Introduction
Despite the recent advances in minimally invasive glaucoma surgery trabeculectomy remains the gold standard surgical technique for glaucoma that is refractory to medical therapy. Following the refinement of the surgical technique good trabeculectomy outcomes with low rates of surgical complications can now be achieved, but intensive proactive postoperative care is often required [1].
Mastering these new techniques requires time and practice, but the number of trabeculectomy operations being performed in the UK is reducing [2], so access to surgical training for trainees is becoming more challenging. Using simulation and wet-lab models to enhance learning is therefore becoming increasingly important. Such models are commonplace in cataract surgery [3] but are limited for glaucoma surgery. Those models previously described include a formalin-prepared pig eye model [4]; however, this requires the sourcing of materials that can potentially be difficult to access and expensive. We therefore propose a new novel wet-lab model that is inexpensive and easily accessible using a green apple, cling film and disposable instruments.
Methods
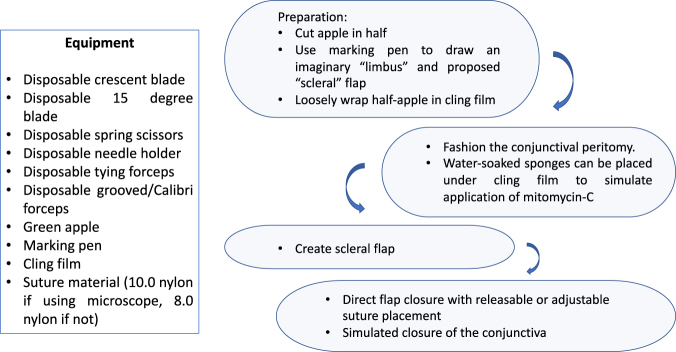
The equipment along with the steps required are detailed in Fig. 1.
Fig. 1.
Equipment and steps required
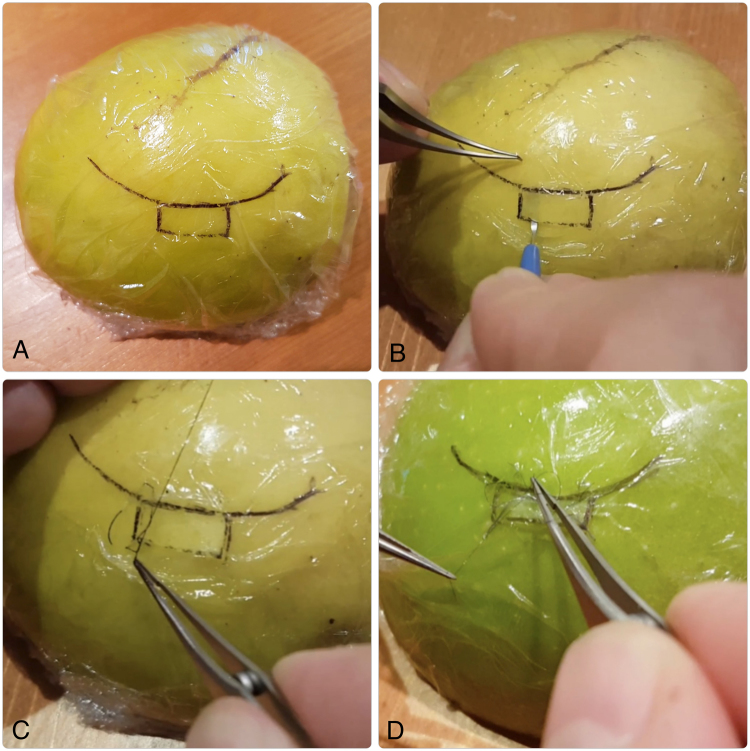
The firm consistency of the skin and cortex of a green apple lends itself to the creation of the scleral flap as the tissue does not easily disintegrate, and when the flap is opened the thickness and uniformity of the flap can be assessed. As the apple surface is curved like an eye the trainee can practice tilting the crescent blade to ensure the curvature is followed when extending sideways (Fig. 2).
Fig. 2.
a Prepared apple model detailing limbal marks and cling-film, b creation of the scleral flap using the crescent blade, c placement of releasable suture, d placement of conjunctival suture
Discussion
The benefits of this model are as follows: it is cost-effective and safe and can be used in both a clinical and non-clinical environment with or without the use of an operating microscope. It is not meant to be an accurate recreation of a human eye and there are models available that are designed to recreate this. The aim of this model is to provide a cheap and easily repeatable platform that any trainee can set-up and use in any situation that can recreate the key steps involved in the surgery.
This model not only allows glaucoma trainees to practice the steps of a trabeculectomy but can also be used as an aid to practice scleral suturing in cases of traumatic scleral or corneal perforations and closing of sclerostomies, in addition to practicing conjunctival suturing and closure with the use of the cling-film. Formative assessments could also potentially be undertaken on suture technique.
Model eyes and simulators are invaluable surgical tools for trainees and senior surgeons learning new techniques. We feel our apple model is a cost-effective tool for surgeons to practice their scleral and conjunctival incisions and suturing. A key aspect of learning a new surgical technique is repeated deliberate practice [5], therefore having a model that is easy to set-up and practice techniques repeatedly leads to an improvement in muscle memory and could potentially shorten the learning curve and importantly maximise the learning potential when starting to perform trabeculectomy surgery on patients.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Kirwan JF, Lockwood AJ, et al. Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology. 2013;120:2532–9. doi: 10.1016/j.ophtha.2013.07.049. [DOI] [PubMed] [Google Scholar]
- 2.Murphy C, Ogston S, Cobb C, MacEwan C. Recent trends in glaucoma surgery in Scotland, England and Wales. Br J Ophthalmol. 2015;99:308–12. doi: 10.1136/bjophthalmol-2013-304465. [DOI] [PubMed] [Google Scholar]
- 3.Thomsen AS, Kilgaard JF, Kjaerbo H, La Cour M, Konge L. Simulation-based certification for cataract surgery. Acta Ophthalmol. 2015;93:416–21. doi: 10.1111/aos.12691. [DOI] [PubMed] [Google Scholar]
- 4.Lee GA, Chiang MYM, Shah P. Pig eye trabeculectomy – a wet-lab teaching model. Eye. 2006;20:32–37. doi: 10.1038/sj.eye.6701784. [DOI] [PubMed] [Google Scholar]
- 5.Kavic MS. Teaching and learning of surgery. J Soc Laparoendosc Surg. 2012;16:341–4. doi: 10.4293/108680812X13427982376103. [DOI] [PMC free article] [PubMed] [Google Scholar]