Abstract
Background and objective
To assess clinical outcomes after foreign body ingestion and food impaction; to identify predictors of foreign body presence at the time of endoscopy.
Methods
A prospective study including consecutive adult patients with foreign body ingestion or suspected food impaction between May 2014 and August 2016.
Results
In total, 521 patients were included, 320 with foreign body ingestion and 201 with suspected food impaction. Food impaction patients were significantly older and more frequently had a history of oesophageal disease. The foreign body was encountered in the upper digestive tract in 43% of the patients with foreign body ingestion, and food impaction was confirmed in 87%. Older age (odds ratio (OR)year 1.04, 95% confidence interval (CI) 1.02–1.06) and early presentation (ORfirst six hours 4.41, 95% CI 2.24–8.66) were independent predictors of foreign body presence, while a history of psychiatric disease was an independent predictor of food impaction (OR 6.69, 95% CI 1.66–26.9). Successful endoscopic treatment was achieved in more than 90% of the cases, with adverse events occurring in fewer than 5%. Foreign body forceps was the preferred device in foreign body ingestion, while retrieval basket and mobilisation were preferred in food impaction. The need to use more than one instrument was significantly higher in food impaction.
Conclusion
Foreign bodies are encountered at endoscopy in almost half of the cases. Older age and earlier presentation are independent predictors of its presence. Given the high proportion of patients with foreign body at endoscopy and the low risk of complications, endoscopic evaluation is probably justified in the majority of cases.
Keywords: Endoscopy, foreign body ingestion, food impaction, emergency, therapeutic endoscopy
Key summary
- Summarise the established knowledge on this subject.
- Foreign body ingestion and food impaction are one of the most frequent emergencies in gastroenterology/flexible endoscopy.
- Most studies are retrospective and evaluate foreign body ingestion and food impaction together, although they are different entities.
- Older studies suggest that the majority (80–90%) of the foreign bodies spontaneously pass the gastrointestinal tract, with a minimal risk of complications.
- There are no studies evaluating predictors of foreign body presence at endoscopy.
2. What are the significant and/or new findings of this study?
In almost half of the patients with foreign body ingestion, a foreign body is found at endoscopy.
Older age and earlier presentation to the emergency department are independent predictors of foreign body presence at endoscopy.
Endoscopic treatment is successful in the majority of cases (>90%), with a minimal risk of adverse events (<5%).
Given the high likelihood of finding the ingested foreign body at endoscopy, the high treatment success rate and the low risk of complications, endoscopy is probably justified in the majority of patients.
Introduction
Foreign body ingestion (FBI) and food impaction (FI) are frequent emergencies that can result in significant morbidity and even mortality if not treated promptly and adequately. Although FBI and FI are frequent emergencies, studies evaluating treatment strategies and their outcomes are scarce and the majority is retrospective.1–4 Indeed, the need to perform radiological exams before endoscopy, the endoscopic methods used to retrieve the foreign body or FI and the post-endoscopy attitude are generally decided on a case by case basis, based on the type, size, shape of the foreign body and also on physical examination and symptoms or signs of complications.5–10 This contributes to significant heterogeneity in attitudes and also in their reporting, with some studies reporting FBI and FI therapeutics and outcomes together although they are different entities.1–3
Endoscopy is the mainstay of diagnosis and treatment of FBI and FI, although some controversies exist concerning the indications and the best timing for its execution. Indeed, recent European guidelines report that although 10–20% of ingested foreign bodies require endoscopic removal, 80–90% of them spontaneously pass the gastrointestinal tract,7 and thus a significant proportion would not benefit from endoscopy. This estimate of 80% is based on old studies performed before the era of flexible endoscopy and when conservative treatment was the preferred management.11,12 In addition, most of the recent studies on this topic include only patients with confirmed foreign body presence at endoscopy,13 and so the proportion of patients with FBI in whom the foreign body will be encountered at endoscopy is not precisely known. Thus it is important to assess the proportion of patients with FBI in which the foreign body is encountered at endoscopy and also to identify predictors for its presence, because it can identify patients with a higher probability of actually having a foreign body in the upper digestive tract, and it can modify the threshold to perform endoscopy.
