Abstract
Objectives:
The purpose of this study was to compare the static and dynamic mechanical properties of a modified crossed cannulated screw configuration (CS), the inverted triangle cannulated screw configuration (IT) and a compression hip screw with derotation screw (CHS) in Pauwels Type III femoral neck fractures.
Methods:
Thirty synthetic femora were divided into three groups and vertical femoral neck osteotomies were made. Ten osteotomized femora were fixed with a modified cross screw (CS) configuration, ten were fixed with three parallel screws in an inverted triangle (IT) configuration, and the remaining ten osteotomized femora were fixed with a compression hip screw (CHS) construct. All groups were tested using a cyclic (up to 15,000 load cycles) axial loading protocol and survivors were statically loaded to failure. Cycles to failure, load to failure and stiffness were calculated. The Kaplan-Meier method was used to estimate survival functions and were compared among fixation methods. The relationship between construct structural properties (maximum load and stiffness) and treatment were assessed using general linear modeling.
Results:
All CHS fixation constructs survived the 15,000 cycle loading protocol. They endured longer (p = 0.034) than the CS fixation constructs (mean failure 13,332 cycles), but were not different from IT fixation constructs (mean failure 13,592 cycles). Maximum loads to failure for CS (3,870 N) and IT (3,756 N) fixation constructs were not different, but were less (p<0.0001) than the maximum loads to failure for the CHS fixation constructs (5,654 N). These findings parallel the results of the axial stiffness measurements: CS fixation constructs (663.01 N/mm) were not stiffer than IT fixation constructs (620.0 N/mm), but were less (p=0.0005) than the axial stiffness of the CHS fixation constructs (1,241.86 N/mm).
Conclusions:
The biomechanical performance of the compression hip screw (CHS) fixation method was superior to both the modified cross screw (CS) fixation method and the inverted triangle (IT) fixation method using a synthetic femoral model and this test protocol. Biomechanical performance of the latter two groups was indistinguishable. We recommend the use of CHS with derotational screw construct for Pauwels III femoral neck fractures whenever possible.
Introduction
Femoral neck fractures are primarily seen in the geriatric population after low-nergy falls. Fractures about the hip occur in 280,000 Americans annually, and are expected to increase to 500,000 annually over the next 40 years as the average age of the population increases.1 However there is a bimodal distribution of these fractures, with 2–3% occurring in young patients less than 50 years old after high-energy trauma.2,3 These fractures frequently have a more vertical orientation, are subject to high shear forces and construct failure following repair. Rates of non-union in young patients are reported from 10–30%.2,3,4,5,6 The treatment of choice for these fractures is anatomic reduction, preservation of the blood supply and internal fixation.
Classification of femoral neck fractures is based upon the verticality of the fracture orientation as originally described by Pauwels in 1935. Type I fractures are less than 30° from the horizontal, Type II fractures are 30–50° from the horizontal, and Type III fractures are greater than 50° from the horizontal.7 Vertical femoral neck fractures (Pauwels Type III) (OTA classification 31-B2.3) are often high-energy injuries occurring in young patients.3,8,9 These challenging injuries experience high shear forces explaining the relatively high rates of non-union and potential for other clinical problems, including hardware cutout and the need for revision surgery.7,8 Most biomechanical studies support the use of fixed angle devices to maximize stability for Pauwels III fractures.10,11,12
Despite this, in clinical practice preferred treatment is split between fixed angle devices and cannulated screw configurations for Pauwels III fractures.13 The inverted triangle, with screws abutting the anterior, inferior and posterior cortices, is the most commonly utilized configuration for Pauwels I and II fractures and thus far has been the most biomechanically stable screw arrangement analyzed for these fractures.14,15,16 It is also often used for fixation of Pauwels III fractures despite a paucity of biomechanical data.13 While a configuration consisting of a horizontal screw orthogonal to the vertical fracture line has been proposed, little biomechanical data exists.17 Nowotarski et al showed this construct, with an inferior off axis screw, had greater axial stiffness than CHS constructs and inverted triangle constructs.17
The horizontal cross screw, similar to the 4.5mm cortical transverse calcar screws used in a previous study (see Figure, Supplemental Digital Content 1 which demonstrates this previously tested construct), was modified for this experiment by using an additional cannulated screw superiorly (Figure 1B). This was done to theoretically engage the denser bone in the central and inferior regions of the femoral head, recently demonstrated on micro CT studies.18 This positioning also has the added theoretical advantage of allowing for retrograde intramedullary nail placement in the case of ipsilateral femoral shaft fractures. Femoral neck fractures are associated with shaft fractures 1% to 9% of the time, with 20% to 50% of femoral neck fractures missed initially.19 This screw arrangement also helps to avoid stress risers in the subtrochanteric region associated with the inferior screw in the inverted triangle configuration.20,21
Fig 1a-c.
