Abstract
Importance
Based on the new 2017 blood pressure guidelines, the prevalence of high blood pressure (BP) among adults has increased from 32% to 46%. Based on new norms and diagnostic thresholds that better align with adult definitions, new clinical practice guidelines were also published for children. The American Academy of Pediatrics clinical practice guidelines for the management of elevated BP in children replace the 2004 fourth report from the National Heart, Lung, and Blood Institute.
Objectives
To assess the consequences of the American Academy of Pediatrics clinical practice guidelines for the management of elevated BP in children on the prevalence and severity of elevated BP among children and to characterize risk factors for children with new-onset hypertension or a worsening in clinical stage (“reclassified upward”).
Design, Setting, and Participants
This study applied both sets of guidelines to classify BP in 15 647 generally healthy, low-risk children aged 5 to 18 years from National Health and Nutrition Examination Surveys (from January 1, 1999, to December 31, 2014). In the case-control portion of the study, children whose BP was reclassified upward (cases) were matched for sex, age, and height with controls with normal BP. Anthropometric and laboratory risk factors were compared, and age- and sex-specific z scores for weight, waist circumference, and body mass index were calculated. Blood pressure was measured by auscultation by trained personnel. After the child rested quietly for 5 minutes, 3 to 4 consecutive BP readings were recorded.
Main Outcomes and Measures
Blood pressure percentiles and clinical classification based on either the 2017 American Academy of Pediatrics guidelines or the 2004 National Heart, Lung, and Blood Institute report.
Results
Among the 15 647 children in the study (7799 girls and 7848 boys; mean [SD] age, 13.4 [2.8] years), based on the American Academy of Pediatrics guidelines, the estimated (weighted) population prevalence of elevated BP increased from 11.8% (95% CI, 11.1%-13.0%) to 14.2% (95% CI, 13.4%-15.0%). Overall, 905 of 15 584 children (5.8%) had newly diagnosed hypertension (n = 381) or a worsening in clinical stage (n = 524), which represents a substantial increase in disease burden for the health care system. Children whose BP was reclassified upward were more likely to be overweight or obese, with higher z scores for weight, waist circumference, and body mass index. The prevalence of abnormal laboratory test results was also increased, with adverse lipid profiles and increased hemoglobin A1c levels (prediabetes).
Conclusions and Relevance
Clustering of cardiovascular risk factors in otherwise healthy US children suggests that those whose BP was reclassified represent a high-risk population whose cardiovascular risk may previously have been underestimated.
This study uses NHANES data to characterize changes in population prevalence of hypertension after publication in 2017 of the American Academy of Pediatrics’ (AAP) clinical practice guideline for screening and management of high blood pressure in children and adolescents.
Key Points
Question
What are the consequences of the new American Academy of Pediatrics clinical practice guidelines on the prevalence and severity of elevated blood pressure among US children?
Finding
In this cohort study of 15 647 children, the population prevalence of elevated blood pressure increased from 11.8% to 14.2%; overall, 905 children (5.8%) had newly diagnosed hypertension (n = 381) or a worsening in clinical stage (n = 524), a substantial increase in disease burden. Children whose blood pressure was reclassified upward were more likely to be overweight or obese, with adverse lipid profiles and increased hemoglobin A1c levels (prediabetes).
Meaning
Clustering of cardiovascular risk factors suggests that children whose blood pressure has been reclassified represent a high-risk population whose cardiovascular risk may previously have been underestimated.
Introduction
In August 2017, new clinical practice guidelines for the diagnosis and management of elevated blood pressure (BP) in children were published by the American Academy of Pediatrics (AAP) and the American Heart Association (AHA)1 to replace those previously developed in the fourth report from the National Institutes of Health’s National Heart, Lung, and Blood Institute (NIH/NHLBI) in 2004.2 Developed by the AAP Subcommittee on Screening and Management of High Blood Pressure in Children, the new BP norms are based on the same core data set (ie, 49 967 children from the 1996 National High Blood Pressure Education Program Working Group).3 The new norms differ in important respects.1,4 To minimize bias from their higher BP readings, children who were overweight or obese (ie, body mass index [BMI] z score >1 or percentile >85%)5,6 were excluded from the reference data, shifting the percentile curves downward.1,4 As shown in Table 1,1,2 new cutoffs were developed to better define elevated BP (90th-95th percentile values, previously called prehypertension), stage 1 hypertension, and stage 2 hypertension. The definitions of stage 1 and stage 2 hypertension were specifically chosen to align with new 2017 adult guidelines from the American College of Cardiology (ACC).7,8 The fourth report from the NIH/NHLBI2 provided polynomial regression equations for calculating each child’s BP percentile as a function of measured BP, age, sex, and height z score. The new guidelines are based on the 2008 reanalysis by Rosner et al,4 which applied quantile regression with segmented natural splines to define each child’s BP percentiles (1-99) as a function of sex, age, and height for comparison with the measured BP.
