Abstract
Perrow's models of organizational technologies provide a framework for analyzing clinical work processes and identifying the management structures and informatics tools to support each model. From this perspective, health care is a mixed model in which knowledge workers require flexible management and a variety of informatics tools. A Venn diagram representing the content of clinical decisions shows that uncertainties in the components of clinical decisions largely determine which type of clinical work process is in play at a given moment. By reducing uncertainties in clinical decisions, informatics tools can support the appropriate implementation of knowledge and free clinicians to use their creativity where patients require new or unique interventions.
Outside health care, information technologies have made possible breakthrough strategies for business success that would otherwise have been impossible. Can health informatics work similar magic and help health care agencies fulfill their social mission while establishing sound business practices? One way to do this would be through personalized health care. Extensive data collected from patients could be aggregated and analyzed to support better decisions for the care of individual patients as well as provide projections of the need for health services for strategic and tactical planning. By making excellent care for each patient possible, reducing the “inventory” of little-needed services, and targeting resources to population needs, informatics can offer a route to the “promised land” of adequate resources and high-quality care.
In Western society, health is perceived as a very great good, almost a supreme good. Accordingly, health care professionals perform within a social covenant to promote health. It is this social contract that differentiates health care from “ordinary” industries. Yet health care, too, must operate by sound business principles or lose the resources necessary to fulfill its mission. As a result, there is a tension in health care between the will to do good and the demand to conserve resources or even to make a profit. Can informatics make any important contribution to either of these opposing forces? Can it even bring them together? And can we learn anything from industries outside health care that will show us the way?
Organizational Technologies: Work Processes and Informatics Support
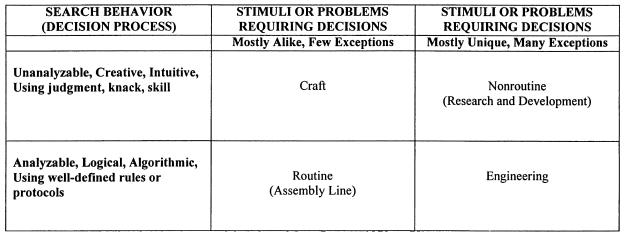
Perrow1 proposed that two dimensions define the ways organizations do their work, which he called “organizational technologies.” The first dimension is the degree of variability of the stimuli or problems to which members of the organization must respond. The second is the nature of the “search behavior” by which members of the organization decide what to do when presented with a stimulus. Perrow dichotomized and cross-classified these dimensions to produce four models of organizational technologies, as shown in ▶. Perrow called the technology models craft, routine (assembly line), engineering, and nonroutine (research and development). He asserted that these models apply to all organizations, including people-processing organizations. Moreover, each model worked best to achieve organizational goals with its own distinctive style of management and communication.
Figure 1.
Organizational technology models (adapted from Perrow1).
Craft
A skilled craftsperson can turn raw material into beautiful creations. One lump of clay may be much like another, but the potter can turn it into a bowl or a mug or a sculpture. If any aspect of health care is practiced as a craft, perhaps it is in the more directly manipulative disciplines, such as surgery. At least during the operation itself, the patient is quite passive, and the surgeon must be the skilled craftsperson who finds the best way to deal with the materials at hand. Most obviously in plastic and reconstructive surgery, but also in other surgical subspecialties, the practitioner must be artful in implementing the science to produce the best result. The management structure that most effectively supports a craft maximizes the autonomy of the practitioner, although more senior practitioners may instruct and give orders to their juniors and assistants. Communication flows downward from the master to the apprentices and helpers. Upward communication consists of responses to the queries of the master practitioner. Information systems that support the practice of health care as a craft will treat each master practitioner as autonomous. These systems will support communication of orders and reporting of results. Because the practitioner's decisions rely heavily on intuition and creativity, decision support will consist of the provision of information requested by the practitioner, which the practitioner considers creatively in reaching a decision.
Routine
Although the notion of “assembly line” health care is anathema to most professionals, approaches such as protocols, standard care plans, guidelines, and clinical pathways do set out to routinize as much of health care as possible, in accordance with “best practices” as determined by consensus or evidence. It is plausible that planning systematically for predictable care events to occur in the appropriate temporal order and at the optimal time would improve both the effectiveness and the efficiency of health care. Indeed, studies have demonstrated significant efficiencies with clinical pathways, and simultaneous positive effects on the quality of care.2,3,4,5,6 Routinized health care is appropriate to the degree that knowledge defines precisely what should be done for a patient. In a completely routinized system, the optimal management structure is the classical bureaucracy, with orders flowing from top to bottom and reports from bottom to top. Decision support for routinized health care consists of access to policies, protocols, and procedures that provide the details of how to carry out the prescribed care processes.
