Abstract
Rationale: Bronchoscopy procedures should be tracked for safety, quality improvement, and federal regulations.
Objective: The aim of this study was to develop and test a method for evaluating flexible bronchoscopy use and outcomes using the electronic medical record (EMR) system in current clinical use at a large children’s hospital.
Methods: We created a custom bronchoscopy procedure note for our EMR system (Epic Systems Corporation) to track demographics, bronchoscopist, coordinated procedures, and outcome. Unplanned outcomes in children were defined as a disposition (admission to the hospital or elevation of care) after flexible bronchoscopy that differed from the preoperative plan. Readmissions to the hospital and emergency visits within our hospital system were also tracked electronically. Unplanned outcomes and readmissions were evaluated by a bronchoscopy quality team.
Measurements and Main Results: Over 2.5 years, we tracked 1,297 bronchoscopic procedures performed on 1,161 patients (60% male, 78% American Society of Anesthesiologists class 2 or 3, mean age 5.5 yr [range, 0.02–40 yr]). Overall, 27 unplanned outcomes occurred (2.1%). The risk of unplanned outcomes did not appear to be different between procedures performed by a trainee with faculty oversight and those performed by a faculty member alone. Patients with multiple same-day procedures were more likely to have unplanned outcomes (21 of 27 [78%], P = 0.004) than were patients who had flexible bronchoscopy alone. The relative risk (RR) of having an unplanned outcome was not different from flexible bronchoscopy alone in the subset of patients with multiple procedures coordinated through our multidisciplinary aerodigestive clinic (RR 0.7; 95% CI, 0.1–3.4). The risk of unplanned events was significantly elevated in children with coordinated procedures scheduled outside the aerodigestive group (RR, 5.8; 95% CI, 2.4–14.5). Ten patients (<1%) were readmitted or seen urgently within 1 week; three of these unplanned outcomes were attributed to complications of the bronchoscopy.
Conclusions: An EMR system may be used to track procedural outcomes. Unplanned outcomes after flexible bronchoscopy were infrequent at our institution. Children who underwent multiple procedures had unplanned outcomes more often; however, the subset of children who underwent coordinated procedures through our multidisciplinary aerodigestive clinic did not demonstrate this increased risk.
Keywords: aerodigestive, diagnostic techniques, flexible bronchoscopy, safety
The development of small flexible bronchoscopes vastly improved the diagnostic and therapeutic armamentarium for pediatric pulmonary physicians (1–4). Early case series focused primarily on which children might derive clinical benefit from flexible bronchoscopy, with less focus on the complications (5–10). Over the past 2 decades, the risks of bronchoscopy have been explored in the literature. The risk of serious events in children has been reported to be low (11–13), although death has been reported (7, 14).
Previous reports of complications and risks are limited by physician recall and by the manual collection of data from patient charts and hospital records. In addition, complication rates are self-reported, often with only a small number of bronchoscopists performing the procedures. With widespread use of electronic medical records (EMRs), data capture can be automated. When our hospital adopted EPIC (Epic Systems Corporation, Madison, WI) as our EMR system, the bronchoscopy procedure note was identified as an area of potential improvement that might be easy to track.
The purpose of this report is to demonstrate the successful use of our EMR to automatically identify and quantify the bronchoscopic experience at a large tertiary children’s hospital with 22 attending bronchoscopists performing procedures. Our quality team regularly reviewed automated bronchoscopy outcome reports, which allowed us to optimize the electronic note and to evaluate our program. We adjusted the automated reports to facilitate their use by external accrediting agencies as well as for internal medical staff reviews. This report details our findings of 1,297 bronchoscopic procedures completed over a 2.5-year period at Children’s Hospital Colorado. Some of the results of these studies have been reported previously in the form of an abstract (15).
Methods
Flexible Bronchoscopy
Flexible bronchoscopy is performed on children in a number of locations in our institution. The majority of flexible bronchoscopies are performed in the operating room or in a nonsterile endoscopy suite under general anesthesia administered by a pediatric anesthesiologist or anesthetist. These are performed either nasally without a supplemental airway or through laryngeal mask airway or endotracheal tube on the basis of the indications of the procedure and the preference of the attending bronchoscopist. Supplemental oxygen is used routinely to try to avoid desaturations that might interrupt the procedure and to prevent hemodynamic instability.