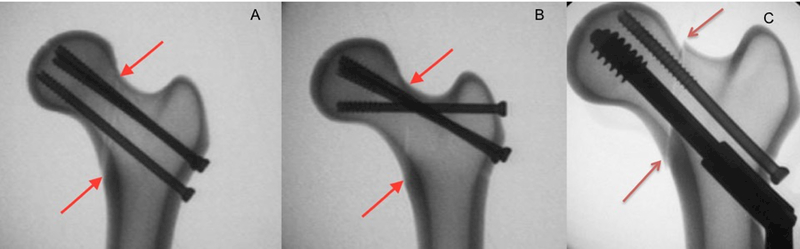
The A-P view under fluoroscopy of the three groups. To the left (2a) is the inverted triangle, 2b is the modified transverse screw and 2c is the CHS with derotation screw. The arrows indicate the location of the osteotomy.
While there are many studies comparing fixation strategies for vertical femoral neck fractures, there is, in fact, little consensus among experts. A recent survey of two-hundred and seventy-two active Orthopedic Trauma Association (OTA) members illustrates this point. Treating surgeons had very disparate responses when asked their preferred method of treatment for vertical femoral neck fractures in young healthy patients: 47% selected sliding hip screws with or without a derotational screws, 28% selected cannulated screws with an off-axis screw, and 15% selected parallel cannulated screws.13
The purpose of this study was to use a synthetic bone model to compare the static and dynamic biomechanical properties of three means of fixing vertical femoral neck fractures in healthy bone.
Materials and Methods
Experimental Model:
Thirty standard, left-sided 4th generation synthetic composite femora (model #3,403 Sawbones, Pacific Labs, Vashon, WA) equally allocated among three groups. These femora have a size, shape and consistency similar to the type of human bone seen in patients who typically sustain Pauwels III fractures, including dense cortices and thick sub-chondral bone. Anatomic reduction was facilitated by drilling holes, using fluoroscopy, for the planned fixation screw paths before creating the vertical osteotomies in all synthetic femora.
Vertical osteotomies to simulate Pauwels III femoral neck fractures were created using a circular saw. These osteotomies were initiated at the junction of the femoral head and neck superiorly and oriented parallel to a line down the femoral shaft (90° from the horizontal) (Figure 1A-C).10
Fixation Methods:
The first group was fixed in an inverted triangle (IT) configuration using 6.5mm titanium cannulated screws with 16mm threads (Asnis III, Stryker, Mahwah, NJ) (Figure 1A). The femurs had three screw paths pre-drilled with a 4.9mm drill bit. These parallel paths abutted the inferior, posterior and anterior cortices of the femoral neck. The second group was fixed with a modified cross screw configuration (CS), again using 6.5mm cannulated titanium screws with 16mm threads (Asnis III, Stryker, Mahwah, NJ) (Figure 1B). Anterior and posterior screw paths were placed exactly as they were in the first group. The third path was created proximally on the lateral femoral cortex so as to cross the intended osteotomy at a 90° angle, and engage the inferior femoral head and neck cancellous trabeculae. Screw paths were standardized using custom templates created for each group, and all paths were confirmed on fluoroscopy. Depths for all screws were approximately 5mm from the articular surface to allow screw placement into the material that simulates subchondral bone. All screws were compressed simultaneously in the inverted triangle group, while the cross screw was compressed first in the modified cross screw group, followed by the parallel anterior and posterior screws.
