Abstract
Abstinence from alcohol is often considered a critical element of recovery from alcohol use disorder. Yet, low risk drinking may be more desirable for some patients. There is mixed literature on whether low risk drinking is achievable and stable. Low risk drinking outcomes during treatment and outcomes three years following treatment were examined using data from the outpatient arm in Project MATCH (n=877). Drinking outcomes were defined by repeated measures latent class analysis of weekly abstinence, low risk drinking days (<4/5 drinks for women/men), and heavy drinking days (≥4/5 drinks for women/men) during 12 weeks of treatment. Functioning outcome measures included psychosocial functioning, alcohol use, and alcohol-related consequences. Mixture modeling was used to examine the association between drinking classes and functioning outcomes. We identified seven classes based on drinking during treatment: persistent heavy drinking, abstinence to heavy drinking, abstinence and heavy drinking, heavy drinking to mostly abstinent, low risk and heavy drinking, abstinence and low risk drinking, and abstinence. As compared to heavier drinkers, individuals who achieved mostly abstinence or low risk drinking, even with some heavy drinking episodes during treatment, had significant improvements in alcohol use, alcohol-related consequences, and psychosocial functioning three years following treatment. Those who were mostly abstinent or engaged in low risk drinking during treatment did not differ on any outcomes at three years following treatment. Findings indicate that low risk drinking is achievable for some individuals during treatment and that improvement in functioning among low risk drinkers can be observed at three years following treatment.
Keywords: alcohol use disorder, alcohol treatment, recovery, mixture models, low risk drinking
Introduction
Abstinence from alcohol is often considered a critical element of recovery from alcohol use disorder (AUD; Betty Ford Institute Consensus Panel, 2007; Substance Abuse and Mental Health Services Adminitsration (SAMHSA), 2011). Yet, the majority of individuals with AUD do not seek treatment (Hasin, Stinson, Ogburn, & Grant, 2007), largely because they do not want to stop drinking (SAMHSA, 2013). Treatment options for low risk drinking are available and efficacious (Aubin et al., 2015; Mann, Aubin, & Witkiewitz, 2017; Sobell, Sobell, & Agrawal, 2009; van Amsterdam & van den Brink, 2013; Walters, 2000) and acceptance of low risk drinking goals has increased among alcohol treatment providers (Davis & Rosenberg, 2013). Moreover, low risk drinking outcomes are achievable during treatment (Kline-Simon et al., 2013) and reductions in drinking during treatment are associated with significant improvements in one year functioning (Witkiewitz, Roos, et al., 2017). Yet, there are questions regarding the potential instability of low risk drinking outcomes and whether low risk drinking is associated with longer term positive outcomes (Ilgen, Wilbourne, Moos, & Moos, 2008).
Low Risk Drinking Outcomes and Longer Term Functioning
A few studies have evaluated whether low risk drinking outcomes during and following treatment are associated with longer term (beyond one year) improvements in functioning. Kline-Simon and colleagues (2017) compared individuals who were abstinent, low risk drinkers (defined as no days of drinking more than 5 drinks), or heavy drinkers (defined as 1 or more days of 5+ drinks) and found low risk drinkers were not different from abstainers on numerous indicators of psychosocial functioning at a 9-year follow-up assessment.
Additional studies have examined whether abstinence versus low risk drinking behavior in the years following treatment are associated with longer term functioning. Gual and colleagues (1999, 2009) conducted several analyses of a cohort of 850 patients who received alcohol treatment and were categorized as abstainers (defined as no drinking or drinking fewer than 5 drinks per occasion on fewer than 1 occasion/month), low risk drinkers (defined as drinking fewer than 5 drinks per occasion on more than one occasion per month and fewer than 7 drink days/week), and heavy drinkers (defined as 5 or more drinks per occasion and/or daily drinking). Results indicated that abstainers had better outcomes than heavy drinkers at 5-year (Gual, Lligoña, & Colom, 1999) and 20-year follow-up assessments (Gual, Bravo, Lligoña, & Colom, 2009); however, both abstainers and low risk drinkers had significantly better functioning than heavy drinkers (Gual et al., 1999; Miquel et al., 2017). Maisto and colleagues (Maisto, Clifford, Stout, & Davis, 2006, 2007) examined whether abstainers, low risk drinkers (no occasions of 4/5 drinks for women/men in the year post-treatment), and heavy drinkers (at least one occasion of 4/5 drinks for women/men in the year post-treatment) were significantly different on alcohol use or alcohol-related consequences at 3-years following treatment in the Project MATCH outpatient sample. Results indicated abstainers reported significantly fewer drinking days and drinks per drinking day than moderate and heavy drinkers (Maisto et al., 2006). However, moderate drinkers did not differ from abstainers on consequences (Maisto et al., 2007).