Coordination of flexible bronchoscopy, rigid bronchoscopy, and upper intestinal endoscopy on children seen as part of the multidisciplinary aerodigestive program occurs most weeks. Flexible bronchoscopies are also combined with otolaryngological, gastrointestinal, and other procedures (general surgery, dental, radiology, etc.) outside the aerodigestive program in an effort to limit episodes of general anesthesia.
Flexible bronchoscopies are performed in patients in the pediatric, cardiac, and neonatal intensive care units (ICUs) by pediatric pulmonary faculty and fellows. In this situation, sedative and analgesic medications are administered by ICU staff. Flexible bronchoscopy with tracheostomy is performed in unsedated children in the hospital and in the outpatient clinic. Only flexible bronchoscopies performed by faculty and fellows in the pulmonary section who used the bronchoscopy procedure note in the EMR were reviewed for this project.
Creation of Electronic Note
We created a custom bronchoscopy note in EPIC, our EMR (see online supplement), to track demographics, bronchoscopist, coordinated procedures with other services, and outcome. Unplanned outcomes in children were defined a disposition (admission to the hospital or elevation of care to an ICU) after flexible bronchoscopy that differed from the preoperative plan. Complications were assessed in all bronchoscopy procedures rather than in just those with unplanned outcomes. Complications during the bronchoscopy were defined as events during the procedure that, in the opinion of the bronchoscopist, transiently interrupted the procedure or terminated the procedure early. Predefined options for selection in the note included hypoxemia, laryngospasm, bronchospasm, cardiac complications, bleeding, and other complications.
All faculty and fellow trainees were instructed in the definitions of the outcomes and complications and in the proper way to complete the procedure note. They were asked to describe in narrative form the treatment given for any complications reported. Bronchoscopy notes are completed shortly after completion of the procedure and can be amended if escalation of care occurs after the operative note was completed. Providers were instructed to amend their bronchoscopy note if unexpected escalation occurred after their note was completed, but we did not systematically review each procedure to make sure an addendum was created if escalation occurred. Because of concern about missing untoward events after note completion, the function to identify emergency department visits and admissions within 1 week of the procedure was added.
Readmissions to the hospital and emergency department or urgent care visits within the hospital system within 1 week of the procedure were compiled electronically, and all were reviewed by the quality team in an effort to relate the event to the bronchoscopy. Bronchoscopy data were collected monthly using automated functions within the medical record, collated, and stored in a secure research electronic data capture (REDCap) database (16). This report is based on procedures documented with the EMR; no attempts to review procedures outside the EMR were made.
All flexible bronchoscopies performed by the pediatric pulmonary section use the bronchoscopy note described in this report. The final automated report detailed in this article was captured after the most recent iteration of the note template. It is the authors’ intent to modify the note as indicated to improve the quality of the data captured as this evaluation continues.
Review Process
This project was considered a “program evaluation” and did not require institutional or quality board review. Our bronchoscopy quality team (E.M.D., G.S.K., P.C.S.) made modifications to the procedure note during the third quarter of 2012 to improve capture of all the complications and the nature of the complications as described previously. Readmission assessment was added to the analysis after initial review. Verbal and e-mail surveys of all the bronchoscopists were conducted twice yearly at the time each provider’s report was provided, to ensure that the automated process did not miss any unplanned outcomes. Because unplanned events have been uncommon, there is often discussion regarding them. The quality team documents all unplanned outcomes of which they are made aware. The ability of the automatic reports to capture all these events has validated the success of the system.
At quarterly review sessions, the quality team discussed every procedure with an “unplanned outcome” or a documented readmission. Team members did not review their own cases. The causes of the unplanned outcomes were categorized on the basis of the consensus opinion of the quality team. The quality team’s assessment was entered manually into REDCap. During analysis, it appeared that children who underwent multiple same-day procedures were being discussed repeatedly; therefore, data regarding coordinated procedures from the endoscopy suite or operating room were obtained electronically for all patients in the database.
Reports from REDcap, with overall and provider-specific outcome rates and complication rates, were created, including the quality team’s assessment regarding the unplanned outcomes. Descriptive statistics of demographics and outcomes were reviewed. Fisher exact test was used to compare proportions, and relative risk (RR) was calculated for different subgroups. Student’s two-tailed t test was used to compare continuous outcome variables. Spearman’s correlation was used to define the correlation between the number of bronchoscopies performed and the rate of unplanned outcomes.
