Key Points
Question
Is emergent whole-body computed tomography associated with a lower mortality for children with blunt trauma compared with selective computed tomography?
Findings
In this propensity-weighted study using records from the National Trauma Data Bank on 42 912 children, there was no significant difference in mortality between children with blunt trauma who received emergent whole-body computed tomography and those who received a selective computed tomography approach.
Meaning
The results of this study raise questions about the routine, indiscriminate use of emergent whole-body computed tomography for children with blunt trauma; a more selective approach to computed tomography imaging for children with blunt trauma is warranted.
Abstract
Importance
Although several studies have demonstrated an improvement in mortality for injured adults who receive whole-body computed tomography (WBCT), it is unclear whether children experience the same benefit.
Objective
To determine whether emergent WBCT is associated with lower mortality among children with blunt trauma compared with a selective CT approach.
Design, Setting, and Participants
A retrospective, multicenter cohort study was conducted from January 1, 2010, to December 31, 2014, using data from the National Trauma Data Bank on children aged 6 months to 14 years with blunt trauma who received an emergent CT scan in the first 2 hours after emergency department arrival. Data analysis was conducted from February 2 to December 29, 2017.
Exposures
Patients were classified as having WBCT if they received CT head, CT chest, and CT abdomen/pelvis scans in the first 2 hours and as having a selective CT if they did not receive all 3 scans.
Main Outcomes and Measures
The primary outcome was in-hospital mortality in the 7 days after ED arrival. To adjust for potential confounding, propensity score weighting was used. Subgroup analyses were performed for those with the highest mortality risk (ie, occupants and pedestrians involved in motor vehicle crashes, children with a Glasgow Coma Scale score lower than 9, children with hypotension, and those admitted to the intensive care unit).
Results
Of the 42 912 children included in the study (median age [interquartile range], 9 [5-12] years; 27 861 [64.9%] boys), 8757 (20.4%) received a WBCT. Overall, 405 (0.9%) children died within 7 days. After adjusting for the propensity score, children who received WBCT had no significant difference in mortality compared with those who received selective CT (absolute risk difference, −0.2%; 95% CI, −0.6% to 0.1%). All subgroup analyses similarly showed no significant association between WBCT and mortality.
Conclusions and Relevance
Among children with blunt trauma, WBCT, compared with a selective CT approach, was not associated with lower mortality. These findings do not support the routine use of WBCT for children with blunt trauma.
This cohort study examines the mortality rate in children who experienced blunt trauma and underwent whole-body vs selective computed tomography.
Introduction
Trauma is the leading cause of death among children in the United States.1 Prompt and accurate detection are essential to the successful treatment of life-threatening injuries. To meet this challenge, the use of computed tomography (CT) in the evaluation of injured patients has risen steadily over the past 25 years.2,3,4 Computed tomography has the capability of providing the clinician with a high-quality, 3-dimensional image of the injured patient. Some studies have suggested that the use of emergent whole-body CT (WBCT), particularly in those with severe trauma, may improve survival by identifying occult injury that would otherwise not have been detected with selective CT scanning.5,6,7,8 As a result, the use of WBCT has increased considerably, becoming the standard imaging tool at many centers for patients who experience blunt trauma.9,10 Although these studies evaluated mostly adults, several physicians support the use of emergent WBCT in children with blunt trauma.11,12
While CT is accurate in diagnosing injury, it exposes the patient to a substantial amount of ionizing radiation that several studies have found to be associated with an increased risk for future cancer.13,14,15 Children appear to be especially sensitive to radiation and at higher risk for cancer compared with adults, because their organs are still developing and they have more time to manifest that risk.
The lack of pediatric-specific data regarding WBCT has forced many clinicians to extrapolate the findings of adult studies to children. Children have different injury patterns than adults16,17 and many injuries identified on CT do not require an operation.18 Balancing the risk of occult, life-threatening injury and the risk of radiation-induced cancer is therefore a challenge for emergency and trauma specialists. The objective of this study is to determine whether emergent WBCT is associated with a lower mortality rate among injured children compared with a selective CT approach.
Methods
Data Source and Design
We conducted a retrospective, multicenter cohort study, using the National Trauma Data Bank (NTDB), of children injured between January 1, 2010, and December 31, 2014.19 Data analysis was performed from February 2 to December 29, 2017. The study protocol was approved by the institutional review board at the Albert Einstein College of Medicine. Data were deidentified prior to release to the public.
Patients
Children between the ages of 6 months and 14 years with a history of sustaining blunt trauma were eligible for analysis. To avoid including patients who were too severely injured to undergo a CT scan, only those who received at least 1 CT scan within the first 2 hours of emergency department (ED) arrival were studied. This group therefore included both patients who received a WBCT and those who had the opportunity to receive WBCT but the clinician chose not to order it. In addition, we excluded patients who were transferred to or from another facility and those for whom a time of death or hospital discharge was not recorded.
Exposure Measures
Using International Classification of Diseases, Ninth Revision (ICD-9) procedure codes, patients were classified as having an emergent WBCT if they received CT head, CT chest, and CT abdomen/pelvis scans within the first 2 hours of ED arrival. Patients were classified as having selective CT if they did not receive WBCT within the first 2 hours of arrival. Traditionally, cervical spine CT has been included in the description of WBCT. However, there is no ICD-9 procedure code specific to cervical spine CT and thus we were unable to include this type of CT as part of our WBCT definition. We believe that this definition is acceptable as the mortality of children with cervical spine injuries is most often due to concomitant injuries (eg, head injury).20
Primary Outcome Measure
The primary outcome was in-hospital mortality in the 7 days after ED arrival. The cause of death is often different for patients who die in the first week of hospitalization compared with those who die in subsequent weeks.21 We chose to not incorporate these latter patients among those experiencing the outcome so as not to include patients who died from complications of hospitalization (eg, infection) and not directly as a result of trauma.