Current Study
Several recent studies have evaluated long-term functioning outcomes among individuals classified as low risk drinkers following treatment, yet there have been two primary limitations of this prior work. First, prior studies have used varying time-periods following treatment to characterize low risk drinking, including 6-months following treatment intake (Kline-Simon et al., 2013; Kline-Simon, Litten, Weisner, & Falk, 2017), up to 12-months following treatment intake (Maisto et al., 2006, 2007), and up to 5 years following treatment (Gual et al., 2009, 1999). Thus, these prior studies have not considered low risk drinking during the course of the treatment episode. Studying low risk drinking patterns during the course of the treatment episode is important to inform future clinical decision making regarding the likelihood of long term outcomes. Second, prior studies have relied on categorization of low risk and heavy drinking using a 5 drink cutoff for heavy drinking (or 4 drinks for women in Maisto et al., 2006, 2007). Specifically, the prior studies created groups based on never exceeding the 5 (or 4) drink cutoff on a single occasion. However, this single drinking event cutoff for “success or failure” lacks validity (Pearson, Kirouac, & Witkiewitz, 2016) and is not a good cutoff for delineating functioning following treatment (Wilson, Bravo, Pearson, & Witkiewitz, 2016).
Recent work used an empirical approach to deriving subgroups of individuals based on probability of endorsing abstinence, low risk drinking (less than 4/5 drinks for women/men), and heavy drinking (4/5 or more drinks for women/men) (Witkiewitz, Pearson, et al., 2017; Witkiewitz, Roos, et al., 2017). This approach allows for exceeding the cutoff on some occasions and still provides guidance about overall patterns of drinking over time. Yet, this prior work did not address the question of whether those who achieve low risk drinking during treatment can maintain functional improvements for multiple years following treatment, which is important given concerns that low risk drinking may be a less stable outcome (Ilgen et al., 2008). The goals of the current paper were to address limitations of prior work by examining the association between empirically derived patterns of abstinence, low risk drinking, and heavy drinking during the treatment episode and outcomes at three years following treatment.
Method
Participants and Procedure
The current study was a secondary data analysis of the outpatient arm of Project MATCH (Project MATCH Research Group, 1997), a randomized clinical trial of three psychosocial treatments for AUD: Cognitive Behavioral Therapy (CBT; Kadden et al., 1995), Motivational Enhancement Therapy (MET; Miller, Zweben, DiClemente, & Rychtarik, 1994), and Twelve-Step Facilitation (TSF; Nowinski, Baker, & Carroll, 1995). Participants (n=952), who met criteria for DSM-III-R alcohol abuse (4.6%) or alcohol dependence (95.4%), were recruited from nine research centers in the United States and included individuals who were actively drinking during the 3 months prior to study enrollment and who were seeking outpatient treatment. Of the 952 patients in the outpatient sample, 889 patients (93.4%) had any drinking data available during the treatment period and were included in the present analyses of drinking patterns during treatment. The three year follow-up (36 months post-treatment) was completed by 806 participants (87.1% of the outpatient sample). Among the outpatient sample included in the current study, 28.5% were female, 20.0% were non-White, and mean age was 38.9 (SD = 10.6). Follow-up measures included in the current study were assessed at 36 months post-treatment (see Table 1). There were no differences between those with available data at 36 months and those who did not complete the 36 month follow-up assessment on any baseline characteristics.
Table 1.
Descriptives for Functioning Measures at Baseline (n = 952) and 36-Month Follow-up (n = 806)
| Continuous Measures | Baseline Mean (SD) |
36-Month Follow-up Mean (SD) |
|---|---|---|
| Percent drinking days | 65.22% (30.18%) | 30.82% (35.49%) |
| Percent heavy drinking days | 58.05% (30.7%) | 20.00% (29.91%) |
| Drinks per drinking day | 13.49 (7.99) | 4.62 (5.38) |
| Drinker Inventory of Consequences | 47.17 (22.09) | 33.36 (25.19) |
| PFI Social Behavior Score | 3.22 (0.50) | 3.43 (0.47) |
| PFI Social Role Performance Score | 3.52 (0.78) | 2.96 (0.78) |
Note. PFI = Psychosocial Functioning Inventory.
Measures
Alcohol consumption
Alcohol use was measured using the Form-90 (Miller, 1996), a calendar-based method to obtain daily-level reports of alcohol use in the previous 90-day period. Weekly drinking data were used to create indicators for the repeated measures latent class analysis: abstinent (no drinking during a given week); low risk drinking (1 or more days of consuming alcohol and no heavy drinking days during a given week); and heavy drinking (at least 1 day with 4/5 or more drinks during a given week)1. The three year post-treatment summary alcohol use variables included percent heavy (4/5 drinks in a day for women/men) drinking days (PHDD), percent drinking days (PDD), and drinks per drinking day (DDD).