Table 1. Classification of BP by 2004 NIH/NHLBI and 2017 AAP Guidelinesa.
| NIH/NHLBI 2004 | AAP 2017 for Children 1-13 y | AAP 2017 for Children ≥13 y | |||
|---|---|---|---|---|---|
| Classification | SBP/DBP Percentile | Classification | SBP/DBP Percentile | Classification | Absolute Threshold |
| Normal | <90th | Normal | <90th | Normal | <120/<80 mm Hg |
| Prehypertension | 90th to <95th, Or if BP exceeds 120/80 mm Hg, even if <90th, up to <95th |
Elevated BP | ≥90th to <95th Or 120/80 mm Hg to <95th (whichever is lower) |
Elevated BP | 120/<80 to 129/<80 mm Hg |
| Stage 1 hypertension | 95th-99th Plus 5 mm Hg | Stage 1 hypertension | ≥95th to <95th Plus 12 mm Hg or 130/80-139/89 mm Hg (whichever is lower) |
Stage 1 hypertension | 130/80 to 139/89 mm Hg |
| Stage 2 hypertension | >99th Plus 5 mm Hg | Stage 2 hypertension | ≥95th Plus 12 mm Hg or ≥140/90 mm Hg (whichever is lower) |
Stage 2 hypertension | ≥140/≥90 mm Hg |
For adults, the November 2017 report of the ACC/AHA Task Force on Clinical Practice Guidelines was the first major redefinition of BP since 2003.7,8 Muntner et al9 suggest that the proportion of US adults with elevated BP has increased from 32% to 46%. For children and adolescents, it is difficult to anticipate the net effect of changes in both population percentiles and diagnostic cutoffs. Consequently, our primary objective was to assess the consequences of the new guidelines on the prevalence and severity of elevated BP in an unselected and generally healthy sample of US children aged 5 to 18 years from the 1999-2014 National Health and Nutrition Examination Surveys (NHANES) with ausculatory BP measured in a single ambulatory sitting. Our secondary objectives used a case-control design to characterize clinical and laboratory risk factors for children whose BP level was reclassified upward (ie, those who developed new-onset hypertension or were assigned a more advanced stage under the new 2017 guidelines).
Methods
Data were drawn from 8 biennial NHANES cycles A to H from January 1, 1999, to December 31, 2014, from the Centers for Disease Control and Prevention (CDC) repository, which includes data on cross-linked demographics, diet, physical examinations, laboratory values, and survey data sets.10 For children, anthropometric measurements were collected using a standardized measurement protocol11; in brief, calibrated stadiometer heights were measured to the nearest 0.1 cm by trained staff. Weight in kilograms and BMI (calculated as weight in kilograms divided by height in meters squared) were recorded to 1 decimal place. A snug tape measure was used to measure waist circumference to the closest 0.1 cm after palpating and marking the iliac crests in the midaxillary lines while participants placed their hands on their opposite shoulders. Blood pressure was measured by auscultation by trained and certified personnel. Participants were required to rest quietly in a seated position for 5 minutes in the mobile examination center. After determination of maximum inflation pressures, 3 and sometimes 4 consecutive BP readings were recorded; means were calculated after dropping the first measurement. Ethics approval was obtained from the Health Research Ethics Board of the University of Manitoba’s Faculty of Medicine for the use of anonymous data from an existing database for epidemiologic investigations.
Age- and sex-specific z scores were calculated for height, weight, and BMI using LMS (Lambda Mu Sigma) tables from both the CDC and the World Health Organization (WHO).5,6,12 The z scores for waist circumference and the waist to height ratio were based on NHANES III reference data and are generally more strongly associated with cardiometabolic risks than the z scores for BMI.13,14,15 For both the 2004 NIH/NHLBI and the 2017 AAP references, age-, sex-, and height-specific BP percentiles were calculated for systolic BP (SBP) and diastolic BP (DBP) and classified per Table 1.1,2,4 High BP is here defined as elevated, stage 1, or stage 2 levels.
To assess cardiovascular risk, laboratory data were pooled and merged with anthropometric measures for all participants aged 5 to 18 years in NHANES cycles A to H (1999-2014), with details available in the individual survey manuals.11 Laboratory data were analyzed for total cholesterol (participants aged 6-18 years), high-density lipoprotein cholesterol (participants aged 6-18 years), low-density lipoprotein (LDL) cholesterol measured while participants were fasting (participants aged 12-18 years), triglycerides measured while participants were fasting (participants aged 12-18 years), and hemoglobin A1c (participants aged 12-18 years). For each measure, abnormal cutpoints were defined by the NIH/NHLBI Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents16 and the American Diabetes Association. Defining criteria were a total cholesterol level of 200 mg/dL or higher (to convert to millimoles per liter, multiply by 0.0259), an LDL cholesterol level of 130 mg/dL or higher (to convert to millimoles per liter, multiply by 0.0259), a high-density lipoprotein cholesterol level of lower than 40 mg/dL (to convert to millimoles per liter, multiply by 0.0259), and a triglyceride level of 100 mg/dL or higher (to convert to millimoles per liter, multiply by 0.0113) for children aged 9 years or younger or of 130 mg/dL or more for those older than 9 years. For both children and adults, the American Diabetes Association defines a hemoglobin A1c level of higher than 5.6% as abnormal (to convert to proportion of total hemoglobin, multiply by 0.01 [based on the AMA Manual of Style]; to convert to millimoles per mole, multiply by 10.93 and subtract 23.5 [based on the International Federation of Clinical Chemistry and Laboratory Medicine (http://www.ifcchba1c.net/node/32)]), with 5.6% to 6.4% considered prediabetes, and higher than 6.5% as overt diabetes mellitus.17 Race/ethnicity categories were defined as follows: European American (white), African American (black), Mexican American, other Hispanic, and other.10
Study Sample
Because children in NHANES are generally healthy, they are frequently used to develop normative references for anthropometric and physiological measures.1,5,6,12,13 The 8 survey cycles include data on 82 091 respondents aged 2 to 90 years, with 21 895 respondents between the ages of 5 and 18 years. After removing 6248 children missing data on height, SBP, or DBP, the final sample consisted of 15 647 children.