Covariates
We examined the following patient and hospital characteristics as potential confounders: age, sex, race, mechanism of injury, payment type, Glasgow Coma Scale (GCS) score (ranging from 0 [not responsive] to 15 [fully responsive]), hypoxia, hypotension, use of assisted respirations, packed red blood cell (PRBC) transfusion received, plasma transfusion received, platelet transfusion received, chest tube thoracostomy placed, hospital type, adult and pediatric trauma center status, hospital region, and the number of pediatric beds at the hospital.
Statistical Analysis
Continuous variables were described using medians and interquartile ranges (IQRs) and compared between groups using a Mann-Whitney test. Categorical variables were described using frequencies and percentages and compared between groups using χ2 tests. For all analyses of treatment effects, a robust variance estimator accounted for the correlation due to clustering of patients within hospitals. A P value <.05 was considered statistically significant for all analyses. Testing was 2-tailed and unpaired. All analyses were performed using Stata, version 15.1 (StataCorp).
Propensity Model
Children who receive WBCT are inherently different and often more severely injured than those who receive selective CT. To account for potential confounding in the association of WBCT and mortality, we created a propensity score for each patient and applied inverse probability weighting using the Treatment-Effects package in Stata, version 15.1.22 The propensity score represented the predicted probability of receiving treatment (ie, WBCT) conditional on the covariates listed above and was used to adjust covariate differences across WBCT and selective CT groups. Propensity score analyses adjust for selection bias that is intrinsic to observational studies and attempt to simulate the conditions present in a randomized clinical trial by balancing covariates across treatment groups before determining the outcome.23,24,25,26
The propensity score for treatment was determined using a logistic regression model with WBCT as the dependent variable and the above-listed covariates as independent variables. In addition, we examined 6 clinically plausible interactions: hypoxia and assisted respirations, pediatric trauma center status and number of pediatric beds, pediatric trauma center status and adult trauma center status, pediatric trauma center status and age, hypotension and PRBC transfusion, and PRBC transfusion and chest tube thoracostomy. We included the statistically significant interactions as product terms in the creation of this treatment model. We confirmed that the area of common support was sufficient by examining overlap plots of the propensity scores by treatment group. In addition, to meet the overlap assumption, patients with propensity scores smaller than the default tolerance of 1.00 • e−5 were excluded from the model (eTable 1 in the Supplement).22
The propensity score was next used to create inverse probability weights for each patient. Using these weights, a propensity-weighted sample was created to make the WBCT and selective CT groups more similar, with respect to their baseline covariate distributions, than the overall sample. To confirm that the WBCT and selective CT groups were similar in the propensity-weighted sample, we next examined covariate balance. The following ranges for each covariate were used to indicate acceptable balance between groups: standardized difference, −0.15 to 0.15; and variance ratio, 0.5 to 2.0.27
To account for missing values in several of the independent covariates, we used a missing indicator approach. Missing values were coded as such and missing was included as a category for the variable. The propensity score thus attempted to balance both distributions of observed covariates, as well as distributions of missing data, across treatment groups.28
Outcomes and Subgroup Analyses
As the primary outcome, the absolute risk difference and relative risk (RR) of death between treatment groups were then calculated for both the unadjusted sample and the propensity-weighted samples.
For secondary outcomes, we explored the association of WBCT and ED length of stay (LOS) and total hospital LOS. Because the distributions of both ED LOS and total hospital LOS were right-skewed, we calculated the absolute median difference between groups. This calculation was accomplished using a propensity-score–weighted quantile regression model, with LOS as the dependent variable and WBCT as the only independent variable.29
As prespecified subgroup analyses, we also examined separate propensity models for children with the highest likelihood of dying: occupants in motor vehicle crashes (MVCs), pedestrians in MVCs, patients with GCS scores lower than 9, patients with hypotension, and patients admitted to the intensive care unit.6,30,31
Sensitivity Analyses
We performed 3 sensitivity analyses to examine the stability of the primary outcome. First, as several authors have advised against adjusting for Injury Severity Score when examining the association of WBCT and mortality,6,32 we repeated the analysis with the addition of Injury Severity Score (ranging from 0 [uninjured] to 75 [usually unsurvivable injuries]) to examine its association with our results. Second, because head injury is the leading cause of death in children due to trauma but alone does not often necessitate WBCT,6 we performed an additional analysis excluding patients with isolated head injury.31 Third, we conducted post hoc tests of endogeneity to examine for the presence of potential unmeasured confounding variables that would alter our observations. A further description of these methods can be found in the eAppendix in the Supplement.
