Abstract
Boerhaave syndrome refers to a spontaneous perforation of the esophagus that results from severe straining or vomiting. This uncommon situation may lead to serious outcome with chemical mediastinitis, and is associated with high morbidity and mortality. Surgery, although associated with high morbidity and mortality remains the treatment of choice, whereas endoscopic management with stent placement is preserved to treat inoperable patients. Removal of the stent is generally recommended after 4-6 weeks. We report a case of an elderly patient who presented with a large complicated Boerhaave's mid-esophageal perforation, with a complete recovery after a 3-month treatment with a long esophageal stent.
Keywords: Boerhaave syndrome, Esophageal rupture, Esophageal stent
1. Introduction
Boerhaave syndrome refers to a spontaneous perforation of the esophagus that results from severe straining or vomiting. This uncommon situation may lead to serious outcome with chemical mediastinitis, and is associated with high morbidity and mortality. Surgery, although associated with high morbidity and mortality remains the treatment of choice, whereas endoscopic management with stent placement is preserved to treat inoperable patients. Removal of the stent is generally recommended after 4-6 weeks [1], [2].
We report a case of an elderly patient who presented with a large complicated Boerhaave's mid-esophageal perforation. The patient fully recovered after being treated by a long esophageal stent which remained in place for 3 months.
2. Case report
An 86-year-old man was diagnosed with acute gastroenteritis and suffered from a prominent vomiting. One day later he was admitted to a hospital with a severe clinical situation of pneumomediastinitis and shock due to Borehaave's syndrome. The esophageal rupture was demonstrated by computed tomography scan (Fig. 1).
Fig. 1.
Computed tomography shows esophageal rupture with contrast media extravasation, and mediastinal and bilateral pleural effusions.
The patient's age, comorbidities, and severe condition were considered high risk for thoracic surgery; therefore the patient underwent conservative therapeutic maneuvers including drainage of pleural effusions, broad spectrum antibiotics, and feeding jejunostomy. Three weeks after admission an endoscopy demonstrated a 5-cm long, full-thickness mid-esophageal tear, covered by fibrin and pus.
A nitinol fully covered 18-cm long esophageal stent was inserted (Taewoong Niti-S) (Figs. 2 and 3), covering the esophageal rupture. Two weeks afterward, the patient started a gradual oral feeding.
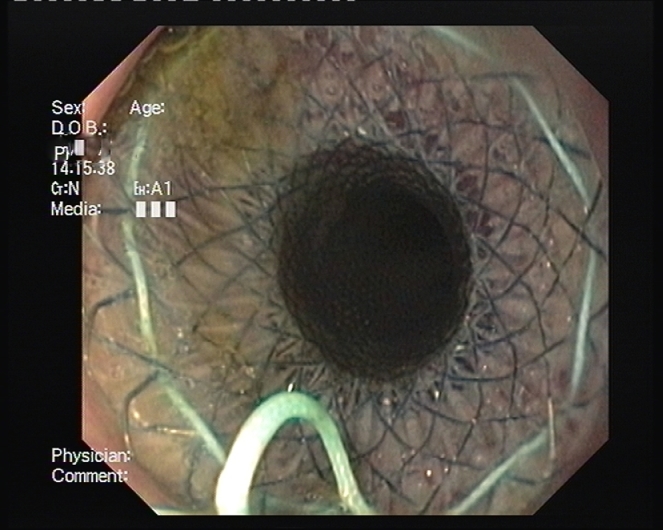
Fig. 2.
Endoscopic 18 cm. Niti-s stent was inserted under fluorography guidance.
Fig. 3.
Computed tomography shows the stent position and the coverage of the esophageal hole.
The patient was put under close clinical and radiographic observation and follow-up. The stent was kept in place for 3 months, and was then partially dislodged toward the stomach. Our goals were to achieve clinical and radiological-confirmed improvement and resolution of pleural effusions. Since these targets were met by this time, the stent was endoscopically removed and the esophageal wall remained intact (Fig. 4).
Fig. 4.
A follow-up computed tomography after 3 months of recovery, shows a complete resolution of bilateral pleural effusions. The stent was withdrawn from the esophagus.
3. Discussion and conclusion
Esophageal Boerhaave syndrome is a devastating clinical condition and without a surgical repair the mortality is high. Thoracic surgery by itself carries high morbidity and mortality risks, especially in the sick and elderly patient.
Treatment of the esophageal rupture with a long covered esophageal stent is an alternative option for selected and inoperable patients. However, several observational studies showed that substantial proportion of these patients needed further endoscopic or surgical intervention. The optimal time for stent removal is unknown, but short-term insertion (until 6 weeks) is usually advocated [3], [4].
Despite a very difficult starting point our patient showed a quite rapid healing process and could resume oral nutrition very soon after the stent placement and continued to have gradual favorable course of recovery.
Allowing the esophageal stent to remain in place for 3 months until complete clinical and radiographic resolution is possible and even beneficial.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2018.04.026.
Contributor Information
Kopelman Y, Email: Yaelk@hy.health.gov.il.
Abu baker F, Email: Fa_fd@hotmail.com.
Troiza A, Email: Troitsa@hy.health.gov.il.
Hebron D, Email: Danh@hy.health.gov.il.
Appendix. Supplementary materials
References
- 1.van Heel N.C., Haringsma J., Spaander M.C., Bruno M.J., Kuipers E.J. Short-term esophageal stenting in the management of benign perforations. Am J Gastroenterol. 2010;105(7):1515. doi: 10.1038/ajg.2010.104. [DOI] [PubMed] [Google Scholar]
- 2.Freeman R.K., Ascioti A.J., Dake M., Mahidhara R.S. An assessment of the optimal time for removal of esophageal stents used in the treatment of an esophageal anastomotic leak or perforation. Ann Thorac Surg. 2015;100(2):422–428. doi: 10.1016/j.athoracsur.2015.03.085. [DOI] [PubMed] [Google Scholar]
- 3.Schweigert M., Beattie R., Solymosi N., Booth K., Dubecz A., Muir A. Endoscopic stent insertion versus primary operative management for spontaneous rupture of the esophagus (Boerhaave syndrome): an international study comparing the outcome. Am Surg. 2013;79:634. doi: 10.1177/000313481307900627. [DOI] [PubMed] [Google Scholar]
- 4.Dasari B.V., Neely D., Kennedy A., Spence G., Rice P., Mackle E. The role of esophageal stents in the management of esophageal anastomotic leaks and benign esophageal perforations. Ann Surg. 2014;259:852. doi: 10.1097/SLA.0000000000000564. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.