The main aims of this study were: (a) to evaluate the proportion of patients with foreign body or FI in the upper digestive tract; (b) to identify predictors of foreign body and FI presence; (c) to assess therapeutic strategies and outcomes in FBI and FI.
Methods
Selection of participants
This was a prospective cohort study including consecutive adult patients with FBI or suspected FI referred to the gastroenterology department of Centro Hospitalar do Porto between May 2014 and August 2016. Centro Hospitalar do Porto is a tertiary referral centre with a 24-hour gastroenterology emergency service. At night and on weekends, the gastroenterology department of Centro Hospitalar do Porto receives patients from other hospitals in the northern region of Portugal with gastrointestinal emergencies. Consecutive adult patients with suspected FBI or FI referred to the gastroenterology department were included in the study. No exclusion criteria were defined and all patients were included in the analysis.
Data collection included demographic and clinical variables that were registered on a predefined paper form. Clinical data included the presence of symptoms (no symptoms, dysphagia, foreign body perception, pain), history of oesophageal disease (stenosis, rings, eosinophilic oesophagitis) or psychiatric conditions (schizophrenia, dementia, major depression), previous episodes of FBI/FI, time from ingestion to presentation to the emergency department and the use of medical therapy such as glucagon. Endoscopies were performed by gastroenterology specialists and dedicated endoscopy nurses, without sedation unless there was intolerance to the procedure, in which case deep sedation with propofol was administered by an anaesthesiologist. Endoscopy findings were recorded and included the presence or absence of FBI/FI, the accessories used in endoscopic treatment, oesophageal diseases, complications and the need to use sedation. The decision to perform oesophageal biopsies in the case of FI was left at the discretion of the performing endoscopist. Patients were followed until discharge from the hospital; clinical records were also reviewed to assess if there were late adverse events/re-admissions after discharge.
Statistical analysis
Descriptive statistics included mean and standard deviation or median and interquartile range for quantitative variables and proportions for categorical variables. Continuous variables were compared with independent samples t-test or Mann–Whitney U test. Proportions were compared with chi-square test or Fisher’s exact test as adequate. Logistic regression was performed to identify significant predictors of foreign body and FI presence on endoscopy; variables entered in the logistic model (stepwise method) were age, sex and variables with P < 0.20 in univariable analysis. Adjusted odds ratios (ORs) along with 95% confidence intervals (CIs) are reported. Significance level was defined as P < 0.05 for all comparisons. Statistical analysis was performed using IBM SPSS version 22 (Armonk, NY, USA).
Results
In total, 521 patients were included (320 with FBI and 201 with suspected FI). Clinical and demographic variables are shown in Table 1. Patients with FI were significantly older (60 vs. 54 years), more frequently men (60% vs. 48%), and more frequently reported osophageal disease and previous episodes (Table 1). In the FI group, the most common oesophageal diseases were benign strictures (peptic, radiogenic or caustic; n = 26), Schatzki rings (n = 12) and malignant strictures (n = 8); only two patients had eosinophilic oesophagitis. Oesophageal disease was less prevalent in the FBI group and the most common aetiology was Schatzki rings (n = 4). The prevalence of psychiatric disorders was similar between the groups, with schizophrenia being the most frequent diagnosis in the FBI group while dementia was the most frequent in the FI group. Regarding symptoms, FI patients were more frequently symptomatic (91.5%), while in the FBI group 15.0% were asymptomatic. Foreign body perception and pain were significantly more frequent in the FBI group, while dysphagia was the predominant symptom in FI. Before endoscopy, otorhinolaryngology observation was performed in 67% of the patients with FBI, while radiology exams were performed in a minority of these patients (18.1%). Otorhinolaryngology observation and radiological exams were less frequent in the FI group (25% and 7%, respectively). The patients in the FI group submitted to radiological exams (chest X-ray in all cases) were patients with meat bolus impaction in whom there was uncertainty if the food bolus had a bone component. Deep sedation was needed in 5.0% of the cases of FI and in 6.0% of FBI patients.