Results
Patient Characteristics
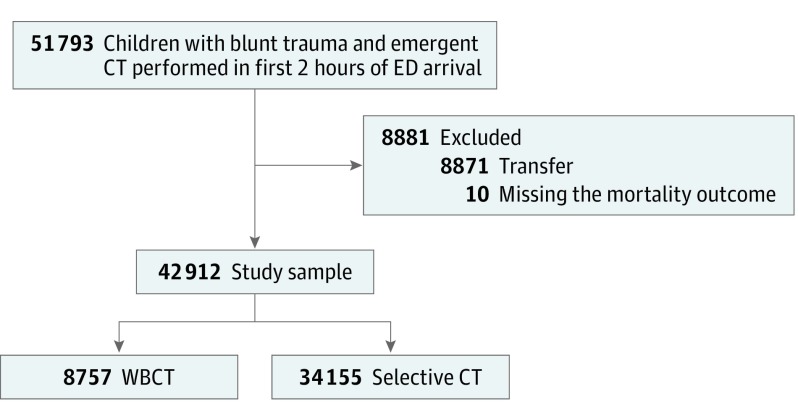
From 2010 to 2014, there were 51 793 children with blunt trauma who had a CT performed in the first 2 hours of their evaluation. After exclusions, 42 912 patients at 631 hospitals overall were eligible for analysis. The median number of patients enrolled per hospital was 24 (IQR, 6-83). A total of 8757 (20.4%) children received WBCT (Figure). These children were more likely to be older, be involved in a MVC, have a GCS score lower than 9, have hypoxia, have hypotension, and require assisted respiration, a chest tube, or blood products (Table 1). In addition, these patients were less likely to be seen at a university hospital, pediatric trauma center, or the largest of pediatric hospitals. Forty-two (0.1%) patients were noted to have both blunt and penetrating trauma; 3 (7.1%) of these children received WBCT.
Figure. CONSORT Diagram of Patient Eligibility and Flow.
CT indicates computed tomography; ED, emergency department; and WBCT, whole-body CT.
Table 1. Patient and Hospital Characteristics by CT Exposure Group for Overall and Weighted Samplesa.
| Characteristic | No. (%) | Standardized Difference | No. (%) | Standardized Difference | ||
|---|---|---|---|---|---|---|
| WBCT (n = 8757) |
Selective CT (n = 34 155) |
Weighted WBCT (n = 20 992) |
Weighted Selective CT (n = 21 920) |
|||
| Patient Characteristics | ||||||
| Age, median (IQR), y | 10 (6 to 13) | 9 (5 to 12) | 0.16 | 9 (5 to 13) | 9 (5 to 12) | 0.03 |
| Sex | ||||||
| Female | 3234 (36.9) | 11 800 (34.5) | 0 [Reference] | 7333 (34.9) | 7701 (35.1) | 0 [Reference] |
| Male | 5517 (63.0) | 22 344 (65.4) | −0.05 | 13 652 (65.0) | 14 209 (64.8) | 0 |
| Missing | 6 (0.1) | 11 (0) | 0.02 | 7 (0) | 10 (0) | 0 |
| Race | ||||||
| White | 5216 (59.6) | 19 690 (57.6) | 0 [Reference] | 12 655 (60.3) | 12 770 (58.3) | 0 [Reference] |
| Black | 1258 (14.4) | 6044 (17.7) | −0.09 | 3360 (16.0) | 3695 (16.9) | −0.02 |
| Hispanic/Latino | 1396 (15.9) | 5213 (15.3) | 0.02 | 2975 (14.2) | 3353 (15.3) | −0.03 |
| Other | 887 (10.1) | 3208 (9.4) | 0.02 | 2001 (9.5) | 2102 (9.6) | 0 |
| Mechanism of Trauma | ||||||
| Other | 1533 (17.5) | 5461 (16.0) | 0 [Reference] | 3637 (17.3) | 3536 (16.1) | 0 [Reference] |
| Fall from height | 368 (4.2) | 1220 (3.6) | 0.03 | 747 (3.6) | 803 (3.7) | −0.01 |
| Fall | 809 (9.2) | 10 971 (32.1) | −0.59 | 5401 (25.7) | 5969 (27.2) | −0.03 |
| Assault | 328 (3.7) | 4640 (13.6) | −0.36 | 2417 (11.5) | 2516 (11.5) | 0 |
| MVC pedestrian | 1622 (18.5) | 3669 (10.7) | 0.22 | 2726 (13.0) | 2767 (12.6) | 0.01 |
| MVC occupant | 3355 (38.3) | 6493 (19.0) | 0.44 | 4845 (23.1) | 5080 (23.2) | 0 |
| MVC other | 742 (8.5) | 1701 (5.0) | 0.14 | 1218 (5.8) | 1249 (5.7) | 0 |
| Payment | ||||||
| Medicaid/Medicare | 2885 (32.9) | 11 965 (35.0) | 0 [Reference] | 6934 (33.0) | 7558 (34.5) | 0 [Reference] |
| Private | 3122 (35.7) | 14 822 (43.4) | −0.16 | 8700 (41.4) | 9144 (41.7) | −0.01 |
| Other | 2750 (31.4) | 7368 (21.6) | 0.22 | 5358 (25.5) | 5218 (23.8) | 0.04 |
| Clinical Presentation | ||||||
| GCS scoreb | ||||||
| ≥9 | 7331 (83.7) | 31 676 (92.7) | 0 [Reference] | 18 855 (89.8) | 19 741 (90.1) | 0 [Reference] |
| <9 | 1177 (13.4) | 1251 (3.7) | 0.36 | 1421 (6.8) | 1439 (6.6) | 0.01 |
| Missing | 249 (2.8) | 1228 (3.6) | −0.04 | 717 (3.4) | 739 (3.4) | 0 |
| Hypoxia | ||||||
| Oxygen saturation ≥94% | 7395 (84.4) | 29 159 (85.4) | 0 [Reference] | 18 003 (85.8) | 18 600 (84.9) | 0 [Reference] |
| Oxygen saturation <94% | 763 (8.7) | 1226 (3.6) | 0.21 | 1158 (5.5) | 1098 (5.0) | 0.02 |
