniors living in long-term care facilities, 2014 [Internet] Ottawa, ON: CIHI; 2016. Available from: https://secure.cihi.ca/free_products/LTC_AiB_v2_19_EN_web.pd. [Google Scholar]