Abstract
Background:
Nail involvement in psoriasis is often complicated by concomitant fungal infections. The aim of this study was to investigate the prevalence of fungal infections in nail psoriasis and correlate it with the severity of nail psoriasis.
Materials and Methods:
This retrospective study included patients with nail psoriasis aged ≥18 years with at least one fingernail and one toenail involvement who were treated at Siriraj Hospital from September 2012 to January 2014. Severity of nail psoriasis was assesed by Nail Psoriasis Area Severity Index (NAPSI) score. The nail clippings from the the least and most severely involved psoriatic fingernails and toenails were cultured to determine the presence of coexisting fungal infections and isolate the fungal species.
Results:
Sixty-two patients (33 males, 29 females) fulfilling the inclusion criteria were included in the study. The mean age at the time of presentation was 51.3 years mention SD. The most common nail change consistent with psoriasis was onycholysis, followed by subungual hyperkeratosis. The most commonly isolated fungi in the most severely affected fingernails were Candida spp. (41.9%) manifesting as paronychia in 5 patients (19.2%). The most commonly isolated fungi in the most severely affected toenails were nondermatophytes (NDMs) other than candida (32.3%). Dermatophytes were not detected from any of the psoriatic nails. The fungal species isolated from the most severely affected fingernails were significantly different than the isolated fungal species in the most severely affected toenails (P = 0.026). Fungal organisms were identified in 32.3% of the most severely affected fingernails and in 27.4% of the most severely affected toenails. The overall rate of isolation of fungus was significantly significantly higher in severely affected nails than in the least affected nails (P < 0.005).
Conclusion:
A high rate of concomitant fungal infections, especially yeasts and NDMs, was found in psoriatic nail patients. The rate of isolation of fungal species was higher in severely involved psoriatic nails than mildly involved ones. The spectrum of fungal species isolated from the the severely involved toenails and fingernails were also different from each other. These organisms may be true pathogens that cause onychomycosis or their presence may reflect colonization, contamination, or concurrent infection.
Keywords: Fingernails, fungal infection, nail psoriasis, prevalence, severity, Thailand, toenails
Introduction
Psoriasis is one of the most common chronic inflammatory skin disease. Nail involvement can be found in approximately 20–78% of patients with psoriasis.[1,2] Moreover, psoriatic patients with nail involvement may have nail changes that are similar to the manifestations of onychomycosis. Treatment options in psoriatic nail patients include topical corticosteroid, intralesional corticosteroid, and/or immunosuppressive drugs, whereas patients with onychomycosis require systemic and topical antifungal agents. A subset of patients with nail psoriasis may have concomitant fungal infections. This study was aimed to investigate the prevalence of fungal infections in nail psoriasis and correlate it with the severity of nail psoriasis.
Materials and Methods
Patients
This retrospective study included patients with nail psoriasis aged 18 years or older with at least one fingernail and one toenail involvement who were treated at the Department of Dermatology, Siriraj Hospital from September 2012 to January 2014. Siriraj Hospital is Thailand's largest university-based national tertiary referral center. Patients who received treatment with systemic or topical antifungal agents within a period of 6 months prior to the enrollment were excluded. The protocol for this study was approved by the Siriraj Institutional Review Board (SIRB), Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand. Written informed consent was obtained from all the study participants.
Clinical examination
Demographic data, including age, gender, occupation, underlying diseases, types of psoriasis, disease duration, and treatments, were recorded. Severity of the skin involvement was evaluated by the Psoriasis Area Severity Index (PASI). Severity of the nail involvement was assessed by Nail Psoriasis Area Severity Index (NAPSI).[3]
Mycological examinations
The least and the most affected toenails and fingernails based on the minimum and maximum NAPSI score, respectively, were selected. Culture was used as a definite criterion to determine the presence of dermatophytes or nondermatophytes (NDMs) and to isolate the fungal species. According to the study by Gupta et al., a diagnosis of NDM onychomycosis required a consistent organism from culture in repeated isolations.[4]
Statistical analysis
All data analyses were performed using SPSS Statistics version 18 (SPSS, Inc., Chicago, IL, USA). Comparison of rate of positive fungal culture results among the most severely affected fingernail and the most severely affected toenail gwas analyzed using McNemar–Bowker test. Chi-square test was employed to compare pathogens between fingernails and toenails. Data are presented as number or number and percentage. A P-value less than 0.05 was regarded as being statistically significant.
Results
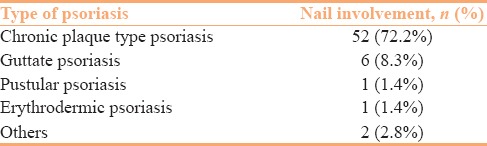
Sixty-two patients (33 males, 29 females) with a mean age of 51.3 years at the time of presentation (range: 18–80) were enrolled. Mean PASI score was 13.0 (range: 0.2–55.8). The distribution of patients with nail psoriasis based on the morphological variant of cutaneous psoriasis has been presented in Table 1.