| Missing | 599 (6.8) | 3770 (11.0) | −0.15 | 1831 (8.7) | 2222 (10.1) | −0.05 |
| Hypotension | ||||||
| No | 8291 (94.7) | 32 361 (94.7) | 0 [Reference] | 19 790 (94.3) | 20 682 (94.4) | 0 [Reference] |
| Yes | 393 (4.5) | 666 (1.9) | 0.14 | 657 (3.1) | 630 (2.9) | 0.02 |
| Missing | 73 (0.8) | 1128 (3.3) | −0.17 | 545 (2.6) | 608 (2.8) | −0.01 |
| Assisted respirations | ||||||
| No | 7341 (83.8) | 30 191 (88.4) | 0 [Reference] | 18 261 (87.0) | 19 014 (86.7) | 0 [Reference] |
| Yes | 1056 (12.1) | 1338 (3.9) | 0.30 | 1501 (7.2) | 1391 (6.4) | 0.03 |
| Missing | 360 (4.1) | 2626 (7.7) | −0.15 | 1231 (5.9) | 1516 (6.9) | −0.04 |
| Chest tube | 251 (2.9) | 107 (0.3) | 0.21 | 207 (1.0) | 294 (1.3) | −0.03 |
| Transfusions | ||||||
| PRBCs | 239 (2.7) | 171 (0.5) | 0.18 | 230 (1.1) | 262 (1.2) | −0.01 |
| Plasma | 100 (1.1) | 64 (0.2) | 0.12 | 89 (0.4) | 99 (0.5) | 0 |
| Platelets | 38 (0.4) | 19 (0.1) | 0.08 | 28 (0.1) | 35 (0.2) | −0.01 |
| Hospital Characteristics | ||||||
| Hospital type | ||||||
| Community | 4048 (46.2) | 13 083 (38.3) | 0 [Reference] | 8296 (39.5) | 8800 (40.1) | 0 [Reference] |
| University | 3547 (40.5) | 16 805 (49.2) | −0.18 | 10 209 (48.6) | 10 365 (47.3) | 0.03 |
| Nonteaching | 1162 (13.3) | 4267 (12.5) | 0.02 | 2487 (11.9) | 2755 (12.6) | −0.02 |
| Adult trauma center | 7543 (86.1) | 20 943 (61.3) | 0.59 | 14 467 (68.9) | 14 617 (66.7) | 0.05 |
| Pediatric trauma center | 4007 (45.8) | 19 350 (56.7) | −0.22 | 10 981 (52.3) | 11 899 (54.3) | −0.04 |
| Region | ||||||
| Midwest | 1988 (22.7) | 10 206 (29.9) | 0 [Reference] | 6199 (29.5) | 6254 (28.5) | 0 [Reference] |
| Northeast | 1722 (19.7) | 6194 (18.1) | 0.04 | 3950 (18.8) | 4046 (18.5) | 0.01 |
| South | 3427 (39.1) | 9858 (28.9) | 0.22 | 6246 (29.8) | 6792 (31.0) | −0.03 |
| West | 1430 (16.3) | 7498 (22.0) | −0.14 | 4297 (20.5) | 4529 (20.7) | 0 |
| Missing | 190 (2.2) | 399 (1.2) | 0.08 | 300 (1.4) | 299 (1.4) | 0.01 |
| No. of pediatric beds | ||||||
| 0 | 508 (5.8) | 2195 (6.4) | 0 [Reference] | 1364 (6.5) | 1369 (6.3) | 0 [Reference] |
| 1-10 | 1012 (11.6) | 2776 (8.1) | 0.12 | 1826 (8.7) | 1913 (8.7) | 0 |
| 11-15 | 508 (5.8) | 2122 (6.2) | −0.02 | 1396 (6.7) | 1361 (6.2) | 0.02 |
| 16-30 | 1830 (20.9) | 5204 (15.2) | 0.15 | 3347 (15.9) | 3570 (16.3) | −0.01 |
| 31-80 | 2082 (23.8) | 5766 (16.9) | 0.17 | 4418 (21.0) | 4104 (18.7) | 0.06 |
| >80 | 2772 (31.7) | 15 951 (46.7) | −0.31 | 8554 (40.8) | 9512 (43.4) | −0.05 |
| Missing | 45 (0.5) | 141 (0.4) | 0.01 | 87 (0.4) | 92 (0.4) | 0 |
Abbreviations: CT, computed tomography; GCS, Glasgow Coma Scale; IQR, interquartile range; MVC, motor vehicle crash; PRBCs, packed red blood cells; WBCT, whole-body CT.
Percentages may not total 100% due to rounding. Weighted frequencies are rounded to whole numbers; therefore, group composite may not equal total.
Score lower than 9 generally indicates severe brain injury.
Four interaction product terms were found to be statistically significant and included in the creation of the propensity score: hypoxia and assisted respirations (χ24 = 18.5, P = .001), pediatric trauma center status and number of pediatric beds (χ25 = 11.8, P = .04), pediatric trauma center status and adult trauma center status (χ21 = 14.0, P < .001), and PRBC transfusion and chest tube thoracostomy (χ21 = 8.9, P = .003). The distribution of baseline covariates in the propensity-weighted sample mirrored that of the overall sample (Table 1). When stratified by exposure group, however, covariate differences between the WBCT and selective CT groups that were present in the overall sample were no longer apparent in the propensity-weighted sample.
