Abstract
Caruncular lesions are uncommon and could be related to hair follicles, sebaceous glands, sweat glands, and accessory lacrimal gland harbored in caruncle. As the lesions of caruncle are diverse, the clinical diagnosis is difficult. Majority of the caruncular lesions are benign although rare malignant lesions have also been reported. Caruncular oncocytoma (CO) is a rare ocular neoplasm with an incidence of <3%, as per the Western literature. However, only two cases of ocular oncocytoma are reported in the Indian literature. Here, we report two more cases of CO from India with their histochemical and ultrastructural characteristics.
Keywords: Caruncle, ocular, oncocytoma
Introduction
Oncocytic or eosinophilic change is a common histomorphological variation of different skin tumors and the tumors of cutaneous adnexa. Oncocytic changes are known to occur in apocrine adenoma, apocrine hidradenoma, apocrine chondroid syringoma, granular cell tumor, eccrine acrospiroma, melanocytic nevi, and many other tumors. Oncocytoma is a benign neoplasm of the glandular and secretory epithelium and can involve many organs including salivary gland, thyroid, parathyroid, adrenal, gastrointestinal tract, and kidneys.[1] The oncocytoma is composed of deeply eosinophilic cells containing abundant mitochondria and can occur in relation to the cutaneous (including ocular) adnexa, the most common site being the ocular caruncle and medial eyelid canthus.[2] Caruncle is a small, pink, globular modified skin present at the inner corner of the eye.[3] The incidence of caruncular oncocytoma (CO) is around 3% of all biopsies of caruncular lesions.[4,5,6,7,8] There have been only two case reports in the English literature from India to the best of our knowledge, though a few case series exist in the Western literature. We describe two new cases of CO with histochemical and ultrastructural features along with the review of literature.
Case Reports
Case 1
A 72-year-old female patient presented with a small, painless, mucosa covered pinkish nodular swelling at inner canthus of the right eye for 4 months [Figure 1a]. There was no reduction in visual acuity, no impairment of ocular motility, strabismus, or any associated symptoms. No history of loss of weight or appetite was present. On investigations, blood counts, renal function tests, and liver function tests were normal. The tumor was localized to the medial canthus with normal looking overlying mucosa. The mass was excised and sent for histopathology. Grossly, it measured 11 mm × 5 mm × 3 mm with smooth surface, round contour, and was red in color. The cut surface was cystic with minute beige to brown colored papillary excrescences. Microscopy revealed a well encapsulated mass in the subepithelium stretching the overlying conjunctival epithelium. The mass showed both cystic (60%) and solid (40%) areas with papillary configuration [Figure 1b]. These papillae showed delicate fibrovascular cores lined by double layer of epithelium with the abluminal layer composed of flat epithelial cells with central round nuclei. The luminal cells were long columnar with basally located nuclei and abundant amount of granular eosinophilic cytoplasm [Figure 1c]. Periodic acid Schiff–alcian blue stain (PAS-AB) showed finely granular intracytoplasmic PAS positivity. The cystic areas showed AB positive secretory material and phospho-tungstic acid hematoxylin (PTAH) stain showed blue colored fine granules within the cytoplasm of the luminal cells corresponding to the mitochondria. Many goblet cells interspersed with the oncocytic cells were seen and were AB positive in PAS-AB stain [Figure 1d] and PAS positive in PAS stain. Electron microscopy of the tumor revealed an abundance of mitochondria in the tumor cells, many of which were giant with large cristae. The tumor did not recur after 25 months on follow up. Elastotic degeneration of the subepithelium was also seen.
Figure 1.