Alcohol-related negative consequences
The Drinker Inventory of Consequences (DrInC; Miller, Tonigan, & Longabaugh, 1995) was used to measure alcohol-related negative consequences at 3-years post-treatment. Clients reported on a 4-point scale (1 = never, 4 = daily or almost daily) the frequency of 45 alcohol-related consequences. Internal consistency of the DrInC in this sample was α = 0.97 at the three year post-treatment follow-up.
Psychosocial functioning
The Psychosocial Functioning Inventory (PFI; Feragne, Longabaugh, & Stevenson, 1983) was used to measure social functioning at three years post-treatment. The social behavior subscale includes 10 items that assess the frequency of problematic social behavior and social interactions in the past 30 days (e.g., “Did you avoid talking with family members or friends?”, scored 1=almost daily to 4=not at all). The social role subscale includes four items assessing social roles (e.g., “As a friend, how well have you been doing this past month?”, scored 1=very poorly to 5=very good) and one item assessing leisure activities over the past 30 days (“Did you feel satisfied with leisure, social, or recreational activities?). Higher scores on the PFI indicate better psychosocial functioning. Internal consistencies of the social behavior and social role subscales exceeded α = 0.83.
Analytic Approach
Repeated measures latent class analysis (RMLCA; Collins & Lanza, 2009) was used to identify patterns of drinking across 12 weeks of treatment, as described elsewhere (Witkiewitz, Roos, et al., 2017). RMLCA is a latent variable mixture model in which the indicators of the latent class are repeated measures. After the classes of drinking during treatment were identified, we examined mean differences in three year functioning by latent class membership using a Wald chi-square test via a distal outcomes analysis (the "BCH" method; Asparouhov & Muthén, 2014; Bolck, Croon, & Hagenaars, 2004). Comparisons between classes derived from the RMLCA on 3-year post-treatment outcomes were examined for PDD, PHDD, DDD, DrInC total score, PFI social behavior subscale, and PFI social role subscale.
All statistical analyses were conducted in Mplus version 8 ( Muthén & Muthén, 2017). Parameters were estimated using a weighted maximum likelihood function, and all standard errors were computed using a sandwich estimator (i.e., MLR in Mplus; B. O. Muthén & Satorra, 1995). The robust maximum likelihood estimator provides the estimated variance-covariance matrix for the available outcome data and, therefore, all available drinking data during treatment were included in the models. Model fit was examined using the Lo Mendell Rubin Likelihood Ratio test (LRT), the Bootstrapped Likelihood Ratio Test (BLRT), Bayesian Information Criterion (BIC) and sample-size–adjusted BIC (aBIC). A significant LRT and BLRT indicates a significantly better fit for a k profile model (e.g., 3 profiles) versus a k-1 profile model (e.g., 2 profiles), and a non-significant LRT and BLRT indicates that adding an additional profile does not significantly improve model fit (Nylund, Asparouhov, & Muthen, 2007). In addition, lower BIC and aBIC indicates a better fitting model (Nylund et al., 2007) and the smallest class of any class-solution should not contain less than 5% of the sample (Nagin, 2005). Classification precision (defined by relative entropy) was used to evaluate how well the final latent profile solution classified individuals into latent classes and values of entropy greater than .80 were considered good classification precision (Nylund et al., 2007).
Results
Repeated Measures Latent Class Models of Weekly Drinking During Treatment
Repeated measures latent class models with 2 to 10 classes were estimated, and a 7-class model was retained as the optimal solution with excellent entropy (entropy = .915) in the current sample (Table 2). We selected the 7-class model because its fit was better than a 6-class model based on the aBIC and BLRT, and because a 7-class solution has previously been validated (Witkiewitz, Pearson, et al., 2017; Witkiewitz, Roos, et al., 2017). In addition, the 8-, 9-, and 10-class models had multiple classes with class sizes that were small (5% of the sample or less).
Table 2.
Model Fit Statistics for Repeated Measures Latent Class Models of Weekly Drinking During Treatment
| Class Solution | Entropy | Likelihood (k) | BIC | aBIC | LRT | BLRT |
|---|---|---|---|---|---|---|
| 2 Class | 0.96 | −7461.15 (49) | 15255.01 | 15099.39 | 4613.69** | 4644.57** |
| 3 Class | 0.96 | −6568.80 (74) | 13640.06 | 13405.05 | 1774.25** | 1784.70** |
| 4 Class | 0.93 | −6245.29 (99) | 13162.80 | 12848.40 | 643.22** | 647.01** |
| 5 Class | 0.91 | −6099.39 (124) | 13040.75 | 12646.95 | 290.09 | 291.80** |
| 6 Class | 0.91 | −5963.65 (149) | 12939.03 | 12465.84 | 269.89 | 271.48** |
| 7 Class | 0.92 | −5885.25 (174) | 12951.98 | 12399.39 | 155.88 | 156.80** |
| 8 Class | 0.91 | −5819.18 (199) | 12989.59 | 12357.60 | 131.38 | 132.15** |
| 9 Class | 0.92 | −5772.97 (224) | 13066.92 | 12355.53 | 91.88 | 92.42** |
| 10 Class | 0.92 | −5728.04 (249) | 13146.81 | 12356.03 | 88.15 | 88.67** |
Note.
p < 0.001; k = number of parameters; BIC = Bayesian Information Criteria; aBIC = sample size adjusted BIC; LRT = Lo Mendell Rubin Likelihood Ratio Test; BLRT = Bootstrapped Likelihood Ratio Test.