Engineering
Engineering consists of using well-defined logic and algorithms to solve problems. When patients' needs vary from the expectations defined in a clinical pathway, clinicians “engineer” solutions that customize the pathway to accommodate individual differences. Indeed, much of health care might take place near the border between routine and engineering, where clinicians routinize what they can and engineer most of the rest. An excellent example of using engineering to create new routines is the treatment of leg ulcers. Frustrated by the low rate of success of conventional treatments, Burton7 applied knowledge from anatomy, vascular hemodynamics, and dermatology to devise a new and more successful treatment, which has been widely emulated as a best practice. The management structure that supports engineering provides for two-way vertical and lateral communication to solve problems. Decision support includes access to literature and databases that might shed light on a patient's unique problems.
Nonroutine
Nonroutine health care is called for when engineering indicates that known solutions are not effective for a patient. In this quadrant we find true research and development of new diagnostic and treatment modalities and creative problem solving for individual patients. Here the clinician considers the uniqueness of the individual patient and the full range of the sciences and the humanities to devise, often in concert with the patient, an appropriate and unique solution. The clinical researcher formulates hypotheses and implements randomized clinical trials. The management structure for nonroutine health care provides for consultation among peers and the giving of advice based on expertise, rather than on hierarchic models. Decision support would consist of access to a wide variety of knowledge resources and databases, as well as to tools for creative problem solving and research.
Organizational Technologies in Health Care: Mixed Models
After describing the four models, Perrow explained that the borders between them are permeable, so that the work of an organization may cross borders. Moreover, the work of an organization may occur near the junction of technology types (in the case of less pure or blended organizational technologies) or in an outer corner (in the case of the purest, most extreme types). As we have seen, high-quality, cost-effective health care can legitimately occur in all four quadrants. Indeed, activity in all four quadrants is necessary for efficient and effective responses to the variety of health care needs in a situation of growing but imperfect knowledge. The domain of organizational technologies in health care could thus be depicted as a rough circle around the nexus of the four quadrants. Health care workers, according to this view, are necessarily knowledge workers, because even where health care is routinized individual differences among patients need to be accommodated. The appropriate administrative structure would be mixed, accommodating the need for clinicians to vary routines, solve problems, and be creative in meeting both clinical and management demands. To support this practice, health informatics would have to provide for communication to include ad hoc queries and responses, order entry, results reporting, vertical and horizontal messaging, and consultation. Decision support would include access to a variety of knowledge resources and databases, to algorithms and creative problem-solving tools, and to policies, procedures, guidelines, and standard practices.
The Content of Clinical Decisions and the Role of Informatics
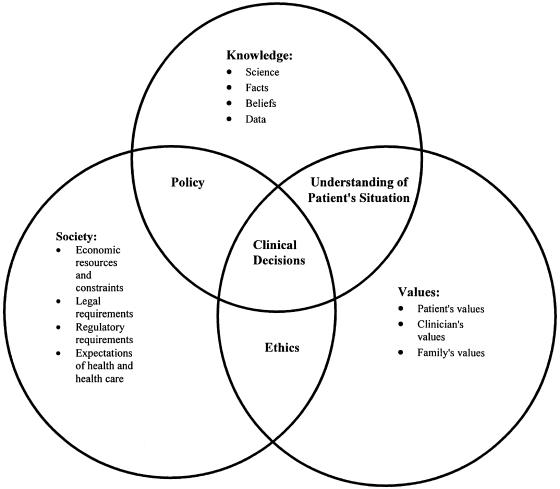
If Perrow's models define types of clinical work processes and the kinds of communication and decision support that these processes require, another model illustrates the content of the clinical decisions at the heart of the work processes. These clinical decisions occur at transactions between a clinician and a patient, in the context of the organization and the society. Indeed, the role of the patient is to be emphasized, because even the most therapeutically ideal prescription will be useless unless the patient accepts it and carries out his or her part in implementing it.
In the Venn diagram shown in ▶, clinical decisions occur at the intersection of knowledge, values, and society. According to this model, human beings make the clinical decisions. The role of informatics is to deliver to the decision makers relevant knowledge and data; policy documents; information about legal, regulatory, and economic requirements and constraints; ethical consultations and statements of ethical positions; and tools for decision analysis that include consideration of subjective values. Where knowledge, societal issues, and values are well defined, uncertainty about the decision problem and how to solve it will be low. Where some or all of these are less well defined, uncertainty will be higher.
Figure 2.
Content of clinical decisions.