Statistical Analysis
Statistical analyses were performed in R, version 3.4.2,18 with a 2-sided P < .05 considered statistically significant. Continuous variables are summarized by the median and interquartile range; mean values were compared by a paired t test. Categorical variables were reported as percentages with 95% CIs and compared by χ2 or Fisher exact tests. Agreement between the 2 rating systems was assessed with the Cohen κ, a 0 to 1 measure of categorical agreement above that expected by chance. Blood pressure percentiles under the 2 sets of guidelines were compared by Bland-Altman limits of agreement,19 where the mean discrepancy measures systematic bias and the 95% limits of agreement reflect discrepancies likely to be seen in day-to-day practice.
To properly account for multistage sampling, NHANES provides identifiers for primary sampling units and strata. To account for nonresponse and undercoverage and to permit valid population inferences, they also furnish inverse-probability sample weights for the mobile examination center. These weights were combined as recommended for analysis of NHANES subsets,20 using the R survey package to estimate population parameters (demographics, hexagonal heat maps, Cohen κ, and Bland-Altman limits of agreement). In comparing BP classification under both sets of guidelines, children whose BP readings were reclassified at a higher level under the 2017 guidelines were considered “reclassified upward” and treated as cases for a case-control comparison. Each case (n = 905) was matched for sex, age (year), and height (CDC quintile) with a randomly selected control (n = 13 207) whose BP readings were normal based on both sets of guidelines. The case-control analysis was an unweighted, paired comparison of sample patients whose BP levels were reclassified upward vs matched, normotensive controls.
Results
The demographic and clinical characteristics of the 15 647 children studied are shown in Table 2,4,20,21 where it can be seen that the sample prevalence of high BP increased from 2006 of 15 647 children under the NIH/NHLBI definition (12.8%; 95% CI, 12.3%-13.0%) to 2337 of 15 584 children with the AAP definition (15.0%; 95% CI, 14.4%-16.0%) (P < .001). The estimated (weighted) population prevalence similarly increased from 11.8% (95% CI, 11.1%-13.0%) to 14.2% (95% CI, 13.4%-15.0%). Body mass index and weight z scores were significantly larger based on WHO reference charts compared with the CDC reference charts (BMI z scores, 0.65 vs 0.55; P < .001; weight z scores, 0.60 vs 0.56; P < .001), and the proportion of children who were overweight and obese (BMI z score >1) or just obese (BMI z score >2) increased significantly as a result (Table 2).
Table 2. Demographic and Clinical Characteristics of Children Aged 5 to 18 Years in NHANES With Measured Height, SBP, and DBPa.
| Characteristic | Sample, No.b | Population (Weighted)c | P Valued |
|---|---|---|---|
| Male, % (95% CI) | 7848 | 50.3 (49.2 to 51.0) | NA |
| Age, median (IQR), y | 13.4 | 13.2 (10.8 to 15.7) | NA |
| Race/ethnicity, % | |||
| White | 4171 | 58.6 | NA |
| Black | 4555 | 14.4 | |
| Mexican American | 4680 | 13.1 | |
| Hispanic | 1113 | 6.6 | |
| Other | 1128 | 7.3 | |
| Income (INDFMPIR), median (IQR)e | 1.57 | 2.33 (1.10 to 4.04) | NA |
| Height z score, median (IQR) | |||
| CDC | 0.14 | 0.20 (−0.47 to 0.89) | <.001 |
| WHO | 0.18 | 0.25 (−0.42 to 0.95) | |
| Weight z score, median (IQR) | |||
| CDC (n = 15 617) | 0.61 | 0.56 (−0.21 to 1.37) | <.001 |
| WHO (n = 15 617) | 0.65 | 0.60 (−0.20 to 1.54) | |
| BMI z score, median (IQR) | |||
| CDC (n = 15 617) | 0.64 | 0.55 (−0.23 to 1.40) | <.001 |
| WHO (n = 15 617) | 0.76 | 0.65 (−0.22 to 1.71) | |
| WC z score (n = 15 420) | 0.42 | 0.39 (−0.27 to 1.17) | NA |
| WHtR z score (n = 15 420) | 0.23 | 0.16 (−0.50 to 1.00) | NA |
| Overweight or obese, % (95% CI) | |||
| CDC (n = 15 617) | 6048 | 35.9 (34.9 to 37.0) | <.001 |
| WHO (n = 15 617) | 6750 | 40.6 (39.5 to 42.0) | |
| Obese, % (95% CI) | |||
| CDC (n = 15 617) | 1873 | 10.3 (9.7 to 11.0) | <.001 |
| WHO (n = 15 617) | 3408 | 19.5 (18.7 to 20) | |
| SBP percentile (95% CI) | |||
| NHLBI | 39 | 38 (19 to 61) | <.001 |
| AAP (n = 15 584) | 46 | 46 (23 to 69) | |
| DBP percentile (95% CI) | |||
| NHLBI | 33 | 33 (12 to 58) | <.001 |
| AAP (n = 15 584) | 32 | 32 (12 to 60) | |
| 90th-95th BP percentiles, % (95% CI) | |||
| NHLBIf | 1569 | 9.1 (8.6 to 10.0) | <.001 |
| AAP (n = 15 584)g | 1450 | 8.7 (8.1 to 9.0) | |
| Stage 1, % (95% CI) | |||
| NHLBI | 426 | 2.6 (2.3 to 3.0) | <.001 |
| AAP (n = 15 584) | 822 | 5.1 (4.6 to 6.0) | |
| Stage 2, % (95% CI) | |||
| NHLBI | 11 | 0.06 (0.03 to 0.09) | <.001 |
| AAP (n = 15 584) | 65 | 0.4 (0.3 to 1.0) | |
| “High BP,” % (95% CI) | |||
| NHLBI | 2006 | 11.8 (11.1 to 13.0) | <.001 |
| AAP (n = 15 584) | 2337 | 14.2 (13.4 to 15.0) |
Abbreviations: AAP, American Academy of Pediatrics; BMI, body mass index; CDC, Centers for Disease Control and Prevention; BP, blood pressure; DBP, diastolic blood pressure; INDFMPIR, ratio of family income to poverty; IQR, interquartile range; NHANES, National Health and Nutrition Examination Survey; NHLBI, National Heart, Lung, and Blood Institute; SBP, systolic blood pressure; WC, waist circumference; WHO, World Health Organization; WHtR, waist to height ratio.