Table 1.
Distribution of patients with nail involvement by the morphological type of cutaneous psoriasis (n=62)
The most common psoriatic nail change was onycholysis (83.9%), followed by subungual hyperkeratosis (51.6%). The mean duration of nail changes at the time of presentation was 7.3 years (range: 1 month to 40 years). The median NAPSI score of the most and least severely affected fingernails was 6 (range: 1–8) and 4 (range: 0–8), respectively. Median NAPSI score of the most and least severely affected toenails was 6 (range: 1–8) and 2 (range: 0–8), respectively. The most commonly isolated fungal species in the most severely affected fingernail belonged to Candida spp. (41.9%) manifesting as paronychia in 5 patients (19.2%). The most commonly isolated fungal species in the most severely affected toenails were NDMs other than candida (32.3%). Dermatophytes were not detected from any of the psoriatic nails [Table 2]. The causative fungal species in the most severely affected fingernails were significantly different than those in the most severely affected toenails (P = 0.026).
Table 2.
The results of fungal cultures compared by severity between fingernails and toenails in psoriatic nail patients
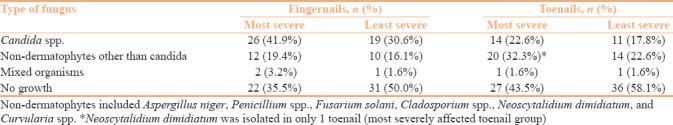
Fungal organisms were identified in 32.3% of the most severely affected fingernails and in 27.4% of the most severely affected toenails. The rate of isolation of fungus was significantly higher in severely affected fingernails and toenails than in the least affected fingers and toenails (both P < 0.005).
Discussion
The association of onychomycosis and nail psoriasis remains unclear and sometimes contradictory, as observed from studies outlined in Table 3. The clinical differentiation of psoriatic nails with onychomycosis can be challenging sometimes.
Table 3.
Literature review of onychomycosis in psoriatic nail patients
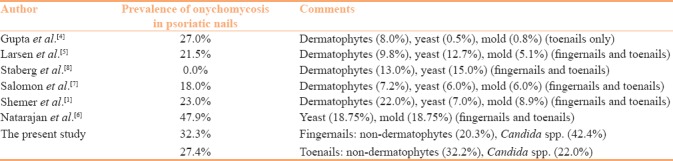
Few of the previous studies reported that the prevalence of onychomycosis in patients with nail psoriasis did not differ significantly from the rate observed in the control group, whereas some other studies showed higher prevalence in the study group.[5,6,7,8,9,10] These sometimes disparate differences in findings may be due to variations in study methodology and diagnostic criteria.
In the present study, NDMs were frequently discovered in more severely involved psoriatic toenails. These finding may be suggestive of contamination rather than true pathogens given the fact that the NDM species are widely distributed in the environment. Yeasts were likely to be found more often in more severely involved psoriatic fingernails than in toenails probably owing to the fact that fingernails are more oftenly exposed to water than toenails.
Bunyaratavej et al. reported Neoscytalidium dimidiatum to be a common cause of onychomycosis among general population in Thailand.[11] In contrast, N. dimidiatum infection was isolated in only one toenail in the present study. Even though dermatophytes are a common cause of onychomycosis worldwide, this study did not find any dermatophyte-related onychomycosis. Rapid growth of psoriatic nails may decrease the probability of fungal invasion of the nail plate.[7,11,12] Moreover, the presence of antimicrobial peptides, such as β-defensin-2 and cathelicidin, in the skin and nail units in psoriatic patients strengthens the immune defense against pathogens. Increased expression of cytokine interleukin-17 (IL-17A) may also play a significant role in defense mechanisms against extracellular bacterial and fungal infections, especially in psoriasis.[12,13,14] However, the exact mechanisms remain unknown.
There are a few limitations of this study. First, this was not a case-control study as no healthy controls were recruited. Second, dermoscopic examinations for supportive evidence of clinical findings to distinguish onychomycosis from nail psoriasiswere not performed. Third, this study also enrolled older cases of nail psoriasis who were previously treated with systemic immunosuppressive therapy, which may have increased the risk of overgrowth of organisms, especially yeasts.