Results
Between April 2012 and September 2014, 22 pulmonary faculty performed 1,297 bronchoscopies in 1,161 patients. The mean age of the patients was 5.5 years, and 60.4% were male (Table 1). Six hundred fifty-eight flexible bronchoscopies (50.7%) were coordinated with procedures including microlaryngoscopy, rigid bronchoscopy, upper intestinal endoscopy, tonsillectomy, adenoidectomy, lung biopsy, and cardiac catheterization (Table 2). Overall, 27 unplanned outcomes occurred (2.1%). The mean age of these patients was 4.4 years, and 48.1% were male (Table 1). The quality committee determined that these unplanned events were predominantly caused by the risk of the procedure and unexpected findings necessitating a new plan (Table 3). Patient age was not significantly different between children with planned and unplanned outcomes (P = 0.31).
Table 1.
Demographics of patients and flexible bronchoscopy procedures
| Total | Unplanned Events | |
|---|---|---|
| Bronchoscopies, No. | 1,297 | 27 (2.1) |
| Patients, No. | 1,161 | 27 (2.3) |
| Male sex | 784 (60.4) | 13 (48.1) |
| Age, mean (SD), yr | 5.5 (5.7) | 4.4 (5.5)* |
| ASA class | ||
| 1, 2, or 2E | 490 (37.8) | 5 (18.0) |
| 3 or 3E | 451 (34.8) | 15 (55.6) |
| 4, 4E, or 5E | 133 (10.3) | 2 (7.4) |
| None specified | 223 (17.2) | 4 (14.8) |
| Patient status | ||
| Inpatient | 567 (43.7) | 9 (33.3) |
| Outpatient | 657 (50.7) | 15 (55.6) |
| Unrecorded | 73 (5.6) | 2 (7.4) |
| Performed by fellow and faculty | 590 (45.5) | 17 (63.0)† |
| Faculty only | 707 (54.5) | 10 (37.0)† |
| Coordinated aerodigestive procedures | 309 (23.8) | 2 (7.4)‡ |
| Coordinated procedures (not aerodigestive) | 349 (26.9) | 19 (70.4)‡ |
Definition of abbreviation: ASA = American Society of Anesthesiologists.
Data are presented as No. (%) unless indicated otherwise.
P value = 0.31.
There was no significant difference between outcomes of bronchoscopies performed by fellows and those performed by faculty alone (P = 0.08).
There were significantly fewer unplanned events in children who had procedures coordinated within the aerodigestive program compared with those who were not coordinated by the aerodigestive program (P = 0.0005).
Table 2.
Procedures most commonly coordinated with flexible bronchoscopy*
| No. (% of Total Bronchoscopies) | No. with Unplanned Events (% of 27 Unplanned) | |
|---|---|---|
| Aerodigestive rigid bronchoscopy and upper intestinal endoscopy | 309 (23.8) | 2 (7.4) |
| Not aerodigestive | ||
| Rigid bronchoscopy | 129 (9.9) | 11 (40.7) |
| Upper intestinal endoscopy | 35 (2.7) | 1 (3.7) |
| Adenoidectomy with or without tonsillectomy | 26 (2.0) | 0 |
| Cardiac catheterization | 21 (1.6) | 1 (3.7) |
| Lung biopsy | 15 (1.2) | 0 |
| Sleep nasal endoscopy | 12 (0.9) | 0 |
| Endoscopic sinusectomy | 10 (0.8) | 0 |
| Nissen fundoplication | 9 (0.7) | 0 |
Other procedures with unplanned outcomes were combined with peripheral line insertion, supraglottoplasty, laparoscopic gastrostomy tube insertion, dental cleaning, chest computed tomography scan, and brain magnetic resonance imaging.
Table 3.
Causes of unplanned events and readmission after pediatric flexible bronchoscopy as determined by quality committee
| Unplanned Event/Readmission | No. |
|---|---|
| Unplanned events | 27 |
| Part of the risk of the procedure* | 21 |
| Skill of the bronchoscopist | 0 |
| Unexpected finding necessitating new plan† | 14 |
| Risk of a coordinated procedure | 2 |
| Anesthesia complication | 1 |
| Unrelated to procedures | 1 |
| Admission to hospital or seen in emergency department or urgent care | 10 |
| Definitely related to bronchoscopy | 3 |
| Possibly related to bronchoscopy | 0 |
| Unlikely related to bronchoscopy | 3 |
| Definitely not related to bronchoscopy | 4 |
Including hypoxemia requiring supplemental oxygen (n = 9), stridor with increased work of breathing (n = 2), need for noninvasive or invasive ventilation (n = 9), wheezing requiring frequent albuterol (n = 1).