Standardized differences and variance ratios for baseline covariates prior to propensity weighting ranged from −0.59 to 0.59 and 0.19 to 8.92, respectively. After propensity score adjustment, standardized differences and variance ratios for baseline covariates ranged from −0.06 to 0.06 and 0.62 to 1.14, respectively, indicating improved covariate balance between the WBCT and selective CT groups (eTable 2 in the Supplement). Each subgroup analysis, after adjustment, similarly demonstrated improved covariate balance within the desired limits (eTables 3-7 in the Supplement).
Outcomes
Overall, 405 (0.9%) children died within 7 days from ED arrival. Mortality varied by mechanism, with MVC carrying the highest risk: MVC pedestrian, 101 (1.9%); MVC occupant, 167 (1.7%); MVC other, 35 (1.4%); fall from height, 11 (0.7%); assault, 23 (0.5%); fall, 30 (0.3%); other, 38 (0.5%). In addition, mortality was significantly higher for children with a GCS score lower than 9 (13.8% vs 0.1%; RR, 141.6; 95% CI, 101.5-197.6), children who were hypotensive (9.6% vs 0.7%; RR, 13.2; 95% CI, 10.7-16.4), or children admitted to the intensive care unit (3.1% vs 0.2%; RR, 16.5; 95% CI, 12.5-21.6), compared with those who were not. None of the patients who experienced both blunt and penetrating trauma died.
In an unadjusted analysis, children who received WBCT had a significantly higher risk of death compared with those who received selective CT. After propensity score adjustment, however, this association was attenuated and no longer significant (Table 2). This lack of association similarly persisted after adjustment regardless of whether the child was a pedestrian struck by a motor vehicle, was an occupant in a MVC, had a GCS score lower than 9, was hypotensive, or was admitted to the intensive care unit.
Table 2. Propensity Score–Weighted Mortality Risk for Children Who Received WBCT vs Selective CT.
| Sample | No. | No. (%) | Absolute Risk Difference, % (95% CI) | Relative Risk (95% CI) | |
|---|---|---|---|---|---|
| WBCT | Selective CT | ||||
| Unadjusted sample | 42 912 | 228 (2.6) | 177 (0.5) | 2.1 (1.7 to 2.4) | 5.0 (4.1 to 6.1) |
| Adjusted samples | |||||
| Overall | 42 912 | 224 (1.1) | 284 (1.3) | −0.2 (−0.6 to 0.1) | 0.8 (0.6 to 1.1) |
| Mechanism | |||||
| MVC pedestrian | 5291 | 56 (2.2) | 84 (3.1) | −0.9 (−2.2 to 0.3) | 0.7 (0.4 to 1.1) |
| MVC occupant | 9844 | 98 (2.0) | 83 (1.7) | 0.3 (−0.4 to 1.1) | 1.2 (0.8 to 1.8) |
| GCS score <9a | 2427 | 181 (14.9) | 173 (14.2) | 0.7 (−2.6 to 3.9) | 1.0 (0.8 to 1.3) |
| Hypotension | 1056 | 62 (11.9) | 56 (10.5) | 1.4 (−2.9 to 5.8) | 1.1 (0.8 to 1.7) |
| Admitted to ICU | 11 106 | 182 (3.3) | 203 (3.6) | −0.3 (−1.2 to 0.7) | 0.9 (0.7 to 1.2) |
Abbreviations: CT, computed tomography; GCS, Glasgow Coma Scale; ICU, intensive care unit; MVC, motor vehicle crash; WBCT, whole-body CT.
Score lower than 9 generally indicates severe brain injury.
Overall and for most subgroups, after adjustment, WBCT was associated with a shorter median ED LOS, but this difference was at most 30 minutes (Table 3). Median total hospital LOS, however, was consistently prolonged in the WBCT group overall and in every subgroup. This difference varied, depending on the analysis, from 19 to 48 hours.
Table 3. Propensity Score–Weighted ED and Total Hospital LOS for Children Who Received WBCT vs Selective CT.
| Sample | ED LOS, h | Total Hospital LOS, ha | ||||
|---|---|---|---|---|---|---|
| Median (IQR) | Difference (95% CI) | Median (IQR) | Difference (95% CI) | |||
| WBCT | Selective CT | WBCT | Selective CT | |||
| Unadjusted sample | 2.7 (1.7 to 4.0) | 3.2 (2.1 to 4.5) | −0.5 (−0.5 to −0.4) | 43.0 (13.2 to 100.1) | 22.0 (4.6 to 46.5) | 21.0 (19.9 to 22.1) |
| Adjusted samples | ||||||
| Overall | 2.7 (1.7 to 4.0) | 3.1 (2.0 to 4.4) | −0.4 (−0.4 to −0.3) | 41.3 (14.3 to 91.5) | 22.4 (4.6 to 48.2) | 18.9 (16.7 to 21.0) |
| Mechanism | ||||||
| MVC pedestrian | 2.6 (1.6 to 3.9) | 2.9 (1.9 to 4.3) | −0.3 (−0.5 to −0.2) | 49.4 (19.1 to 117.8) | 29.3 (16.6 to 73.6) | 20.1 (13.0 to 27.3) |
| MVC occupant | 3.0 (1.7 to 4.4) | 3.2 (2.0 to 4.7) | −0.2 (−0.4 to −0.1) | 49.4 (19.9 to 113.2) | 26.9 (6.6 to 69.6) | 22.5 (19.2 to 25.8) |
| GCS score <9b | 1.4 (0.9 to 2.3) | 1.3 (0.9 to 2.2) | 0.1 (−0.1 to 0.2) | 122.4 (20.6 to 328.3) | 92.0 (18.2 to 291.3) | 30.4 (5.0 to 55.9) |
| Hypotension | 1.9 (1.1 to 3.2) | 2.3 (1.3 to 3.9) | −0.5 (−0.8 to −0.1) | 78.6 (19.4 to 218.5) | 30.7 (5.4 to 139.7) | 47.9 (15.4 to 80.3) |
| Admitted to ICU | 1.9 (1.1 to 3.1) | 2.3 (1.2 to 3.6) | −0.4 (−0.6 to −0.3) | 94.2 (46.5 to 195.2) | 68.7 (35.5 to 139.2) | 25.5 (19.2 to 31.8) |
Abbreviations: CT, computed tomography; ED, emergency department; GCS, Glasgow Coma Scale; ICU, intensive care unit; IQR, interquartile range; LOS, length of stay; MVC, motor vehicle crash; WBCT, whole-body CT.