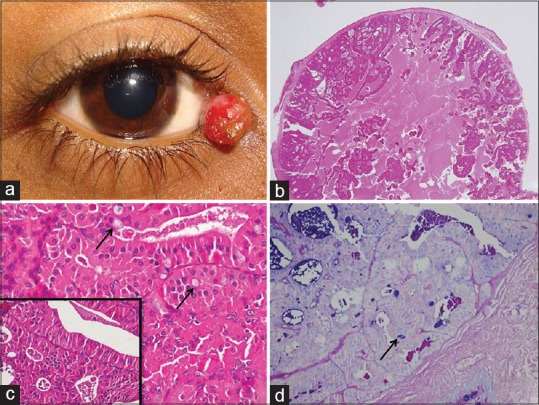
Photographs from Case 1: (a) pinkish nodular mass at the inner canthus of the right eye; (b) the scanner view showing the well-circumscribed mass stretching the overlying conjunctiva and a papillary-cystic pattern (Hematoxylin and Eosin, ×20); (c) higher magnification showing three types of cells, namely, the luminal oblong oncocytes, abluminal flattened cuboidal myoepithelial, and few interspersed goblet cells (black arrow) (Hematoxylin and Eosin, ×400); the inset further highlighting the dual population of cells; (d) the goblet cells were highlighted by the blue color (black arrow) (periodic acid Schiff–alcian blue stain, ×100)
Case 2
An 80-year-old male patient presented with a tiny nodule over the right caruncle for 5 months with no reduction in the visual acuity. No impairment in the ocular motility or strabismus was noted. The overlying mucosa was normal and the mass was excised under local anesthesia. Grossly, the mass measured 6 mm × 4 mm × 3 mm with a smooth external surface. The cut surface was solid and tan in color. Microscopy showed a well encapsulated tumor arranged in the form of nests and groups surrounded by delicate capillaries with central cystic degeneration [Figure 2a]. These small cystic structures were filled with eosinophilic secretion and debris [Figure 2b]. Individual nests and acini showed dual lining epithelium, the luminal/central one was oncocytic and the abluminal one was flat cuboidal. These epithelial cells were large with centrally placed round nuclei, vesicular chromatin, prominent nucleoli, and abundant amount of eosinophilic, finely granular cytoplasm. The PTAH stain showed fine blue intracytoplasmic granules highlighting abundance of mitochondria in these oncocytic cells [Figure 2c]. Occasional scattered mucus secreting goblet cells containing PAS positive mucin were also seen interspersed within the tumor. Electron microscopy revealed numerous mitochondria, similar to the Case 1 [Figure 2d]. There is no recurrence of the tumor after 8 months of surgery.
Figure 2.
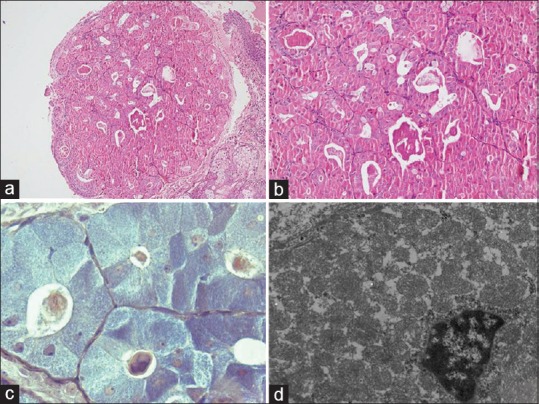
Photographs from Case 2: (a and b) the mass showing a tubular/acinar pattern with eosinophilic secretion and scattered goblet cells (Hematoxylin and Eosin, ×40 and ×200); (c) the oncocytes stain blue with phospho-tungstic acid hematoxylin stain (PTAH) (×1000); (d) electron microscopy of the tumor cells showed preponderance of mitochondria with a relative diminution of other cytoplasmic organelles, some of the mitochondria having large crista (uranyl acetate and lead citrate; ×6000)
Discussion
Oncocytomas are benign tumors characterized by the presence of voluminous granular eosinophilic cytoplasm, which represents abundant mitochondria when examined ultrastructurally.[1] In cutaneous presentations, the most common sites are the ocular caruncle, medial eyelid canthus, eyelid, and cheek.[2] The caruncle, present at inner corner of the eye, is a modified skin bearing hairs, sebaceous, and sweat glands along with goblet cells, and lacrimal tissue.[3] The predominant caruncular tumors include nodular basal cell carcinoma, hemangioma, nevus, benign cyst, or a salivary gland/adnexal neoplasm of the ocular adnexa. Oncocytoma is a rare tumor at ocular caruncle constituting <3–7.1% of all biopsies of caruncular lesions and it is difficult to distinguish these lesions grossly.[4,5,6,7,8] There are only two cases of ocular oncocytoma reported from India till date to the best of our knowledge, which is shown below in Table 1.