For a total of 15 647 children, unless otherwise indicated.
Sample column reports number for categorical variables or median for continuous variables.
Corresponding weighted population estimates20 are reported as percentage (95% CI) or median (IQR).
Paired t tests for continuous variables or χ2 tests of proportions for categorical variables, in both cases weighted for population estimates.
Index for the ratio of family income to poverty defined by the Department of Health and Human Services.21
The NHLBI defines the 90th to 95th BP percentiles as prehypertension.
The AAP defines the 90th to 95th BP percentiles as “elevated BP.” For AAP BP percentiles, the number of children was 15 584 because 63 participants could not be assigned BP percentiles with “outlier” heights (z score <−3.09 or >3.09).4
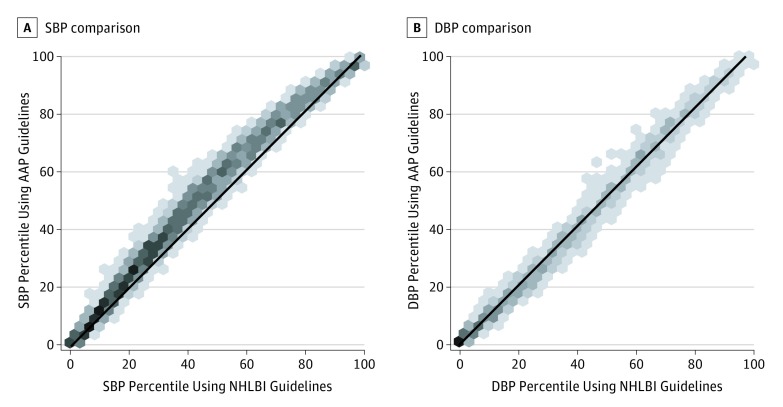
Compared with the 2004 fourth report, the mean SBP percentile was higher with the 2017 guidelines; the proportions of children with stages 1 or 2 levels increased significantly. The association between BP percentiles under the 2 systems is illustrated by the heatmap (Figure), with the diagonal line of identity for comparison. For SBP and DBP percentiles, the Bland-Altman mean error (bias) and 95% limits of agreement were 5.3 (−1.0 to 13.0) for SBP and 0.7 (–5.0 to 6.0) for DBP (AAP-NHLBI). These differences were statistically significant in each case (P < .001 by 1-sample t test), although the diastolic bias is clinically negligible.19
Figure. Comparison of Blood Pressure Percentiles in the 2017 American Academy of Pediatrics (AAP) vs 2004 National Institutes of Health’s National Heart, Lung, and Blood Institute (NIH/NHLBI) Guidelines.
A, Systolic blood pressure (SBP). B, Diastolic blood pressure (DBP). To resolve overlapping points, individual points are first grouped in hexagonal bins, with darker shading as bin counts increase. The solid line indicates the line of identity.
Overall, 905 of 15 584 children (5.8%) in the cohort were reclassified upward under the new AAP guidelines compared with the 2004 NIH/NHLBI report (Table 3). Of these, 381 were deemed normotensive by NHLBI but are now considered to have elevated (n = 368) or stage 1 levels (n = 13) by AAP criteria. In addition, 470 children with prehypertension were reclassified as stage 1 by AAP guidelines, and an additional 54 children whose BP readings were previously consistent with stage 1 levels were reclassified as stage 2. Few children regressed to a lower level (40 from prehypertension to normal and 33 from stage 1 to elevated). A total of 13 207 (84.8%) children were deemed to be normotensive by both criteria. The overall agreement between assigned categories in Table 3 is given by κ = 0.73 (95% CI, 0.71-0.75; P < .001).
