Case Report
An otherwise fit and healthy 75-year-old man presented with a 2-year history of intermittent dysphagia and odynophagia localized predominantly around the suprasternal notch. His symptoms were most noticeable when he swallowed saliva, although he was able tolerate a fairly normal diet with no holdup or regurgitation. Examination of his oropharynx was normal. Flexible nasendoscopy showed an unremarkable postnasal space, pharynx, and larynx, although there was some evidence of mild post-cricoid edema. Barium swallow suggested the presence of a cricopharyngeal bar with early formation of a pharyngeal pouch. He was commenced on a proton pump inhibitor and antacid for suspected laryngopharyngeal reflux. When this failed to control or improve his symptoms, he underwent upper endoscopy, which ruled out esophageal abnormality. He subsequently underwent injection of botulinum toxin into the cricopharyngeus muscle to treat cricopharyngeal hypertrophy. This provided only limited symptomatic relief. It was noted from the patient’s medical history that he had undergone bilateral tonsillectomy 2 years earlier for an enlarged right tonsil. He reported that his symptoms seemed to have started soon after this. A computed tomography (CT) scan of the neck revealed bilateral elongated styloid processes (Figure 1). This was also demonstrated on his previous barium swallow (Figure 2). The patient underwent bilateral surgical excision of the styloid processes. This was successful in achieving a partial response to his symptoms. He was discharged from our care.
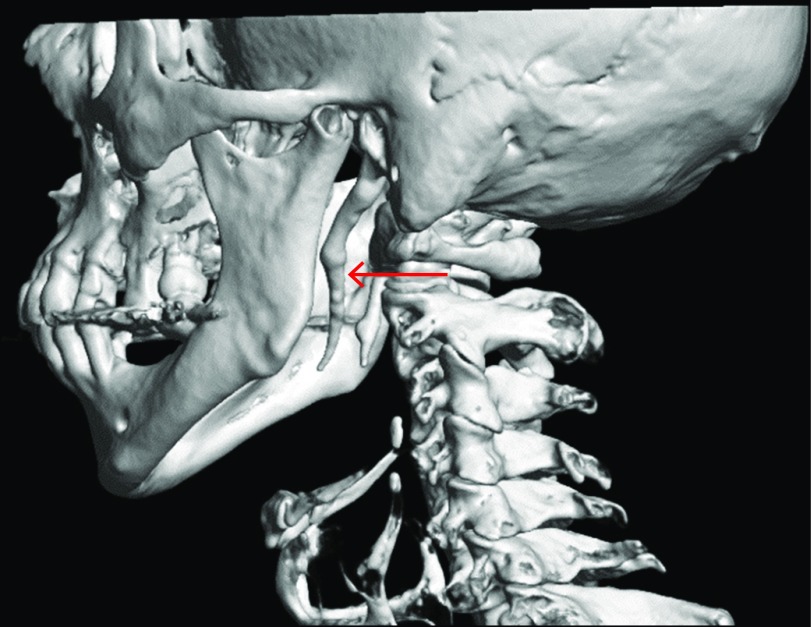
Figure 1.
Three-dimensional reconstruction of multi-detector computed tomography scans showing elongated styloid processes extending down to the level of angle of mandible (arrow).