The third group was fixed with a 130 degree compression hip screw and two-hole side plate construct (CHS) (Omega3, Stryker, Mahwah, NJ) and 6.5mm cannulated titanium derotation screw with a 16mm thread length (Figure 1C). The CHS trajectory was standardized to a 130 degree angle as this provided the best fit to the saw bones allowing for a center-center tip-apex ending point of a 90mm compression screw. A 130 degree jig was used to position the guide wire in each femoral head, each femoral head was then drilled with a step drill to the subchondral area of the femoral head. A guide wire for the parallel derotation screw was then placed and predrilled. After instrumentation, all CHS screws were radiographically determined to have a tip apex distance of between ten and fifteen millimeters.22 Prior to mechanical testing, each CHS construct had a 32mm compression screw placed and tightened to allow for compression of the fracture site. Femurs were prepared two at a time from each treatment group to prevent a learning curve bias.
Biomechanical Testing:
Cycles to Failure: Survival Testing
After fixation, all femora were osteotomized at the distal diaphysis and potted in a 2-part polyurethane compound (Smooth-On, Easton, PA), with the femur oriented co-axially within polyvinyl chloride tubes of 2-inch diameter for mechanical testing. The bone model was placed in a custom fixture that allowed for load orientation in 20° of adduction to simulate single leg stance (See Figure, Supplemental Digital Content 2 for a visual representation of the testing apparatus).11 The loading program consisted of several parts. Initially, each femur was incrementally loaded up to 1,400N at a rate of 50N per second with a cycling rate of 3Hz (1,400 N meant to simulate the force of single leg stance for a 70kg person).10,23 Next, specimens that survived the incremental loading were loaded at 1,400N for 10,000 cycles, a number chosen to represent the average number of gait cycles performed in a 4–6 week post-op period.10,11 Femora that survived the initial cyclic loading were then taken through 5,000 cycles at 2,450N (a force of 3.5 times body weight meant to simulate single leg stair climb).24 Finally, femora that survived the entire cyclic loading protocol were loaded to failure at 1mm per minute.
Load to Failure: Structural Properties
Loads were applied utilizing a servohydrolic material testing system (MTS 810, MTS Corp, Prairie Eden, MN). Cycles to failure and maximum failure load were recorded directly from the test frame. Stiffness was calculated using custom software (MTS Flex Test SE MPT 3.5B Labview; National Instruments Corporation, Austin, TX). Displacement vs cycle count was observed in real time during testing to assess deformation of the constructs and to determine if functional failure was reached. Functional failure was defined as osteotomy displacement greater than 10mm, screw migration greater than 5mm, or fracture extension beyond the plane of the osteotomy.
Statistics:
Cycles to Failure: Survival Analysis
Survival events were categorized as catastrophic failure or functional failure, all specimens that completed the 15,000 cycle protocol were deemed run out. The Kaplan-Meier method was used to estimate the survival functions which were compared between treatment groups using Wilcoxon weighting. A Tukey adjustment for multiple comparisons was used.
Load to Failure: Structural Properties
Stiffness was found to be positively skewed and was log (natural) transformed before subsequent statistical analysis. The linear relationship between construct structural properties (maximum load and stiffness) and treatment (CS, CHS, and IT; Tukey adjustment for multiple comparisons) were assessed using general linear modeling. In all cases statistical significance was set to p < 0.05 a priori. SAS was used for all statistical analyses (version 9.4, Cary, NC).
Results
Mean cycles to failure, failure load and axial stiffness for the three fixation methods are shown in Table 1.