Unexpected findings included foreign body (n = 1), bacterial bronchitis (n = 4), Pneumocystis jirovecii infection (n = 1), vascular ring (n = 2), pulmonary hemorrhage (n = 2), endobronchial mass (n = 1), subglottic stenosis (n = 3).
The number of bronchoscopies performed by our 22 faculty ranged from 1 to 237, and the rate of unplanned outcomes varied from 0 to 0.07, with one outlier of 0.17 in a faculty member with 1 unplanned outcome in only 6 total bronchoscopies. The total number of bronchoscopies performed did not significantly correlate with a provider’s rate of unplanned outcomes (R2 = 0.0056). Although unplanned outcomes were higher in bronchoscopies performed with a fellow trainee, the difference was not statistically significant (P = 0.08).
Patients with multiple same-day procedures were more likely to have unplanned outcomes (21 of 27 [78%], P = 0.004) than were patients who had the flexible bronchoscopy alone. Of this group, 2 of 21 (9.5%) of those patients with coordinated procedures had flexible bronchoscopies as part of the hospital’s multidisciplinary aerodigestive program. The risk of unplanned events in children who had bronchoscopies with other procedures coordinated outside the aerodigestive program was significantly elevated compared with children who underwent flexible bronchoscopy alone (RR, 5.8; 95% CI, 2.4–14.5). This was not the case for children with bronchoscopy and other procedures coordinated through the aerodigestive program. In this group, the risk of an unplanned outcome was not significantly elevated compared with children who underwent a flexible bronchoscopy alone (RR, 0.7; 95% CI, 0.1–3.4).
Ten children (1.3%) were readmitted or seen urgently within 1 week of their bronchoscopy. Of these, only 3 of 10 (33%) were determined to definitely have complications caused by the bronchoscopy because the children had symptoms of respiratory distress, wheezing, or cough (Table 3). The other patients were seen for diagnoses that were either unlikely to be or definitely not related to bronchoscopy (e.g., broken femur, nasogastric tube fell out).
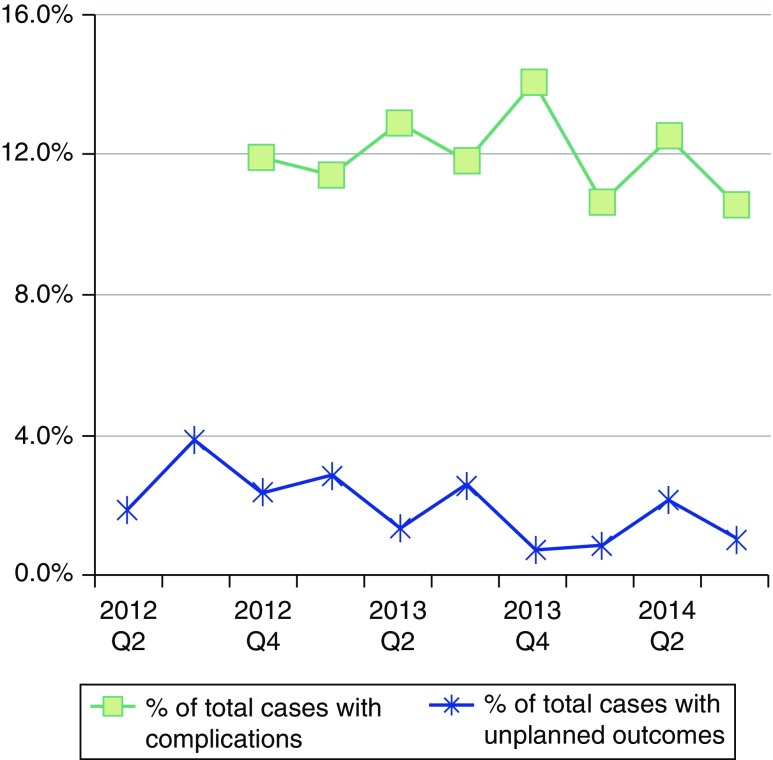
Regarding complications, results from the second and third quarters of 2012 were incomplete, but this was improved by the third quarter of the study after enhancements to the operative note (Figure 1). During the remainder of the project, complications were documented in 134 bronchoscopies (12.6%) (Table 4). There was no difference in the age of children with and without complications, although younger children tended to have more complications (mean age, 5.48 yr vs. 4.65 yr; P = 0.10).
Figure 1.