Table 1.
Clinical and demographic variables.
| FBI (n = 320) | FI (n = 201) | P value | |
|---|---|---|---|
| Age, mean (SD) | 53.9 (17.8) | 60.2 (19.1) | <0.001 |
| Male gender, n (%) | 128 (40.0%) | 139 (69.2%) | <0.001 |
| Oesophageal disease | |||
| Yes | 9 (2.8%) | 61 (30.3%) | <0.001 |
| Previous episode | |||
| Yes | 28 (8.7%) | 107 (53.2%) | <0.001 |
| Psychiatric disordera | |||
| Yes | 34 (10.6%) | 20 (9.9%) | 0.823 |
| Symptoms (any) | 272 (85.0%) | 184 (91.5%) | <0.001 |
| Foreign body perception | 206 (64.4%) | 91 (45.3%) | <0.001 |
| Dysphagia | 60 (18.7%) | 142 (70.6%) | <0.001 |
| Pain | 105 (32.8%) | 22 (10.9%) | <0.001 |
| ORL observation | 215 (67.2%) | 51 (25.4%) | <0.001 |
| Radiology exams | 58 (18.1%) | 15 (7.5%) | 0.001 |
FBI: foreign body ingestion; FI: food impaction; SD: standard deviation; ORL: otorhinolaryngology specialist.
Schizophrenia, dementia or major depression.
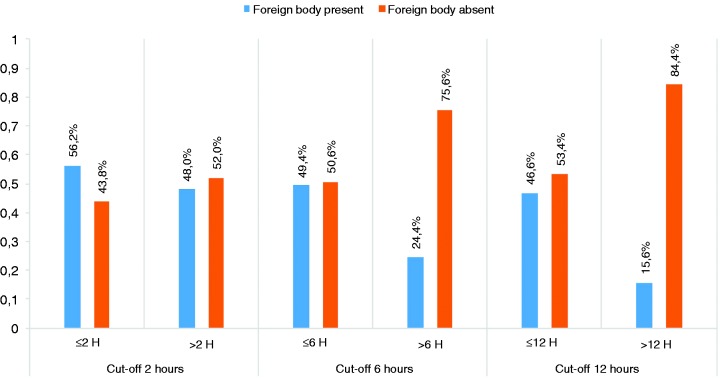
Foreign body ingestion
Of the 320 patients with FBI, a foreign body was found in the upper digestive tract in 138 (43.1%). Medical treatment such as glucagon was not prescribed to any patient. Older age, previous episodes and early presentation to the emergency department were found as independent predictors of foreign body presence (Table 2). Gender, history of oesophageal disease and psychiatric disorder were not associated with foreign body presence, and neither was the presence of symptoms (rather than history of FBI alone). Foreign body perception was the most frequent symptom in patients with FBI (64.4%, Table 1), and its presence was similar in patients with and without confirmed FBI at endoscopy (Table 2). On the other hand, dysphagia and pain were significantly associated with foreign body presence at endoscopy (Table 2). Early presentation to the emergency department was also associated with foreign body presence. Indeed, patients without foreign body at endoscopy had a higher median time to presentation (Table 2), and the proportion of patients with foreign body at endoscopy decreased as the time to presentation increased (Figure 1). The majority of the foreign bodies were found in the oesophagus (80.4%, the majority in the upper third) and only one was found in the duodenum.
Table 2.