Table 1:
Mean cycles to failure, failure load and axial stiffness for the three fixation methods are shown.
| Cycle To Failure | Load to Failure (N) |
Axial Stiffness (N/mm2} |
|
|---|---|---|---|
| Cross Screw 95% Cl |
13,332 | 3,870 3307, 4433 |
663.06 388, 698 |
| Inverted Triangle 95% Cl |
13,592 | 3,756 3193, 4319 |
620 396, 712 |
| CHS 95% Cl |
15,205 | 5653 5256, 6052 |
1242 958, 1450 |
| p value (CS VS IT, CHS VS IT, CHS vs CS) |
0.9111, 0.1117, 0.0344 |
0.7669, <0.0001, <0.0001 |
0.9222, 0.0005, 0.0005 |
Cycles to Failure: Survival Analysis
All constructs in the three groups survived the initial ramp loading to 1,400 N and 10,000 cycles at 1400 N (See Table, Supplemental Digital Content 3 for a table representation of cycles to failure). All specimens that failed in each group by screw toggling at the lateral cortex and subsequent fracture displacement. No differences were found with cycles to failure when comparing the CHS and the IT group or the CS and the IT group. (Fig 2)
Fig 2.
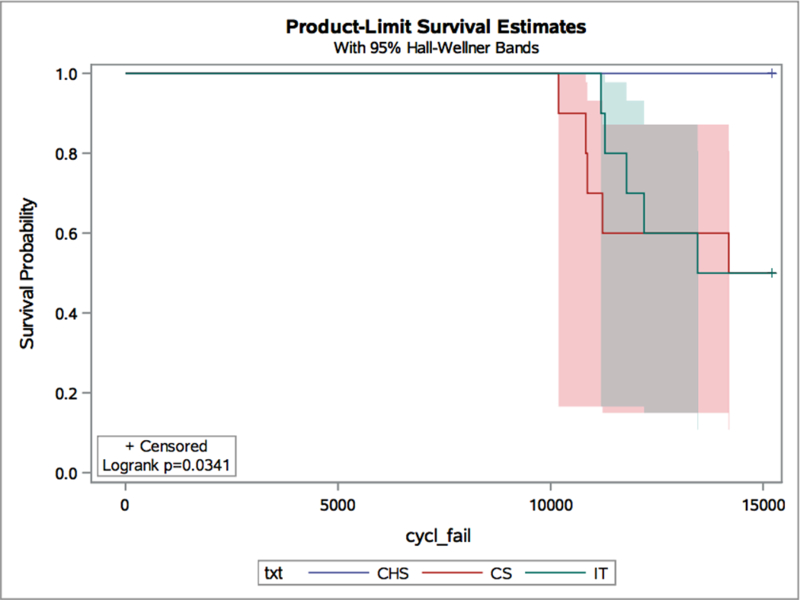
The average number of cycles to failure for each group. All failures that occurred during cyclic loading occurred at 2450N. The y-axis is the average number of cycles. The cannulated screw groups were not significantly different from each other (p=0.911). The CHS group had longer survival than both cannulated screw groups (CHS vs CS p= 0.0344; CHS vs IT p= 0.117).
Load to Failure
Failure loads were determined only for the specimens that completed cyclic loading at both 1,400 and 2,450 N (5, 10, and 5 samples in the CS, CHS, and IT groups, respectively). The group stabilized with modified CS configuration sustained an average maximum failure load of 3,870 [3307, 4433] N (square brackets indicate the 95% confidence interval) compared to 3,756 [3193, 4319] N in the IT group (p=0.7669) (Figure 3). There was no clear difference in the failure mechanism of the two groups. There was no screw toggling, backing out, or bending. In all specimens the primary mode of failure was collapse through the simulated proximal femoral trabecular bone at the core of the specimen, with subsequent screw cutout and inferior displacement.
Fig 3.