Table 3. Reclassification Matrix Based on Children’s 2004 or 2017 BP Classificationa.
| NIH/NHLBI | American Academy of Pediatrics | |||
|---|---|---|---|---|
| Normal BP | Elevated BP | Stage 1 | Stage 2 | |
| Normal | 13 207 (97.2) | 368 (2.7) | 13 (0.1) | 0 |
| Prehypertension | 40 (2.6) | 1049 (67.3) | 470 (30.1) | 0 |
| Stage 1 | 0 | 33 (7.7) | 339 (79.6) | 54 (12.7) |
| Stage 2 | 0 | 0 | 0 | 11 (100) |
Abbreviations: BP, blood pressure; NIH/NHLBI, National Institutes of Health’s National Heart, Lung, and Blood Institute.
For 15 584 children. The values in parentheses are row percentages.
Compared with the normotensive children (Table 3, N = 13 207), those reclassified upward were more likely to be male (62.7% [567 of 905] vs 47.6% [6291 of 13 207]; P < .001) and slightly taller (mean [SD] CDC height z score, 0.44 [0.95] vs 0.11 [1.0]; P < .001). The mean (SD) age of those reclassified upward was 12.2 [3.4] years vs 13.2 [2.8] years for controls (P < .001).
To better characterize the 905 children with this additional disease burden, cases are compared with sex-, age-, and height-matched controls (Table 4). The groups differed significantly in anthropometric measures of adiposity, including z scores for BMI, weight, waist circumference, and waist to height ratio. As a result, the proportion of children who were overweight or obese (BMI z score >1) was 55.9% among those reclassified upward (504 of 901) vs 35.0% among controls (315 of 901) (P < .001), and the proportion who were obese (BMI z score >2) was 23.5% among those reclassified upward (212 of 901) vs 11.6% among controls (105 of 901) (P < .001). These proportions increased further with the use of WHO growth charts and diagnostic criteria.
Table 4. Clinical and Laboratory Characteristics of the 905 Cases Reclassified Upward vs Normotensive Controls Matched for Age, Sex, and Heighta.
| Characteristic | Cases (n = 905) | Controls (n = 905) | P Value |
|---|---|---|---|
| Race/ethnicity, No. (%) | |||
| White | 246 (27.2) | 248 (27.4) | .20 |
| Black | 289 (31.9) | 282 (31.2) | |
| Mexican American | 259 (28.6) | 230 (25.4) | |
| Hispanic | 52 (5.7) | 70 (7.7) | |
| Other | 59 (6.5) | 74 (8.2) | |
| SBP percentile, mean (SE) | |||
| NHLBI | 76.6 (0.7) | 35.1 (0.7) | <.001 |
| AAP | 82.1 (0.7) | 41.4 (0.8) | <.001 |
| DBP percentile, mean (SE) | |||
| NHLBI | 54.3 (1.1) | 34.2 (0.8) | <.001 |
| AAP | 55.9 (1.2) | 32.8 (0.9) | <.001 |
| Weight z score, mean (SE) | |||
| CDC | 1.10 (0.04) | 0.61 (0.04) | <.001 |
| WHO | 1.40 (0.05) | 0.81 (0.05) | <.001 |
| BMI z score, mean (SE) | |||
| CDC | 1.04 (0.04) | 0.50 (0.04) | <.001 |
| WHO | 1.45 (0.05) | 0.75 (0.05) | <.001 |
| WC z score, mean (SE) | 0.80 (0.03) | 0.29 (0.03) | <.001 |
| WHtR z score, mean (SE) | 0.60 (0.04) | 0.15 (0.04) | <.001 |
| Overweight or obese (CDC), No./Total No. | 504/901 | 315/901 | <.001 |
| % (SE) | 55.9 (0.4) | 35.0 (0.4) | |
| Obese (CDC), No./Total No. | 212/901 | 105/901 | <.001 |
| % (SE) | 23.5 (0.4) | 11.6 (0.4) | |
| Overweight or obese (WHO), No./Total No. | 548/901 | 355/901 | <.001 |
| % (SE) | 60.8 (0.4) | 39.4 (0.4) | |
| Obese, (WHO), No./Total No. | 356/901 | 170/901 | <.001 |
| % (SE) | 39.5 (0.4) | 18.9 (0.3) | |
| Income (INDFMPIR), mean (SE)b | 1.98 (0.05) | 2.14 (0.05) | .03 |
| Total cholesterol, mean (SE), mg/dL | 164.9 (1.0) | 159.9 (1.0) | .001 |
| HDL-C, mean (SE), mg/dL | 50.7 (0.4) | 53.2 (0.4) | <.001 |
| LDC-C, mean (SE), mg/dL | 96.7 (1.0) | 91.0 (0.8) | .05 |
| Hemoglobin A1c, mean (SE), % | 5.22 (0.02) | 5.20 (0.01 | .60 |
| Triglycerides, mean (SE), mg/dL | 92.7 (1.7) | 80.4 (1.6) | .04 |
| High total cholesterol, No./Total No.c | 96/776 | 75/804 | .06 |
| % (SE) | 12.4 (1.2) | 9.3 (1.0) | |
| Low HDL-C level, No./Total No.d | 105/653 | 110/683 | >.99 |
| % (SE) | 16.1 (1.4) | 16.1 (1.4) | |
| High LDL-C level, No./Total No.e | 27/222 | 9/229 | .002 |
| % (SE) | 12.2 (2.3) | 3.9 (1.3) | |
| High hemoglobin A1c level, No./Total No.f | 12/349 | 2/347 | .02 |
| % (SE) | 3.4 (1.0) | 0.6 (0.4) | |
| High triglyceride level, No./Total No.g | 52/230 | 25/234 | <.001 |
| % (SE) | 22.6 (2.8) | 10.7 (2.0) |
Abbreviations: AAP, American Academy of Pediatrics; BMI, body mass index; CDC, Centers for Disease Control and Prevention; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; INDFMPIR, ratio of family income to poverty; LDL-C, low-density lipoprotein cholesterol; NHLBI, National Heart, Lung, and Blood Institute; SBP, systolic blood pressure; WC, waist circumference; WHO, World Health Organization; WHtR, waist-to-height ratio.