Foreign body ingestion.
| Foreign body present (n = 138) | Foreign body absent (n = 182) | P value | P (MV analysis) | Adjusted OR (95% CI) | |
|---|---|---|---|---|---|
| Age, mean (SD) | 57.7 (17.3) | 51.0 (17.6) | 0.001 | <0.001 | 1.04 (1.02–1.06) |
| Male gender, n (%) | 57 (41.3%) | 71 (39.0%) | 0.678 | 0.268 | |
| Oesophageal disease, n (%) | 4 (2.9%) | 5 (2.7%) | 0.846 | – | |
| Previous episode, n (%) | 16 (11.6%) | 12 (6.6%) | 0.083 | 0.043 | 0.35 (0.13–0.97) |
| Psychiatric disordera | 14 (10.1%) | 20 (11.0%) | 0.945 | – | |
| Symptoms (any), n (%) | 121 (87.7%) | 151 (83.0%) | 0.073 | 0.056 | 0.37 |
| Foreign body perception | 90 (65.2%) | 116 (63.7%) | 0.606 | (0.14–1.02) | |
| Dysphagia | 38 (27.6%) | 22 (12.1%) | <0.001 | ||
| Pain | 61 (44.2%) | 44 (24.2%) | <0.001 | ||
| Time to ER (hours), median (IQR)b | 2.5 (1–5.5) | 5.0 (2–15.5) | <0.001 | ||
| Time to ER (hours)c | |||||
| ≤6 hours | 77 (79.4%) | 79 (56.0%) | <0.001 | <0.001 | 4.41 |
| >6 hours | 20 (20.6%) | 62 (44.0%) | (2.24–8.66) | ||
MV: multivariable analysis; OR: odds ratio; CI: confidence interval; SD: standard deviation; ER: emergency room; IQR: interquartile range; FBI: foreign body ingestion; FI: food impaction.
Schizophrenia, dementia or major depression.
Mann–Whitney U test.
In 82 cases (41 in the FBI group and 41 in the FI group) the time to presentation was missing.
Figure 1.
Foreign body presence according to time to presentation.
The most frequent foreign bodies encountered were meat and fish bones (54% and 39%, respectively). The type of foreign body was not significantly associated with its presence on endoscopy, although there was a trend to higher detection in the case of meat bones (53.6% vs. 39.1% in fish bones, P = 0.124). The foreign body was retrieved successfully in 92.8%, with foreign body forceps being the preferred instrument for removal (used in 64% of the cases). More than one instrument was used in 7.8% of the cases, while mobilisation alone was used in some cases of small bones encountered in the oesophagus. Protector hood or overtube were used in three cases.
The majority of the patients with non-successful endoscopic removal of the foreign body were referred for rigid oesophagoscopy performed by otorhinolaryngology (n = 6), three patients had a repeat endoscopy with successful removal and one patient with several metallic objects in the stomach not amenable to endoscopic removal was referred for surgery.
Overall, major adverse events occurred in four patients of those with confirmed foreign body (2.9%) – one perforation closed endoscopically, two deep oesophageal lacerations closed endoscopically and one significant haemorrhage controlled with endoscopic therapy. In addition, there were eight patients with oesophageal lacerations in the locality where the foreign body was impacted that did not require endoscopic closure but led to a short admission for surveillance. In patients without FBI at endoscopy, no adverse events occurred.
Food impaction
The majority (86.6%) of the patients with clinical suspicion of FI had the diagnosis confirmed at endoscopy (Table 3). Patients with confirmed FI were significantly older and more frequently had psychiatric disorders. However, on multivariable analysis the only independent predictor of FI presence was psychiatric disease (dementia in most cases). Previous episodes, history of oesophageal disease, the presence of symptoms and time to emergency department presentation were not different in patients with and without FI. Dysphagia (70.6%) and foreign body perception (45.3%) were the most frequent symptoms overall, and these were the symptoms associated with confirmed FI diagnosis. Pain was not significantly different in patients with and without confirmed FI. Nearly half of the cases of FI occurred in the lower oesophagus (Table 4), and oesophageal rings or benign strictures were found in 22.4% and 19.9% of the entire FBI cohort, respectively.