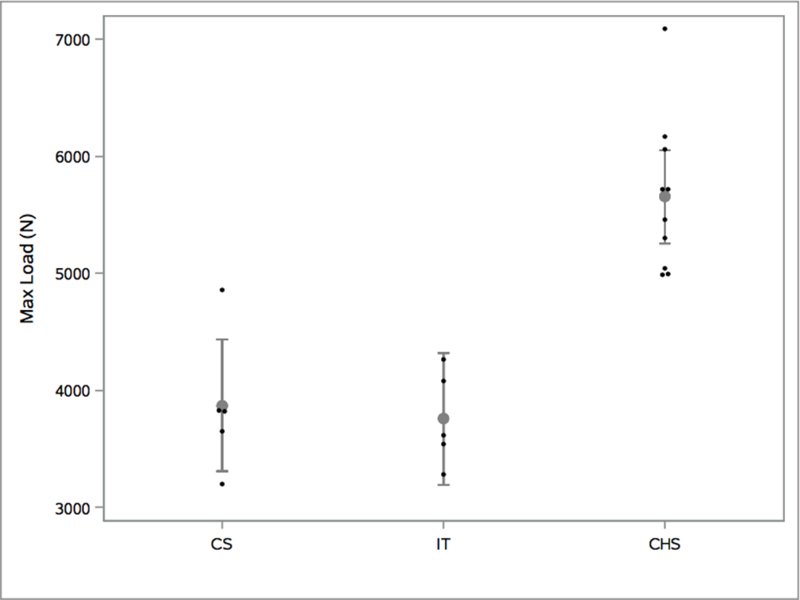
The max failure load of each group. The y-axis is the load to failure in N. The cannulated groups were not significantly different from each other (p=0.7669). The CHS group had a higher maximum load to failure than both cannulated groups (CHS vs CS p<0.0001; CHS vs IT p< .0001).
The CHS group had a significantly higher average maximum failure load at 5,654 [5256, 6052] N (CHS vs CS p< 0.0001; CHS vs IT p<0.0001) (Figure 3). For all specimens, the primary mode of failure was collapse through the simulated bone with screw cutout and inferior displacement.
Axial Stiffness
There was no significant difference in axial stiffness between the modified cross screw (CS) and inverted triangle (IT) groups 520 [388, 698] and 531 [396, 712] N/mm, respectively. The axial stiffness of the CHS group was significantly higher than the other two groups 1,179 [958, 1450] N/mm (CHS vs CS p= 0.0005; CHS vs IT p=0.0005) (Figure 4).
Fig 4.
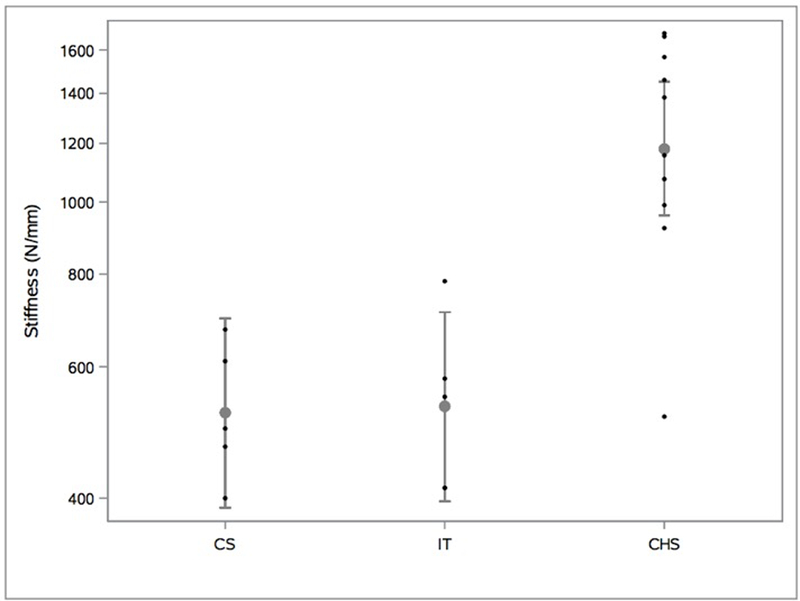
The axial stiffness of each group. The y-axis is the axial stiffness in N/mm. The cannulated screw groups were not significantly different from each other (p=0.9222). The CHS group was significantly more stiff than either cannulated screw group (CHS vs CS p= 0.0005; CHS vs IT p=0.0005).
Discussion
The key finding of this study was that CHS constructs demonstrated greater failure loads and axial stiffness compared to two different cannulated screw constructs in a synthetic model simulating a Pauwels III femoral neck fracture. While CHS constructs survived more cycles of loading, this was only statistically significant when compared to the IT group. Our model was unable to distinguish any statistical differences in cycles to failure or structural properties between the cannulated screw groups.