SI conversion factors: To convert total cholesterol, HDL-C, and LDL-C to millimoles per liter, multiply by 0.0259; triglycerides to millimoles per liter, multiply by 0.0113; and hemoglobin A1c to proportion of total hemoglobin, multiply by 0.01 (based on the AMA Manual of Style); to convert to millimoles per mole, multiply by 10.93 and subtract 23.5 (based on the International Federation of Clinical Chemistry and Laboratory Medicine [http://www.ifcchba1c.net/node/32]).
Fasting blood tests were not performed for participants younger than 12 years, and laboratory data were not available on all participants. Descriptive statistics are based on the cited total numbers, with paired comparisons based on the smaller of the 2 values.
Index for the ratio of family income to poverty defined by the Department of Health and Human Services.21
High total cholesterol level (≥200 mg/dL).
Low HDL-C level (<40 mg/dL).
High LDL-C level (≥130 mg/dL).
High hemoglobin A1c level (>5.6%).
High triglyceride level (≥100 mg/dL for children ≤9 years or ≥130 mg/dL for children >9 years).
Among the children reclassified upward, there were small differences in mean concentrations of total cholesterol, LDL cholesterol, high-density lipoprotein cholesterol, and triglycerides compared with controls (Table 4). Using clinical cutpoints from the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents16 and the American Diabetes Association,17 the cases experienced more elevated concentrations of total cholesterol (96 of 776 [12.4%] vs 75 of 804 [9.3%]; P = .06), LDL cholesterol (27 of 222 [12.2%] vs 9 of 229 [3.9%]; P = .002), triglycerides (52 of 230 [22.6%] vs 25 of 234 [10.7%]; P < .001), and hemoglobin A1c (12 of 349 [3.4%] vs 2 of 347 [0.6%]; P = .02). There were only 126 cases and 140 controls with complete measures on BMI z scores, triglycerides, total cholesterol, LDL cholesterol, high-density lipoprotein cholesterol, and hemoglobin A1c, which could be used to examine the prevalence of concurrent cardiac risk factors. Being overweight or obese was the most common additional risk factor. Overall, 67.5% of cases with complete data (85 of 126) had other risk factors (in addition to elevated BP) vs 35% of controls (49 of 140), and 19.0% of cases with complete data (24 of 126) had more than 2 additional risk factors vs 3.6% of controls (5 of 140) (P < .001).
Discussion
Overall, the new guidelines have increased the prevalence of elevated BP levels in this cohort from 12.8% (95% CI, 12.3%-13.0%) to 15.0% (95% CI, 14.4%-16.0%), with a comparable increase in the estimated population prevalence, from 11.8% (95% CI, 11.1%-13.0%) to 14.2% (95% CI, 13.4%-15.0%). Perhaps more importantly, 5.8% of the children in the cohort (905 of 15 584) have been reclassified with either new-onset hypertension or a more severe clinical stage of hypertension, and only 73 (0.5%) regressed to a lower level. Based on recommendations from the 2017 AAP subcommittee report, the mean of multiple ausculatory BP readings at a single visit is used to formulate follow-up instructions; for these children, reclassification has consequences.1 For those with elevated BP, lifestyle modifications are recommended (healthy diet, sleep, and physical activity), and the BP is to be reassessed after 6 months instead of 1 year as in children with normal BP. Similarly, asymptomatic children with stage 1 levels should be reassessed in 1 to 2 weeks, and those with stage 2 levels require more urgent evaluation or referral to a subspecialist within the week. Although some of these children will subsequently have normal BP or have “white-coat hypertension” (elevated BP when measured in a medical environment), the persistence of elevated BP or hypertension should prompt additional evaluation (eg, echocardiography or 24-hour ambulatory monitoring) and further treatment.
With more than 5% of generally healthy individuals reclassified upward under the new guidelines, the additional disease burden faced by caregivers, families, and patients is nontrivial. As the AAP subcommittee notes,1 long-term follow-up studies of cardiovascular morbidity and mortality will ultimately be needed to precisely define cardiovascular risk. In the shorter term, their approach to risk stratification relies on careful alignment with adult cutoffs at age 19 years; this strategy is based on the fact that childhood BP typically tracks into adulthood, and children with elevated BP are more likely to develop primary hypertension and metabolic syndrome as adults.22,23,24,25 Because pediatric cardiovascular risk factors are known to cluster,26 we might also examine the risk profiles of children with either new-onset hypertension or worsening of their clinical stage, which was the goal of our case-control study.