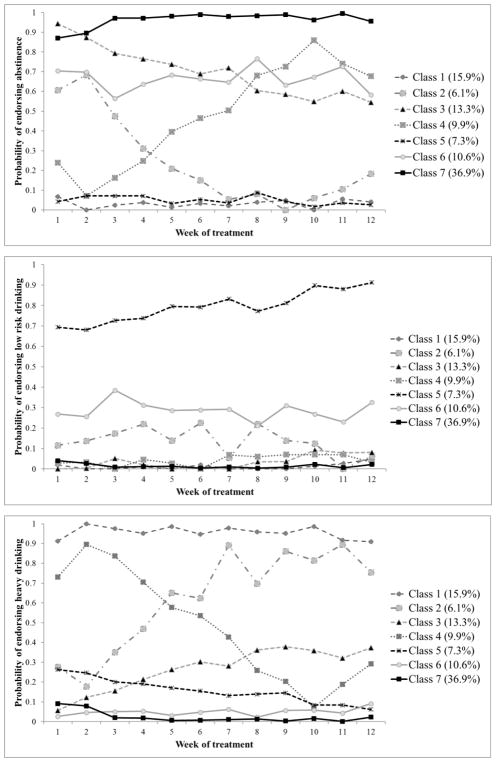
The class prevalence and individual item probabilities (Figure 1) of the 7-class model selected in the current sample were similar to previous findings (Witkiewitz, Roos, et al., 2017). Class 1 (15.9% of the sample), “persistent heavy drinking”, reported a high probability of heavy drinking during all weeks of treatment with average percent heavy drinking days (PHDD) over the course of treatment of 52.2% (SD=28.4%). Class 2 (6.1% of the sample), “abstinence to heavy drinking”, reported abstinence initially and a higher probability of heavy drinking by the end of treatment with average PHDD over the course of treatment of 8.6% (SD=8.8%). Class 3 (13.3% of the sample), “abstinence and heavy drinking”, reported a mix of heavy drinking and abstinence across the treatment period with average PHDD over the course of treatment of 24.8% (SD=20.5%). Class 4 (9.9% of the sample), “heavy drinking to mostly abstinent”, reported heavy drinking initially and a higher probability of abstinence by the end of treatment with average PHDD over the course of treatment of 19.9% (SD=14.7%). Class 5 (7.3% of the sample), “low risk and heavy drinking”, reported low risk drinking with some heavy drinking throughout treatment and average PHDD over the course of treatment of 5.1% (SD=8.3%). Class 6 (10.6% of the sample), “abstinence and low risk drinking”, reported a mix of low risk drinking and abstinence with average PHDD over the course of treatment of 0.9% (SD=1.8%). Class 7 (36.9% of the sample), “abstainers”, reported a high probability of abstinence throughout the entire treatment period with average PHDD over the course of treatment of 0.8% (SD=2.1%).
Figure 1. Response Probabilities for Levels of Drinking (abstinence, low risk drinking, and heavy drinking) across Weeks of Treatment by Class.
The y-axes indicate the probability of endorsing a particular level of drinking, the x-axes indicate week of treatment, and the lines represent response probabilities for each latent class. Latent class proportions are provided in the Figure 1 legend. Class 1=persistent heavy drinking, Class 2=abstinence to heavy drinking, Class 3=abstinence and heavy drinking, Class 4=heavy drinking to mostly abstinent, Class 5=low risk and heavy drinking, Class 6=abstinence and low risk drinking, and Class 7=abstinence.
Demographics, baseline dependence severity (as measured by the Alcohol Dependence Scale (Skinner & Horn, 1984)), and treatment condition by latent classes are presented in Table 3. Individuals in the low risk drinking classes (Classes 5 and 6) had lower dependence severity than those in the mixed heavy drinking classes (Classes 2 and 4). Individuals who received MET were more likely to be in the heavy and low risk drinking classes (Classes 3 and 5) and those who received CBT were less likely to be in the abstinent and heavy drinking class (Class 3).
Table 3.