Thus, it is the interplay of issues in the content of clinical decisions, shown in ▶, that determines the nature of both the stimuli, or decision problems (familiar or unfamiliar), and the search behavior, or decision processes (analytic or intuitive), in Perrow's models as depicted in ▶. The ability of the clinician to incorporate these issues into the clinical decision with greater or lesser certainty and by intuitive or logical processes defines whether, in that moment, health care is being practiced predominantly as Craft, Routine, Engineering, or Nonroutine. The role of informatics is to reduce uncertainty in the human decision-making process by delivering state-of-the-art information, cues, and alerts and to offer well-defined decision algorithms where those exist. It remains a human grace and a professional responsibility to make intellectual leaps when uncertainty is unavoidable and to be creative when algorithms are inadequate.
Health Informatics: The Route to a Promised Land
In industries outside health care, informatics has led to “promised lands” of dramatically greater success by revolutionizing ways in which organizations have worked toward goals. If the functions of health informatics are to create and deliver knowledge, to reduce uncertainty in clinical decisions, and to support clinical work processes, how can informatics create new strategies to resolve the dilemma of health care in Western society? What innovations and applications of health informatics could provide the means to achieve an appropriate balance between health care's will to do good and its need to conserve or increase resources? Surely a “promised land” worth seeking would be one in which health care providers and agencies were able to generate reasonable income and avoid waste while fulfilling the social compact to restore and promote the health of individuals and the public.
Informatics leads to promised lands by making new strategies for success possible. Wal-Mart, Dell Computer, and Amazon.com greatly increased profits by, among other strategies, minimizing inventory and optimizing response to customer demand. Levi Strauss & Company carried these strategies further by offering customers, for a moderate surcharge, custom-fit jeans modified to measure from hundreds of templates stored in computer files, with selection and purchase available through in-store kiosks or over the Internet. This approach, called “mass customization,” enabled Levi's to give customers what they wanted while minimizing inventory, reducing purchase of materials, and avoiding manufacture of unwanted products, thereby increasing profits.
How might informatics make it possible for health care agencies to use mass customization to give clients the health care they want and need while reducing waste and generating appropriate income? Health care organizations could provide better care to patients and follow better business practices if they expanded the admission assessment or history and physical examination to include a detailed health profile, to be maintained in an institutional database. Epidemiologic analyses of the database would produce statistics on the current and projected incidence and prevalence of diseases and health risks, as well as the need for health promotion for age groups across the life span. From these statistics, each health care organization (or affiliated group of organizations) could make business and public health decisions about the “inventory” of medical expertise and health services to be maintained. It would make business sense, for example, to centralize in relatively few locations the specialists dealing with less prevalent conditions, to use telemedicine technologies for preliminary and follow-up care in those specialties, and to transport patients to the specialists only when in-person care is required.
For most of the population, most of the time, the detailed health profile (in an appropriate informatics infrastructure) would permit such personalized health care as follows:
Customized public health guidelines for screening to match the individual's health risks, with reminders automatically sent both to the primary care practitioner and to those patients who subscribe to a secure Internet service.
Unified care for an individual's multiple health problems and risks in the context of the family and the socioeconomic situation, with a case manager coordinating services and communication among a variety of providers.
Offer of health promotion services (fitness, nutrition, stress management, baby and child care, lifestage development, support groups, psychosocial services, etc.) in accordance with the health profile.
From the clinician's perspective, the commitment to personalized health care and the appropriate informatics infrastructure make better decisions for the patient's welfare possible by decreasing the unknowns in each component of the content of clinical decisions. The detailed health profile provides more information about the patient's health issues and concerns. Epidemiologic analyses of the aggregated patient data increase general knowledge of the effectiveness of interventions for health promotion, disease prevention, and treatment of illnesses. Frank consideration of ethics, policy, economics, and values helps providers and patients reach decisions about which services must be provided, which can be provided, and which are not to be provided. From accumulated knowledge will grow guidelines, protocols, pathways, and procedures for routinizing those aspects of care strongly supported by evidence. From aggregated experience will also grow algorithms to engineer commonly occurring modifications and customizations of care. Freed from the obligation to design the entire plan of care of each patient de novo, caregivers can devote their creative skills to those unique needs of individual patients that require original approaches to reach better health, and to true research and development of better health care modalities.
From the business perspective, mass customization of health care offers the possibility of efficiencies derived from reducing or eliminating those services, and the associated overhead, for which there is little demand. Other efficiencies come from being prepared to respond to the actual demand. Knowledge of the age, health status, family status, and socioeconomic status of patients makes it possible to market health promotion services to target groups, whether the payer is the individual, the employer, or a social services agency. Knowledge of the cost effectiveness of interventions facilitates shrewd decisions about which interventions to support. Detailed, longitudinal clinical data (as opposed to crude administrative data) permit understanding of which patient conditions justify more expensive interventions for a better ultimate outcome. Such knowledge confers a competitive advantage in obtaining contracts to provide care and in fulfilling the contracts cost effectively. Over time, if the population served is stable or if institutional data are further aggregated into public health databases, it will be possible to determine the value of services provided for health promotion and disease prevention. Which constellations of services have a detectable impact on long-term health? What are the economic consequences to the patient and family, the provider, the health care organization, and the payer? Answers to these questions will guide strategic planning, policy formation, and renewal of the social contract to promote and provide for the health of the population.