Table 3.
Food impaction.
| FI present (n = 174) | FI absent (n = 27) | P value | P (MV analysis) | Adjusted OR (95% CI) | |
|---|---|---|---|---|---|
| Age, mean (SD) | 61.4 (18.3) | 52.1 (22.1) | 0.045 | 0.064 | |
| Male gender, n (%) | 122 (70.1%) | 17 (63.0%) | 0.454 | 0.939 | |
| Oesophageal disease, n (%) | 54 (31.0%) | 7 (25.9%) | 0.354 | – | |
| Previous episode, n (%) | 64 (36.8%) | 8 (29.6%) | 0.223 | – | |
| Psychiatric disordera | 12 (6.9%) | 8 (29.6%) | 0.001 | 0.008 | 6.69 (1.66–26.9) |
| Symptoms (any), n (%) | 157 (90.2%) | 27 (100%) | 1.000 | – | |
| Foreign body perception | 70 (40.2%) | 21 (77.8%) | 0.002 | ||
| Dysphagia | 130 (74.7%) | 12 (44.4%) | <0.001 | ||
| Pain | 21 (12.1%) | 1 (3.7%) | 0.207 | ||
| Time to ER (hours), median (IQR)b | 5 (2–17) | 3 (2–20.25) | 0.870 | – |
MV: multivariable analysis; OR: odds ratio; CI: confidence interval; SD: standard deviation; ER: emergency room; IQR: interquartile range.
Schizophrenia, dementia or major depression.
Mann–Whitney U test.
Table 4.
Outcomes of confirmed foreign body ingestion and food impaction.
| Foreign body (n = 138) | Food impaction (n = 174) | P value | |
|---|---|---|---|
| Location | |||
| Hypopharynx | 12 (8.7%) | – | – |
| Upper oesophagus | 90 (65.2%) | 60 (34.5%) | |
| Middle oesophagus | 12 (8.7%) | 29 (16.7%) | |
| Lower oesophagus | 9 (6.5%) | 85 (48.8%) | |
| Stomach | 14 (10.1%) | – | |
| Duodenum | 1 (0.7%) | – | |
| Successful endoscopic removal | |||
| Yes | 128 (92.8%) | 169 (97.1%) | 0.073 |
| No | 10 (7.8%) | 5 (2.9%) | |
| Endoscopic methods used | |||
| Foreign body forceps | 88 | 20 | – |
| Retrieval basket | 17 | 94 | |
| Polipectomy snare | 3 | 13 | |
| Tripod | 4 | 34 | |
| Mobilisation | 27 | 75 | |
| Overtube | 1 | 0 | |
| Protector hood | 2 | 0 | |
| Use of more than one instrument | |||
| Yes | 10 (7.8%) | 38 (21.8%) | <0.001 |
| No | 128 (92.8%) | 136 (78.2%) | |
| Adverse events | |||
| No | 134 (97.1) | 166 (95.6%) | 0.438 |
| Yes | 4 (2.9) | 8 (4.6%) | |
FI was removed in 97.1% of the cases, with retrieval basket being the preferred instrument for removal (used in 54% of cases). Simple mobilisation of the food bolus through the stomach with gentle pushing or air insufflation was the approach in 28.2%. The need to use more than one instrument was significantly higher than in FBI (22.5% in FI vs. 7.8% in FBI, P < 0.001).
Patients with non-successful endoscopic resolution of the FI were referred for rigid oesophagoscopy. Adverse events occurred in eight patients with confirmed FI (4.6%), all related to oesophageal ulceration around the food bolus and not caused by endoscopic removal – one frank perforation was found that was closed endoscopically in a patient with prolonged FI (>72 hours); two haemorrhages and five deep oesophageal lacerations were treated conservatively but required short inpatient surveillance. There were no adverse events in patients with suspected FI submitted to endoscopy but in whom FI was not confirmed at endoscopy. There were no re-admissions after hospital discharge.