Descriptives for Demographics, Dependence Severity, and Treatment Condition by Latent Classes
| Class | Male N (%) | Age | ADS | CBT N (%) | MET N (%) | TSF N (%) |
|---|---|---|---|---|---|---|
| Class 1: Persistent heavy drinking | 99 (69.2%) | 37.9 (11.2) | 14.7 (6.2) | 40 (28.0%)3 | 51 (35.7%) 3,5 | 52 (36.4%) |
| Class 2: Abstinence to heavy drinking | 89 (78.1%) | 36.0 (8.9) 5,7 | 16.5 (8.0) 5,6 | 38 (33.3%) 3 | 40 (35.1%) 3,5 | 36 (31.6%) |
| Class 3: Abstinence and heavy drinking | 38 (73.1%) | 38.4 (9.9) | 15.2 (7.3) | 10 (19.2%)1,2,4,5,6,7 | 30 (57.7%) 1,2,4,6,7 | 12 (23.1%) |
| Class 4: Heavy drinking to abstinent | 60 (68.2%) | 38.9 (9.7) | 16.4 (8.2) 5,6 | 30 (34.1%) 3 | 24 (27.3%) 3,5 | 34 (38.6%) |
| Class 5: Low risk and heavy drinking | 44 (68.8%) | 41.9 (11.0) 2 | 12.0 (6.2) 2,4 | 18 (28.1%) 3 | 31 (48.4%) 1,2,4,6,7 | 15 (23.4%) |
| Class 6: Abstinence and low risk drinking | 69 (74.2%) | 37.8 (9.9) | 12.5 (7.0) 2,4 | 32 (34.4%) 3 | 33 (35.5%) 3,5 | 28 (30.1%) |
| Class 7: Abstainers | 249 (74.3%) | 39.9 (11.4) 2 | 14.8 (7.3) | 114 (34.0%) 3 | 88 (26.3%) 3,5 | 133 (39.7%) |
Note. ADS = Alcohol Dependence Scale; CBT = Cognitive Behavioral Therapy; MET = Motivation Enhancement Therapy; TSF = Twelve Step Facilitation.
In each column, superscript numbers indicate significant differences between latent classes on means and proportions based on χ2 tests for binary variables and Tukey post hoc comparisons for continuous variables.
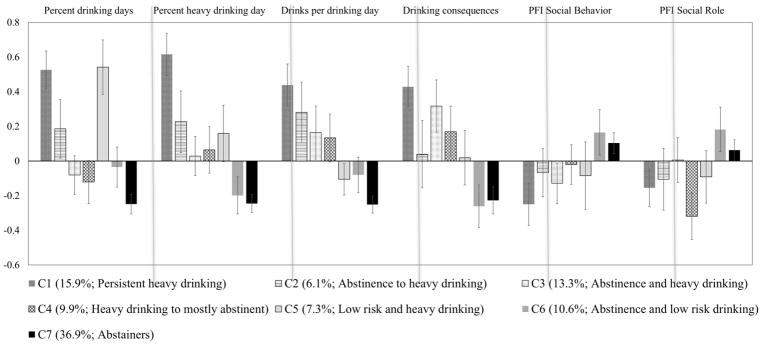
Distal Outcome Analysis of Functioning at 3-Years Post-Treatment
Results from the distal outcome analyses are presented in Table 4, with the observed means and standard errors (SE) of all outcomes, and Figure 2, with standardized scale scores (each outcome has a mean=0 and SD=1) by latent class. As seen in Table 4, abstainers and low risk drinkers (Class 6 and 7) were distinguished from the other five classes on most outcomes. Individuals with low risk and some heavy drinking (Class 5) also reported fewer drinks per drinking days and drinking consequences than the heavier drinking classes (Classes 1, 3), but did not differ on psychosocial functioning. Individuals in the abstinence and low risk drinking class (Class 6) were not significantly different from abstainers (Class 7) on any outcomes.
Table 4.
Distal Outcome Analysis of Continuous Outcomes at Three Years following Treatment by Latent Classes
| Class | Percent drinking days | Percent heavy drinking day | Drinks per drinking day | Drinking consequences | PFI Social Behavior | PFI Social Role Performance |
|---|---|---|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |
| Class 1: Persistent heavy drinking | 49.5% (3.85) 3,4,6,7 | 38.4% (3.65) 3,4,5,6,7 | 6.98 (0.66) 5,6,7 | 44.16 (2.94) 5,6,7 | 3.32 (0.06) 6,7 | 2.84 (0.09) 6 |
| Class 2: Abstinence to heavy drinking | 37.4% (5.99) 7 | 26.8% (5.33) 6,7 | 5.51 (0.94) 7 | 34.38 (4.92) | 3.40 (0.07) | 2.88 (0.14) |
| Class 3: Abstinence and heavy drinking | 27.9% (3.98) 1,5 | 20.9% (3.38) 1,7 | 6.14 (0.83) 5,7 | 41.37 (3.80) 6,7 | 3.38 (0.07) | 2.97 (0.10) |
| Class 4: Heavy drinking to mostly abstinent | 26.5% (4.39) 1,5 | 21.9% (4.04) 1,7 | 5.34 (0.74) 7 | 37.65 (3.71) 6,7 | 3.43 (0.05) | 2.71 (0.11) 6,7 |
| Class 5: Low risk and heavy drinking | 50.1% (5.58) 3,4,6,7 | 24.8% (4.88) 1,7 | 4.06 (0.49) 1,3 | 33.86 (3.95) 1 | 3.39 (0.09) | 2.89 (0.12) |
| Class 6: Abstinence and low risk drinking | 29.6% (4.13) 1,5 | 14.1% (3.20) 1,2 | 4.20 (0.55) 1 | 26.80 (3.10) 1,3,4 | 3.51 (0.06) 1 | 3.11 (0.10) 1,4 |
| Class 7: Abstainers | 22.0% (2.01) 1,2,5 | 12.6% (1.53) 1,2,3,4,5 | 3.27 (0.27) 1,2,3,4 | 27.65 (1.96) 1,3,4 | 3.48 (0.03) 1 | 3.01 (0.05) 4 |
| Sample average (SD) | 30.8% (35.4%) | 20.0% (25.9%) | 4.62 (5.58) | 32.36 (25.19) | 3.43 (0.47) | 2.96 (0.78) |
Note.