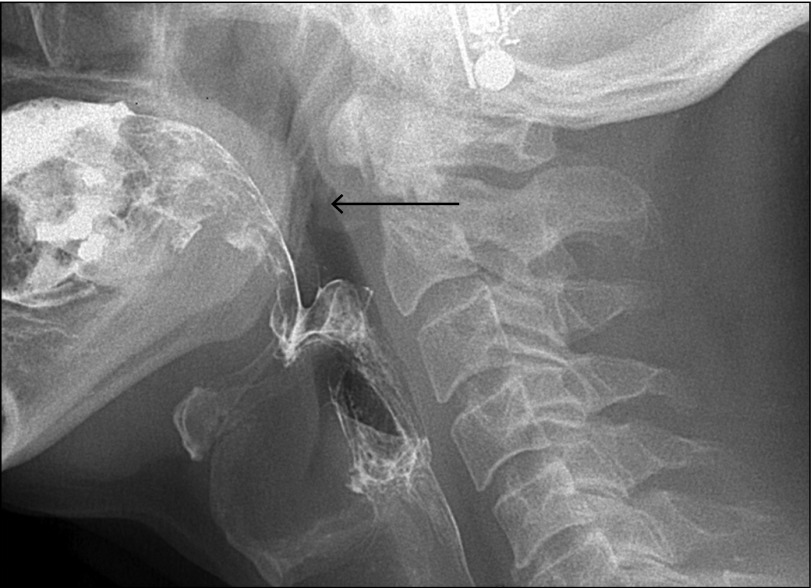
Figure 2.
Lateral fluoroscopy image from a single contrast barium swallow. The elongated styloid processes can just be seen behind the mandibular rami (arrow).
Eagle syndrome, also known as stylohyoid syndrome, refers to a rare and poorly understood complex of symptoms associated with styloid process elongation or stylohyoid ligament calcification.1 First described by American otolaryngologist Watt W. Eagle in 1937, the etiology and pathophysiology of this syndrome remain controversial.2 Although elongated styloid processes are estimated to be present in approximately 4% of the general population, only a small proportion of those (between 4% and 10.3%) become symptomatic.3
Clinically, the syndrome may present with a variety of symptoms, none of which are pathognomonic. The most common features are reported to be throat and neck pain and the sensation of a foreign body in the throat. Less frequent symptoms include referred otalgia, carotidynia, dizziness, and dysphagia.4
The diagnosis is confirmed radiologically. Traditionally, this was achieved with a panoramic radiograph or lateral plain film of the cervical spine. However, plain radiographs are prone to geometric distortion, magnification and superimposition of structures. A CT scan with 3D reconstruction is considered superior. This has the added advantage of allowing for more accurate assessment of the length and spatial orientation of the styloid processes which can be useful in surgical planning as well as in explaining to the patient the nature of the problem.5
Treatment options include conservative management with analgesia and local infiltration of steroids and long-acting local anesthetic agents or surgical excision of the elongated styloid processes (styloidectomy).6
Disclosures
Author contributions: S. Ishaq and GM Jama share first authorship of this manuscript. GM Jama performed the literature review and wrote the manuscript. A. Hall provided the images and edited the manuscript. J. Danino, CJJ Mulder and N. Molony edited the manuscript. S. Ishaq is the article guarantor.
Financial disclosures: None to report.
Informed consent was obtained for this case report.
References
- 1.Badhey A, Jategaonkar A, Anglin Kovacs AJ, et al. Eagle syndrome: A comprehensive review. Clin Neurol Neurosurg. 2017;159:34–8. [DOI] [PubMed] [Google Scholar]
- 2.Eagle WW. Elongated styloid processes: Report of two cases. Arch Otolaryngol. 1937;25(5):584–7. [Google Scholar]
- 3.Rechtweg JS, Wax MK. Eagle's syndrome: A review. Am J Otolaryngol. 1998;19(5):316–21. [DOI] [PubMed] [Google Scholar]
- 4.Zeckler SR, Betancur AG, Yaniv G. The eagle is landing: Eagle syndrome–an important differential diagnosis. Br J Gen Pract. 2012;62(602):501–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nayak DR, Pujary K, Aggarwal M, Punnoose SE, Chaly VA. Role of three-dimensional computed tomography reconstruction in the management of elongated styloid process: A preliminary study. J Laryngol Otol. 2007;121(4):349–53. [DOI] [PubMed] [Google Scholar]
- 6.Piagkou M, Anagnostopoulou S, Kouladouros K, Piagkos G. Eagle's syndrome: A review of the literature. Clin Anat. 2009;22(5):545–58. [DOI] [PubMed] [Google Scholar]