Not surprisingly, being overweight and obese (BMI z score >1) or just obesity (BMI z score >2) were significantly more common among cases. These conditions have well-documented implications1,27; a recent study of 2.3 million Israeli adolescents showed that a normal adolescent BMI between the 50th and 74th percentiles (BMI z score, 0-0.64) was associated with increased cardiovascular and all-cause mortality during 40 years of follow-up, with a hazard ratio for cardiovascular mortality of 4.1 (95% CI, 3.1-5.4) after 30 to 40 years.27 Because the prevalence of overweight and obesity was increased with use of the WHO reference growth charts for school-age children, the CDC charts may be underestimating cardiovascular risk.6 In adults and children, central adiposity (as measured by waist circumference and waist to height ratio) appear to have greater prognostic significance than BMI alone13,14,15; their increased z scores therefore add to concerns regarding weight-related risk.
Known risk factors determined by laboratory test results were also noted with increased frequency in the cases, including hypercholesterolemia (elevated LDL cholesterol), hypertriglyceridemia, and prediabetes. Like overweight and obesity, these laboratory test results may have their own effects on BP or reflect a common etiology associated with the individual’s lifestyle.28,29,30 Differences in risk profiles for laboratory test results were more clearly seen when age-specific cutoffs were used to identify abnormal values. For those with complete data on laboratory measures, 2 in 3 cases had additional cardiac risk factors, compared with only 1 in 3 controls. Moreover, 1 in 5 cases had more than 2 additional risk factors, compared with only 1 in 25 controls. To put this in context, the AHA has identified “Life’s Simple 7” as key contributors to cardiovascular health, including 4 ideal health behaviors (not smoking, achieving a normal BMI, engaging in physical activity, and eating a healthy diet) and 3 ideal health factors (normal total cholesterol, normal blood glucose, and normal BP).31 We should also bear in mind that analyses of the NHANES databases using the NHLBI definitions of hypertension generally show increasing prevalence over time, with higher rates among children who are overweight or obese, male, adolescent, and African American or Hispanic.29,32,33,34 Although the rate of dyslipidemia appears to be declining,29 worrisome trends are further exacerbated by a low prevalence of ideal cardiovascular health behaviors, particularly among adolescents.35
To our knowledge, there are no other studies in pediatrics to date to assess the effect of the new criteria for elevated BP; we noted a modest increase from 11.8% to 14.2% in the population prevalence of elevated BP. The effect of the more stringent 2017 criteria for adults is more dramatic, with an increase from 32% to 46% with elevated BP.9 And while most reclassified adults do not require new medications, long-term studies will be required to assess the effect of these changes on cardiovascular outcomes, which will no doubt result in further refinement of the BP guidelines for children.
The new 2017 AAP guidelines were developed using a reference population that excluded children with a BMI z score greater than 1.4 By excluding those with higher BP levels owing to overweight or obesity, the AAP subcommittee sought to create a normative standard rather than a reference.1,6 A similar approach was taken with the WHO growth charts for individuals aged 5 to 19 years,6 which were based on the same core data as the CDC 2000 charts, except that the WHO dropped more recent data (1973-1994) and excluded children with “unhealthy” weight to height ratios. In Table 2, this methodological difference leads to a mean (SD) discrepancy of 0.24 (0.34) in BMI z scores (P < .001 by paired t test) when comparing the WHO and CDC measures.6,36
For the same reason, the BP percentiles assigned by the 2017 AAP guidelines will generally be higher than those from the 2004 report.1,4 This difference is clear when both are applied in our NHANES cohort of children aged 5 to 18 years (Figure) and is particularly true for SBP, where the Bland-Altman bias was 5.3 percentile points (95% CI, −1.0 to 13.0; AAP-NHLBI). The bias in DBP percentiles in clinical practice is less. It is of course difficult to predict a priori the net effect of the new guidelines because the new percentile charts are combined with new clinical thresholds in Table 1 to define normal and high BP.
Strengths and Limitations
The strengths of this study include a large sample with 3 to 4 BP readings measured by the criterion standard of auscultation in a single sitting by trained professionals. Participants in NHANES are generally unselected and at low risk for conditions that might predispose to secondary hypertension. Detailed anthropometric and laboratory measures allowed for a comprehensive assessment of cardiovascular risk. The limitations include insufficient numbers for the assessment of race-, sex-, and age-specific differences; lack of information pertaining to medical history, family history, and comorbidities; and no long-term follow-up.
Conclusions
Among the 15 647 children aged 5 to 18 years who participated in biennial NHANES cycles between 1999 and 2016, the 2017 AAP guidelines for the screening and management of high BP saw an upward shift in BP percentiles, particularly for SBP. When combined with new diagnostic thresholds that better align with adult guidelines, the prevalence of high BP in this cohort increased from a mean (SE) of 12.8% (0.3%) to 15.0% (0.3%). In addition, we identified 905 of 15 584 children (mean [SE], 5.8% [0.2%]) who were reclassified upward with newly diagnosed high BP (n = 381) or a worsening clinical stage (n = 524). Because reclassification necessitates additional follow-up and possibly treatment, it represents a new and significant disease burden for practitioners and patients alike. After matching by sex, age, and height with controls with normal BP, the children who were reclassified upward were more likely to be overweight or obese and to experience an increased prevalence of risk factors as determined by laboratory test results, including adverse lipid profiles (elevated LDL cholesterol and triglycerides) and prediabetes. These data suggest that we may previously have been underestimating cardiovascular risk in otherwise healthy US children. Clustering of risk factors suggests that reclassified children represent a high-risk population, which serves to validate the new, more stringent 2017 guidelines.