Total hospital LOS includes ED LOS.
Score lower than 9 generally indicates severe brain injury.
Sensitivity Analyses
Children who received WBCT had a significantly higher median Injury Severity Score than those who underwent selective CT (10; IQR 5-17; vs 5; IQR, 3-10; P < .001). Adjusting for Injury Severity Score in our propensity models, however, produced similar results to our primary analysis (eTable 8 in the Supplement). In addition, there was little difference from our primary analysis after excluding patients with isolated head injury (eTable 9 in the Supplement). Moreover, there was no evidence of significant endogeneity in our primary analysis or in any of the subgroup analyses (eTable 10 in the Supplement), suggesting an overall lack of unmeasured confounding.
Discussion
In this large, multicenter, propensity-weighted study of children with blunt trauma, we found no evidence that WBCT was associated with lower mortality compared with selective CT. In addition, subgroup analyses of children with the highest risk of death did not demonstrate any significant survival benefit for those who received WBCT. The lack of improvement in mortality that we observed may suggest that any additional injuries that might have been detected by WBCT were either not life-threatening or did not offset the potential risk of an injured patient receiving a prolonged CT scan.
The association of WBCT and mortality is difficult to evaluate for several reasons and we designed our study with each reason in mind. First, while trauma is the leading cause of death for children in the United States, death due to blunt trauma occurs infrequently. Established in 1989, the NTDB represents the largest collection of trauma data ever assembled in the United States and provided us with a unique opportunity to study this rare outcome. Second, to examine any intervention that affects mortality using an observational cohort, the researcher must consider immortal time bias. Immortal time bias occurs when more severely injured patients die prior to receiving the intervention and thus, by design, are assigned to the comparison group.33 Inclusion of such patients can make the intervention misleadingly appear to improve survival and has been a criticism of prior studies involving WBCT.34 To control for this bias, we included only patients who received at least 1 CT scan in the first 2 hours and thus must have had the opportunity to receive WBCT. Third, this association is subject to confounding by indication. Specifically, children with blunt trauma who receive multiple CTs are likely to be more injured than those who receive less imaging. This was demonstrated in our unadjusted analysis: children who received WBCT had a higher mortality rate than those who underwent selective CT. We attempted to deal with this bias by using propensity score weighting and making the WBCT and selective CT groups as similar as possible with respect to their baseline covariates prior to ascertaining the outcome. Moreover, we confirmed the stability of these findings in several high-risk subgroup and sensitivity analyses.
While most of the prior investigations on adults have focused on whether WBCT improves survival, a few studies have attempted to address other possible benefits of WBCT, such as LOS. Our data concurred with the previous literature with regard to ED LOS and total hospital LOS. Although WBCT was associated with a shorter ED LOS, this difference in time was small; the pooled estimate of prior studies was approximately 15 minutes and in our overall adjusted analysis was approximately 25 minutes.8 Moreover, this finding was consistent in all of the severely injured subgroups that we studied. Similarly, our study results agree with previous research demonstrating that WBCT is associated with an approximately 1 day longer hospital LOS compared with selective CT.8 We surmise that the WBCT group in our study, despite being balanced with the selective CT group on multiple covariates, may have had more non–life-threatening injuries and incidental findings detected and that the physicians caring for them spent more time addressing these findings. While we recognize that the importance of identifying all non–life-threatening injuries and incidental findings will continue to be a matter of debate,35 there is a shift in recent times for researchers to focus on identifying only injuries that are believed to be clinically important.36,37,38
Limitations
Our findings should be interpreted in light of the following limitations. First, our study investigated only mortality and LOS outcomes, and perhaps WBCT may have other benefits that would be helpful to the care of injured children, such as identifying nonlethal occult injuries. Second, because the NTDB includes only patients who were admitted or died after arrival, our sample may have been more severely injured than most children with blunt trauma who present to an ED. Most studies regarding WBCT have focused, however, on patients with higher acuity who, many believe, are more likely to benefit from WBCT.5,6,7 Third, propensity score analyses can only balance exposure groups based on the variables included in the propensity score. While we attempted to include as many confounders as reasonably feasible using a preassembled national data set and after adjustment achieved good balance between groups for all measured covariates, residual confounding may have affected our results.