In the promised land, health care delivery would not consist of isolated transactions between providers and patients in response to discrete perceived needs. Instead, professionals would care for individual patients with awareness of each patient's total health situation and the ensemble of coordinated services, while contributing to and drawing from knowledge of population health. Personal health management would consist not merely of following professional advice but of increasing personal knowledge, involvement, and responsibility. Successful operation of health care organizations would be based not merely or even primarily on meeting short-term financial goals but on generating revenues, eliminating waste, and allocating resources to support the kind of care that increases the health of individuals and populations.
Getting to the Promised Land
A strong informatics infrastructure may be the route to the promised land of appropriate, personalized health care, but getting there is no mere drive through the park. To give clinicians the organizational technologies and the information they need to make sound clinical decisions, to give patients the care they need to optimize their health within their circumstances, and to give organizational officials the business advantages they need to keep resources flowing will require fundamental changes. However the organizational structure is drawn, clinicians are powerful players in health care organizations. Determining that a sound business case could not be made for retaining some specialties in a particular organization would not be easy, particularly because the decision would go against the self-interest of some of the decision makers. Finding an alternative that would serve the interests of all concerned would require ingenuity. Maintaining the detailed patient database that would yield the information to guide both clinical and business decisions would require great attention to security and confidentiality. Patients who entrusted such information to the organization would need to be repaid both by appropriate protections and by adequate rewards in the form of noticeably more personalized care—and perhaps by lower insurance premiums or copayments, if justified by economic efficiencies. Health care administrators may be enticed by the prospect of greater efficiencies and new revenue streams in the promised land, but it falls to them to pay for the journey. Can they be convinced that an expensive information system that supports patient care first and management second will yield richer rewards than a more conventional business-oriented system?
To set out for the promised land has historically required bold vision, significant investment, and faith that rewards were waiting over the horizon. Actually reaching the promised land has depended on navigation, luck, and divine providence. If informatics is to be the route to the promised land of health care, members of the American College of Medical Informatics may serve as visionary leaders, navigators, or proselytizers, but we will not get there alone. We must enlist the support of clinicians, administrators, and representatives of the public. We must convince them that health informatics can deliver them to a better world of health care, if they are willing to make some difficult changes to live in that world. And then we must prove worthy of their trust.
Acknowledgments
Among those whose ideas strongly influenced this paper are Robert Braude, Patricia Brennan, Charles Friedman, Lael Gatewood, William Hersh, Walter Pankow, and William Yasnoff. Dr. Hersh initially sketched the Venn diagram, inspired by one that appeared in Haynes et al.8 Mark Tuttle introduced the idea of a “promised land” in a presentation on Feb 13, 1999. Mark Frisse described the business strategy of mass customization in his presentation on Feb 14, 1999. This paper owes much to the ideas of my colleagues. Any errors of interpretation are my own.
This paper is based on discussions among the fellows of the American College of Medical Informatics (ACMI) during the 1999 ACMI Scientific Symposium, held Feb 12-14, 1999, in Tucson, Arizona.
References
- 1.Perrow C. Organizational analysis: a sociological view. Belmont, Calif.: Wadsworth, 1970.
- 2.Cohen EL. Nursing case management: does it pay? J Nurs Admin. 1991; 21(4):20-5. [PubMed] [Google Scholar]
- 3.Ethridge P, Lamb GS. Professional nursing case management improves quality, access and costs. Nurs Manage. 1989;20(3): 30-5. [PubMed] [Google Scholar]
- 4.Rosenstein AH. Cost-effective health care: tools for improvement. Health Care Manage Rev. 1994;10(2):53-61. [PubMed] [Google Scholar]
- 5.Nichol G, Walls R, Goldman L, et al. A critical pathway for management of patients with acute chest pain who are at low risk for myocardial ischemia: recommendations and potential impact. Ann Intern Med. 1997;127:996-1005. [DOI] [PubMed] [Google Scholar]
- 6.Koch MO, Seckin B, Smith JA. Impact of a collaborative care approach to radical cystectomy and urinary reconstruction. J Urol. 1995;154:996-1001. [PubMed] [Google Scholar]
- 7.Burton CS III. Treatment of leg ulcers. Dermatol Clin. 1993; 11(2):315-23. [PubMed] [Google Scholar]
- 8.Haynes RB, Sackett DL, Gray JRM, Cook DL, Guyatt GH. Transferring evidence from research into practice, Part 1: the role of clinical care research evidence in clinical decisions [editorial]. ACP J Club 1996;125:A14-16. [PubMed] [Google Scholar]