Decrease in unplanned events over 2.5 years. Complications are reported starting in Q4 of 2012, because of improvements in electronic medical record tracking. Overall unplanned events trended down over time, but the decrease was not statistically significant. Q2 = quarter 2; Q4 = quarter 4.
Table 4.
Frequency of complications during pediatric flexible bronchoscopy starting in Quarter 4 of 2012
| Complications | No. (% of 1,062 Bronchoscopies) |
|---|---|
| Any | 134 (12.6) |
| Hypoxemia | 112 (10.5) |
| Laryngospasm | 19 (1.8) |
| Bronchospasm | 12 (1.1) |
| Bleeding | 8 (0.8) |
| Bradycardia or hypotension | 3 (0.3) |
Adapted by permission from Reference 15.
Because our hospital is not a lung transplant center, transbronchial biopsies are performed infrequently by only four of the pulmonologists included in this report. None of the unplanned outcomes in this report included a transbronchial biopsy. There were no deaths attributed to bronchoscopy. Unplanned outcomes trended down by 1.7% per quarter during the study; however, the change was not statistically significant (P = 0.07) (Figure 1).
Discussion
We successfully manipulated our EMR to track procedural outcomes for the purpose of internal review as well as for required external documentation. The unplanned outcomes after flexible bronchoscopy at our institution were infrequent (2.1%). The complication rate in our patients was low as has been reported in other series describing experiences with flexible bronchoscopy in children, even in critically ill children (4, 10, 12, 17–19). We report no fatal complications, which is also consistent with previous reports. There has been a small number of deaths (7, 12, 14, 20), which have usually been attributed to the underlying or associated illness rather than to the bronchoscopy procedure.
Most of our unplanned events were from either a known risk of the procedure as described in the recent American Thoracic Society standards (21) or from an unexpected finding that required a new therapeutic plan. The most common complication was hypoxemia (10.5%), which has been described as a common occurrence during bronchoscopy (22). Because oxygen desaturation is common with anesthesia and airway manipulation, we only considered desaturation a “complication” if it transiently interrupted or terminated the procedure before completion. Laryngospasm and bronchospasm were less common and generally responded well to intervention. Serious complications such as pneumothorax, respiratory arrest, apnea, bradycardia, and death have been reported (7, 18); therefore, the bronchoscopy team should maintain a healthy respect for the potential for serious adverse outcomes. We believe our low rate of anesthetic complications may have been because our procedures were done under general anesthesia with the assistance of an anesthesia team or with an ICU team managing patient comfort and sedation.
The bronchoscopy quality team did not attribute any of the unplanned events to the lack of skill of the bronchoscopist. There was no difference in the complication rate for bronchoscopies performed by the faculty physician alone vs those performed by a trainee with faculty supervision. Although there appeared to be an increased rate of unplanned outcomes when the bronchoscopy was performed with a fellow, this did not reach statistical significance. The fellow trainees are involved with almost all the bronchoscopies performed in the sickest patients in the ICUs and are rarely involved with bronchoscopies performed in the aerodigestive program. Although previous studies have shown increased complications when trainees are involved (23), we believe the confounders associated with fellow trainee procedures may bias our comparison. Future studies designed to understand these multivariate relationships are planned.
Our success in tracking unplanned outcomes and complications has built the foundation for our team to discuss practice improvement and patient safety. In our cohort, children who underwent multiple procedures were at increased risk of having unplanned outcomes. Although we cannot determine causality in this report, we can hypothesize the factors that may contribute to this risk. Children who undergo multiple procedures likely have higher preoperative risk. A limitation of this evaluation is the use of American Society of Anesthesiologists physical status (class), which was not recorded in 17% of the bronchoscopies; in addition, the American Society of Anesthesiologists guidelines may be insufficient to stratify risk in this population. The number of comorbidities and the severity of comorbidities need to be assessed to adequately determine if the increased preoperative risk biases this outcome.
Children who undergo multiple procedures experience longer anesthetic exposure not only because of the time required for the additional procedures, but also because of the transition between procedures. To further assess this confounder, we are assessing anesthesia time as a risk factor as this project continues.