In each column, superscript numbers indicate significant differences between latent classes on mean outcomes (p < 0.05) based on Wald chi-square tests. SE = standard error; SD = standard deviation.
Figure 2. Standardized Mean Scores (Mean=0, SD=1) with Standard Errors of Estimates from the Distal Outcome Analysis for Three Year Outcome Measures by Latent Class (C).
Discussion
The current study replicated and extended recent work (Kline-Simon et al., 2013; Witkiewitz, Roos, et al., 2017) by showing that low risk drinking is achievable by a subset of patients and that low risk drinkers and abstainers do not differ on a wide variety of outcomes at three years following treatment. This is important given that individuals in the low risk and abstainer classes did have some occasions of heavy drinking during treatment but had significantly better outcomes than those individuals with more occasions of heavy drinking.
Current findings highlight clinically important nuances in heavy drinking during treatment. Contrary to previous methodologies that characterized all participants with any heavy drinking into one category (i.e., treatment “failures”), the findings from the current study indicate that the overall pattern of drinking is potentially more important than never exceeding an arbitrary cutoff. Individuals who were mostly abstinent, even with occasions of heavier drinking (Class 6 and 7), had the best outcomes. Individuals who engaged in persistent heavy drinking (Class 1) had worse outcomes than all other classes, including those classes with other patterns of heavy drinking. Thus, it may be important for clinicians to assess for patterns of drinking and to encourage at least some abstinent days, even among those clients with low risk drinking goals. Simultaneously, it is important to consider medical safety of abstinence to avoid potential alcohol withdrawal effects (Mirijello et al., 2015). Those individuals who are unable to achieve any abstinent or low risk drinking days may require a higher level of care.
In prior analyses, there were no differences between the low risk drinking classes (Class 5 and 6) in drinking or psychosocial functioning in the year following treatment (Witkiewitz, Roos, et al., 2017). However, the current study showed that Class 6 had better drinking outcomes at three years following treatment than Class 5. Individuals with expected membership in Class 5 (low risk and heavy drinking) had a low probability of abstinence days during treatment, whereas individuals in Class 6 (abstinence and low risk drinking) had a higher probability of abstinence days throughout treatment. Some days of abstinence during treatment may be important for longer term functioning among those engaging in low risk drinking during treatment. Those with greater dependence severity were unlikely to be classified as low risk drinkers during treatment and clinicians may consider assessing dependence severity in developing intervention strategies and collaborating with patients regarding the selection of abstinence or low risk drinking goals.
Limitations and Future Directions
The current study was a secondary data analysis and was limited by the measures assessed in the original Project MATCH study. Most notably, there were no measures of drinking goals and all of the Project MATCH treatments were delivered under the assumption of an abstinence goal. It is unclear whether the same patterns of drinking would be found among clients with low risk drinking goals. Correspondence between an individual’s drinking goal and the approach of the treatment program can affect long term outcome, so this is an important limitation (Berglund, Svensson, Berggren, Balldin, & Fahlke, 2016). Further, the aftercare sample, which was more severe at baseline was not followed for the three year follow-up assessment. It is also important to note that Project MATCH included individuals who met DSM-III-R criteria for alcohol abuse (4.6%) or dependence (95.4%), and it is unclear whether the small proportion of individuals with alcohol abuse would meet DSM-5 criteria for AUD. Finally, the measure of psychosocial functioning was not specific to alcohol use and only captured social behavior and roles.
Results from this study support the need for a broader conceptualization of the clinical course of AUD (Maisto, Witkiewitz, Moskal, & Wilson, 2016) that does not rely solely on binary cutoffs to determine treatment success (e.g., abstinence). Research is needed to explore time-varying predictors of low risk drinking and alternative definitions of reduction outcomes (e.g., World Health Organization risk levels; Witkiewitz, Hallgren, et al., 2017) that may promote beneficial longer term functioning. Such findings would aid in refining AUD treatment and would provide more information for clinicians to improve clinical decision-making.