Discussion
FBI and FI are one of the most frequent emergencies in gastroenterology, yet studies on this topic are scarce and the majority is retrospective.
In this prospective study conducted in a tertiary gastroenterology centre, we found that in almost half of the patients with FBI submitted to endoscopy the foreign body was encountered in the upper digestive tract, and was retrieved successfully without complications in more than 90% of the patients. Older age and earlier presentation to the emergency department were independent predictors of foreign body presence. Indeed, older patients may have impaired oesophageal motility and foreign bodies may have a lower probability of spontaneously dislodging from the oesophagus. Earlier presentation as a predictor for foreign body presence can be related to greater symptom severity in patients who present earlier. However, this hypothesis could not be tested in this study because only symptom presence was assessed rather than symptom severity. Concerning suspected FI, approximately 86% had their clinical diagnosis confirmed at endoscopy, the majority was successfully solved endoscopically. The only independent predictor of FI presence was psychiatric disease (mostly dementia). Successful removal of foreign body and FI occurred in over 90% of the cases, and complications occurred in approximately 5%. Deep sedation was needed in only 5% of the cases.
Although we acknowledge that this study design does not allow conclusions about the natural history of FBI, we found that in almost 50% of the patients a foreign body is found at endoscopy in a real-life setting. Our findings contrast with older studies (performed more than 50 years ago), which report that up to 80–90% of the foreign bodies spontaneously pass through the gastrointestinal tract, with complications occurring in a minority.11,12 Our rate can be slightly overestimated because the patients included were referred for gastroenterology evaluation; it is possible that some patients with FBI and no alarm symptoms or signs could have been discharged without gastroenterology consultation, although this is unlikely due to the organisation of the emergency department in our centre, in which gastroenterology consultation is the norm in both FBI and FI.
Based on older reports, the European Society of Gastrointestinal Endoscopy (ESGE) guidelines recommend that asymptomatic patients with ingestion of blunt and small objects (except batteries and magnets) can avoid endoscopy.7 However, in a high proportion of cases patients are not sure if the object (e.g. bone, dentary prosthesis component) is blunt or sharp, and the majority of patients present with some kind of symptom. In addition, the potential adverse events of FBI and FI are severe, and endoscopic evaluation and therapy have high rates of success with a good safety profile. This, together with our finding of more than 50% of foreign bodies in the upper digestive tract, suggests that endoscopy is beneficial in the majority of patients with FBI because it can remove the foreign body, prevent complications (namely late complications such as fistulisation and abscess) and can also have a reassuring effect. Although pharmacological treatment was not used in any patient in this study (in accordance with ESGE guidelines7 and also supported by a recent multicentre study that showed no benefit of glucagon therapy),14 our results further support endoscopy as the first line approach.
Thus we consider that the threshold to perform endoscopy should be low because it can prevent those poor outcomes. However, based on our findings, young asymptomatic patients who present over 12 hours after FBI have a lower probability of foreign body in the upper digestive tract; these patients can possibly avoid endoscopy and clinical surveillance may be an option in these cases.
Our finding of a low complication risk also contrasts with a recent study that found complications in half of the patients.13 That study included minor haematomas and ulcerations as complications, which justify the higher complication rate. However, we consider that minor endoscopic findings should not be reported as complications because they will not alter management in the majority of cases, as also suggested by the American Society of Gastrointestinal Endoscopy (ASGE).15 Lower adverse event rates were also found in some other retrospective studies that reported their occurrence in less than 10%.1
Regarding treatment strategies, foreign body forceps was the preferred instrument in FBI while retrieval basket was preferred in FI, although mobilisation alone was sufficient in a quarter of cases. We also found that in FI the use of more than one instrument is more likely, suggesting that the whole array of endoscopic instruments should be promptly available if FI is suspected. This suggests that the majority of cases of FBI can be removed with foreign body forceps and the majority of FI with retrieval baskets, although the decision between the different types of instruments should be taken on a case by case basis.