Despite the majority of biomechanical data suggesting that fixed angle devices are necessary to adequately treat Pauwels III femoral neck fractures, it is still common practice to use cancellous cannulated screws with and without “off-axis” screws.10,11,12,13 Reasons for this likely include that it is a less technically demanding procedure, ease of insertion and decreased blood loss associated with less invasive surgery.3,13 Moreover, with the modified cross screw configuration proposed in this study, retrograde intramedullary nail placement in the case of ipsilateral femoral shaft fractures is possible and stress risers in the subtrochanteric region associated with the inferior screw in the inverted triangle configuration can be avoided.19,20,21
Biomechanically, an “off-axis” or transverse screw placed orthogonally to the fracture site allows for greater compression and therefore ability to withstand high shear forces in Pauwels III fractures. This construct contrasts with the traditional inverted triangle configuration which, by its very nature, prevents perpendicular screw placement. Additionally, while the inverted triangle more effectively resists torsion, it does not equally counter vertical shear and bending forces that are known to be the dominant deforming forces in vertical femoral neck fractures.4,8
Given the mode of failure during cyclic loading of the cancellous screw groups, this appears most likely related to the absence of a fixed angle construct. This was seen in previous biomechanical work performed by Nowotarski et al.17 However, our results differed from the study by Nowotarski et al, which demonstrated greatly improved axial stiffness with a transverse lag screw compared to the standard inverted triangle (2207.23 N/mm vs 3029.89 N/mm p<0.05) and compared to a compression hip screw (CHS) with a derotation screw (3029.89 N/mm vs 2778.99 N/mm).17
In their study, Nowotarski et al used 3rd generation sawbones, which have the same geometry as the 4th generation, but different resistance to fatigue and fracture. The femurs also differ in tensile as well as compressive properties and it has been shown that 4th generation sawbones better represent the biomechanical properties of human bone.25 There are several other possible reasons for the discrepancy in axial stiffness obtained between the two studies. First, the protocol in the study by Nowotarski et al involved placement of a transverse screw with bicortical purchase into the femoral calcar. This screw placement likely provided a mechanical advantage, but utilized a technique not described in the clinical literature. Also, in the setting of a high angle femoral neck fracture, this piece of femoral calcar may be too small for reliable lag screw placement. Additionally, Nowotarski et al loaded the femurs at a much lower force of 350N in 7° of valgus to simulate partial weightbearing during two-legged stance. This is in contrast to the protocol used by the authors in which the femurs were loaded to a force of 1400N and then 2450N in 20° of adduction to simulate 2x and 3.5x weight bearing during single leg stance and stair climb, respectively. It is unclear whether a calcar screw could create a stress riser with risk of peri-trochanteric fracture if used in clinical practice.
The present study was unable to determine any statistical differences in cycles to failure, load to failure or axial stiffness of two cannulated screw configurations used by nearly half of orthopaedic trauma surgeons, according to survey data.12 The present study also demonstrates improved load to failure and axial stiffness of a CHS with derotation screw construct to both of cannulated screw groups. It is important to note that these configurations may not be equivalent in the clinical situation as several aspects of the current design study could have led to an underestimation of the biomechanical strength of the constructs tested. First, femoral neck fractures were created using smooth saw cuts. This most likely did not simulate the jagged nature of a true femoral neck fracture and therefore even with anatomic reduction, fracture interdigitation and the potential inherent stability associated with this was not obtained. Second, the osteotomy angle used in this analysis (90° from the horizontal) was highly vertical, maximizing the potential for shear force creation.
Limitations of this study include those inherent in the synthetic bone model used, recent studies based on micro CT have shown that the densest bone in the femoral head is located centrally and inferiorly.18 Because the synthetic cancellous bone used in this study has a uniform density of 0.27g/cm3 throughout the femoral head (normal range from 0.11– 1.11 g/cm3), it is possible that utilization of cadaveric or live specimens would be associated with improved fixation stiffness and strength of the cross screw configuration. However, these synthetic femurs, which are engineered to mimic real properties of bone, have been used and validated in previous studies.17,25,26 These specimens were chosen because they are modeled after young healthy bone, which is the target population for this study, and because these synthetic femurs greatly reduced variability in experimentation. Our study was 95% powered to detect a difference of 1140N of load to failure, and 285 N/mm of axial stiffness between construct groups. This power analysis was adequate to demonstrate differences between the CHS group when compared to the IT or CS group, however, we were unable to determine if any differences between the IT or CS group were significant as the differences fell below the threshold of our power analysis.