Acknowledgments
Author Note. Preparation of this manuscript was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism (R01 AA022328, R01 AA025539, K05 AA016928, K01 AA024796, and T32 AA018108). The current findings were disseminated, in part, via a symposium presentation at the 41st Annual Meeting of the Research Society on Alcoholism in June 2018. Katie Witkiewitz, Department of Psychology, University of New Mexico; Megan Kirouac, Department of Psychology, University of New Mexico; Corey R. Roos, Department of Psychology, University of New Mexico; Adam D. Wilson, Department of Psychology, University of New Mexico; Kevin A. Hallgren, Department of Psychiatry and Behavioral Sciences, University of Washington; Adrian J. Bravo, Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico; Kevin S. Montes, Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico; Stephen A. Maisto, Department of Psychology, Syracuse University.
Footnotes
We also examined low risk drinking definitions using weekly limits of 7 and 14 drinks for women and men, respectively. Fewer than 2.5% of participants exceeded weekly limits and did not exceed daily limits. Results were not substantively changed when weekly limits were analyzed, thus we report the results using daily limits.
Contributor Information
Katie Witkiewitz, University of New Mexico.
Megan Kirouac, University of New Mexico.
Corey R. Roos, University of New Mexico
Adam D. Wilson, University of New Mexico
Kevin A. Hallgren, University of Washington
Adrian J. Bravo, University of New Mexico
Kevin S. Montes, University of New Mexico
Stephen A. Maisto, Syracuse University
References
- Asparouhov T, Muthén BO. Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary second model. 2014. Mplus Web Notes No. 21. [Google Scholar]
- Aubin HJ, Reimer J, Nutt DJ, Bladström A, Torup L, François C, Chick J. Clinical relevance of as-needed treatment with nalmefene in alcohol-dependent patients. European Addiction Research. 2015;21(3):160–8. doi: 10.1159/000371547. [DOI] [PubMed] [Google Scholar]
- Berglund KJ, Svensson I, Berggren U, Balldin J, Fahlke C. Is There a Need for Congruent Treatment Goals Between Alcohol-Dependent Patients and Caregivers? Alcoholism: Clinical and Experimental Research. 2016;40(4):874–879. doi: 10.1111/acer.13003. [DOI] [PubMed] [Google Scholar]
- Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. Journal of Substance Abuse Treatment. 2007;33(3):221–228. doi: 10.1016/j.jsat.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Bolck A, Croon M, Hagenaars JA. Estimating latent structure models with categorical variables: One-step versus three-step estimators. Political Analysis. 2004;12(1):3–27. doi: 10.1093/pan/mph001. [DOI] [Google Scholar]
- Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences. New York, NY: Wiley; 2009. [Google Scholar]
- Davis AK, Rosenberg H. Acceptance of Non-Abstinence Goals by Addiction Professionals in the United States. Psychology of Addictive Behaviors. 2013;27(4):1102–1109. doi: 10.1037/a0030563. [DOI] [PubMed] [Google Scholar]
- Feragne MA, Longabaugh R, Stevenson JF. The Psychosocial Functioning Inventory. Evaluation & the Health Professions. 1983;6(1):25–48. doi: 10.1177/016327878300600102. [DOI] [PubMed] [Google Scholar]
- Gual A, Bravo F, Lligona A, Colom J. Treatment for Alcohol Dependence in Catalonia: Health Outcomes and Stability of Drinking Patterns over 20 Years in 850 Patients. Alcohol and Alcoholism. 2009;44(4):409–415. doi: 10.1093/alcalc/agp032. [DOI] [PubMed] [Google Scholar]
- Gual A, Lligoña A, Colom J. Five-year outcome in alcohol dependence. A naturalistic study of 850 patients in Catalonia. Alcohol and Alcoholism. 1999;34(2):183–92. doi: 10.1093/alcalc/34.2.183. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10344779. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64(7):830–42. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Wilbourne PL, Moos BS, Moos RH. Problem-free drinking over 16 years among individuals with alcohol use disorders. Drug and Alcohol Dependence. 2008;92(1–3):116–122. doi: 10.1016/j.drugalcdep.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden RM, Carroll KM, Donovan DM, Cooney NL, Monti PM, Abrams D, … Hester RK. Cognitive-behavioral coping skills therapy manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. Retrieved from https://pubs.niaaa.nih.gov/publications/MATCHSeries3/ProjectMATCHVol_3.pdf. [Google Scholar]