Table 1.
List of Indian series of ocular oncocytomas
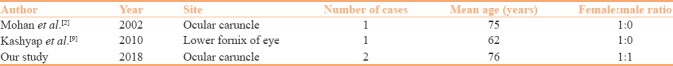
CO is reported to occur in the elderly patients with a female predisposition as an asymptomatic mass or nodule in the eye. Both the earlier reported cases from India were in elderly females.[2,9] In contrast, one of our cases occurred in an 80-year-old male patient. These are slowly growing painless mass and the lesion could be cystic or has a bright cherry red color as was seen in our Case 1. The gross diagnosis of oncocytoma and its distinction from the other tumors of the similar location is extremely difficult if possible. However, the presence of a telangiectatic papule with tan brown to reddish coloration may give an important clue to the clinician.
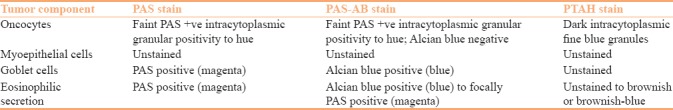
Histologically, three architectural patterns are described in oncocytoma,[5] including (1) tubular, (2) papillary-cystic, and (3) solid-trabecular. Our first case depicted a papillary-cystic architectural pattern composed predominantly of cystic structures with true papillary fronds projected within the cyst. The second case showed a tubular/pseudoacinar pattern. In both the cases, the presence of oncocytes and flat myoepithelial (abluminal) cells admixed with scattered goblet cells were noted. The presence of the dual cell population is important as it distinguishes it from granular cell tumor, which shows a diffuse sheet like architecture. Moreover, the cells of granular cell tumor show S100 positivity and ultrastructurally contain abundant giant lysosomes instead of mitochondria. None of the cases showed a lymphoid component thereby ruling out Warthin's tumor arising from the ocular adnexa. It is important to note that the oncocytic changes in different tumors involving the cutaneous adnexa are more common than oncocytoma, like apocrine adenoma or hidradenoma, eccrine acrospiroma, granular cell tumor, and melanocytic nevi. It is usually a percentage of the tumor cells in other tumors that show the oncocytic change in contrast to the oncocytoma where all the cells are oncocytic. Moreover, the absence of apocrine snouts and decapitation secretion distinguish oncocytoma from the apocrine lesions. The goblet cells occur in relation to the caruncular or conjunctival lesions due to the peculiarity of the conjunctival epithelium to contain goblet cells that get included in the tumor. Histochemical stains including PAS-AB and PTAH were useful to highlight the mucus component (AB), secretion (PAS and AB), and abundant mitochondria (PTAH and PAS). The histochemical features are highlighted in the Table 2. Pathological examination is mandatory in establishing the diagnosis of CO.
Table 2.
The histochemical features of oncocytoma with different components
Basal cell carcinoma, nevus, or hemangioma does not pose problem microscopically. However, nodular or diffuse oncocytosis, oncocytic carcinoma, Warthin's tumor, or other benign cysts may be considered as differential diagnosis of an oncocytoma. Oncocytosis (nodular or diffuse) usually lacks the thin capsule of the oncocytoma. Nodular oncocytosis can sometimes contain partial encapsulation. Warthin's tumor is extremely rare in the ocular adnexa and lacrimal glands and shows presence of a dominant lymphocytic component in the stroma of the lesion.[5] Other benign cysts rarely cause a diagnostic difficulty except for epidermal inclusion cyst, as oncocytoma at times can undergo squamous metaplasia. The papillary-cystic variant of oncocytoma can sometimes show predominant cystic area with few oncocytic cell clusters thereby making the possibility of a benign cyst pertinent.