In this study, we were unable to separate complications caused by flexible bronchoscopy from complications caused by the coordinated procedures. Regarding complications of rigid bronchoscopy, data are limited. However, in a review of approximately 1,300 pediatric rigid airway evaluations, a complication rate of 1.9% was observed (24). These complications ranged from intraoperative bleeding and arrhythmia to postoperative subglottic edema, bronchospasm, and pneumothorax. It is possible that those cases that included a rigid bronchoscopy may have had complications or unplanned escalation of care because of the rigid rather than the flexible bronchoscopy. One may also speculate that the subset of children who undergo combined rigid and flexible bronchoscopies have more comorbidities or have more severe airway disease than do those requiring only one of the procedures. In 7 of the 11 children who underwent combined rigid and flexible bronchoscopies, their unplanned event was caused by an “unexpected finding necessitating a new plan,” including subglottic stenosis, the presence of a foreign body, or bacterial bronchitis (Table 3). By continued tracking of these procedures, we will attempt to understand and reduce the risk in this population.
The risk of unplanned outcomes decreased in the subpopulation of children with procedures coordinated through the multidisciplinary aerodigestive program. It is standard practice in our aerodigestive program to admit children under the age of 3 years for observation if a ph impedance probe is placed as part of the procedure. This may decrease the number of children with unplanned events, because fewer patients will require an unplanned admission to the hospital. We believe that the lower risk of these patients may be partly a result of the set-up of our aerodigestive program. Children are typically seen by multiple providers in clinic the day before their combined procedures. This allows providers to postpone procedures in children with active illness. In addition, this program is composed of a small number of providers from the fields of anesthesiology, pulmonology, otolaryngology, and gastroenterology who have acquired experience in evaluating complex children in the operating room as a team, starting with induction of anesthesia and progressing through pulmonary, otolaryngologic, and gastrointestinal procedures. Although difficult to measure, this experience may play a role in patient outcome.
Multidisciplinary aerodigestive teams are growing in popularity because of the ability to coordinate care, lower the cost, decrease anesthetic exposure, and potentially increase safety and quality (25). Combining procedures under a single anesthetic exposure is common practice in pediatrics. Although it is controversial, there is concern about an increased risk of developmental problems in young children who undergo multiple episodes of general anesthesia compared with those who undergo none or one (26–28). In our cohort, flexible bronchoscopy was combined with another procedure 51% of the time (658 of 1,297). It is imperative that we determine if this practice has innate risk. During this project we demonstrated the need for inpatient and critical care admission in a number of our patients. Although this outcome metric alone does not measure increased risk of the flexible bronchoscopy as much as it implies increased need for anticipatory care for this subpopulation of patients, it does cause increased cost and stress to the family and the health care system. Further studies are needed to determine the best treatment for patients at increased risk of this definition of unplanned events.
Limitations
There are several limitations to this study and our current methods of data collection. Unplanned outcomes were self-reported on operative notes; however, the definition of unplanned outcomes was given to our faculty and fellow trainees. Our complication rate is based on the bronchoscopist’s perception that the symptom (hypoxemia, etc.) prolonged the procedure or caused him/her to terminate the procedure early. This definition is variable by provider, and it is not clear if it underestimates or overestimates clinically meaningful complications. Our automated method of tracking emergency department visits allowed us to look within our own hospital system, but we were unable to quantify visits to other providers. Because of our low rate of complications, a small number of admissions outside our hospital system could change the conclusions of this study. In addition to our ongoing work in this field, we hope that this article encourages other groups to monitor bronchoscopy outcomes and validate our conclusions.
Other limitations include the lack of information regarding important variables such as location of the procedure, entry into the airway (nasal, laryngeal mask airway, or endotracheal tube), and length of the procedure. These variables are being collected prospectively. Despite these limitations, we believe that the automated nature of our tracking system is an improvement over other methods.
Conclusions
In conclusion, this article describes a method for tracking surgical outcomes and presents initial data to the pediatric pulmonology community regarding safe outcomes of flexible bronchoscopy. Comparisons with other institutions are needed to fully understand our data. We believe that our success in tracking bronchoscopy outcomes using EMR provides a foundation for tracking these outcomes within and among hospital systems to understand regional and systematic differences and to share solutions for improved patient care.
Our future goal is to understand how to minimize risk for children who face unplanned events. By electronically tracking indications for bronchoscopy and comorbidities, we strive to increase our understanding of who exactly is at increased risk. We plan to extend these techniques to analyze the outcomes of rigid bronchoscopies performed by otolaryngologists, in an effort to fully understand the risks, benefits, and costs of all bronchoscopies in children at Children’s Hospital Colorado.
Acknowledgments
Acknowledgment
The authors acknowledge Kate Johnston, Dawn Law, and Elin Towler for their help with the EMR and data collection. The authors also acknowledge the support of the pulmonary faculty and fellow trainees as we initiated this electronic tracking system.