- Kline-Simon AH, Falk DE, Litten RZ, Mertens JR, Fertig J, Ryan M, Weisner CM. Posttreatment low-risk drinking as a predictor of future drinking and problem outcomes among individuals with alcohol use disorders. Alcoholism, Clinical and Experimental Research. 2013;37(Suppl 1):E373–80. doi: 10.1111/j.1530-0277.2012.01908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline-Simon AH, Litten RZ, Weisner CM, Falk DE. Posttreatment Low-Risk Drinking as a Predictor of Future Drinking and Problem Outcomes Among Individuals with Alcohol Use Disorders: A 9-Year Follow-Up. Alcoholism: Clinical and Experimental Research. 2017;41(3):653–658. doi: 10.1111/acer.13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Drinking in the year after treatment as a predictor of three-year drinking outcomes. Journal of Studies on Alcohol. 2006;67(6):823–32. doi: 10.15288/jsa.2006.67.823. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17060998. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Moderate drinking in the first year after treatment as a predictor of three-year outcomes. Journal of Studies on Alcohol and Drugs. 2007;68(3):419–27. doi: 10.15288/jsad.2007.68.419. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17446982. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Witkiewitz K, Moskal D, Wilson AD. Is the Construct of Relapse Heuristic, and Does It Advance Alcohol Use Disorder Clinical Practice? Journal of Studies on Alcohol and Drugs. 2016;77(6):849–858. doi: 10.15288/jsad.2016.77.849. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27797685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann K, Aubin HJ, Witkiewitz K. Reduced Drinking in Alcohol Dependence Treatment, What Is the Evidence? European Addiction Research. 2017;23(5):219–230. doi: 10.1159/000481348. [DOI] [PubMed] [Google Scholar]
- Miller WR. Form 90: A structured assessment interview for drinking and related behaviors (Project MA) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1996. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC) (Project MA) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivation enhancement therapy manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1994. [Google Scholar]
- Miquel L, Gual A, Vela E, Lligoña A, Bustins M, Colom J, Rehm J. Alcohol Consumption and Inpatient Health Service Utilization in a Cohort of Patients With Alcohol Dependence After 20 Years of Follow-up. Alcohol and Acoholism. 2017;52(2):227–233. doi: 10.1093/alcalc/agw075. [DOI] [PubMed] [Google Scholar]
- Mirijello A, D’Angelo C, Ferrulli A, Vassallo G, Antonelli M, Caputo F, … Addolorato G. Identification and management of alcohol withdrawal syndrome. Drugs. 2015;75(4):353–365. doi: 10.1007/s40265-015-0358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, Satorra A. Complex sample data in structural equation modeling. Sociological Methodology. 1995;25:267–316. [Google Scholar]
- Muthén LK, Muthén BO. Mplus users guide. 8. Los Angeles, CA: Muthén & Muthén; 1998–2017. [Google Scholar]
- Nowinski J, Baker S, Carroll KM. Twelve step facilitation therapy manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- Pearson MR, Kirouac M, Witkiewitz K. Questioning the validity of the 4+/5+ binge or heavy drinking criterion in college and clinical populations. Addiction. 2016;111(10):1720–6. doi: 10.1111/add.13210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58(1):7–29. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8979210. [PubMed] [Google Scholar]
- Skinner HA, Horn JL. Alcohol Dependence Scale (ADS) user’s guide. Toronto: Addiction Research Foundation; 1984. [Google Scholar]
- Sobell LC, Sobell MB, Agrawal S. Randomized controlled trial of a cognitive-behavioral motivational intervention in a group versus individual format for substance use disorders. Psychology of Addictive Behaviors. 2009;23(4):672–83. doi: 10.1037/a0016636. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: 2013. [Google Scholar]
- Substance Abuse and Mental Health Services Adminitsration. SAMHSA working definition of recovery: 10 guiding principles of recovery. Rockville, MD: Department of Health and Human Services; 2011. [Google Scholar]
- van Amsterdam J, van den Brink W. Reduced-risk drinking as a viable treatment goal in problematic alcohol use and alcohol dependence. Journal of Psychopharmacology. 2013;27(11):987–997. doi: 10.1177/0269881113495320. [DOI] [PubMed] [Google Scholar]
- Walters GD. Behavioral self-control training for problem drinkers: A meta-analysis of randomized control studies. Behavior Therapy. 2000;31(1):135–149. doi: 10.1016/S0005-7894(00)80008-8. [DOI] [Google Scholar]
- Wilson AD, Bravo AJ, Pearson MR, Witkiewitz K. Finding success in failure: using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction. 2016;111(12):2145–2154. doi: 10.1111/add.13518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Pearson MR, Hallgren KA, Maisto SA, Roos CR, Kirouac M, … Heather N. Who achieves low risk drinking during alcohol treatment? An analysis of patients in three alcohol clinical trials. Addiction. 2017;112(12):2112–2121. doi: 10.1111/add.13870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Roos CR, Pearson MR, Hallgren KA, Maisto SA, Kirouac M, … Heather N. How much is too much? Patterns of drinking during alcohol treatment and associations with post-treatment outcomes across three alcohol clinical trials. Journal of Studies on Acohol and Drugs. 2017;78(1):59–69. doi: 10.15288/jsad.2017.78.59. [DOI] [PMC free article] [PubMed] [Google Scholar]