Clinically, aggressive behavior has not been documented in oncocytomas arising in the caruncle; however, very rarely, it can progress to oncocytic carcinoma.[10] It is important to identify a malignant oncocytoma as it has an aggressive course and can also show lymph node metastasis.[10] Despite limited data, approximately 5–10% of the oncocytoma may turn malignant if left untreated.[11,12] An infiltrative margin, pleomorphism, and mitosis along with sheet like architecture are the clues to diagnose an oncocytic carcinoma. Hence, any change in color, size, or vascularization of a caruncular lesion necessitates excision and histopathological examination.
Surgical excision is curative and a recurrence following complete excision is not reported in the literature. None of our cases showed any evidence of recurrence on follow up (8 and 25 months).
In brief, oncocytoma is a rare benign neoplasm of the cutaneous adnexa, the most common site being the caruncle. Due to varied clinical differentials, histopathological examination is mandatory. A close collaboration between clinicians and pathologists is required to establish the diagnosis and proper treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Filho JP, Vianna RN, Coutinho AB, Arthurs B, Burnier MN., Jr Oncocytoma of the caruncle: A clinicopathologic case report. Int Ophthalmol. 2004;25:321–3. doi: 10.1007/s10792-005-2036-x. [DOI] [PubMed] [Google Scholar]
- 2.Mohan ER, Biswas J, Krishnakumar S. Oncocytoma of the caruncle. Indian J Ophthalmol. 2002;50:60–1. [PubMed] [Google Scholar]
- 3.Levy J, Ilsar M, Deckel Y, Maly A, Pe'er J. Lesions of the caruncle: A description of 42 cases and a review of the literature. Eye (Lond) 2009;23:1004–18. doi: 10.1038/eye.2008.316. [DOI] [PubMed] [Google Scholar]
- 4.Ostergaard J, Prause JU, Heegaard S. Caruncular lesions in Denmark 1978-2002: A histopathological study with correlation to clinical referral diagnosis. Acta Ophthalmol Scand. 2006;84:130–6. doi: 10.1111/j.1600-0420.2005.00543.x. [DOI] [PubMed] [Google Scholar]
- 5.Pecorella I, Garner A. Ostensible oncocytoma of accessory lacrimal glands. Histopathology. 1997;30:264–70. doi: 10.1046/j.1365-2559.1997.d01-601.x. [DOI] [PubMed] [Google Scholar]
- 6.Luthra CL, Doxanas MT, Green WR. Lesions of the caruncle: A clinicohistopathologic study. Surv Ophthalmol. 1978;23:183–95. doi: 10.1016/0039-6257(78)90155-8. [DOI] [PubMed] [Google Scholar]
- 7.Kaeser PF, Uffer S, Zografos L, Hamedani M. Tumors of the caruncle: A clinicopathologic correlation. Am J Ophthalmol. 2006;142:448–55. doi: 10.1016/j.ajo.2006.04.035. [DOI] [PubMed] [Google Scholar]
- 8.Shields CL, Shields JA, White D, Augsburger JJ. Types and frequency of lesions of the caruncle. Am J Ophthalmol. 1986;102:771–8. doi: 10.1016/0002-9394(86)90407-1. [DOI] [PubMed] [Google Scholar]
- 9.Kashyap S, Meel R, Bajaj MS, Pushker N. Ocular oncocytoma of the fornix. Indian J Pathol Microbiol. 2010;53:882–3. doi: 10.4103/0377-4929.72034. [DOI] [PubMed] [Google Scholar]
- 10.Marglani O, Alherabi A, Corsten M. Malignant oncocytoma of the lacrimal sac with cervical metastasis: Case report and literature review. J Otolaryngol Head Neck Surg. 2008;37:E8–10. [PubMed] [Google Scholar]
- 11.Morand B, Bettega G, Bland V, Pinel N, Lebeau J, Raphael B. Oncocytoma of the eyelid: An aggressive benign tumor. Ophthalmology. 1998;105:2220–4. doi: 10.1016/S0161-6420(98)91219-2. [DOI] [PubMed] [Google Scholar]
- 12.Biggs SL, Font RL. Oncocytic lesions of the caruncle and other ocular adnexa. Arch Ophthalmol. 1977;95:474–8. doi: 10.1001/archopht.1977.04450030116017. [DOI] [PubMed] [Google Scholar]