Footnotes
Supported by National Institutes of Health/National Center for Advancing Translational Science Colorado Clinical and Translational Science Award grant UL1 TR001082.
Author Contributions: E.M.D. contributed to the study design, review team, and first draft of the manuscript; J.D.P. contributed to data interpretation and manuscript revision; G.S.K. contributed to study design, review team, and manuscript revision; P.C.S. contributed to study design, review team, and writing of the first draft of the manuscript. All authors approved the final version and take accountability for all aspects of the work.
The views expressed in this article do not communicate an official position of the University of Colorado School of Medicine or the Children’s Hospital Colorado.
This article has an online supplement, which is accessible from this issue’s table of contents online at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Wood RE, Fink RJ. Applications of flexible fiberoptic bronchoscopes in infants and children. Chest. 1978;73:737–740. doi: 10.1378/chest.73.5_supplement.737. [DOI] [PubMed] [Google Scholar]
- 2.Nussbaum E. Flexible fiberoptic bronchoscopy and laryngoscopy in children under 2 years of age: diagnostic and therapeutic applications of a new pediatric flexible fiberoptic bronchoscope. Crit Care Med. 1982;10:770–772. doi: 10.1097/00003246-198211000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Wood RE, Postma D. Endoscopy of the airway in infants and children. J Pediatr. 1988;112:1–6. doi: 10.1016/s0022-3476(88)80109-4. [DOI] [PubMed] [Google Scholar]
- 4.Fan LL, Sparks LM, Fix FJ. Flexible fiberoptic endoscopy for airway problems in a pediatric intensive care unit. Chest. 1988;93:556–560. doi: 10.1378/chest.93.3.556. [DOI] [PubMed] [Google Scholar]
- 5.Stillwell PC, Radford PJ. Should all children with stridor undergo flexible bronchoscopy? J Bronchol. 1994;1:276–280. [Google Scholar]
- 6.Downing GJ, Kilbride HW. Evaluation of airway complications in high-risk preterm infants: application of flexible fiberoptic airway endoscopy. Pediatrics. 1995;95:567–572. [PubMed] [Google Scholar]
- 7.Rock MJ. The diagnostic utility of bronchoalveolar lavage in immunocompetent children with unexplained infiltrates on chest radiograph. Pediatrics. 1995;95:373–377. [PubMed] [Google Scholar]
- 8.Connett GJ, Doull IJ, Keeping K, Warner JO. Flexible fibre-optic bronchoscopy in the management of lung complications in cystic fibrosis. Acta Paediatr. 1996;85:675–678. doi: 10.1111/j.1651-2227.1996.tb14123.x. [DOI] [PubMed] [Google Scholar]
- 9.Chan CC, Abi-Saleh WJ, Arroliga AC, Stillwell PC, Kirby TJ, Gordon SM, Petras RE, Mehta AC. Diagnostic yield and therapeutic impact of flexible bronchoscopy in lung transplant recipients. J Heart Lung Transplant. 1996;15:196–205. [PubMed] [Google Scholar]
- 10.Schellhase DE, Fawcett DD, Schutze GE, Lensing SY, Tryka AF. Clinical utility of flexible bronchoscopy and bronchoalveolar lavage in young children with recurrent wheezing. J Pediatr. 1998;132:312–318. doi: 10.1016/s0022-3476(98)70451-2. [DOI] [PubMed] [Google Scholar]
- 11.Picard E, Schwartz S, Goldberg S, Glick T, Villa Y, Kerem E. A prospective study of fever and bacteremia after flexible fiberoptic bronchoscopy in children. Chest. 2000;117:573–577. doi: 10.1378/chest.117.2.573. [DOI] [PubMed] [Google Scholar]
- 12.Nussbaum E. Pediatric fiberoptic bronchoscopy: clinical experience with 2,836 bronchoscopies. Pediatr Crit Care Med. 2002;3:171–176. doi: 10.1097/00130478-200204000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Efrati O, Sadeh-Gornik U, Modan-Moses D, Barak A, Szeinberg A, Vardi A, Paret G, Toren A, Vilozni D, Yahav Y. Flexible bronchoscopy and bronchoalveolar lavage in pediatric patients with lung disease. Pediatr Crit Care Med. 2009;10:80–84. doi: 10.1097/PCC.0b013e31819372ea. [DOI] [PubMed] [Google Scholar]