Not all of the physiologic force components associated with ambulation and muscle contraction were simulated. Femora were statically and dynamically axially loaded in one direction, but torsional forces to account for the changing direction of loads during ambulation as the hip flexes and extends were not tested. While one construct could be stronger in torsion, those forces on the head are relatively low due to the low coefficient of friction of the hip joint.
In conclusion, no statistically significant differences were found for axial stiffness, cycles to failure, or ultimate load to failure between the modified cross screw and inverted triangle groups for three screw fixation. In terms of axial stiffness and load to failure, the CHS construct was demonstrated to be biomechanically superior validating other studies. Cycles to failure were greater for the CHS constructs compared to both cannulated screw constructs, however this was only statistically significant when comparing the CHS group to the IT group. Further cadaveric studies of fixation methods may be of value. However, based upon the results of our investigation, if anatomic or pre-existing implant concerns preclude the use of a CHS construct, either cannulated screw configuration could be used based on the patient’s anatomy, other necessary implants or surgeon preference. Our study demonstrated that CHS constructs in an in vitro model have superior load to failure and axial stiffness to cannulated screw constructs for fixation of Pauwels III femoral neck fractures. Based on our results, and those of previous studies, we recommend that treating surgeons consider the use of CHS constructs instead of cannulated screw constructs for the treatment of Pauwels III femoral neck fractures when anatomic or hardware concerns do not preclude the use of CHS constructs.
Supplementary Material
Acknowledgments
Sources of Funding:
Dr. Born is a consultant to Stryker Orthopedics but received no compensation in this study.
The authors have received funding in the form of implant donation for this study from Stryker Trauma (Mahwah, NJ).
This study was supported in part by a grant from the National Institutes of Health; (2P20 GM104937) (COBRE Bioengeering Core).
Footnotes
Conflicts of Interest
Level of Evidence: N/A (Basic Science)
References
- 1.Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos. Int. J. Establ. Result Coop. Eur. Found. Osteoporos. Natl. Osteoporos. Found. USA 1992. November;2(6):285–289. [DOI] [PubMed] [Google Scholar]
- 2.Protzman RR, Burkhalter WE. Femoral-neck fractures in young adults. J. Bone Joint Surg. Am 1976. July;58(5):689–695. [PubMed] [Google Scholar]
- 3.Ly TV, Swiontkowski MF. Management of femoral neck fractures in young adults. Indian J. Orthop 2008;42(1):3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swiontkowski MF, Winquist RA, Hansen ST. Fractures of the femoral neck in patients between the ages of twelve and forty-nine years. J. Bone Joint Surg. Am 1984. July;66(6):837–846. [DOI] [PubMed] [Google Scholar]
- 5.Kofoed H Femoral neck fractures in young adults. Injury 1982. September;14(2):146–150. [DOI] [PubMed] [Google Scholar]
- 6.Haidukewych GJ, Rothwell WS, Jacofsky DJ, et al. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J. Bone Joint Surg. Am 2004. August;86–A(8):1711–1716. [DOI] [PubMed] [Google Scholar]
- 7.Bartonícek J Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J. Orthop. Trauma 2001. July;15(5):358–360. [DOI] [PubMed] [Google Scholar]
- 8.Liporace F, Gaines R, Collinge C, et al. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J. Bone Joint Surg. Am 2008. August;90(8):1654–1659. [DOI] [PubMed] [Google Scholar]