Because a randomized clinical trial39 to investigate the effect of WBCT on mortality in children with blunt trauma is impractical and may be considered unethical by some, this study offers the best available evidence on this issue to date in the pediatric literature. Further prospective study is needed to determine whether a selective CT approach performs as well as WBCT in other areas, such as the identification of clinically important occult injuries. This information would be particularly beneficial when performing a cost-effectiveness analysis utilizing novel low-dose CT imaging technology.40
Conclusions
In this large, multicenter, propensity-weighted study of children with blunt trauma, emergent WBCT was not associated with lower mortality for children with blunt trauma, compared with a selective CT approach. This outcome was consistent regardless of how severely injured the children were. These results have implications for how emergency and trauma specialists care for injured children. Although WBCT may provide more information about the injured child, that information does not appear to be lifesaving. With growing concerns regarding excessive radiation exposure for injured children, physicians should attempt to limit CT exposure whenever possible.
eTable 1. List of Excluded Patients Due to Failure of Overlap Assumption in Propensity Score Model
eTable 2. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: Overall
eTable 3. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: MVC Pedestrian Subgroup
eTable 4. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: MVC Occupant Subgroup
eTable 5. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: Glasgow Coma Scale < 9 Subgroup
eTable 6. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: Hypotension Subgroup
eTable 7. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: ICU Admission Subgroup
eTable 8. Propensity Score Weighted Mortality Risk for Children Who Received WBCT vs Selective CT: Additionally Adjusted for Injury Severity Score (ISS)
eTable 9. Propensity Score Weighted Mortality Risk for Children Who Received WBCT vs Selective CT: Excluding Children with Isolated Head Injury
eTable 10. Endogeneity Tests for Presence of Residual Confounding in the Overall and Subgroup Treatment Effects Models
eAppendix. Expanded Notes on Methods
References
- 1.Heron M. Deaths: Leading Causes for 2014. Natl Vital Stat Rep. 2016;65(5):1-96. [PubMed] [Google Scholar]
- 2.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998-2007. JAMA. 2010;304(13):1465-1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larson DB, Johnson LW, Schnell BM, Goske MJ, Salisbury SR, Forman HP. Rising use of CT in child visits to the emergency department in the United States, 1995-2008. Radiology. 2011;259(3):793-801. [DOI] [PubMed] [Google Scholar]
- 4.Blackwell CD, Gorelick M, Holmes JF, Bandyopadhyay S, Kuppermann N. Pediatric head trauma: changes in use of computed tomography in emergency departments in the United States over time. Ann Emerg Med. 2007;49(3):320-324. [DOI] [PubMed] [Google Scholar]
- 5.Huber-Wagner S, Lefering R, Qvick LM, et al. ; Working Group on Polytrauma of the German Trauma Society . Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet. 2009;373(9673):1455-1461. [DOI] [PubMed] [Google Scholar]
- 6.Yeguiayan JM, Yap A, Freysz M, et al. ; FIRST Study Group . Impact of whole-body computed tomography on mortality and surgical management of severe blunt trauma. Crit Care. 2012;16(3):R101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huber-Wagner S, Biberthaler P, Häberle S, et al. ; TraumaRegister DGU . Whole-body CT in haemodynamically unstable severely injured patients—a retrospective, multicentre study. PLoS One. 2013;8(7):e68880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chidambaram S, Goh EL, Khan MA. A meta-analysis of the efficacy of whole-body computed tomography imaging in the management of trauma and injury. Injury. 2017;48(8):1784-1793. [DOI] [PubMed] [Google Scholar]
- 9.James MK, Schubl SD, Francois MP, Doughlin GK, Lee SW. Introduction of a pan-scan protocol for blunt trauma activations: what are the consequences? Am J Emerg Med. 2017;35(1):13-19. [DOI] [PubMed] [Google Scholar]
- 10.Hinzpeter R, Boehm T, Boll D, et al. Imaging algorithms and CT protocols in trauma patients: survey of Swiss emergency centers. Eur Radiol. 2017;27(5):1922-1928. [DOI] [PubMed] [Google Scholar]
- 11.Munk RD, Strohm PC, Saueressig U, et al. Effective dose estimation in whole-body multislice CT in paediatric trauma patients. Pediatr Radiol. 2009;39(3):245-252. [DOI] [PubMed] [Google Scholar]
- 12.Bayer J, Reising K, Kuminack K, Südkamp NP, Strohm PC. Is whole-body computed tomography the standard work-up for severely-injured children? results of a survey among German trauma centers. Acta Chir Orthop Traumatol Cech. 2015;82(5):332-336. [PubMed] [Google Scholar]
- 13.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176(2):289-296. [DOI] [PubMed] [Google Scholar]
- 14.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380(9840):499-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miglioretti DL, Johnson E, Williams A, et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessel B, Dagan J, Swaid F, et al. ; Israel Trauma Group . Rib fractures: comparison of associated injuries between pediatric and adult population. Am J Surg. 2014;208(5):831-834. [DOI] [PubMed] [Google Scholar]
- 17.Hermans E, Cornelisse ST, Biert J, Tan ECTH, Edwards MJR. Paediatric pelvic fractures: how do they differ from adults? J Child Orthop. 2017;11(1):49-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Notrica DM, Linnaus ME. Nonoperative management of blunt solid organ injury in pediatric surgery. Surg Clin North Am. 2017;97(1):1-20. [DOI] [PubMed] [Google Scholar]
- 19.National Trauma Data Bank National Trauma Data Bank User Manual: Admission Years 2002-2014. Chicago, IL: Committee on Trauma, American College of Surgeons; 2015. [Google Scholar]
- 20.Platzer P, Jaindl M, Thalhammer G, et al. Cervical spine injuries in pediatric patients. J Trauma. 2007;62(2):389-396. [DOI] [PubMed] [Google Scholar]
- 21.Sobrino J, Shafi S. Timing and causes of death after injuries. Proc (Bayl Univ Med Cent). 2013;26(2):120-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stata Treatment-Effects Reference Manual: Potential Outcomes/Counterfactual Outcomes. Version 15. College Station, Texas: Stata Press. https://www.stata.com/manuals/te.pdf. Updated 2017. Accessed January 3, 2018.