References
- 1.Flynn JT, Kaelber DC, Baker-Smith CM, et al. ; Subcommittee on Screening and Management of High Blood Pressure in Children . Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. [DOI] [PubMed] [Google Scholar]
- 2.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2)(Suppl 4th Report):555-576. [PubMed] [Google Scholar]
- 3.National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;98(4, pt 1):649-658. [PubMed] [Google Scholar]
- 4.Rosner B, Cook N, Portman R, Daniels S, Falkner B. Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am J Epidemiol. 2008;167(6):653-666. [DOI] [PubMed] [Google Scholar]
- 5.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1-190. [PubMed] [Google Scholar]
- 6.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online November 7, 2017]. J Am Coll Cardiol. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 8.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online November 7, 2017]. J Am Coll Cardiol. doi: 10.1016/j.jacc.2017.11.005 [DOI] [PubMed] [Google Scholar]
- 9.Muntner P, Carey RM, Gidding S, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018;71(2):109-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. Accessed December 5, 2017.
- 11.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: NHANES 2015-2016 examination data. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Examination&CycleBeginYear=2015. Accessed December 5, 2017.
- 12.Rodd C, Metzger DL, Sharma A; Canadian Pediatric Endocrine Group (CPEG) Working Committee for National Growth Charts . Extending World Health Organization weight-for-age reference curves to older children. BMC Pediatr. 2014;14:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma AK, Metzger DL, Daymont C, Hadjiyannakis S, Rodd CJ. LMS tables for waist-circumference and waist-height ratio Z-scores in children aged 5-19 y in NHANES III: association with cardio-metabolic risks. Pediatr Res. 2015;78(6):723-729. [DOI] [PubMed] [Google Scholar]
- 14.Khoury M, Manlhiot C, McCrindle BW. Role of the waist/height ratio in the cardiometabolic risk assessment of children classified by body mass index. J Am Coll Cardiol. 2013;62(8):742-751. [DOI] [PubMed] [Google Scholar]
- 15.Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275-286. [DOI] [PubMed] [Google Scholar]
- 16.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute . Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213-S256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Diabetes Association 2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40(suppl 1):S11-S24. [DOI] [PubMed] [Google Scholar]
- 18.R Core Team R Foundation for Statistical Computing. R: A language and environment for statistical computing. http://www.R-project.org/. Accessed December 10, 2017.
- 19.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307-310. [PubMed] [Google Scholar]
- 20.Lumley T. Chapter 5. In: Complex Surveys: A Guide to Analysis Using R. Wiley Series in Survey Methodology. Hoboken, New Jersey: Wiley and Sons; 2010:98-104. [Google Scholar]
- 21.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: 2015-2016 data documentation, codebook, and frequencies: demographic variables and sample weights. https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/DEMO_I.htm. Published September 2017. Accessed December 5, 2017.
- 22.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119(2):237-246. [DOI] [PubMed] [Google Scholar]
- 23.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117(25):3171-3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Juhola J, Oikonen M, Magnussen CG, et al. Childhood physical, environmental, and genetic predictors of adult hypertension: the cardiovascular risk in young Finns study. Circulation. 2012;126(4):402-409. [DOI] [PubMed] [Google Scholar]
- 25.Juhola J, Magnussen CG, Viikari JSA, et al. Tracking of serum lipid levels, blood pressure, and body mass index from childhood to adulthood: the Cardiovascular Risk in Young Finns Study. J Pediatr. 2011;159(4):584-590. [DOI] [PubMed] [Google Scholar]
- 26.Garnett SP, Baur LA, Srinivasan S, Lee JW, Cowell CT. Body mass index and waist circumference in midchildhood and adverse cardiovascular disease risk clustering in adolescence. Am J Clin Nutr. 2007;86(3):549-555. [DOI] [PubMed] [Google Scholar]
- 27.Twig G, Yaniv G, Levine H, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med. 2016;374(25):2430-2440. [DOI] [PubMed] [Google Scholar]
- 28.Lurbe E, Torro I, Aguilar F, et al. Added impact of obesity and insulin resistance in nocturnal blood pressure elevation in children and adolescents. Hypertension. 2008;51(3):635-641. [DOI] [PubMed] [Google Scholar]
- 29.Kit BK, Kuklina E, Carroll MD, Ostchega Y, Freedman DS, Ogden CL. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999-2012. JAMA Pediatr. 2015;169(3):272-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang T, Zhang H, Li S, et al. Impact of adiposity on incident hypertension is modified by insulin resistance in adults: longitudinal observation from the Bogalusa Heart Study. Hypertension. 2016;67(1):56-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steinberger J, Daniels SR, Hagberg N, et al. ; American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; Council on Functional Genomics and Translational Biology; and Stroke Council . Cardiovascular health promotion in children: challenges and opportunities for 2020 and beyond: a scientific statement from the American Heart Association. Circulation. 2016;134(12):e236-e255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension. 2013;62(2):247-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116(13):1488-1496. [DOI] [PubMed] [Google Scholar]
- 34.Yang Q, Zhong Y, Merritt R, Cogswell ME. Trends in high blood pressure among United States adolescents across body weight category between 1988 and 2012. J Pediatr. 2016;169:166-173.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005-2010. Circulation. 2013;127(13):1369-1376. [DOI] [PubMed] [Google Scholar]
- 36.de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137(1):144-148. [DOI] [PubMed] [Google Scholar]