- 14.Wagener JS. Fatality following fiberoptic bronchoscopy in a two-year-old child. Pediatr Pulmonol. 1987;3:197–199. doi: 10.1002/ppul.1950030314. [DOI] [PubMed] [Google Scholar]
- 15.DeBoer E, Kerby G, Stillwell PC. Measuring pediatric bronchoscopy outcomes using the electronic medical record. Am J Respir Crit Care Med. 2015;191:A1909. doi: 10.1513/AnnalsATS.201509-576OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wood RE. Pitfalls in the use of the flexible bronchoscope in pediatric patients. Chest. 1990;97:199–203. doi: 10.1378/chest.97.1.199. [DOI] [PubMed] [Google Scholar]
- 18.Raine J, Warner JO. Fibreoptic bronchoscopy without general anaesthetic. Arch Dis Child. 1991;66:481–484. doi: 10.1136/adc.66.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamat PP, Popler J, Davis J, Leong T, Piland SC, Simon D, Harsch A, Teague WG, Fortenberry JD. Use of flexible bronchoscopy in pediatric patients receiving extracorporeal membrane oxygenation (ECMO) support. Pediatr Pulmonol. 2011;46:1108–1113. doi: 10.1002/ppul.21480. [DOI] [PubMed] [Google Scholar]
- 20.Wood RE. Spelunking in the pediatric airways: explorations with the flexible fiberoptic bronchoscope. Pediatr Clin North Am. 1984;31:785–799. doi: 10.1016/s0031-3955(16)34645-4. [DOI] [PubMed] [Google Scholar]
- 21.Faro A, Wood RE, Schechter MS, Leong AB, Wittkugel E, Abode K, Chmiel JF, Daines C, Davis S, Eber E, et al. American Thoracic Society Ad Hoc Committee on Flexible Airway Endoscopy in Children. Official American Thoracic Society technical standards: flexible airway endoscopy in children. Am J Respir Crit Care Med. 2015;191:1066–1080. doi: 10.1164/rccm.201503-0474ST. [DOI] [PubMed] [Google Scholar]
- 22.Schnapf BM. Oxygen desaturation during fiberoptic bronchoscopy in pediatric patients. Chest. 1991;99:591–594. doi: 10.1378/chest.99.3.591. [DOI] [PubMed] [Google Scholar]
- 23.Stather DR, MacEachern P, Chee A, Dumoulin E, Tremblay A. Trainee impact on procedural complications: an analysis of 967 consecutive flexible bronchoscopy procedures in an interventional pulmonology practice. Respiration. 2013;85:422–428. doi: 10.1159/000346650. [DOI] [PubMed] [Google Scholar]
- 24.Hoeve LJ, Rombout J, Meursing AE. Complications of rigid laryngo-bronchoscopy in children. Int J Pediatr Otorhinolaryngol. 1993;26:47–56. doi: 10.1016/0165-5876(93)90195-9. [DOI] [PubMed] [Google Scholar]
- 25.Collaco JM, Aherrera AD, Au Yeung KJ, Lefton-Greif MA, Hoch J, Skinner ML. Interdisciplinary pediatric aerodigestive care and reduction in health care costs and burden. JAMA Otolaryngol Head Neck Surg. 2015;141:101–105. doi: 10.1001/jamaoto.2014.3057. [DOI] [PubMed] [Google Scholar]
- 26.Ing C, DiMaggio C, Whitehouse A, Hegarty MK, Brady J, von Ungern-Sternberg BS, Davidson A, Wood AJ, Li G, Sun LS. Long-term differences in language and cognitive function after childhood exposure to anesthesia. Pediatrics. 2012;130:e476–e485. doi: 10.1542/peds.2011-3822. [DOI] [PubMed] [Google Scholar]
- 27.Ing CH, DiMaggio CJ, Malacova E, Whitehouse AJ, Hegarty MK, Feng T, Brady JE, von Ungern-Sternberg BS, Davidson AJ, Wall MM, et al. Comparative analysis of outcome measures used in examining neurodevelopmental effects of early childhood anesthesia exposure. Anesthesiology. 2014;120:1319–1332. doi: 10.1097/ALN.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 28.Rappaport BA, Suresh S, Hertz S, Evers AS, Orser BA. Anesthetic neurotoxicity--clinical implications of animal models. N Engl J Med. 2015;372:796–797. doi: 10.1056/NEJMp1414786. [DOI] [PubMed] [Google Scholar]