Conclusion
A high rate of concomitant fungal infection, especially yeasts and NDMs, was found in patients with psoriatic nails. The rate of isolation of fungal species was higher in severely involved psoriatic nails than mildly involved ones. The spectrum of fungal species isolated from the the severely involved toenails and fingernails were also different from each other. These organisms may be true pathogens that cause onychomycosis or their presence may reflect colonization, contamination, or concurrent infection in patients with nail psoriasis. Interestingly, although N. dimidiatim is the most common cause of NDM onychomycosis in Thailand, this pathogen was isolated in only one toenail, which was in the most severely affected toenail group. Further prospective controlled studies are encouraged to confirm these findings and further elucidate the relationship between nail psoriasis and fungal infection.
Financial support and sponsorship
Nil.
Conflicts of interest
All authors declare no personal or professional conflicts of interest, and no financial support from the companies that produce and/or distribute the drugs, devices, or materials described in this report.
Acknowledgements
The authors gratefully acknowledge the patients who generously agreed to participate in this study.
References
- 1.Shemer A, Trau H, Davidovici B, Grunwald MH, Amichai B. Onychomycosis in psoriatic patients-rationalization of systemic treatment. Mycoses. 2010;53:340–3. doi: 10.1111/j.1439-0507.2009.01726.x. [DOI] [PubMed] [Google Scholar]
- 2.Rizzo D, Alaimo R, Tilotta G, Dinotta F, Bongiorno MR. Incidence of onychomycosis among psoriatic patients with nail involvement: A descriptive study. Mycoses. 2013;56:498–9. doi: 10.1111/myc.12042. [DOI] [PubMed] [Google Scholar]
- 3.Rich P, Scher RK. Nail Psoriasis Severity Index: A useful tool for evaluation of nail psoriasis. J Am Acad Dermatol. 2003;49:206–12. doi: 10.1067/s0190-9622(03)00910-1. [DOI] [PubMed] [Google Scholar]
- 4.Gupta AK, Drummond-Main C, Cooper EA, Brintnell W, Piraccini BM, Tosti Antonella. Systemic review of nondermatophyte mold onychomycosis: Diagnosis, clinical types, epidemiology, and treatment. J Am Acad Dermatol. 2012;66:494–502. doi: 10.1016/j.jaad.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 5.Gupta AK, Lynde CW, Jain HC, Sibbald RG, Elewski BE, Daniel CR, 3rd, et al. A higher prevalence of onychomycosis in psoriatics compared with non-psoriatics: A multicentre study. Br J Dermatol. 1997;136:786–9. [PubMed] [Google Scholar]
- 6.Larsen GK, Haedersdal M, Svejgaard EL. The prevalence of onychomycosis in patients with psoriasis and other skin diseases. Acta Derm Venereol. 2003;83:206–9. doi: 10.1080/00015550310007229. [DOI] [PubMed] [Google Scholar]
- 7.Salomon J, Szepietowski JC, Proniewicz A. Psoriatic nails: A prospective clinical study. J Cutan Med Surg. 2007;7:317–21. doi: 10.1007/s10227-002-0143-0. [DOI] [PubMed] [Google Scholar]
- 8.Natarajan V, Nath AK, Thappa DM, Singh R, Verma SK. Coexistence of onychomycosis in psoriatic nails: A descriptive study. Indian J Dermatol Venereol. 2010;76:723. doi: 10.4103/0378-6323.72468. [DOI] [PubMed] [Google Scholar]
- 9.Staberg B, Gammeltoft M, Onsberg P. Onychomycosis in patients with psoriasis. Acta Derm Venereol. 1983;63:436–8. [PubMed] [Google Scholar]
- 10.Kaçar N, Ergin S, Ergin C, Erdogan BS, Kaleli I. The prevalence, aetiological agents and therapy of onychomycosis in patients with psoriasis: A prospective controlled trial. Clin Exp Dermatol. 2007;32:1–5. doi: 10.1111/j.1365-2230.2006.02215.x. [DOI] [PubMed] [Google Scholar]
- 11.Bunyaratavej S, Prasertworonun N, Leeyaphan C, Chaiwanon O, Muanprasat C, Matthapan L. Distinct characteristics of Scytalidium dimidiatum and non-dermatophyte onychomycosis as compared with dermatophyte onychomycosis. J Dermatol. 2015;42:258–62. doi: 10.1111/1346-8138.12768. [DOI] [PubMed] [Google Scholar]
- 12.Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361:496–509. doi: 10.1056/NEJMra0804595. [DOI] [PubMed] [Google Scholar]
- 13.Zaias N. Psoriasis of the nail. A clinical-pathologic study. Arch Dermatol. 1969;99:567–79. [PubMed] [Google Scholar]
- 14.Szepietowski JC, Salomon J. Do fungi play a role in psoriatic nails? Mycoses. 2007;50:437–42. doi: 10.1111/j.1439-0507.2007.01405.x. [DOI] [PubMed] [Google Scholar]