- 9.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma 2007. December;21(10 Suppl):S1–133. [DOI] [PubMed] [Google Scholar]
- 10.Aminian A, Gao F, Fedoriw WW, et al. Vertically oriented femoral neck fractures: mechanical analysis of four fixation techniques. J. Orthop. Trauma 2007. September;21(8):544–548. [DOI] [PubMed] [Google Scholar]
- 11.Baitner AC, Maurer SG, Hickey DG, et al. Vertical shear fractures of the femoral neck. A biomechanical study. Clin. Orthop 1999. October;(367):300–305. [PubMed] [Google Scholar]
- 12.Bonnaire FA, Weber AT. Analysis of fracture gap changes, dynamic and static stability of different osteosynthetic procedures in the femoral neck. Injury 2002. December;33 Suppl 3:C24–32. [DOI] [PubMed] [Google Scholar]
- 13.Luttrell K, Beltran M, Collinge C. Pre-operative Decision-Making in the Treatment of High-Angle “Vertical” Femoral Neck Fractures in Young Adult Patients. J. Orthop. Trauma 2014. April 1; [DOI] [PubMed]
- 14.Alves T, Neal JW, Weinhold PS, et al. Biomechanical comparison of 3 possible fixation strategies to resist femoral neck shortening after fracture. Orthopedics 2010. April;33(4). [DOI] [PubMed] [Google Scholar]
- 15.Selvan VT, Oakley MJ, Rangan A, et al. Optimum configuration of cannulated hip screws for the fixation of intracapsular hip fractures: a biomechanical study. Injury 2004. February;35(2):136–141. [DOI] [PubMed] [Google Scholar]
- 16.Zdero R, Keast-Butler O, Schemitsch EH. A biomechanical comparison of two triple-screw methods for femoral neck fracture fixation in a synthetic bone model. J. Trauma 2010. December;69(6):1537–1544. [DOI] [PubMed] [Google Scholar]
- 17.Nowotarski PJ, Ervin B, Weatherby B, et al. Biomechanical analysis of a novel femoral neck locking plate for treatment of vertical shear Pauwel’s type C femoral neck fractures. Injury 2012. June;43(6):802–806. [DOI] [PubMed] [Google Scholar]
- 18.Jenkins PJ, Ramaesh R, Pankaj P, et al. A micro-architectural evaluation of osteoporotic human femoral heads to guide implant placement in proximal femoral fractures. Acta Orthop 2013. October;84(5):453–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tornetta P, Kain MSH, Creevy WR. Diagnosis of femoral neck fractures in patients with a femoral shaft fracture. Improvement with a standard protocol. J. Bone Joint Surg. Am 2007. January;89(1):39–43. [DOI] [PubMed] [Google Scholar]
- 20.Pelet S, Leyvraz PF, Garofalo R, et al. Sub- or intertrochanteric fracture following screw fixation of an intracapsular proximal femoral fracture: true complication or technical error? Swiss Surg. Schweiz. Chir. Chir. Suisse Chir. Svizzera 2003;9(2):82–86. [DOI] [PubMed] [Google Scholar]
- 21.Kloen P, Rubel IF, Lyden JP, et al. Subtrochanteric fracture after cannulated screw fixation of femoral neck fractures: a report of four cases. J. Orthop. Trauma 2003. March;17(3):225–229. [DOI] [PubMed] [Google Scholar]
- 22.Baumgaertner MR, Curtin SL, Lindskog DM, et al. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Joint Surg. Am 1995. July;77(7):1058–1064. [DOI] [PubMed] [Google Scholar]
- 23.Denham RA. Hip mechanics. J. Bone Joint Surg. Br 1959. August;41–B:550–557. [DOI] [PubMed] [Google Scholar]
- 24.Crowninshield RD, Johnston RC, Andrews JG, et al. A biomechanical investigation of the human hip. J. Biomech 1978;11(1–2):75–85. [DOI] [PubMed] [Google Scholar]
- 25.Heiner AD. Structural properties of fourth-generation composite femurs and tibias. J. Biomech 2008. November 14;41(15):3282–3284. [DOI] [PubMed] [Google Scholar]
- 26.Cristofolini L, Viceconti M, Cappello A, et al. Mechanical validation of whole bone composite femur models. J. Biomech 1996. April;29(4):525–535. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