This study has some limitations. Despite the prospective design, some data concerning time to presentation to the emergency department were missing. In addition, we only assessed the presence of symptoms and not their severity, which can also be associated with foreign body presence. The decision to perform biopsies in patients with FI without an obvious reason was left at the discretion of the endoscopist, and so the real prevalence of eosinophilic oesophagitis could not be assessed. Finally, as adverse events were rare, our study is underpowered to identify risk factors for complications and this deserves further clarification in larger prospective studies.
In conclusion, foreign bodies are encountered during upper digestive endoscopy in almost 50% of the patients who present to the emergency department after FBI, and they can be treated successfully and safely in more than 90% of cases. Older age and early presentation are independent predictors for their presence in the upper digestive tract and should lower the threshold to perform endoscopy.
Acknowledgements
The authors acknowledge the contribution of all gastroenterologists and nurses working at URGE – Urgência Regional de Gastrenterologia do Norte/Centro Hospitalar do Porto in data collection and the contribution of Dr Inês Pita in the language revision of this manuscript.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the ethical committee of Centro Hospitalar do Porto (08/09/2010).
Informed consent
Informed consent was obtained from patients included in the study.
References
- 1.Geraci G, Sciume C, Di Carlo G, et al. Retrospective analysis of management of ingested foreign bodies and food impactions in emergency endoscopic setting in adults. BMC Emerg Med 2016; 16: 42–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yao CC, Wu IT, Lu LS, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract of adults. Biomed Res Int 2015; 2015: 658602–658602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erbil B, Karaca MA, Aslaner MA, et al. Emergency admissions due to swallowed foreign bodies in adults. World J Gastroenterol 2013; 19: 6447–6452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen T, Wu HF, Shi Q, et al. Endoscopic management of impacted esophageal foreign bodies. Dis Esophagus 2013; 26: 799–806. [DOI] [PubMed] [Google Scholar]
- 5.Bekkerman M, Sachdev AH, Andrade J, et al. Endoscopic management of foreign bodies in the gastrointestinal tract: a review of the literature. Gastroenterol Res Pract 2016; 2016: 8520767–8520767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magalhaes-Costa P, Carvalho L, Rodrigues JP, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: an evidence-based review article. GE Port J Gastroenterol 2016; 23: 142–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Birk M, Bauerfeind P, Deprez PH, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016; 48: 489–496. [DOI] [PubMed] [Google Scholar]
- 8.Triadafilopoulos G, Roorda A, Akiyama J. Update on foreign bodies in the esophagus: diagnosis and management. Curr Gastroenterol Rep 2013; 15: 317–317. [DOI] [PubMed] [Google Scholar]
- 9.Ambe P, Weber SA, Schauer M, et al. Swallowed foreign bodies in adults. Dtsch Arztebl Int 2012; 109: 869–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loh WS, Eu DK, Loh SR, et al. Efficacy of computed tomographic scans in the evaluation of patients with esophageal foreign bodies. Ann Otol Rhinol Laryngol 2012; 121: 678–681. [DOI] [PubMed] [Google Scholar]
- 11.Grekin TD, Musselman MM. The management of foreign bodies in the alimentary tract. Ann Surg 1952; 135: 528–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carp L. Foreign bodies in the intestine. Ann Surg 1927; 85: 575–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geng C, Li X, Luo R, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a retrospective study of 1294 cases. Scand J Gastroenterol 2017; 52: 1286–1291. [DOI] [PubMed] [Google Scholar]
- 14.Bodkin RP, Weant KA, Baker Justice S, et al. Effectiveness of glucagon in relieving esophageal foreign body impaction: a multicenter study. Am J Emerg Med 2016; 34: 1049–1052. [DOI] [PubMed] [Google Scholar]
- 15.Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 2010; 71: 446–454. [DOI] [PubMed] [Google Scholar]