- 23.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127(8, pt 2):757-763. [DOI] [PubMed] [Google Scholar]
- 24.Martens EP, Pestman WR, de Boer A, Belitser SV, Klungel OH. Systematic differences in treatment effect estimates between propensity score methods and logistic regression. Int J Epidemiol. 2008;37(5):1142-1147. [DOI] [PubMed] [Google Scholar]
- 25.Li G, Holbrook A, Jin Y, et al. Comparison of treatment effect estimates of non–vitamin K antagonist oral anticoagulants versus warfarin between observational studies using propensity score methods and randomized controlled trials. Eur J Epidemiol. 2016;31(6):541-561. [DOI] [PubMed] [Google Scholar]
- 26.Kuss O, Legler T, Börgermann J. Treatments effects from randomized trials and propensity score analyses were similar in similar populations in an example from cardiac surgery. J Clin Epidemiol. 2011;64(10):1076-1084. [DOI] [PubMed] [Google Scholar]
- 27.Linden A, Samuels SJ. Using balance statistics to determine the optimal number of controls in matching studies. J Eval Clin Pract. 2013;19(5):968-975. [DOI] [PubMed] [Google Scholar]
- 28.Harder VS, Stuart EA, Anthony JC. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychol Methods. 2010;15(3):234-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee AH, Fung WK, Fu B. Analyzing hospital length of stay: mean or median regression? Med Care. 2003;41(5):681-686. [DOI] [PubMed] [Google Scholar]
- 30.Haider AH, Crompton JG, Oyetunji T, et al. Mechanism of injury predicts case fatality and functional outcomes in pediatric trauma patients: the case for its use in trauma outcomes studies. J Pediatr Surg. 2011;46(8):1557-1563. [DOI] [PubMed] [Google Scholar]
- 31.Sathya C, Alali AS, Wales PW, et al. Mortality among injured children treated at different trauma center types. JAMA Surg. 2015;150(9):874-881. [DOI] [PubMed] [Google Scholar]
- 32.Stengel D, Frank M, Matthes G, et al. Primary pan-computed tomography for blunt multiple trauma: can the whole be better than its parts? Injury. 2009;40(suppl 4):S36-S46. [DOI] [PubMed] [Google Scholar]
- 33.Suissa S. Immortal time bias in pharmaco-epidemiology. Am J Epidemiol. 2008;167(4):492-499. [DOI] [PubMed] [Google Scholar]
- 34.Andersohn F. Effect on survival of whole-body CT during trauma resuscitation. Lancet. 2009;374(9685):197. [DOI] [PubMed] [Google Scholar]
- 35.Shannon L, Peachey T, Skipper N, et al. Comparison of clinically suspected injuries with injuries detected at whole-body CT in suspected multi-trauma victims. Clin Radiol. 2015;70(11):1205-1211. [DOI] [PubMed] [Google Scholar]
- 36.Murphy SP, Hawthorne N, Haase D, Chiku C, Wen J, Rodriguez RM. Low yield of clinically significant injury with head-to-pelvis computed tomography in blunt trauma evaluation. J Emerg Med. 2017;53(6):865-870. [DOI] [PubMed] [Google Scholar]
- 37.Kuppermann N, Holmes JF, Dayan PS, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170. [DOI] [PubMed] [Google Scholar]
- 38.Holmes JF, Lillis K, Monroe D, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013;62(2):107-116.e2. [DOI] [PubMed] [Google Scholar]
- 39.Sierink JC, Treskes K, Edwards MJ, et al. ; REACT-2 study group . Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. Lancet. 2016;388(10045):673-683. [DOI] [PubMed] [Google Scholar]
- 40.Ebner L, Knobloch F, Huber A, et al. Feasible dose reduction in routine chest computed tomography maintaining constant image quality using the last three scanner generations: from filtered back projection to sinogram-affirmed iterative reconstruction and impact of the novel fully integrated detector design minimizing electronic noise. J Clin Imaging Sci. 2014;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. List of Excluded Patients Due to Failure of Overlap Assumption in Propensity Score Model
eTable 2. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: Overall
eTable 3. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: MVC Pedestrian Subgroup
eTable 4. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: MVC Occupant Subgroup
eTable 5. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: Glasgow Coma Scale < 9 Subgroup
eTable 6. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: Hypotension Subgroup
eTable 7. Standardized Differences and Variance Ratios for Propensity Model Covariates, Before and After Propensity Weighting: ICU Admission Subgroup
eTable 8. Propensity Score Weighted Mortality Risk for Children Who Received WBCT vs Selective CT: Additionally Adjusted for Injury Severity Score (ISS)
eTable 9. Propensity Score Weighted Mortality Risk for Children Who Received WBCT vs Selective CT: Excluding Children with Isolated Head Injury
eTable 10. Endogeneity Tests for Presence of Residual Confounding in the Overall and Subgroup Treatment Effects Models
eAppendix. Expanded Notes on Methods